Abstract
In Asian populations, a high prevalence of stroke, high salt intake and high salt sensitivity, the effects of which are partly augmented by epidemic obesity, are associated with hypertension. These factors are closely associated with resistant hypertension, especially with the disrupted circadian rhythm of blood pressure (BP), that is, non-dipper and riser patterns. An ambulatory BP profile-based strategy combined with medication and devices (renal denervation and baroreceptor activation therapy) would help to achieve ‘perfect 24-h BP control’, consisting of strict reduction of the 24-h BP level, restoring disrupted circadian BP rhythms and reducing excess BP variability. Such BP control would protect high-risk patients with resistant hypertension against systemic hemodynamic atherothrombotic syndrome (which involves systemic atherothrombotic vascular diseases and target-organ damage, advanced by the composite risks of pulsatile hemodynamic stress from central pressure and blood flow and by thrombometabolic risk factors). Information technology-based home sleep BP pressure monitoring may be useful for assessing the risk during sleep in high-risk patients with resistant hypertension and sleep apnea syndrome.
Similar content being viewed by others

Introduction
High blood pressure (BP) is directly associated with cardiovascular events and mortality in all populations regardless of ethnicity.1 Various classes of antihypertensive drugs are available, and combination therapy using these drugs is recommended in both domestic and international guidelines for hypertension management.2 However, BP control below the target threshold remains insufficient in clinical practice. In addition, recent increases in the aging population, increases in the prevalence of chronic kidney disease and epidemic obesity in Japanese hypertension patients are increasing the prevalence of drug-resistant hypertension.3, 4 Strategies for effective BP control are required for high-risk patients with resistant hypertension, whose BP remains high even when treated with three or more antihypertensive drugs. In recent years, renal denervation has been introduced into the management of resistant hypertension worldwide.5, 6
In Hypertension Research 2013, the editors have initiated a topical series on resistant hypertension, and distinguished researchers will provide up-to-date information on this timely topic from their various viewpoints. As a start, in this mini-review, I have proposed my strategy for the management of resistant hypertension in the era of renal denervation, and have stressed the importance of ‘perfect 24-h BP control’7 in this high-risk hypertension population.
Asian impact of controlling resistant hypertension
In Asia, there are several characteristics of hypertensive populations (Table 1). First, stroke occurs more often than coronary artery disease does in Asian countries compared with Western countries.8, 9 Stroke is more closely associated with BP than coronary artery disease is.10 Second, the slope of the association between BP and stroke is steeper among Asians than among Westerners.10 Third and fourth, Asians are likely to have a genetically high salt sensitivity, and to have a greater salt intake than Westerners.11, 12 Fifth, in response to the introduction of the Western lifestyle in Asia, the prevalence of obesity and the related metabolic syndrome is increasing.13 Obesity and metabolic syndrome are known to increase salt sensitivity.14, 15 In fact, the threshold at which obesity increases BP is lower in Asians than in Westerners, and being overweight or mildly obese may increase BP in Asians with high salt intake and higher salt sensitivity. The impact of a body mass index of 25 in Asians is comparable with a body mass index of 30 in Westerners as a determinant of prehypertension and hypertension.16, 17 Finally, these characteristics are associated with non-dipping of nocturnal BP; a previous review demonstrated a higher prevalence of non-dippers in Asian cohorts than Western cohorts.18
Although the precise prevalence of resistant hypertension in Asian hypertensives remains unclear in Asia, the above characteristics suggest that controlling resistant hypertension is important for the effective prevention of cardiovascular events, particularly stroke, in Asia.
Evaluation using ambulatory BP monitoring
Resistant hypertension is diagnosed when clinical BP remains above 140/90 mm Hg despite the concurrent use of three antihypertensive agents of different classes.19 Ideally, one of the three agents should be a diuretic, and all agents should be prescribed at optimal doses. The standard combination of antihypertensive agents is a long-acting calcium channel blocker (CCB), renin–angiotensin system (RAS) inhibitors (angiotensin-receptor blocker, angiotensin-converting enzyme inhibitor) and diuretics (thiazide, thiazide-like diuretic).
To manage resistant hypertension, secondary hypertension should first be excluded (Figure 1). Particularly, sleep apnea is the most common cause of resistant hypertension.20, 21 Approximately two-thirds of resistant hypertension cases are caused by sleep apnea,21 although the precise percentage of sleep apnea in Asian non-obese patients with resistant hypertension remains unclear.
Second, ambulatory BP monitoring (ABPM) is recommended to separate the patients with resistant hypertension diagnosed by clinical BP into those with ‘white-coat’ resistant hypertension (24-h BP <130/80 mm Hg) and ‘true’ resistant hypertension (24-h BP ⩾130/80 mm Hg). The clinical prognosis of patients with ‘true’ resistant hypertension is much worse than that of patients with ‘white-coat’ resistant hypertension.22
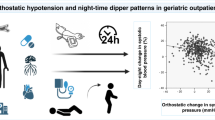
With the aim of achieving ‘perfect 24-h BP control’, which would achieve more effective cardiovascular protection (that is, strict BP control <130/80 mm Hg for 24-h BP), adequate circadian rhythm (dipper type) and the suppression of the exaggerated morning BP surge are two other important components that ABPM could detect.7) Nocturnal BP is more closely associated with a poor cardiovascular prognosis in patients with resistant hypertension than daytime BP is.23 Patients with non-dipper (diminished nocturnal BP fall) and riser (higher nocturnal BP than daytime BP) patterns present advanced target organ damage,24, 25, 26, 27 and exhibit the worst prognosis in terms of future cardiovascular disease and end-stage renal failure,27, 28, 29, 30 which are more common in patients with resistant hypertension than those with better-managed hypertension.31 Finally, exaggerated morning BP surge is also associated with cardiovascular risk independently of 24-h BP levels and nocturnal dipping status.32, 33
Systemic hemodynamic atherothrombotic syndrome
The above BP variabilities and vascular disease of both the large and small arteries are closely related to each other and create the vicious cycle that advances systemic hemodynamic atherothrombotic syndrome (SHATS).33 SHATS is a syndrome of systemic atherothrombotic vascular diseases and target organ damage advanced by the composite risks of pulsatile hemodynamic stress from central pressure and blood flow in relation to thrombometabolic risk factors. Both the management of cardiovascular risk factors and the reduction of pulsatile hemodynamic stress by restoring disrupted circadian BP rhythms and reducing excess BP variability would protect against the development of SHATS in high-risk patients with resistant hypertension.
Proposal of an ambulatory BP-based strategy
For patients with ‘true’ resistant hypertension, we should reconsider lifestyle and medication changes. Particularly, strict salt restriction would be very effective for Asian patients with resistant hypertension,34 because even mild obesity and high salt intake are the important risk factors for resistant hypertension in Asians with high salt sensitivity. In one study, salt restriction changed patients’ nocturnal BP dipping status from non-dipper to dipper.35
The ambulatory BP profile of ‘true’ resistant hypertension may separate the arterial stiffness type characterized by increased BP variability, such as excess morning BP surges, from the volume retention type characterized by non-dipper or riser nocturnal BP patterns (Figure 1), as previously proposed in guidelines for RAS inhibitor-based combination therapy.36
Arterial stiffness type
For the arterial stiffness type of resistant hypertension, increased doses of the long-acting CCB that the patient is already taking is preferable because of the three classes of antihypertensive drugs (CCBs, RAS inhibitors and diuretics), CCBs are the most effective for reducing BP variability.37 This ability to reduce BP variability is stronger at higher doses and remains significant even when used in combination therapy.38 The higher the baseline BP, the greater the BP-lowering effect to be expected from the CCB.39, 40 The maximum dose of long-acting CCB minimizes the exaggerated morning BP surge, because the CCBs can decrease the highest morning BP more extensively than other drugs without causing any reduction in the lowest nocturnal BP.33, 39
Volume retention type
For the volume retention type, aldosterone-receptor blockers are preferable among the three classes of antihypertensives (CCB, RAS inhibitors and diuretic). The non-dipping of nocturnal BP is closely associated with increased circulating volume retention. Diuretics are the most effective class of antihypertensives for changing non-dipping nocturnal BP to a dipping pattern.41 This property of diuretics persisted when used in combination with RAS inhibitors.42 However, increasing doses of thiazide may worsen glucose metabolism. Particularly in Asians, small doses of diuretics may be sufficient to reduce nocturnal BP when combined with RAS inhibitors.43 Aldosterone-receptor blockers reduce circulating volume without impairing glucose metabolism. Low-dose spironolactone clearly reduced BP in subjects with resistant hypertension.44 In our previous study, eplerenone reduced predominantly nocturnal BP compared with daytime BP in uncontrolled hypertensive patients already being treated with RAS inhibitors.45 Angiotensin receptor neprilysin inhibitors may also be effective in non-dippers with ‘true’ resistant hypertension because increased atrial and brain natriuretic peptides may reduce circulating volume. A recent clinical trial of angiotensin receptor neprilysin inhibitor demonstrated effective ambulatory BP lowering, including nocturnal BP reduction, in hypertensive patients46 and effective reduction of N-terminal brain natriuretic peptide, a biomarker of cardiac overload in heart failure patients with preserved left ventricular ejection fraction.47
Circadian medication
When morning BP surges or non-dipper/riser patterns persist, another option is bedtime dosing of antihypertensive drugs, particularly alpha-blockers48 or vasodilating beta-blockers, such as carvedilol49 and nebivolol (unavailable in Japan). This circadian medication would be useful predominantly for reducing nocturnal and morning BP, for shifting non-dipper/riser patterns to dipper patterns and for suppressing the exaggerated morning BP surge. Bedtime administration of angiotensin-receptor blockers improves microalbuminuria more effectively than morning dosing does.50 Controlling nocturnal BP reduction is essentially more important than controlling daytime BP is.51
The above described ambulatory BP-based approach would be effective for achieving ‘perfect 24-h BP control’ with 24-h BP<130/80 mm Hg, dipper-type circadian rhythm, and an adequate morning BP surge.
When BP control is not complete, other classes of drugs, such as central sympatholytics and direct renin inhibitors, could be added.
Renal denervation in Japan
For patients with resistant hypertension being treated with the above described ambulatory BP-based medication strategy, two new device approaches have recently been introduced into clinical practice. One is catheter-based renal sympathetic denervation,5, 6) and the other is the electrical stimulation of the carotid baroreceptor (baroreceptor activation therapy). The renal sympathetic nerves, both efferent and afferent, are located in the adventitia of the renal arteries. The catheter-based renal sympathetic denervation system is designed to deliver low-level radio frequency energy through the wall of the renal artery to achieve renal denervation.
A randomized clinical trial of renal denervation with a control arm, HTN Japan, was initiated to evaluate the efficacy and safety of catheter-based renal denervation in Japanese patients with resistant hypertension in August 2012, and Jichi Medical University conducted the first two cases in Japan with no complications. Inclusion criteria for this trial are (1) high-clinical systolic BP ⩾ 160 mm Hg and high 24-h systolic BP ⩾ 135 mm Hg, even when treated with three or more different classes of antihypertensive drugs, including diuretics; (2) a maintained estimated glomerular filtration rate >45; and (3) no structural abnormality in the renal artery. These inclusion and exclusion criteria are almost the same as those of the Symplicity HTN-1 and Symplicity HTN2 trials,5, 6 both of which demonstrated that renal denervation reduces clinical BP by 30 mm Hg systolic, self-measured home BP by 20 mm Hg and 24-h ambulatory BP by 10 mm Hg, and changes non-dippers to dippers. Previous studies have also demonstrated that catheter-based renal denervation improves insulin resistance (homeostasis model assessment, HOMA index),52 renal resistive index and microalbuminuria values without reducing the glomerular filtration rate,53 and it improves hypertensive heart disease (left ventricular hypertrophy and diastolic dysfunction).54 These target organ protection effects are predominantly caused by the extensive BP lowering effect, but may partly result from a direct sympatholytic effect on the target organ.
Hypothesis of ‘Perfect 24-h BP Control’ by renal denervation
As the mechanism of renal denervation, efferent denervation reduces renal catecholamine production and beta-1 adrenergic renin production. These changes increase renal blood flow and reduce circulating volume, thus explaining the shift from non-dipping to dipping of nocturnal BP in patients with resistant hypertension. In addition, afferent denervation decreases central sympathetic activity in response to increased baroreceptor sensitivity, thus potentially explaining the reduced variability in BP, including the morning BP surge and the 24-h BP reduction, as resulting from decreases in peripheral resistance and cardiac workload. Thus, I hypothesize that renal denervation could achieve ‘perfect 24-h ambulatory BP control’, consisting of a strict reduction in the 24-h BP level, a dipper pattern of nocturnal BP and an adequate morning BP surge (Figure 2).
Cutting-edge sleep BP monitoring at home for resistant hypertension
As mentioned above, sleep BP is more important than awake BP in patients with resistant hypertension. In addition, the most frequent cause of resistant hypertension is sleep apnea syndrome, for which ambulatory BP is likely to exhibit a non-dipper/riser pattern of nocturnal hypertension particularly, with increased sleep BP variability.20 Thus, it is very important to detect sleep apnea syndrome and monitor sleep BP in patients with resistant hypertension.
ABPM has historically been the gold standard for measuring BP during sleep. However, self-measured home BP monitoring could be used to evaluate sleep BP, with results that are comparable with those of ABPM. We have been developing a self-measured home sleep BP monitoring system, as described below.
Basic sleep BP monitoring at home
Recently, working with Omron HealthCare (Kyoto, Japan), we developed a home BP monitoring system with the function of automatic fixed-interval BP measurement during sleep (Medinote, Omron HealthCare). The at-home, self-measured sleep BP using this device (the average of the sleep BPs measured at 0200, 0300 and 0400 hours) was comparable with that measured by ABPM, and we have demonstrated for the first time that at-home, self-measured sleep BP was more closely associated with measures of target organ damage, such as left ventricular mass index and urinary albumin excretion values, than ABPM was.55
The development of Medinote was the first step in detecting basic BP information using at-home, self-measured BP monitoring compared with ABPM, and it extended the scope of previous home BP monitoring that measured BP only once during sleep.56
Trigger sleep BP monitoring
The second advance was the development of trigger sleep BP monitoring (TSP), which was based on the automated fixed interval-measurement technique of Medinote with an added trigger function that initiates BP measurement when oxygen desaturation falls below the variable threshold continuously monitored by pulseoximetry.20, 57 TSP can detect the sleep BP surge found in patients with sleep apnea syndrome. Neither previous home BP monitoring nor ABPM could detect augmented sleep BP or the sleep BP surge specific to each sleep apnea episode.
Figure 3 demonstrates the sleep BPs detected by TSP in the two cases with resistant hypertension and sleep apnea syndrome. Although the patients’ had comparable degrees of sleep apnea syndrome severity (as measured by the apnea hypopnea index), the trigger function of TSP revealed quite different sleep BP surges between these patients.
Different sleep BP surges in two patients with resistant hypertension and sleep apnea syndrome. Dark blue line indicate oxygen saturation (SpO2) measured using pulseoximetry. Pink circle and line indicate BP measured using the hypoxia-triggered method. Red open square and line indicate systolic BP measured at fixed 15 min-intervals. Green circle and line indicate pulse pressure. AHI, apnea hypopnea index.
Information technology-based, at-home trigger sleep BP monitoring
Finally, we have recently developed the Information technology-based, at-home trigger sleep BP monitoring with a 3G web system (ISP) with our colleagues (Toshikazu Shiga, Takahide Tanaka, Mitsuo Kuwabara, Osamu Shirasaki and Yutaka Kobayashi) at Omron HealthCare Inc. (Kyoto, Japan). The ISP system is a cloud computing-based composite management and analysis system for the data sent from the ISP device in the patient’s home. The ISP system can detect repeated and day-to-day variability in sleep BP and the sleep BP surges associated with sleep apnea episodes, the degree of which can be affected by daily environmental changes. Using ISP, we have started the prospective study SPREAD (Sleep pressure and disordered breathing in resistant hypertension and cardiovascular Disease), a registry to evaluate the clinical implications of sleep BP and sleep BP surges in high-risk patients with resistant hypertension, in September 2012.
Conclusion
The ambulatory BP profile-based strategy, in combination with medication and devices for resistant hypertension management, is potentially effective for achieving perfect 24-h BP control, and therefore protecting patients’ cardiovascular and renal systems. ISP may be useful for detecting and managing the risk of SHAT in high-risk patients with resistant hypertension and sleep apnea syndrome.
Change history
05 June 2013
The article has been corrected since Advance Online Publication, and a corrigendum is also printed in this issue.
References
Lewington S, Clarke R, Qizilbash N, Peto R, Collins R, Prospective Studies Collaboration. Age-specific relevance of usual blood pressure to vascular mortality: a meta-analysis of individual data for one million adults in 61 prospective studies. Lancet 2002; 360: 1903–1913.
Ogihara T, Kikuchi K, Matsuoka H, Fujita T, Higaki J, Horiuchi M, Imai Y, Imaizumi T, Ito S, Iwao H, Kario K, Kawano Y, Kim-Mitsuyama S, Kimura G, Matsubara H, Matsuura H, Naruse M, Saito I, Shimada K, Shimamoto K, Suzuki H, Takishita S, Tanahashi N, Tsuchihashi T, Uchiyama M, Ueda S, Ueshima H, Umemura S, Ishimitsu T, Rakugi H., Japanese Society of Hypertension Committee. The Japanese Society of Hypertension Guidelines for the Management of Hypertension (JSH 2009). Hypertens Res 2009; 32: 3–107.
Egan BM, Zhao Y, Axon RN, Brzezinski WA, Ferdinand KC . Uncontrolled and apparent treatment resistant hypertension in the United States, 1988 to 2008. Circulation 2011; 124: 1046–1058.
Daugherty SL, Powers JD, Magid DJ, Tavel HM, Masoudi FA, Margolis KL, O'Connor PJ, Selby JV, Ho PM . Incidence and prognosis of resistant hypertension in hypertensive patients. Circulation 2012; 125: 1635–1642.
Krum H, Schlaich M, Whitbourn R, Sobotka PA, Sadowski J, Bartus K, Kapelak B, Walton A, Sievert H, Thambar S, Abraham WT, Esler M . Catheter-based renal sympathetic denervation for resistant hypertension: a multicentre safety and proof-of-principle cohort study. Lancet 2009; 373: 1275–1281.
Symplicity HTN-2 Investigators, Esler MD, Krum H, Sobotka PA, Schlaich MP, Schmieder RE, Böhm M . Renal sympathetic denervation in patients with treatment-resistant hypertension (The Symplicity HTN-2 trial): a randomised controlled trial. Lancet 2010; 376: 1903–1909.
Kario K . Morning surge in blood pressure in hypertension: clinical relevance, prognostic significance and therapeutic approach. In: Berbari AE, Mancia G (eds). Springer Inc.. 2012 pp 71–89.
Ueshima H, Sekikawa A, Miura K, Turin TC, Takashima N, Kita Y, Watanabe M, Kadota A, Okuda N, Kadowaki T, Nakamura Y, Okamura T . Cardiovascular disease and risk factors in Asia: a selected review. Circulation 2008; 118: 2702–2709.
Ishikawa Y, Ishikawa J, Ishikawa S, Kajii E, Schwartz JE, Pickering TG, Kario K, Jichi Medical School Cohort Investigators Group. Prehypertension and the risk for cardiovascular disease in the Japanese general population: the Jichi Medical School Cohort Study. J Hypertens 2010; 28: 1630–1637.
Perkovic V, Huxley R, Wu Y, Prabhakaran D, MacMahon S . The burden of blood pressure-related disease: a neglected priority for global health. Hypertension 2007; 50: 991–997.
Stamler J . The INTERSALT Study: background, methods, findings, and implications. Am J Clin Nutr. 1997; 65: 626S–642S.
Katsuya T, Ishikawa K, Sugimoto K, Rakugi H, Ogihara T . Salt sensitivity of Japanese from the viewpoint of gene polymorphism. Hypertens Res 2003; 26: 521–525.
Kubo M, Hata J, Doi Y, Tanizaki Y, Iida M, Kiyohara Y . Secular trends in the incidence of and risk factors for ischemic stroke and its subtypes in Japanese population. Circulation 2008; 118: 2672–2678.
Uzu T, Kimura G, Yamauchi A, Kanasaki M, Isshiki K, Araki S, Sugiomoto T, Nishio Y, Maegawa H, Koya D, Haneda M, Kashiwagi A . Enhanced sodium sensitivity and disturbed circadian rhythm of blood pressure in essential hypertension. J Hypertens 2006; 24: 1627–1632.
Chen Jing, Gu Dongfeng, Huang Jianfeng, Rao DC, Jaquish CashellE, Hixson JamesE, Chen Chung-Shiuan, Chen Jichun, Lu Fanghong, Hu Dongsheng, Rice Treva, Kelly TanikaN, Hamm LLee, Whelton PaulK, He. Jiang . Metabolic syndrome and salt-sensitivity of blood pressure among persons without diabetes. Lancet 2009; 373: 829–835.
Ishikawa Y, Ishikawa J, Ishikawa S, Kayaba K, Nakamura Y, Shimada K, Kajii E, Pickering TG, Kario K, Jichi Medical School Cohort Investigators Group. Prevalence and determinants of prehypertension in a Japanese general population: the Jichi Medical School Cohort Study. Hypertens Res 2008; 31: 1323–1330.
Greenlund KJ, Croft JB, Mensah GA . Prevalence of heart disease and stroke risk factors in persons with prehypertension in the United States, 1999-2000. Arch Intern Med 2004; 164: 2113–2118.
Li Y, Wang JG, Gao P, Guo H, Nawrot T, Wang G, Qian Y, Staessen JA, Zhu D . Are published characteristics of the ambulatory blood pressure generalizable to rural Chinese? The JingNing population Study. Blood Press Monit 2005; 10: 125–134.
Calhoun DA, Jones D, Textor S, Goff DC, Murphy TP, Toto RD, White A, Cushman WC, White W, Sica D, Ferdinand K, Giles TD, Falkner B, Carey RM . Resistant hypertension: diagnosis, evaluation, and treatment. A scientific statement from the American Heart Association Professional Education Committee of the Council for High Blood Pressure Research. Hypertension 2008; 51: 1403–1419.
Kario K . Obstructive sleep apnea syndrome and hypertension: ambulatory blood pressure. Hypertens Res 2009; 32: 428–432.
Pedrosa RP, Drager LF, Gonzaga CC, Sousa MG, de Paula LK, Amaro AC, Amodeo C, Bortolotto LA, Krieger EM, Bradley TD, Lorenzi-Filho G . Obstructive sleep apnea: the most common secondary cause of hypertension associated with resistant hypertension. Hypertension 2011; 58: 811–817.
Salles GF, Cardoso CRL, Muxfeldt ES . Prognostic influence of office and ambulatory blood pressures in resistant hypertension. Arch Intern Med 2008; 168: 2340–2346.
Muxfeldt ES, Cardoso CRL, Salles GF . Prognostic value of nocturnal blood pressure reduction in resistant hypertension. Arch Intern Med 2009; 169: 874–880.
Kario K, Matsuo T, Kobayashi H, Imiya M, Matsuo M, Shimada K . Nocturnal fall of blood pressure and silent cerebrovascular damage in elderly hypertensive patients. Advanced silent cerebrovascular damage in extreme dippers. Hypertension 1996; 27: 130–135.
Hoshide S, Kario K, Hoshide Y, Umeda Y, Hashimoto T, Kunii O, Ojima T, Shimada K . Associations between nondipping of nocturnal blood pressure decrease and cardiovascular target organ damage in strictly selected community-dwelling normotensives. Am J Hypertens 2003; 16: 434–348.
Viera AJ, Lin FC, Hinderliter AL, Shimbo D, Person SD, Pletcher MJ, Jacobs DR Jr . Nighttime blood pressure dipping in young adults and coronary artery calcium 10-15 years later: the coronary artery risk development in young adults study. Hypertension 2012; 59: 1157–1163.
Pickering TG, Miller NH, Ogedegbe Gbenga, Krakoff LR, Artinian NT, Goff D . Call to action on use and reimbursement for home blood pressure monitoring a joint scientific statement from the American Heart Association, American Society of Hypertension, and the Preventive Cardiovascular Nurses Association. Hypertension 2008; 52: 10–29.
Kario K, Pickering TG, Matsuo T, Hoshide S, Schwartz JE, Shimada K . Stroke prognosis and abnormal nocturnal blood pressure falls in older hypertensives. Hypertension 2001; 38: 852–857.
Kabutoya T, Hoshide S, Ishikawa J, Eguchi K, Shimada K, Kario K . The effect of pulse rate and blood pressure dipping status on the risk of stroke and cardiovascular disease in Japanese hypertensive patients. Am J Hypertens 2010; 23: 749–755.
Yano Y, Inokuchi T, Hoshide S, Kanemaru Y, Shimada K, Kario K . Association of poor physical function and cognitive dysfunction with high nocturnal blood pressure level in treated elderly hypertensive patients. Am J Hypertens 2011; 24: 285–291.
de la Sierra A, Segura J, Banegas JR, Gorostidi M, de la Cruz JJ, Armario P, Oliveras A, Ruilope LM . Clinical features of 8295 patients with resistant hypertension classified on the basis of ambulatory blood pressure monitoring. Hypertension 2011; 57: 898–902.
Kario K, Pickering TG, Umeda Y, Hoshide S, Hoshide Y, Morinari M, Murata M, Kuroda T, Schwartz JE, Shimada K . Morning surge in blood pressure as a predictor of silent and clinical cerebrovascular disease in elderly hypertensives: a prospective study. Circulation 2003; 107: 1401–1406.
Kario K . Morning surge in blood pressure and cardiovascular risk: evidence and perspectives. Hypertension 2010; 56: 765–773.
Pimenta E, Gaddam KK, Oparil S, Aban I, Husain S, Dell'Italia LJ, Calhoun DA . Effects of dietary sodium reduction on blood pressure in subjects with resistant hypertension: results from a randomized trial. Hypertension 2009; 54: 475–481.
Uzu T, Ishikawa K, Fujii T, Nakamura S, Inenaga T, Kimura G . Sodium restriction shifts circadian rhythm of blood pressure from nondipper to dipper in essential hypertension. Circulation 1997; 96: 1859–1862.
Kario K . Proposal of RAS-diuretic vs. RAS-calcium antagonist strategies in high-risk hypertension: insight from the 24-hour ambulatory blood pressure profile and central pressure. J Am Soc Hypertens 2010; 4: 215–218.
Webb AJ, Fischer U, Mehta Z, Rothwell PM . Effects of antihypertensive-drug class on interindividual variation in blood pressure and risk of stroke: a systematic review and meta-analysis. Lancet 2010; 375: 906–915.
Webb AJ, Rothwell PM . Effect of dose and combination of antihypertensives on interindividual blood pressure variability: a systematic review. Stroke 2011; 42: 2860–2865.
Kario K, Shimada K . Differential effects of amlodipine on ambulatory blood pressure in elderly hypertensive patients with different nocturnal reductions in blood pressure. Am J Hypertens 1997; 10: 261–268.
Wang JG, Kario K, Lau T, Wei YQ, Park CG, Kim CH, Huang J, Zhang W, Li Y, Yan P, Hu D, Asian Pacific Heart Association. Use of dihydropyridine calcium channel blockers in the management of hypertension in Eastern Asians: a scientific statement from the Asian Pacific Heart Association. Hypertens Res 2011; 34: 423–430.
Uzu T, Kimura G . Diuretics shift circadian rhythm of blood pressure from nondipper to dipper in essential hypertension. Circulation 1999; 100: 1635–1638.
Matsui Y, Eguchi K, Ishikawa J, Shimada K, Kario K . Urinary albumin excretion during angiotensin II receptor blockade: comparison of combination treatment with a diuretic or a calcium-channel blocker. Am J Hypertens 2011; 24: 466–473.
Eguchi K, Hoshide S, Kabutoya T, Shimada K, Kario K . Is very low dose hydrochlorothiazide combined with candesartan effective in uncontrolled hypertensive patients? Blood Press Monit 2010; 15: 308–311.
Nishizaka MK, Zaman MA, Calhoun DA . Efficacy of low-dose spironolactone in subjects with resistant hypertension. Am J Hypertens 2003; 16: 925–930.
Yano Y, Hoshide S, Tamaki N, Nagata M, Sasaki K, Kanemaru Y, Shimada K, Kario K . Efficacy of eplerenone added to renin-angiotensin blockade in elderly hypertensive patients: the Jichi-Eplerenone Treatment (JET) study. J Renin Angiotensin Aldosterone Syst 2011; 12: 340–347.
Ruilope LM, Dukat A, Böhm M, Lacourcière Y, Gong J, Lefkowitz MP . Blood-pressure reduction with LCZ696, a novel dual-acting inhibitor of the angiotensin II receptor and neprilysin: a randomised, double-blind, placebo-controlled, active comparator study. Lancet 2010; 375: 1255–1266.
Solomon SD, Zile M, Pieske B, Voors A, Shah A, Kraigher-Krainer E, Shi V, Bransford T, Takeuchi M, Gong J, Lefkowitz M, Packer M, McMurray JJ, . Prospective comparison of ARNI with ARB on Management Of heart failure with preserved ejection fraction (PARAMOUNT) Investigators. The angiotensin receptor neprilysin inhibitor LCZ696 in heart failure with preserved ejection fraction: a phase 2 double-blind randomised controlled trial. Lancet 2012; 380: 1387–1395.
Kario K, Matsui Y, Shibasaki S, Eguchi K, Ishikawa J, Hoshide S, Ishikawa S, Kabutoya T, Schwartz JE, Pickering TG, Shimada K., Japan Morning Surge-1 (JMS-1) Study Group. An alpha-adrenergic blocker titrated by self-measured blood pressure recordings lowered blood pressure and microalbuminuria in patients with morning hypertension: the Japan Morning Surge-1 Study. J Hypertens 2008; 26: 1257–1265.
Marfella R, Siniscalchi M, Nappo F, Gualdiero P, Esposito K, Sasso FC, Cacciapuoti F, Di Filippo C, Rossi F, D'Amico M, Giugliano D . Regression of carotid atherosclerosis by control of morning blood pressure peak in newly diagnosed hypertensive patients. Am J Hypertens 2005; 18: 308–318.
Kario K, Hoshide S, Shimizu M, Yano Y, Eguchi K, Ishikawa J, Ishikawa S, Shimada K . Effect of dosing time of angiotensin II receptor blockade titrated by self-measured blood pressure recordings on cardiorenal protection in hypertensives: the Japan Morning Surge-Target Organ Protection (J-TOP) study. J Hypertens 2010; 28: 1574–1583.
Yano Y, Hoshide S, Shimizu M, Eguchi K, Ishikawa J, Ishikawa S, Shimada K, Kario K . Association of home and ambulatory blood pressure changes with changes in cardiovascular biomarkers during antihypertensive treatment. Am J Hypertens 2012; 25: 306–312.
Mahfoud F, Schlaich M, Kindermann I, Ukena C, Cremers B, Brandt MC, Hoppe UC, Vonend O, Rump LC, Sobotka PA, Krum H, Esler M, Böhm M . Effect of renal sympathetic denervation on glucose metabolism in patients with resistant hypertension: a pilot study. Circulation 2011; 123: 1940–1946.
Mahfoud F, Cremers B, Janker J, Link B, Vonend O, Ukena C, Linz D, Schmieder R, Rump LC, Kindermann I, Sobotka PA, Krum H, Scheller B, Schlaich M, Laufs U, Böhm M . Renal hemodynamics and renal function after catheter-based renal sympathetic denervation in patients with resistant hypertension. Hypertension 2012; 60: 419–424.
Brandt MC, Mahfoud F, Reda S, Schirmer SH, Erdmann E, Böhm M, Hoppe UC . Renal sympathetic denervation reduces left ventricular hypertrophy and improves cardiac function in patients with resistant hypertension. J Am Coll Cardiol 2012; 59: 901–909.
Ishikawa J, Hoshide S, Eguchi K, Ishikawa S, Shimada K, Kario K . Nighttime home blood pressure and the risk of hypertensive target organ damage. Hypertension 2012; 60: 921–928.
Chonan K, Kikuya M, Araki T, Fujiwara T, Suzuki M, Michimata M, Hashimoto J, Ohkubo T, Hozawa A, Yamamoto N, Miyawaki Y, Matsubara M, Imai Y . Device for the self-measurement of blood pressure that can monitor blood pressure during sleep. Blood Press Monit 2001; 6: 203–205.
Shirasaki O, Kuwabara M, Saito M, Tagami K, Washiya S, Kario K . Development and clinical application of a new technique for detecting 'sleep blood pressure surges' in sleep apnea patients based on a variable desaturation threshold. Hypertens Res 2011; 34: 922–928.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Kario, K. Proposal of a new strategy for ambulatory blood pressure profile-based management of resistant hypertension in the era of renal denervation. Hypertens Res 36, 478–484 (2013). https://doi.org/10.1038/hr.2013.19
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/hr.2013.19
Keywords
This article is cited by
-
Effect of renal denervation in attenuating the stress of morning surge in blood pressure: post-hoc analysis from the SPYRAL HTN-ON MED trial
Clinical Research in Cardiology (2021)
-
Expert panel consensus recommendations for home blood pressure monitoring in Asia: the Hope Asia Network
Journal of Human Hypertension (2018)
-
The Sacubitril/Valsartan, a First-in-Class, Angiotensin Receptor Neprilysin Inhibitor (ARNI): Potential Uses in Hypertension, Heart Failure, and Beyond
Current Cardiology Reports (2018)
-
Perfect 24-h management of hypertension: clinical relevance and perspectives
Journal of Human Hypertension (2017)
-
The efficacy and long-term safety of a triple combination of 80 mg telmisartan, 5 mg amlodipine and 12.5 mg hydrochlorothiazide in Japanese patients with essential hypertension: a randomized, double-blind study with open-label extension
Hypertension Research (2017)