Abstract
Background:
Substantial weight loss in the setting of obesity has considerable metabolic benefits. Yet some studies have shown improvements in obesity-related metabolic comorbidities with more modest weight loss. By closely monitoring patients undergoing bariatric surgery, we aimed to determine the effects of weight loss on the metabolic syndrome and its components and determine the weight loss required for their resolution.
Methods:
We performed a prospective observational study of obese participants with metabolic syndrome (Adult Treatment Panel III criteria) who underwent laparoscopic adjustable gastric banding. Participants were assessed for all criteria of the metabolic syndrome monthly for the first 9 months, then 3-monthly until 24 months.
Results:
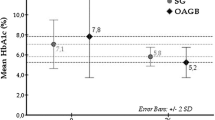
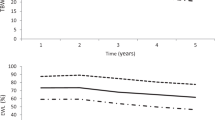
There were 89 participants with adequate longitudinal data. Baseline body mass index was 42.4±6.2 kg m−2 with an average age was 48.2±10.7 years. There were 56 (63%) women. Resolution of the metabolic syndrome occurred in 60 of the 89 participants (67%) at 12 months and 60 of the 75 participants (80%) at 24 months. The mean weight loss when metabolic syndrome resolved was 10.9±7.7% total body weight loss (TBWL). The median weight loss at which prevalence of disease halved was 7.0% TBWL (17.5% excess weight loss (EWL)) for hypertriglyceridaemia; 11% TBWL (26.1–28% EWL) for high-density lipoprotein cholesterol and hyperglycaemia; 20% TBWL (59.5% EWL) for hypertension and 29% TBWL (73.3% EWL) for waist circumference. The odds ratio for resolution of the metabolic syndrome with 10–12.5% TBWL was 2.09 (P=0.025), with increasing probability of resolution with more substantial weight loss.
Conclusions:
In obese participants with metabolic syndrome, a weight loss target of 10–12.5% TBWL (25–30% EWL) is a reasonable initial goal associated with significant odds of having metabolic benefits. If minimal improvements are seen with this initial target, additional weight loss substantially increases the probability of resolution.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout




Similar content being viewed by others
References
Despres J-P, Lemieux I . Abdominal obesity and metabolic syndrome. Nature 2006; 444: 881–888.
Whitlock G, Lewington S, Sherliker P, Clarke R, Emberson J, Halsey J et al. Body-mass index and cause-specific mortality in 900,000 adults: collaborative analyses of 57 prospective studies. Lancet 2009; 373: 1083–1096.
O'Brien PE, MacDonald L, Anderson M, Brennan L, Brown WA . Long-term outcomes after bariatric surgery: fifteen-year follow-up of adjustable gastric banding and a systematic review of the bariatric surgical literature. Ann Surg 2013; 257: 87–94.
Grundy SM, Cleeman JI, Daniels SR, Donato KA, Eckel RH, Franklin BA et al. Diagnosis and management of the metabolic syndrome: an American Heart Association/National Heart, Lung, and Blood Institute Scientific statement. Circulation 2005; 112: 2735–2752.
Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults. Executive summary of the third report of The National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III). JAMA 2001; 285: 2486–2497.
Dixon JB, le Roux CW, Rubino F, Zimmet P . Bariatric surgery for type 2 diabetes. Lancet 2012; 379: 2300–2311.
Slabek JA, Grimm MS, Larson CJ, Mathiason MB, Lambert PJ, Kothari SN . The effect of laparoscopic gastric bypass surgery on dyslipidemia in severely obese patients. Surg Obes Relat Dis 2005; 1: 537–542.
Sjostrom L, Peltonen M, Jacobson P, Sjostrom CD, Karason K, Wedel H et al. Bariatric surgery and long-term cardiovascular events. JAMA 2012; 307: 56–65.
Ricci C, Gaeta M, Rausa E, Asti E, Bandera F, Bonavina L . Long-term effects of bariatric surgery on type II diabetes, hypertension and hyperlipidemia: a meta-analysis and meta-regression study with 5-year follow-up. Obes Surg 2015; 25: 397–405.
Ades PA, Savage PD . Potential benefits of weight loss in coronary heart disease. Prog Cardiovasc Dis 2014; 56: 448–456.
Tuomilehto J, Lindstrom J, Eriksson JG, Valle TT, Hamalainen H, Ilanne-Parikka P et al. Prevention of type 2 diabetes mellitus by changes in lifestyle among subjects with impaired glucose tolerance. N Engl J Med 2001; 344: 1343–1350.
Wing RR, Lang W, Wadden TA, Safford M, Knowler W, Bertoni AG et al. Benefits of modest weight loss in improving cardiovascular risk factors with overweight and obese individuals with type 2 diabetes. Diabetes Care 2011; 34: 1481–1486.
Bray G, Look M, Ryan D . Treatment of the obese patient in primary care: targeting and meeting goals and expectations. Postgrad Med 2013; 125: 67–77.
Gloy VL, Briel M, Bhatt DL, Kashyap SR, Schauer PR, Mingrone G et al. Bariatric surgery versus non-surgical treatment for obesity: a systematic review and meta-analysis of randomised controlled trials. BMJ 2013; 347: f5934.
Laaksonen DE, Lakka HM, Niskanen LK, Kaplan GA, Salonen JT, Lakka TA . Metabolic syndrome and development of diabetes mellitus: aplication and validation of recently suggested definitions of the metabolic syndrome in a prospective cohort study. Am J Epidemiol 2002; 156: 1070–1077.
Bhargava A . A longitudinal analysis of the risk factors for diabetes and coronary heart disease in the Framingham Offspring STudy. Popul Health Metr 2003; 1: 3.
Alberti KGMM, Zimmett PZ . Definition, diagnosis and classification of diabetes mellitus and its complications. Part 1: Diagnosis and classificaiton of diabetes mellitus provisional report of a WHO consultation. Diabet Med 1998; 15: 539–553.
Alberti KGMM, Zimmet P, Shaw J . Metabolic syndrome - a new world-wide definition. A consensus statement from the International Diabetes Federation. Diabet Med 2006; 23: 469–480.
Simmons RK, KGMM Alberti, Gale EAM, Colagiuri S, Tuomilehto J, Qiao Q et al. The metabolic syndrome: useful concept or clinical tool? Report of a WHO Expert Consultation. Diabetologia 2010; 53: 600–605.
Ford ES . The metabolic syndrome and mortality from cardiovascular disease and all-causes: findings from the National Health and Nutrition Examination Survey II Mortality Study. Atherosclerosis 2004; 173: 309–314.
Burton PR, Brown WA . The mechanism of weight loss after laparoscopic adjustable gastric banding: induction of satiety not restriction. Int J Obes 2011; 35: S26–S30.
O'Brien P . The Lap-Band Solution: A Partnership for Weight Loss. Melbourne University Publishing: Carlton, Victoria, Australia, 2010.
D'Agostino RB, Vasan RS, Pencina MJ, Wolf PA, Cobain M, Massaro JM et al. General cardiovascular risk profile for use in primary care: the Framingham Heart Study. Circulation 2008; 117: 743–753.
Magkos F, Fraterrigo G, Yoshino J, Luecking C, Kirbach K, Kelly SC et al. Effects of moderate and subsequent progressive weight loss on metabolic function and adipose tissue biology in humans with obesity. Cell Metab 2016; 23: 1–11.
Vogel JA, Franklin BA, Zalesin KC, Trivax JE, Krause KR, Chengelis DL et al. Reduction in predicted coronary heart disease risk after substantial weight reduction after bariatric surgery. Am J Cardiol 2007; 99: 222–226.
The Look AHEAD Research Group. The Look AHEAD Study: a description of the lifestyle intervention and the evidence supporting it. Obesity 2006; 14: 737–752.
Habib P, Scrocco JD, Terek M, Vanek V, Mikolich JR . Effects of bariatric surgery on inflammatory, functional and structural markers of coronary atherosclerosis. Am J Cardiol 2009; 104: 1251–1255.
Blackman A, Foster GD, Zammit G, Rosenberg R, Aronne L, Wadden T et al. Effect of liraglutide 3.0 mg in individuals with obesity and moderate or severe obstructive sleep apnea: the SCALE Sleep Apnea randomized clinical trial. Int J Obes (2005) 2016; 40: 1310–1319.
Crane J, McGowan B . The GLP-1 agonist, liraglutide, as a pharmacotherapy for obesity. Ther Adv Chronic Dis 2016; 7: 92–107.
Mason EE, Printen KJ, Lewis JW, Scott DH, Blommers TJ . Gastric bypass criteria for effectiveness. Int J Obes 1981; 5: 405–411.
Brolin RE . Critical analysis of results: weight loss and quality of data. Am J Clin Nutr 1992; 55: 557S–581S.
Brown WA, Moszkowicz J, Brennan L, Burton PR, Anderson M, O'Brien PE . Pre-operative weight loss does not predict weight loss following laparoscopic adjustable gastric banding. Obes Surg 2013; 2: 2.
Reaven GM . Role of insulin resistance in human disease. Diabetes 1988; 37: 1595–1607.
Mottillo S, Filion KB, Genest J, Joseph L, Pilote L, Poirier P et al. The metabolic syndrome and cardiovascular risk: a systematic review and meta-analysis. J Am Coll Cardiol 2010; 56: 1113–1132.
Kahn R, Buse J, Ferrannini E, Stern M . The metabolic syndrome: time for a critical appraisal. Diabetes Care 2005; 28: 2289–2304.
Dixon AF, Dixon JB, O'Brien PE . Laparoscopic adjustable gastric banding induces prolonged satiety: a randomized blind crossover study. J Clin Endocrinol Metab 2005; 90: 813–819.
Tao LX, Yang K, Liu XT, Cao K, Zhu HP, Luo YX et al. Longitudinal associations between triglycerides and metabolic syndrome components in a Beijing adult population, 2007-2012. Int J Med Sci 2016; 13: 445–450.
Vliet-Ostaptchouk JV, Nuotio ML, Slagter SN, Doiron D, Fischer K, Foco L et al. The prevalence of metabolic syndrome and metabolically healthy obesity in Europe: a collaborative analysis of ten large cohort studies. BMC Endocr Disord 2014; 14: 9.
Acknowledgements
We acknowledge the kind support of the Royal Australasian College of Surgeons and the National Health and Medical Research Council for supporting GJO and LD in their higher degrees and in completing this research. We thank Ms Cheryl Laurie, Ms Julie Playfair, Mr Stuart Skinner, Mr Gary Crosthwaite, Mr Stephen Blamey and Mr Andrew Smith for their contribution and enthusiasm in recruitment and follow-up of participants and collection of samples.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
GJO, LD, TT, CL, PRB, PEO’B and WAB report being affiliated with the Centre for Obesity Research and Education. The Centre has received funding for research purposes from Allergan and Apollo Endosurgery, the manufacturers of the LapBand. The grant is not tied to any specific research project, and Allergan has no control of the protocol, analysis and reporting of any studies. CORE also receives a grant from Applied Medical towards educational programs. WAB reports financial support for a bariatric surgery registry from the Commonwealth of Australia, Apollo Endosurgery, Covidien, Johnson and Johnson, Gore and Applied Medical and a speaker’s honorarium from Merck Sharpe and Dohme. These are outside of the submitted work. MAC reports grants and personal fees from Novo Nordisk, personal fees and other from Orexigen Therapeutics, outside the submitted work. KS is the Director of Clinical Support Services at Sonic Healthcare; this is unrelated to this work. CWlR has received funding from the Science Foundation Ireland (12/YI/B2480). He also serves on the advisory boards of NovoNordisk and Herbalife and has received speakers fees from Ethicon EndoSurgery. GJO and LD report scholarships from the National Health and Medical Research Council and the Royal Australasian College of Surgeons. PEO’B has written a patient information book entitled ‘The Lap-Band Solution: A partnership for weight loss’, which is given to patients without charge, but some are sold to surgeons and others, for which he receives a royalty. JMW and AE have no other relevant disclosures.
Additional information
Supplementary Information accompanies this paper on International Journal of Obesity website
Supplementary information
Rights and permissions
About this article
Cite this article
Ooi, G., Doyle, L., Tie, T. et al. Weight loss after laparoscopic adjustable gastric band and resolution of the metabolic syndrome and its components. Int J Obes 41, 902–908 (2017). https://doi.org/10.1038/ijo.2017.59
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/ijo.2017.59
This article is cited by
-
Reduction of prevalence of patients meeting the criteria for metabolic syndrome with tirzepatide: a post hoc analysis from the SURPASS Clinical Trial Program
Cardiovascular Diabetology (2024)
-
Standardization of Bariatric Metabolic Procedures: World Consensus Meeting Statement
Obesity Surgery (2019)
-
Diabetes Outcomes More than a Decade Following Sustained Weight Loss After Laparoscopic Adjustable Gastric Band Surgery
Obesity Surgery (2018)
-
Visual Liver Score to Stratify Non-Alcoholic Steatohepatitis Risk and Determine Selective Intraoperative Liver Biopsy in Obesity
Obesity Surgery (2018)
-
The Role of Metabolic Surgery in Non-alcoholic Steatohepatitis Improvement
Current Atherosclerosis Reports (2017)