Abstract
To test the hypothesis that plasma glucose (PG) levels is associated with the incidence of hypertension (HT) in nondiabetic and non-hypertensive first-degree relatives (FDR) of people with type 2 diabetes (T2D). A total of 1089 FDR without diabetes and/or HT of consecutive patients with T2D 30–70 years old were examined and followed for a mean (s.d.) of 6.9 (1.7) years for HT incidence. At baseline and through follow-up, participants underwent a standard 75 gm 2-h oral glucose tolerance test. HT was defined according to the criteria of the Seventh Report of Joint National Committee. We used Cox proportional hazard models to estimate hazard ratio for incident HT and plotted a receiver operating characteristic curve to assess discrimination. The PG levels at baseline were associated with incidence of HT, independently of age, gender, obesity and high cholesterol, high-density lipoprotein cholesterol, low-density lipoprotein cholesterol, triglycerides, education and systolic blood pressure. Those with impaired glucose tolerance were 54% (hazard ratio 1.54; 95% confidence interval (CI) 1.33, 1.77) more likely to develop HT than those with normal glucose tolerance. Those with impaired fasting glucose were also 23% (hazard ratio 1.23; 95% CI 1.01, 1.50) more likely to develop HT. High PG levels were consistently associated with incident HT.
Similar content being viewed by others
Introduction
Type 2 diabetes (T2D) and hypertension (HT) are common causes of morbidity and often coexist, and both are risk factors for cardiovascular disease and might share common genetic and environmental risk factors.1 The relationship between higher levels of glucose and HT is reported independent of established HT risk factors in diabetic and nondiabetic individuals.2, 3, 4, 5, 6, 7, 8, 9, 10, 11, 12, 13, 14, 15 However, the nature of this association is not well understood. Particularly, the impact of family history of T2D or genetic predisposition to T2D on incident of HT remains obscure.16 Uncertainty also exists about the relationship between impaired glucose metabolism and HT incidence. Some prospective studies have examined the risk of HT in people with impaired glucose metabolism;5, 6, 7, 8, 9, 12, 13, 14 the risk of HT appeared to be increased in some4, 5, 6, 13, 14 but not all studies.7, 9, 12, 15 In some of these studies, the association between impaired glucose metabolism and HT attenuate after adjustment for obesity.17, 18
Recently, it has been shown in the general population that parental history of diabetes predisposes to the development of incident HT, independently of conventional risk factors.14 In the majority of the studies which assessed the relation between glucose levels and the risk of HT, the presence of family history of T2D was not mentioned or analyzed.
To our knowledge, the association between glucose metabolism and the risk of HT has not been previously reported in first-degree relatives (FDR) of patients with T2D. Therefore, the objective of this study was to investigate the relationship between plasma glucose (PG) levels and the incidence of HT in nondiabetic and non-hypertensive FDR of people with T2D.
Methods
Data collection
This study was conducted within the framework of the Isfahan Diabetes Prevention Study, an ongoing cohort in central Iran to assess the various potential risk factors for diabetes in subjects with family history of T2D (one of the main risk factors for T2D). The recruitment methods and examination procedures of the Isfahan Diabetes Prevention Study have been described before.19 Our study sample at baseline comprised 3235 (831 men and 2404 women) FDR of consecutive patients with T2D. All patients were attendees at clinics at Isfahan Endocrine and Metabolism Research Center, which is affiliated to Isfahan University of Medical Sciences, Iran. The study was conducted between the years 2003 and 2005. All participants were from Isfahan city and adjoining areas. They completed laboratory tests including a standard 75 g 2-h oral glucose tolerance test, standardized blood pressure (BP), a questionnaire on their health status and on various potential risk factors for diabetes. Participants received follow-up tests according to Standard of Medical Care in Diabetes20 to update information on demographic, anthropometric, lifestyle factors and on newly diagnosed pre-diabetes, diabetes and HT. Accordingly, if oral glucose tolerance test was normal at baseline, repeat testing was carried out at least at 3-year intervals. Otherwise, repeat testing was usually carried out annually. Tenets of the current version of the Declaration of Helsinki were followed, institutional ethical committee approval was granted and an informed consent form was signed by each participant.
Follow-up and ascertainment of HT
Participants with T2D and HT were excluded in this cohort study. Participants with T2D were excluded because there is controversy whether the diagnosis of HT convey additional meaning in individuals with T2D who should already be aggressively treated because of high cardiovascular risk. Among 3235 persons who participated at baseline, 1112 subjects were excluded because of diagnosis of type 1 diabetes, T2D or HT at baseline and 1034 did not attend any follow-up examination, leaving 1089 participants with a mean age 42.0 (6.4) (range 30–70) years for this analysis, all of whom had at least one subsequent review during a mean (s.d.) follow-up period of 6.9 (1.7) (range 2–9) years. Attendees at the follow-up visit did not differ significantly from non-attendees regarding most baseline characteristics: age, height, weight, body mass index, waist circumference (WC), hip circumference, waist-to-hip ratio and levels of hemoglobin A1c (HbA1c), fasting plasma glucose (FPG), low-density lipoprotein cholesterol (LDLC), high-density lipoprotein cholesterol (HDLC), total cholesterol, triglyceride, systolic and diastolic BP and obesity. However, non-attendees had slightly lower PG at 30 min (137.3 mg dl−1 vs. 143.8 mg dl−1, P<0.001), 60 min (138.2 mg dl−1 vs. 148.5 mg dl−1, P<0.001) and 120 min. (109.9 mg dl−1 vs. 120.4 mg dl−1, P<0.001).
Procedures
Information on age, gender, body size, HbA1c, cholesterol, LDLC, HDLC, triglycerides and BP, family and personal medical history was collected at baseline and through follow-ups. The same methodology was used for baseline and follow-up studies. The participants included siblings and children of patients with T2D. Participants reported to clinics in the morning after an overnight fast. They were asked to abstain from vigorous exercise in the evening and in the morning of their visit. Smokers were encouraged to abstain from smoking in the morning of the investigations. First, on arrival at the clinic the information provided by the participants in the questionnaire on family history was verified. Then, with the subjects in light clothing and without shoes, height, weight, WC and hip circumference were measured using standard apparatus. Weight was measured to the nearest 0.1 kg on a calibrated beam scale. Height, WC and hip circumference were measured to the nearest 0.5 cm with a measuring tape. The waist was measured midway between the lower rib margin and the iliac-crest at the end of gentle expiration in the standing position. Hip circumference was measured over the greater trochanters directly over the underwear. BMI was calculated as the weight in kg divided by square of the height in meters. Resting BP was measured at each examination by physician after the participants had been seated for 10 min with a mercury column sphygmomanometer and appropriately sized cuffs, using standard techniques. The systolic BP and diastolic BP were recorded at the first appearance (phase I) and the disappearance (phase V) of Korotkoff sounds. FPG was measured with the glucose oxidase method. Participants with FPG ⩾200 mg dl−1 or pharmacological treatment were considered as persons with T2D. If FPG was ⩾126 mg dl−1 and <200 mg dl−1, a second FPG was measured on another day. If the second FPG was also ⩾126 mg dl−1, participants were considered as persons with T2D. Those with FPG <126 mg dl−1 underwent a standard oral glucose tolerance test (75 g glucose 2 h) at baseline and the follow-up visits. Venous blood was sampled 0, 30, 60 and 120 min after oral glucose administration. Plasma samples were centrifuged and analyzed the same day.
HbA1c (measured by ion-exchange chromatography), total cholesterol, triglycerides, HDLC, LDLC were recorded. The LDLC levels were calculated with the Friedewald Equation21 provided total triglycerides did not exceed 400 mg dl−1. All blood sampling procedures were performed in the central laboratory of the Isfahan Endocrine and Metabolism Research Center using enzyme-linked method.
To convert the values for triglycerides to millimoles per liter, multiply by 0.0113; HDLC, LDLC and total cholesterol to millimoles per liter, multiply by 0.0259; and glucose to millimoles per liter, multiply by 0.0555.
Definitions
Cases of HT were identified according to the criteria of the Seventh Report of Joint National Committee on the Prevention, Detection, Evaluation and Treatment of High Blood Pressure.22 Normal BP was defined as not being on antihypertensive medication and having a systolic BP <120 mm Hg and/or diastolic BP <80 mm Hg. Pre-hypertension was defined as not being on antihypertensive medication and having a systolic BP 120–139 mm Hg and/or diastolic BP 80–89 mm Hg. HT was defined as systolic BP ⩾140 mm Hg and/or diastolic BP ⩾90 mm Hg and/or the current use of antihypertensive medications. Impaired glucose tolerance (IGT) was defined as FPG <126 mg/dl, but the 2-h PG concentration ⩾140 and <200 mg dl−1. If the FPG was in the range of 100–126 mg dl−1 and the 2-h PG was <140 mg dl−1, it was considered as impaired fasting glucose (IFG), whereas if the FPG was below 100 mg dl−1 and the 2-h PG <140 mg dl−1, it was considered a sign of normal glucose tolerance (NGT).23
Determination of HT incidence
Incidence was expressed as the number of cases of HT per 100 person-years of follow-up beginning on the date of completion of the baseline examination in 2003–2005 and continuing until the diagnosis of HT, the date of the last completed follow-up, death or end of follow-up on 31 September 2011, whichever came first.
Analysis
Statistical methods included the Student's t-test, the χ2-test and Cox proportional hazards models. Univariate and multivariate Cox’s proportional hazards models were fitted to identify predictors of new-onset HT using the SPSS version 18 for Windows (SPSS, Chicago, IL, USA). The ability of FPG, 30, 60 and 120 min PG to predict incident HT were examined with receiver operating characteristic (ROC) curves and their respective areas under the curve, in which sensitivity was plotted as a function of 1-specificity. The area under the ROC curve is a global summary statistic of the discriminative value of a model, describing the probability that the FPG, 30, 60 and 120 min PG is higher in an individual developing HT than in an individual not developing HT. Areas under the ROC curves were compared by the algorithm developed by DeLong et al.24 All tests for statistical significance were two-tailed, and all were carried out assuming a type I error probability of <0.05.
Results
Participants with T2D and/or HT were excluded in this cohort study. The baseline characteristics of the 1112 (34.4%) participants who had T2D and/or HT at baseline and 1089 (33.7%) without T2D and/or HT are shown in Table 1. As expected, those who had T2D and/or HT were older and had higher age-adjusted mean weight, BMI, WC, hip circumference, waist-to-hip ratio, FPG, and PG at 30, 60 and 120 min, higher HbA1c, triglyceride, cholesterol and LDLC, and a higher proportion of obesity, abdominal obesity, but lower proportion of NGT, IFG and IGT at baseline, as compared with those without T2D and/or HT.
The baseline characteristics of the 567 (52.1%) participants with NGT, 134 (12.3%) with IFG and 388 (35.6%) with IGT are shown in Table 2. In comparison of variables at baseline, all variables were more likely to increase and follow-up duration was more likely to decrease across all three subject groups. The mean (s.d.) age was 42.4 (7.2) years for those with IFG, 43.3 (6.6.) years for those with IGT and 41.6 (6.0) years for those with NGT.
Prevalent HT
Of the 3235 FDR of people with T2D (831 men and 2404 women), 819 had HT (244 men and 575 women) and 1047 had pre-hypertension (284 men and 763 women). Overall prevalence of HT and pre-hypertension was 25.3% (95% confidence interval (CI): 23.8, 26.8) and 32.4% (95% CI 30.8, 34.0), respectively. Prevalence of HT was higher in men (29.4%; 95% CI: 26.3, 32.5) than women (23.9%; 95% CI: 22.2, 25.6) and 34.2% (95% CI: 31.0, 37.4) of men and 31.7% (95% CI: 29.9, 33.6) of women were pre-hypertensive. As expected, in both gender there was a statistically increasing prevalence of HT with increasing age.
Among the FDR of patients with T2D, 9.1% had diabetes, 21.1% had IGT, 18.2% had IFG, 3.8% had both T2D and HT, and 3.1% had both T2D and pre-hypertension. Of people with HT, 15.1% had diabetes, 23.0% had IGT and 18.8% had IFG.
The prevalence of HT was 26.2% (95% CI 22.6, 29.7) for participants with IFG, 27.5% (95% CI 24.2, 30.9) for participants with IGT, 42.3% (95% CI 36.7, 48.0) for participants with T2D and 21.1% (95% CI 33.3, 40.1) for the NGT.
Glucose and incident HT
During 7461 (1673 men and 5,788 women) person-years of follow-up, 214 (19.6%) (44 men and 170 women) incident cases of HT were observed. Within this cohort without HT and/or T2D at baseline, the overall incidence of subsequent HT was 2.9 (95% CI: 2.5, 3.2) events per 100 person-years. Incidence rates were almost similar in women (2.9, 95% CI: 2.5, 3.4 per 100 person-years) and men (2.6, 95% CI: 1.9, 3.5).
The incidence of HT was 2.9 per 100 person-years (95% CI 2.1, 4.0) for participants with IFG, 3.1 per 100 person-years (95% CI 2.4, 3.9) for participants with IGT and 2.6 per 100 person-years (95% CI 2.1, 3.1) for the NGT. Compared with participants in the NGT, the risk of HT was 27% higher in those with IFG (hazard ratio 1.27; 95% CI: 1.05, 1.53) and 59% higher in those with IGT (hazard ratio1.59; 95% CI: 1.40, 1.82) in age-adjusted model. Controlling for age, gender, cholesterol, HDLC, LDLC, HbA1c, triglycerides, education, BMI, WC and systolic BP slightly attenuated association for incident HT compared with the age-adjusted model but the associations remained statistically significant (Table 3).
When we considered FPG, 30 min, 60 min and 120 min PG as continuous independent variables in fully adjusted model, only FPG was significant risk factors for incident HT (Table 4).
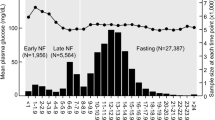
The ROC curves for the incidence of HT for FPG, 30, 60 and 120 min PG are shown in Figure 1. The areas under the ROC curves were 0.585 (95% CI: 0.559, 0.611) for FPG, 0.610 (95% CI: 0.584, 0.636) for 30 min PG, 0.630 (95% CI: 0.605, 0.656) for 1-h PG and 0.583 (95% CI: 0.557, 0.610) for 2-h PG. All parameters were significant predictors for future risk of HT (P<0.001). The areas were almost similar for FPG, 30 min PG, 1-h PG and 2-h PG.
Receiver operating characteristic (ROC) curves for fasting plasma glucose (FPG), 30, 60 and 120 min plasma glucose (PG) to predict incident hypertension in first-degree relatives of patients with type 2 diabetes. The estimates of the area under the ROC curves and their 95% confidence intervals are shown. Areas under the ROC curves were compared by the algorithm developed by DeLong et al.24
Discussion
The present study showed that elevated PG concentration is a strong predictor of incident HT independent of several known or suspected risk factors for HT, in a large cohort of FDR of patients with T2D in Iran. Among participant without T2D and/or HT at baseline, IGT and IFG were associated with 54 and 23% higher risk of incident HT after full adjustment. The association between FPG and HT was relatively similar to that observed with 30, 60 and 120 min PG levels. This observation was confirmed by the results from ROC curve analysis. These associations suggest that in participants without T2D, higher glucose concentration may contribute to the development of HT. Our data are in agreement with the previous observation that FPG,4, 5, 6, 12, 25 elevated 2-h postload glucose concentration,4, 7, 8, 12, 25 IGT8, 25, 26 and IFG4, 5, 6, 25 are associated with incident HT. In the Paris Prospective Study of 4149 men followed for 3 years, Fagot-Campagna et al.5 showed that FPG was a strong predictor of HT after adjustment for obesity. In contrast to this study, Vaccaro et al.15 showed a strong association between IGT and BP at baseline, but this association was not found in a longitudinal analysis. Incomplete exclusion of participants with HT at baseline, incomplete control for confounders or limited number of study population may explain the inconclusive associations. In the San Antonio Heart Study, Haffner et al.7 reported that IGT was not associated with risk of HT after adjustment for age, obesity, body fat distribution, and fasting insulin levels and T2D was associated with risk of HT only among men. The association between impaired glucose metabolism and HT is also supported by two clinical trials in T1D.9, 10 In a Japanese Study, Miyai et al.27 reported that the z-score of mean arterial pressure was significantly higher in subjects with hyperglycemia than in those without metabolic syndrome component.
The mechanisms underlying the increased risk of HT in individuals with higher glucose level are not clear. Insulin resistance and hyperinsulinemia have been thought to be common factors underlying the link between T2D, obesity and HT.17, 18 Persons with impaired glucose metabolism may have a reduced insulin secretion rate or increase in glucose levels over time. Hemodynamic actions of insulin have been suggested28 and a small BP-lowering effect of insulin has been described in nondiabetic individuals.29 These findings suggest that reduced activation of the insulin pathway through diminished insulin secretion capacity, particularly in the presence of insulin resistance, might lead to endothelial dysfunction that favors the development of HT. In parallel, subtle defects in beta cell function might facilitate the development of HT through possible repeated postprandial elevations in glucose levels over time. Glycemic variability might contribute to increase BP through chronic induction of inflammation and enhanced oxidative stress.30, 31 Oxidative stress has been shown to correlate with both glycemic fluctuations and BP variability, suggesting possible alternative mechanisms to explain the increased incidence of HT in relationship to subtle defect in beta cell function.32 Hyperglycemia may also damage the arterial wall through deposition of advanced glycation end product, generation of reactive oxygen species and activation of protein kinase C.33, 34 Reduced arterial elasticity is one result of long-term exposure of the vascular wall to elevated glucose level. Reduced elasticity leads to HT by increasing peripheral vascular resistance.35
It has been hypothesized that the link between T2D and HT is largely because of underlying obesity.17, 18 Indeed, associations of diabetes, glucose and insulin with prevalent and incident HT were attenuated by adjustment for adiposity. However, substantial associations persisted in our data after adjustment for both BMI and WC. Although residual confounding could still exist, it is likely that factors other than obesity also contribute to the glucose-HT link, as discussed above.
The strengths of this study include the use of a sample consisting of both men and women, performance of standard oral glucose tolerance test and information on potential determinants of HT. All participants were examined at one site and BP was measured by the physician, and laboratory samples were measured using the same method both at baseline and follow-ups. We excluded patients with T2D and/or HT at study entry. At follow-up, non-attendees in the entire population did not differ from attendees according to major risk factors for progression to HT, although a difference too small to explain the high progression rate to HT in our study was seen in the mean levels of PG. Our database is one of the few that followed FDR of patients with T2D, thereby enabling us to simultaneously control the genetic factors that may predict HT.
Although this study has much strength, its limitations warrant highlighting. Our study was limited to a cohort of individuals who are at increased risk of developing T2D and HT, because they had a FDR with the patients with T2D; thus, the selection bias may lead to an overestimation of associations. In term of our definition of incidence IGT and IFG, some selection bias may be present, as participants who attend for screening may have been more likely to be tested and consequently diagnosed as having IGT or IFG. Thus, participants with IGT or IFG who had lower risk may have been missed through lack of testing. We could not include several possible confounding variables that are known HT risk factors, such as plasma insulin, alcohol and salt consumption, physical activity and socioeconomic status. These variables could be relevant for explaining the relationship between PG levels and incidence of HT.
In conclusion, these data provide further evidence that PG level is a robust predictor of incident HT, independent of known risk factors for HT, in high-risk individuals. These findings could help to identify those who are at increased risk of developing HT and who should be encouraged to adopt lifestyle modifications.
References
Ferrannini E, Cushman WC . Diabetes and hypertension: the bad companions. Lancet 2012; 380: 601–610.
Bower JK, Appel LJ, Matsushiba K, Young JH, Alonso A, Brancati FL, Selvin E . Glycated hemoglobin and risk of hypertension in the atherosclerosis risk in communities study. Diabetes Care 2012; 35: 1031–1037.
Britton KA, Pradhan AD, Gaziano JM, Manson JE, Ridker PM, Buring JE, Sesso HD . Hemoglobin A1c, body mass index, and the risk of hypertension in women. Am J Hypertens 2011; 24: 328–334.
Bjørnholt JV, Erikssen G, Kjeldsen SE, Bodegard J, Thaulow E, Erikssen J . Fasting blood glucose is independently associated with resting and exercise blood pressures and development of elevated blood pressure. J Hypertens 2003; 5: 1383–1389.
Fagot-Campagna A, Balkau B, Simon D, Ducimetiere P, Eschwege E . Is insulin an independent risk factor for hypertension? The Paris Prospective Study. Int J Epidemiol 1997; 5: 542–550.
Suematsu C, Hayashi T, Fujii S, Endo G, Tsumura K, Okada K, Morii H . Impaired fasting glucose and the risk of hypertension in Japanese men between the 1980s and the 1990s. Diabetes Care 1999; 5: 228–232.
Haffner SM, Valdez R, Morales PA, Mitchell BD, Hazuda HP, Stern MP . Greater effect of glycemia on incidence of hypertension in women than in men. Diabetes Care 1992; 15: 1277–1284.
Boyko EJ, Barr EL, Zimmet PZ, Shaw JE . Two-hour glucose predicts the development of hypertension over 5 years: the AusDiab Study. J Hum Hypertens 2008; 22: 168–176.
Wang W, Lee ET, Fabsitz RR, Devereux R, Best L, Welty TK, Howard BV . A longitudinal study of hypertension risk factors and their relation to cardiovascular disease: the Strong Heart Study. Hypertension 2006; 4: 403–409.
de Boer IH, Kestenbaum B, Rue TC, Steffes MW, Cleary PA, Molitch ME, Lachin JM, Weiss NS, Brunzell JD, Diabetes Control and Complications Trial (DCCT)/Epidemiology of Diabetes Interventions and Complications (EDIC) Study Research Group. Insulin therapy, hyperglycemia, and hypertension in type 1 diabetes mellitus. Arch Intern Med 2008; 168: 1867–1873.
Chiasson JL, Josse RG, Gomis R, Hanefeld M, Karasik A, Laakso M . Acarbose treatment and the risk of cardiovascular disease and hypertension in patients with impaired glucose tolerance: the STOP-NIDDM trial. JAMA 2003; 290: 486–494.
Levin G, Kestenbaum B, Ida Chen YD, Jacobs DR Jr, Psaty BM, Rotter JI, Siscovick DS, de Boer IH . Glucose, insulin, and incident hypertension in the multi-ethnic study of atherosclerosis. Am J Epidemiol 2010; 5: 1144–1154.
Morio M, Inoue M, Inoue K, Akimoto K . Impaired fasting glucose as an independent risk factor for hypertension among healthy middle-aged Japanese subjects with optimal blood pressure: the Yuport Medical Checkup Centre retrospective cohort study. Diabetol Metab Syndr 2013; 5: 81.
Bonnet F, Roussel R, Natali A, Cauchi S, Petrie J, Laville M, Yengo L, Froguel P, Lange C, Lantieri O, Marre M, Balkau B, Ferrannini E, DESIR and RISC Study Groups. Parental history of type 2 diabetes, TCF7L2 variant and lower insulin secretion are associated with incident hypertension. Data from the DESIR and RISC cohorts. Diabetologia 2013; 56: 2414–2423.
Vaccaro O, Imperatore G, Iovino V, Iovine C, Rivellese AA, Riccardi G . Does impaired glucose tolerance predict hypertension? A prospective analysis. Diabetologia 1996; 39: 70–76.
Gloyn AL, Braun M, Rorsman P . Type 2 diabetes susceptibility gene TCF7L2 and its role in beta cell function. Diabetes 2009; 58: 800–802.
Cheung BM, Li C . Diabetes and hypertension: is there a common metabolic pathway? Curr Atheroscler Rep 2012; 14: 160–166.
Cheung BM . The hypertension-diabetes continuum. J Cardiovasc Pharmacol 2010; 55: 333–339.
Amini M, Janghorbani M . Diabetes and impaired glucose regulation in first degree relatives of patients with type 2 diabetes in Isfahan, Iran: Prevalence and risk factors. Rev Diabet Stud 2007; 4: 169–176.
Executive summary: Standard of Medical Care in Diabetes-2013. Diabetes Care 2013; 36: S4–S10.
Friedewald WT, Levy RI, Fredrickson DS . Estimation of the concentration of low-density lipoprotein cholesterol in plasma, without use of the preparative ultracentrifuge. Clin Chem 1972; 18: 499–502.
Chobanian AV, Bakris GL, Black HR, Cushman WC, Green LA, Izzo JL Jr, Jones DW, Materson BJ, Oparil S, Wright JT Jr, Roccella EJ . The Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure: the JNC 7 report. JAMA 2003; 289: 2560–2572.
Expert Committee on the Diagnosis and Classification of Diabetes Mellitus. Report of the expert committee on the diagnosis and classification of diabetes mellitus. Diabetes Care 2003; 26 (suppl 1): S5–20.
DeLong ER, DeLong DM, Clarke-Pearson DL . Comparing the areas under two or more correlated receiver operating characteristic curves: a nonparametric approach. Biometrics 1988; 44: 837–845.
Sun N, Wang H, Sun Y, Chen X, Wang H, Zhao L, Wang J, Zhu Z . Detecting diabetic risk using the oral glucose tolerance test in Chinese patients with hypertension: a cross-sectional study. Hypertens Res 2014; 37: 82–87.
Cheung BM, Wat NM, Tso AW, Tam S, Thomas GN, Leung GM, Tse HF, Woo J, Janus ED, Lau CP, Lam TH, Lam KS . Association between raised blood pressure and dysglycemia in Hong Kong Chinese. Diabetes Care 2008; 31: 1889–1891.
Miyai N, Shiozaki M, Yabu M, Utsumi M, Morioka I, Miyashita K, Arita M . Increased mean arterial pressure response to dynamic exercise in normotensive subjects with multiple metabolic risk factors. Hypertens Res 2013; 36: 534–539.
Baron AD . Hemodynamic actions of insulin. Am J Physiol 1994; 267: E187–E202.
Heise T, Magnusson K, Heinemann L, Sawicki PT . Insulin resistance and the effect of insulin on blood pressure in essential hypertension. Hypertension 1998; 32: 243–248.
Cherney DZ, Scholey JW, Sochett E, Bradley TJ, Reich HN . The acute effect of clamped hyperglycemia on the urinary excretion of inflammatory ytokines/ chemokines in uncomplicated type 1 diabetes: a pilot study. Diabetes Care 2011; 34: 177–180.
Monnier L, Mas E, Ginet C, Michel F, Villon L, Cristol JP, Colette C . Activation of oxidative stress by acute glucose fluctuations compared with sustained chronic hyperglycemia in patients with type 2 diabetes. JAMA 2006; 295: 1681–1687.
Di Flaviani A, Picconi F, Di Stefano P, Giordani I, Malandrucco I, Maggio P, Palazzo P, Sgreccia F, Peraldo C, Farina F, Frajese G, Frontoni S . Impact of glycemic and blood pressure variability on surrogate measures of cardiovascular outcomes in type 2 diabetic patients. Diabetes Care 2011; 34: 1605–1609.
Brownlee M . The pathobiology of diabetic complications: a unifying mechanism. Diabetes 2005; 54: 1615–1625.
Ceriello A . Controlling oxidative stress as a novel molecular approach to protecting the vascular wall in diabetes. Curr Opin Lipidol 2006; 17: 510–518.
McVeigh GE, Bratteli CW, Morgan DJ, Alinder CM, Glasser SP, Finkelstein SM, Cohn JN . Age-related abnormalities in arterial compliance identified by pressure pulse contour analysis: aging and arterial compliance. Hypertension 1999; 33: 1392–1398.
Acknowledgements
We are grateful to M Abyar for technical computer assistance. This study could not have been conducted without the contributions of the relatives of patients with type 2 diabetes who consented to participate.
Author Contributions
Janghorbani M conceived and designed the study, analyzed the data and wrote the manuscript, Bonnet F provided the critical revision, Amini M recruited samples and contributed to the discussion and revision of the manuscript and obtained funding for the IDPS. All authors have given final approval of the version to be published.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Janghorbani, M., Bonnet, F. & Amini, M. Glucose and the risk of hypertension in first-degree relatives of patients with type 2 diabetes. Hypertens Res 38, 349–354 (2015). https://doi.org/10.1038/hr.2015.10
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/hr.2015.10
Keywords
This article is cited by
-
A higher TyG index level is more likely to have enhanced incidence of T2DM and HTN comorbidity in elderly Chinese people: a prospective observational study from the reaction study
Diabetology & Metabolic Syndrome (2024)
-
Association of glycemic control with hypertension in patients with diabetes: a population-based longitudinal study
BMC Cardiovascular Disorders (2023)
-
A high triglyceride glucose index is more closely associated with hypertension than lipid or glycemic parameters in elderly individuals: a cross-sectional survey from the Reaction Study
Cardiovascular Diabetology (2020)
-
Association between changes in systolic blood pressure and incident diabetes in a community-based cohort study in Korea
Hypertension Research (2017)
-
Hypertension with diabetes mellitus: significance from an epidemiological perspective for Japanese
Hypertension Research (2017)