Abstract
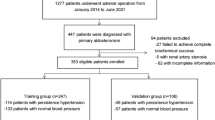
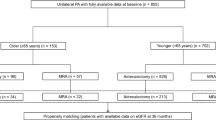
The effect of unilateral adrenalectomy on blood pressure (BP) outcome in primary aldosteronism (PA) is diverse. Therefore, we sought to investigate the preoperative factors contributing to postoperative BP outcome. Data for 96 PA patients who underwent unilateral adrenalectomy at our institution from January 2000 to February 2015 were retrospectively collected. Based on postoperative BP after a 12-month follow-up period, the patients were categorized into two groups: cured (C) (<140/90 mm Hg with no antihypertensive drug) and not cured (NC) (if not normotensive). Patient demographics, blood and urine data, data of loading tests and adrenal vein sampling were evaluated. In all, 46 patients were categorized as C and 50 patients as NC. There were significantly more males in the NC group. Age, body mass index (BMI), number of antihypertensive drugs prescribed, serum uric acid concentration and contralateral ratio (CR) after adrenocorticotropic hormone stimulation were significantly higher in the NC group. In the multivariate model, BMI and CR significantly correlated with resolution outcome. The optimal cutoff values were 23.3 kg m−2 for BMI and 0.5 for CR, and when both parameters were used as predictors, the most optimal cutoff values for BMI and CR were 25.2 kg m−2 and 0.1, respectively. BMI and CR significantly correlated with BP outcome after adrenalectomy. To our knowledge, this is the first report to show that in addition to BMI, CR is a factor in postoperative BP outcome and to determine the optimal cutoff values of BMI and CR and calculate their sensitivities and specificities.
Similar content being viewed by others
Introduction
Primary aldosteronism (PA) is a state in which inappropriate secretion of the mineralocorticoid aldosterone occurs from one or both adrenal glands. Although the true prevalence of PA is difficult to determine, it is a common form of secondary hypertension and has been reported to account for 1 to 10% of hypertensive patients.1, 2 It is associated with cardiovascular,3, 4, 5 renal6, 7, 8 and metabolic9, 10, 11 complications, independent of the organ damage caused by an increase in blood pressure (BP).
Therapeutic options for PA are medical management and surgery. Medical treatment is preferred when the disease is determined as bilateral or when surgery is contraindicated. In cases of unilateral disease, unilateral adrenalectomy is now recognized as the standard therapy. However, the effect of unilateral adrenalectomy on BP outcome in PA is thought to be diverse.12 To predict the postoperative resolution of hypertension, several studies have evaluated the preoperative characteristics of PA patients.13, 14 Factors that have been associated with BP outcome include age, sex, body weight, hypokalemia, duration of hypertension, number of antihypertensive drugs, preoperative response to aldosterone and TT genotype of the aldosterone synthase gene.15, 16, 17, 18, 19, 20 Aldosteronoma Resolution Score, which includes (1) ⩽2 antihypertensive medications, (2) body mass index (BMI) ⩽25 kg m−2, (3) duration of hypertension ⩽6 years and (4) female sex, has been reported to accurately identify individuals at high likelihood of cure in terms of BP reduction after adrenalectomy.13, 21 However, varying measures of disease cure are included in the primary outcomes of these studies.
It has also been reported that treatment with a mineralocorticoid receptor blocker has an effect equivalent to that of surgical treatment in patients with unilateral disease. Prospective studies indicate that mineralocorticoid receptor blockers have therapeutic values comparable to adrenalectomy in terms of correcting metabolic abnormalities22, 23 and reducing the risk of cardiovascular diseases3, 4 and renal disease22, 23, 24 progression. This evidence makes it difficult to select appropriate treatment in PA patients with unilateral disease. However, there is no doubt that the discontinuation of antihypertensive drugs for a lifetime will significantly improve one’s quality of life.
The aim of this study was to retrospectively investigate the preoperative factors contributing to postoperative BP outcome and to determine specific cutoff values for each continuous variable. To our knowledge, this is the first report to show that in addition to BMI, contralateral ratio (CR) is a factor in postoperative BP outcome by analyzing the data from adrenal vein sampling (AVS) and to determine the optimal cutoff values of BMI and CR and calculate their sensitivities and specificities.
Methods
Study population and design
This study is a retrospective review of prospectively collected data from 96 patients with PA who had undergone laparoscopic unilateral adrenalectomy at Tokyo Women’s Medical University Hospital from January 2000 to February 2015. Adrenalectomy was recommended when the lateralized ratio (LR) after adrenocorticotropic hormone (ACTH) stimulation was over 2.6. The study was approved by the ethical review committee of Tokyo Women’s Medical University Hospital.
Patient characteristics were obtained from medical records. Information including age, gender, BMI, presence of complications of diabetes mellitus and dyslipidemia, past history of cerebrovascular disease, smoking and drinking habits, family history of hypertension, number and type of prescribed antihypertensive agents and presence of K+ supplementation was obtained at their first visit. Serum K+, creatinine, uric acid (UA), plasma aldosterone concentration (PAC) and plasma renin activity from venous blood samples were measured with the patient in a sitting position (for at least 15 min) at their first admission, after they had been under antihypertensive treatment with only calcium channel blockers and an α-blocker for >3 weeks. The estimated glomerular filtration rate (eGFR) and aldosterone/renin ratio were calculated. Urinary aldosterone excretion and Na+/K+ ratio were evaluated in overnight urine samples during admission. The necessity for mineralocorticoid receptor blocker medication (after diagnosis) until the operation was also evaluated. Information regarding tumor diameter (maximum diameter on computed tomography), pathologic diagnosis and postoperative medications and BP was collected.
Loading tests
Three loading tests for the diagnosis of PA—the captopril challenge test, the furosemide upright test and the saline loading test—were performed. The aldosterone/renin ratio during the captopril challenge test, peak plasma renin activity level during the furosemide upright test and trough PAC during the saline loading test were evaluated. To detect the presence of the autonomous secretion of cortisol along with aldosterone, we also performed an overnight 1 mg dexamethasone suppression test.
Adrenal vein sampling
AVS was performed as described previously.25 Only calcium channel blockers and an α-blocker were used as antihypertensive medications. Successful cannulation of the adrenal vein was confirmed by adequate adrenal vein to peripheral vein cortisol ratios (>5.0 after ACTH stimulation). Aldosterone to cortisol (A/F) ratios were then calculated to correct PACs for dilution from nonadrenal blood. We also evaluated LR (A/Fdominant:A/Fnondominant) and CR (A/Fnondominant:A/Fperipheral) both before and after ACTH stimulation. The result was considered to demonstrate contralateral suppression (CS) if CR after ACTH stimulation was <1.0.
Outcomes
Office BP was obtained at regular postoperative follow-up with the patient in a sitting position after resting for at least 5 min. The first reading was used in this study. Hypertension was defined as ‘cured (C)’ if patients remained normotensive (BP <140/90 mm Hg) without taking any antihypertensive agents and as ‘not cured (NC)’ if not normotensive after a 12-month follow-up period.
Statistics
All statistical analyses were performed with JMP Pro 12.1.0 software (SAS Institute, Cary, NC, USA). Patient characteristics of each group were compared and analyzed using Student’s t-test for continuous data, and Pearson’s χ2 test was used for categorical data. A P-value of <0.05 was considered statistically significant. Multivariate logistic regression modeling was performed on variables demonstrating statistical significance in the univariate modeling.
To review the sensitivity and specificity of preoperative variables that showed statistical significance in the multivariate modeling, we constructed receiver operating characteristic (ROC) analyses.
Results
From January 2000 to February 2015, a total of 96 PA patients underwent laparoscopic unilateral adrenalectomies at our institution. All of the patients underwent successful AVS. LR was over 2.6 in 83 patients. Although 13 patients did not meet this criterion, 8 of them underwent adrenalectomy because their AVS results revealed contralateral suppression (CR <1). The remaining 5 patients met neither criterion, but the patients desired to have surgery (tumor resection). Tables 1 and 2 show the age, gender distribution, BMI, number of type of prescribed antihypertensive medications, serum K+, UA, eGFR, PAC, plasma renin activity and aldosterone/renin ratio at rest, the results of the loading tests and the AVS data for the entire population.
Patient characteristics by cured vs. not cured
In all, 46 patients were categorized as C and 50 as NC, according to the method mentioned above (Table 1). Autonomous cortisol secretion was observed in 5 patients, all of them in the NC group. Histopathological diagnoses were cortical adenoma, nodular hyperplasia or cortical adenoma with hyperplasia. There were no cases of microadenoma. A significant difference was seen in age at surgery between the two groups (47±12 vs. 55±10 years old, P=0.0009). There were significantly more males in the NC group than in the C group. BMI was significantly higher in the NC group (21.8±3.4 (30.3–16.4) vs. 24.6±3.0 (32.2–18.6) kg m−2, P<0.0001). More types of antihypertensive drugs were prescribed in the NC group before surgery (1.1±0.7 vs. 1.5±1.0, P=0.0338). Preoperative UA also significantly differed between the two groups (4.4±1.1 vs. 5.5±1.4 mg dl−1, P<0.0001). We constructed a multivariate logistic regression model that included gender and UA as the only variables and revealed that UA (β=−0.609, P=0.0034) was an independent predictive factor, but gender (β=−0.370, P=0.1360) was not.
Patients’ diagnostic characteristics by cured and not cured
Diagnostic measures are compared in Table 2. All patients met the diagnostic criteria for three loading tests in the C group, whereas in the NC group two patients did not meet the diagnostic criteria for the captopril challenge test, another patient did not meet the criteria for the captopril challenge test and another patient did not meet the criteria for the saline loading test. The results of the three loading tests did not differ between the two groups. In the AVS results, there were no significant differences in PAC levels for the affected side, LR or CR, before ACTH stimulation. However, after ACTH stimulation, CR was significantly lower (0.4±0.2 (1.1–0.1) vs. 0.7±0.6 (2.6–0.1), P=0.0003), and the percentage of patients with CS was higher (97.6 vs. 76.2%, P=0.0041) in the C group. There was no significant difference in LR after ACTH stimulation between the two groups (13.5±12.1 (56.1–1.2) vs. 12.9±13.8 (71.6–1.1), P=0.8576).
Results of multivariate logistic regression analysis
We constructed a multivariate logistic regression model including all preoperative variables that demonstrated statistical significance between the C and NC groups for the BP outcome following unilateral adrenalectomy (Table 3). BMI (P=0.0473) and CR (P=0.0199) significantly correlated with resolution outcome; however, gender, age, numbers of types of preoperatively prescribed antihypertensive medications and UA did not.
ROC characteristic analysis of BMI and CR
Using BMI and CR, we constructed ROC curves to evaluate their utility as predictors of postoperative outcome (Figure 1). When BMI was used as a predictor, the area under the ROC curve was 73.4% and the highest combination of sensitivity and specificity was obtained at a BMI of 23.2 kg m−2 (sensitivity, 67.4% specificity, 74.0%). When CR was evaluated, the area under the ROC curve was 64.7% and the highest combination of sensitivity and specificity was obtained at a CR of 0.5 (sensitivity, 82.9% specificity 42.9%). The area under the ROC curve reached up to 79.4% when both BMI and CR were used as predictors, and the optimal cutoff values for BMI and CR were 25.2 kg m−2 and 0.1, respectively (sensitivity, 73.2% specificity, 76.2%).
Discussion
The present study showed that in the univariate model, age, BMI, number of antihypertensive drugs prescribed, uric acid and CR after adrenocorticotropic hormone stimulation were significantly higher in the NC group. BMI and CR significantly correlated with BP outcome in the multivariate model. The optimal cutoff values were 23.2 kg m−2 for BMI and 0.5 for CR and when both parameters were used as predictors, the optimal cutoff values for BMI and CR were 25.2 kg m−2 and 0.1, respectively.
Characteristics such as older age,18, 26, 27, 28, 29, 30, 31, 32 male sex,26, 33 presence of family history of hypertension,27, 30 longer duration of hypertension27, 30, 34 and renal dysfunction35 have previously been reported to correlate with BP outcome following unilateral adrenalectomy in PA patients. We found no association between the presence of a family history of hypertension and BP outcome, probably because of the high prevalence of hypertension in Japanese populations. In addition, eGFR was independent of operative outcome in this study, in contrast to previous reports, possibly because the renal function of our study population was relatively preserved (mean eGFR was 78.2±20.8). The mean eGFR of the NC group tended to be lower than that of the C group, although the difference was not significant. In the present study, age and male sex were associated with BP outcome in the univariate but not in the multivariate analysis. Data regarding the duration of hypertension could not be collected in our study because of its retrospective nature.
Low serum UA levels predicted the postoperative resolution of hypertension in a single regression model. It seemed that the high proportion of males affected the results for UA in the NC group, and hence we constructed a multivariate logistic regression model that included gender and UA as the only variables. This revealed that UA was an independent predictive factor, but gender was not, indicating that a high UA level affected the gender distribution in the NC group. Hyperuricemia is highly prevalent among hypertensive patients, including essential hypertension, renal parenchymal hypertension and renovascular hypertension, but not in PA. UA transport is said to be closely related to sodium transport in the renal tubules, particularly at the proximal site, and could also lead to the conclusion that the lower serum UA in PA resulted from the suppression of reabsorption and/or an enhancement of the secretion of UA in the proximal tubule, related to the so-called escape phenomenon.36 Preoperative low serum UA levels may indicate that the rise in BP is due solely to hyperaldosteronism and that hypertension will resolve after adrenalectomy.
Obesity independently alters cardiovascular hemodynamics and impairs cardiac performance.37 It has also been recognized as a predictor of cure following adrenalectomy in PA patients.19, 20 The present study also supports this finding. In a univariate and multivariate regression analysis, BMI was significantly higher in the C group. The association between adipose mass and hyperaldosteronism has been suspected in diverse populations.38 Increased adiposity has been linked to alterations in adrenal function, with increased aldosterone production and mineralocorticoid receptor activity via ‘adipose-adrenal crosstalk’.39, 40 In addition to aldosterone, adipokines such as leptin, adiponectin and osteopontin are also independently linked to hypertension. Hyperinsulinemia is also associated with the development of hypertension because of activation of the sympathetic nervous system.41 Lifestyle factors often observed in overweight patients, including sedentary behavior, excess sodium intake and low potassium intake, also lead to an increase in BP. Hypertension may persist in obese patients even after adrenalectomy, through these diverse mechanisms of the residual obesity.
In PA, AVS is well established as the most reliable method for localization of excess aldosterone production. The present study revealed that patients with CS and lower CR values had better BP outcomes in both a single model and a multivariate regression model. Wolley et al.25 previously assessed 80 patients who underwent unilateral adrenalectomy after successful AVS and found that those with CS had lower postoperative BP and a greater proportion showed cure or improvement of hypertension as well as biochemical cure of PA on fludrocortisone suppression testing. It can be interpreted that abnormal reaction of the contralateral adrenal gland and normal to increased aldosterone production under suppressed renin activity indicate autonomous excretion of aldosterone from the contralateral side, predicting residual hyperaldosteronism after resection of the dominant side. In a previous multicenter study that evaluated 234 patients who underwent AVS procedures before unilateral adrenalectomy, the presence or absence of CS did not correlate with BP outcome.42 However, because eight separate centers were included in this study, protocols to diagnose PA and unilateral disease were not standardized and there was heterogeneity in the patients’ background characteristics.
We also assessed the results to determine the most reliable values for predicting the postoperative BP outcome and found that a BMI of 23.2 and a CR of 0.5 gave the most acceptable sensitivity and specificity. When these two variables were combined, a BMI of 25.2 and a CR of 0.1 were the optimal values, and the area under the ROC curve reached up to 0.7938, increasing the accuracy of prediction of the postsurgery BP outcome.
One of the limitations of our study is that it was based on retrospective data. Although prospective validation would be ideal as all the variables evaluated were objective clinical information and we had a high rate of complete data collection, it is unlikely that the results would be very different if analyzed prospectively. Another weakness of the present study is that the outcome measure of cure was not confirmed biochemically, and whether it represented a true cure is unknown. The strength of the present study is that although AVS is an invasive and difficult technique, a large number of patients in this study underwent AVS and were examined before and after administration of ACTH, making it possible to evaluate various indicators.
In conclusion, BMI and the presence of CS and CR values independently predicted BP outcome after unilateral adrenalectomy in PA patients. Referring to BMI and CR preoperatively may be helpful to determine the appropriate treatment—surgical or medical—for PA patients.
References
Hood S, Cannon J, Foo R, Brown M . Prevalence of primary hyperaldosteronism assessed by aldosterone/renin ratio and spironolactone testing. Clin Med 2005; 5: 55–60.
Mosso L, Carvajal C, Gonzalez A, Barraza A, Avila F, Montero J, Huete A, Gederlini A, Fardella CE . Primary aldosteronism and hypertensive disease. Hypertension 2003; 42: 161–165.
Catena C, Colussi G, Nadalini E, Chiuch A, Baroselli S, Lapenna R, Sechi LA . Cardiovascular outcomes in patients with primary aldosteronism after treatment. Arch Intern Med 2008; 168: 80–85.
Mulatero P, Monticone S, Bertello C, Viola A, Tizzani D, Iannaccone A, Crudo V, Burrello J, Milan A, Rabbia F, Veglio F . Long-term cardio- and cerebrovascular events in patients with primary aldosteronism. J Clin Endocrinol Metabol 2013; 98: 4826–4833.
Savard S, Amar L, Plouin PF, Steichen O . Cardiovascular complications associated with primary aldosteronism: a controlled cross-sectional study. Hypertension 2013; 62: 331–336.
Rossi GP, Bernini G, Desideri G, Fabris B, Ferri C, Giacchetti G, Letizia C, Maccario M, Mannelli M, Matterello MJ, Montemurro D, Palumbo G, Rizzoni D, Rossi E, Pessina AC, Mantero F,, PAPY Study Participants. Renal damage in primary aldosteronism: results of the PAPY Study. Hypertension 2006; 48: 232–238.
Reincke M, Rump LC, Quinkler M, Hahner S, Diederich S, Lorenz R, Seufert J, Schirpenbach C, Beuschlein F, Bidlingmaier M, Meisinger C, Holle R, Endres S,, Participants of German Conn's Registry. Risk factors associated with a low glomerular filtration rate in primary aldosteronism. J Clin Endocrinol Metabol 2009; 94: 869–875.
Sechi LA, Catena C . The dual role of the kidney in primary aldosteronism: key determinant in rescue from volume expansion and persistence of hypertension. Am J Kidney Dis 2009; 54: 594–597.
Giacchetti G, Ronconi V, Turchi F, Agostinelli L, Mantero F, Rilli S, Boscaro M . Aldosterone as a key mediator of the cardiometabolic syndrome in primary aldosteronism: an observational study. J Hypertens 2007; 25: 177–186.
Fallo F, Veglio F, Bertello C, Sonino N, Della Mea P, Ermani M, Rabbia F, Federspil G, Mulatero P . Prevalence and characteristics of the metabolic syndrome in primary aldosteronism. J Clin Endocrinol Metabol 2006; 91: 454–459.
Catena C, Colussi G, Frangipane A, Russo A, Verheyen ND, Sechi LA . Carotid artery stiffness is related to hyperinsulinemia and insulin-resistance in middle-aged, non-diabetic hypertensive patients. Nutr Metabol Cardiovasc Dis 2015; 25: 968–974.
Waldmann J, Maurer L, Holler J, Kann PH, Ramaswamy A, Bartsch DK, Langer P . Outcome of surgery for primary hyperaldosteronism. World J Surg 2011; 35: 2422–2427.
Zarnegar R, Young WF Jr, Lee J, Sweet MP, Kebebew E, Farley DR, Thompson GB, Grant CS, Clark OH, Duh QY . The aldosteronoma resolution score: predicting complete resolution of hypertension after adrenalectomy for aldosteronoma. Ann Surg 2008; 247: 511–518.
Utsumi T, Kamiya N, Endo T, Yano M, Kamijima S, Kawamura K, Imamoto T, Naya Y, Ichikawa T, Suzuki H . Development of a novel nomogram to predict hypertension cure after laparoscopic adrenalectomy in patients with primary aldosteronism. World J Surg 2014; 38: 2640–2644.
Wang W, Hu W, Zhang X, Wang B, Bin C, Huang H . Predictors of successful outcome after adrenalectomy for primary aldosteronism. Int Surg 2012; 97: 104–111.
Rossi GP, Bolognesi M, Rizzoni D, Seccia TM, Piva A, Porteri E, Tiberio GA, Giulini SM, Agabiti-Rosei E, Pessina AC . Vascular remodeling and duration of hypertension predict outcome of adrenalectomy in primary aldosteronism patients. Hypertension 2008; 51: 1366–1371.
Letavernier E, Peyrard S, Amar L, Zinzindohoue F, Fiquet B, Plouin PF . Blood pressure outcome of adrenalectomy in patients with primary hyperaldosteronism with or without unilateral adenoma. J Hypertens 2008; 26: 1816–1823.
Lumachi F, Ermani M, Basso SM, Armanini D, Iacobone M, Favia G . Long-term results of adrenalectomy in patients with aldosterone-producing adenomas: multivariate analysis of factors affecting unresolved hypertension and review of the literature. Am Surg 2005; 71: 864–869.
Carter Y, Roy M, Sippel RS, Chen H . Persistent hypertension after adrenalectomy for an aldosterone-producing adenoma: weight as a critical prognostic factor for aldosterone's lasting effect on the cardiac and vascular systems. J Surg Res 2012; 177: 241–247.
Kazaure HS, Roman SA, Sosa JA . Obesity is a predictor of morbidity in 1629 patients who underwent adrenalectomy. World J Surg 2011; 35: 1287–1295.
Utsumi T, Kawamura K, Imamoto T, Kamiya N, Komiya A, Suzuki S, Nagano H, Tanaka T, Nihei N, Naya Y, Suzuki H, Tatsuno I, Ichikawa T . High predictive accuracy of Aldosteronoma Resolution Score in Japanese patients with aldosterone-producing adenoma. Surgery 2012; 151: 437–443.
Catena C, Lapenna R, Baroselli S, Nadalini E, Colussi G, Novello M, Favret G, Melis A, Cavarape A, Sechi LA . Insulin sensitivity in patients with primary aldosteronism: a follow-up study. J Clin Endocrinol Metabol 2006; 91: 3457–3463.
Karashima S, Yoneda T, Kometani M, Ohe M, Mori S, Sawamura T, Furukawa K, Seta T, Yamagishi M, Takeda Y . Comparison of eplerenone and spironolactone for the treatment of primary aldosteronism. Hypertens Res 2016; 39: 133–137.
Catena C, Colussi G, Lapenna R, Nadalini E, Chiuch A, Gianfagna P, Sechi LA . Long-term cardiac effects of adrenalectomy or mineralocorticoid antagonists in patients with primary aldosteronism. Hypertension 2007; 50: 911–918.
Wolley MJ, Gordon RD, Ahmed AH, Stowasser M . Does contralateral suppression at adrenal venous sampling predict outcome following unilateral adrenalectomy for primary aldosteronism? A retrospective study. J Clin Endocrinol Metabol 2015; 100: 1477–1484.
Stowasser M, Klemm SA, Tunny TJ, Storie WJ, Rutherford JC, Gordon RD . Response to unilateral adrenalectomy for aldosterone-producing adenoma: effect of potassium levels and angiotensin responsiveness. Clin Exp Pharmacol Physiolo 1994; 21: 319–322.
Sawka AM, Young WF, Thompson GB, Grant CS, Farley DR, Leibson C, van Heerden JA . Primary aldosteronism: factors associated with normalization of blood pressure after surgery. Ann Intern Med 2001; 135: 258–261.
Massien-Simon C, Battaglia C, Chatellier G, Guyene TT, Duclos JM, Plouin PF . Conn's adenoma. Diagnostic and prognostic value of the measurement of potassium, renin, aldosterone levels and the aldosterone/renin ratio. Presse Med 1995; 24: 1238–1242.
Obara T, Ito Y, Okamoto T, Kanaji Y, Yamashita T, Aiba M, Fujimoto Y . Risk factors associated with postoperative persistent hypertension in patients with primary aldosteronism. Surgery 1992; 112: 987–993.
Proye CA, Mulliez EA, Carnaille BM, Lecomte-Houcke M, Decoulx M, Wemeau JL, Lefebvre J, Racadot A, Ernst O, Huglo D, Carre A . Essential hypertension: first reason for persistent hypertension after unilateral adrenalectomy for primary aldosteronism? Surgery 1998; 124: 1128–1133.
Pang TC, Bambach C, Monaghan JC, Sidhu SB, Bune A, Delbridge LW, Sywak MS . Outcomes of laparoscopic adrenalectomy for hyperaldosteronism. ANZ J Surg 2007; 77: 768–773.
Blumenfeld JD, Sealey JE, Schlussel Y, Vaughan ED Jr, Sos TA, Atlas SA, Muller FB, Acevedo R, Ulick S, Laragh JH . Diagnosis and treatment of primary hyperaldosteronism. Ann Intern Med 1994; 121: 877–885.
Montori VM, Young WF Jr . Use of plasma aldosterone concentration-to-plasma renin activity ratio as a screening test for primary aldosteronism. A systematic review of the literature. Endocrinol Metabol Clin North Am 2002; 31: 619–632,xi.
Meria P, Kempf BF, Hermieu JF, Plouin PF, Duclos JM . Laparoscopic management of primary hyperaldosteronism: clinical experience with 212 cases. J Urol 2003; 169: 32–35.
Wachtel H, Cerullo I, Bartlett EK, Kelz RR, Cohen DL, Karakousis GC, Roses RE, Fraker DL . Long-term blood pressure control in patients undergoing adrenalectomy for primary hyperaldosteronism. Surgery 2014; 156: 1394–1402,discussion 1402–1393.
Namba M, Kikuchi K, Komura H, Suzuki S, Satoh N, Ohtomo T, Takada T, Marusaki S, Iimura O . Study on uric acid metabolism in patients with primary aldosteronism. Nihon Naibunpi Gakkai Zasshi 1992; 68: 51–61.
Krzesinski P, Stanczyk A, Piotrowicz K, Gielerak G, Uzieblo-Zyczkowska B, Skrobowski A . Abdominal obesity and hypertension: a double burden to the heart. Hypertens Res 2016; 39: 349–355.
Goodfriend TL, Egan BM, Kelley DE . Plasma aldosterone, plasma lipoproteins, obesity and insulin resistance in humans. Prostaglandins Leukot Essent Fatty Acids 1999; 60: 401–405.
Allison MA, Jenny NS, McClelland RL, Cushman M, Rifkin D . The associations of adipokines with selected markers of the renin-angiotensinogen-aldosterone system: the multi-ethnic study of atherosclerosis. J Hum Hypertens 2015; 29: 127–133.
Kargi AY, Iacobellis G . Adipose tissue and adrenal glands: novel pathophysiological mechanisms and clinical applications. Int J Endocrinol 2014; 2014: 614074.
Csabi G, Molnar D, Hartmann G . Urinary sodium excretion: association with hyperinsulinaemia, hypertension and sympathetic nervous system activity in obese and control children. Eur J Pediatr 1996; 155: 895–897.
Monticone S, Satoh F, Viola A, Fischer E, Vonend O, Bernini G, Lucatello B, Quinkler M, Ronconi V, Morimoto R, Kudo M, Degenhart C, Gao X, Carrara D, Willenberg HS, Rossato D, Mengozzi G, Riester A, Paci E, Iwakura Y, Burrello J, Maccario M, Giacchetti G, Veglio F, Ito S, Reincke M, Mulatero P . Aldosterone suppression on contralateral adrenal during adrenal vein sampling does not predict blood pressure response after adrenalectomy. J Clin Endocrinol Metabol 2014; 99: 4158–4166.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Bokuda, K., Yatabe, M., Mizuguchi, Y. et al. Body mass index and contralateral ratio predict outcome following unilateral adrenalectomy in primary aldosteronism. Hypertens Res 40, 988–993 (2017). https://doi.org/10.1038/hr.2017.78
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/hr.2017.78
This article is cited by
-
The Impact of Obesity on the Resolution of Hypertension Following Adrenalectomy for Primary Hyperaldosteronism
World Journal of Surgery (2023)
-
Cosyntropin stimulation in adrenal vein sampling improves the judgment of successful adrenal vein catheterization and outcome prediction for primary aldosteronism
Hypertension Research (2020)
-
Efficient screening of patients with aldosterone-producing adenoma using the ACTH stimulation test
Hypertension Research (2019)
-
Comment on “Body mass index and contralateral ratio predict outcome following unilateral adrenalectomy in primary aldosteronism”
Hypertension Research (2018)