Abstract
Tuberous sclerosis complex is an autosomal dominant neurocutaneous disorder marked by hamartoma growth in multiple organ systems. We performed mutational analyses on 325 individuals with definite tuberous sclerosis complex diagnostic status. We identified mutations in 72% (199/257) of de novo and 77% (53/68) of familial cases, with 17% of mutations in the TSC1 gene and 50% in the TSC2 gene. There were 4% unclassified variants and 29% with no mutation identified. Genotype/phenotype analyses of all observed tuberous sclerosis complex findings in probands were performed, including several clinical features not analyzed in two previous large studies. We showed that patients with TSC2 mutations have significantly more hypomelanotic macules and learning disability in contrast to those with TSC1 mutations, findings not noted in previous studies. We also observed results consistent with two similar studies suggesting that individuals with mutations in TSC2 have more severe symptoms. On performing meta-analyses of our data and the other two largest studies in the literature, we found significant correlations for several features that individual studies did not have sufficient power to conclude. Male patients showed more frequent neurologic and eye symptoms, renal cysts, and ungual fibromas. Correlating genotypes with phenotypes should facilitate the disease management of tuberous sclerosis complex.
Similar content being viewed by others
Main
Tuberous sclerosis complex (TSC) is an autosomal dominant condition affecting multiple organ systems. The incidence is estimated between 1 per 6000 live births and 1 per 25,000; approximately two-thirds of cases are de novo (Online Mendelian Inheritance in Man 191100).1 The clinical diagnosis of TSC relies on familiarity with the published diagnostic criteria.2,3 Two genes have been identified as causative for TSC. The TSC2 gene, located on chromosome 16p13.3, codes for tuberin, named for its association with TSC. This gene has 41 exons distributed over approximately 40 kb of genomic DNA. It has alternative splice sites at two exons (25 and 31) to create isoforms.4,5 Tuberin has a calculated molecular weight of approximately 200 kD coding from a transcript of approximately 5.5 kb. The TSC1 gene was discovered a decade after the initial report of linkage (Online Mendelian Inheritance in Man 191100).6 In contrast with the TSC2 gene, the TSC1 gene has 23 exons extending over approximately 55 kb of genomic DNA on chromosome 9q34.3. The TSC1 gene product is coded from exons 3 to 23. Noncoding sequences include exons 1 and 2, and a 4.5-kb 3′ untranslated region. The protein product of the TSC1 gene (hamartin) has an estimated molecular weight of 130 kD coding from an 8.6-kb mRNA transcript. To date, more than 680 disease-causing mutations have been identified in either the TSC1 or TSC2 genes.7 Approximately 70% to 80% of individuals who meet definite diagnostic criteria have a small identifiable TSC1 or TSC2 gene mutation. The remaining individuals probably have large gene deletions, somatic mosaic mutations, and mutations in unanalyzed gene noncoding regions, rather than an additional TSC gene locus.
Of interest is whether the phenotypic presentation of TSC differs by whether the disease results from mutations in TSC1 or TSC2. Early studies reporting genotype/phenotype correlations did not find evidence for phenotypic differences between patients with TSC1 mutations and patients with no mutation identified (NMI) or patients with TSC1 versus TSC2 mutations.8,9 These studies, however, tended to have smaller sample sizes. Larger studies found that a more severe phenotype was associated with TSC2 mutations. Jones et al.10,11 noted an increased prevalence of mental retardation (MR) with TSC2 mutations. Likewise, Lewis et al.12 found increased MR, autistic disorder, and infantile spasms with TSC2 mutations. The two largest studies published to date found multiple clinical findings more frequent in individuals with TSC2 mutations.13,14 Dabora et al.13 observed more frequent seizures, moderate and severe MR, central nervous system tumors, retinal hamartomas, angiomyolipomas (AMLs), and facial angiofibromas with TSC2 mutations. Sancak et al.14 confirmed some of these observations when they reported an increased prevalence of MR, AMLs, retinal phakomas, and retinal depigmentations with TSC2 mutations. They reported an equal prevalence of seizures and subcortical tubers with TSC1 and TSC2 mutations. All of these studies primarily included patients with de novo TSC and index patients with familial TSC in their analyses.
In this study, we performed mutational analysis for the TSC1 and TSC2 genes on 368 randomly ascertained index cases and compared this with the major and minor diagnostic features and neurobehavioral features to describe the genotype/phenotype association in TSC. As in the previous two largest studies,13,14 the majority of our patients have a mutation in the TSC2 gene. We found that these patients generally have a more severe disease phenotype than those with TSC1 mutations. Our study confirms reported findings and extends the genotype/phenotype associations to the neurobehavioral features. We also compared mutation type (protein truncation [PT] vs. missense [MS]) with phenotypic features, as well as phenotypic features in de novo patients with those observed in familial probands. These latter comparisons were made to determine whether there is additional prognostic information that can be provided to families based on genetic test results or mode of inheritance.
MATERIALS AND METHODS
Patients
Patients with a diagnosis of TSC were enrolled between 1987 and 2004 with informed consents approved by the institutional review boards at The University of Texas Health Science Center at Houston and The University of Texas Southwestern Medical School—Texas Scottish Rite Hospital. The goal for enrolling was to identify the genetic cause of TSC in these patients. Patients enrolled between 1987 and 1999 were evaluated by Dr. Northrup or collaborators in the Texas Scottish Rite Hospital using criteria set up between the groups. All observable clinical features were recorded, including but not limited to known diagnostic features. Patients enrolled between 2000 and 2004 were requested to provide TSC features in a standardized form designed in our laboratory combining diagnostic features we observed and those suggested by Roach et al.2,3 Our study also included samples of several TSC families from the Coriell Cell Repository (TSC families 650, 748, 920, 921, 1036, 2149, 2150, 2500, 2501, and 2502). Patients were characterized according to Roach et al.2 as having a definite, probable, or possible diagnosis of TSC. For familial TSC cases enrolled between 1987 and 1999, we included as many affected and unaffected family members as possible, but only the index patients from families with multiple affected members were used for phenotypic analyses.
Mutation screening
DNA was extracted from peripheral blood lymphocytes using a standard phenol/chloroform extraction method for patient samples collected through 1999 and using Puregene DNA extraction kits (Gentra Systems Inc., Minneapolis, MN) for patient samples collected between 2000 and 2004. Mutational analysis was performed on samples collected before 2000 using a combination of single-strand conformational analysis (SSCA) and direct sequencing when variants were identified. Pre-2000 samples with NMI and samples collected during and after 2000 were tested using direct sequencing. SSCA was performed as described previously.15,16 Direct sequencing was performed for all coding exons of the TSC1 and TSC2 genes following the ABI BigDye Terminator (Applied Biosystems, Foster City, CA) sequencing protocol. Patient DNA sequences were compared with RefSeq sequences of TSC1 (NM_000368) and TSC2 (NM_000548) from the GenBank. A nucleotide change was considered pathogenic when it (1) was a confirmed recurring mutation by independent groups; (2) resulted in PT; (3) was not observed in either parent and paternity was confirmed; and (4) was proved by functional assays. A nucleotide was considered a polymorphism when it was (1) present in the DNA of an unaffected parent, (2) previously reported in the literature as a polymorphic variant, or (3) present in addition to a definite disease-causing variant. A nucleotide change was considered a variant of unknown significance (or unclassifiable variant) when it was novel and parents were unavailable for study.
Statistical analysis
The TSC disease features for the following groups were compared: (1) gene loci mutated TSC1 versus TSC2 versus NMI; (2) MS versus PT, TSC2 MS versus TSC1 and TSC2 PT together, and TSC2 MS versus TSC2 PT; (3) familial versus de novo (familial probands only vs. de novo; all familial patients vs. de novo); and (4) NMI versus different mutation groups. We analyzed our patient clinical findings by grouping our patients according to gender, familial or de novo, mutation in TSC1, TSC2, or NMI, and MS or PT mutation. Because patients came from different sources and may not have all diagnostic criteria assessed, the numbers for each analysis varied. We used information from patients with a definite diagnosis for our statistical analyses. Significance testing was by chi-square analyses and the Fisher exact test. To compare our dataset with those reported by Dabora et al.13 and Sancak et al.,14 we performed meta-analyses on individual and combined data of the TSC features reported. Odds ratios and 95% confidence intervals were calculated to quantify differences between the groups. Alpha was set at 0.05 for significance testing.
RESULTS
Patients' characteristics
Subjects were identified from 368 unrelated families who were enrolled in our research protocol between 1987 and 2004 through three primary sources: the Medical Genetics Clinics of The University of Texas Medical School at Houston, Texas (n = 129); the Texas Scottish Rite Hospital for Children, Dallas, Texas (n = 118); and referrals from the Tuberous Sclerosis Alliance (n = 121). A total of 506 affected individuals (297 de novo and 209 familial cases) were included in the mutation screening process. For each affected individual, we collected phenotype data on the major and minor diagnostic criteria for TSC and neurobehavioral features. The majority of patients (88%) were confirmed to meet the criteria for definite diagnosis.2,3 Clinical information was not available for every feature of TSC on every participant. Approximately 8% of patients (n = 29) did not meet the clinical criteria for definite diagnosis but had clinical findings meeting criteria for either a probable or possible diagnosis. Some patients were referred and enrolled in the mutation screening process without sending sufficient clinical information to determine diagnostic status (n = 14). Patients who did not meet TSC diagnostic criteria or who had no clinical information were not included in the phenotype analysis. We have, however, included them in the description of the mutations. As previously suggested, there is no gender, age, or ethnic preference for either TSC gene mutated. The median age of evaluation for all index patients was 10 years, and the average age was 12.4 years (age range 0–64 years). Our distribution was skewed, and approximately 51% of all patients were evaluated at or less than 10 years of age. Female index patients accounted for 54.6% of subjects (196/359). Table 1 details the demographic characteristics of our study population. A total of 299 patients have ethnic information, and 220 (73.6%) are non-Hispanic white. The remaining 26.4% include Hispanic (14.1%), African American (7.1%), Asian American (4.3%), and Native American (0.9%). As expected, patients with a definite TSC diagnosis were more likely to have a mutation identified (72%, 234/325) than patients with possible (5%; 1/21) and probable (13%; 1/8) diagnoses or no diagnostic information (50%; 7/14). Among patients with a definite diagnosis, identification of a mutation for patients with familial TSC is higher (77%; 52/68) than for patients with de novo TSC (71%; 182/257), but this is not statistically significant.
Mutation analysis
We identified small pathogenic mutations for 243 families and variants of unknown significance for 17 families lacking one or both parents for verification. Two families with large deletions in the TSC2 gene were identified among samples enrolled between 1987 and 1999 who were tested with Southern blot analyses. No small mutation could be identified for 108 patients (29.3%). Among 71 TSC families with multiple affected individuals, 25 (35.2%) have mutations in TSC1 and 28 (39.4%) have mutations in TSC2 resulting in a TSC1:TSC2 ratio of 1:1.1. Thirty-six of 297 patients (12.1%) with de novo TSC have mutations in TSC1 and 154 patients (51.9%) have mutations in TSC2, resulting in a TSC1:TSC2 ratio of approximately 1:4. The TSC1:TSC2 mutation ratios for familial cases is significantly different from the de novo cases (P = .0002).
Almost all mutations identified in TSC1 are predicted to cause PT (98.4%; 60/61), except one patient who has a MS mutation in exon 9 that is confirmed to be de novo (Table 2). Approximately 67% of TSC2 gene mutations are predicted to cause PT, and 32% are MS mutations confirmed as noted in the “Materials and Methods” section.
In this study we observed the largest exon of TSC1 (exon 15) and exon 16 of TSC2 to individually account for the highest percentage of mutations identified, with each contributing approximately 7% (17/243). The largest exon of TSC2 gene (exon 33) accounted for only 4% (10/243) of all mutations. Approximately 12.3% of the mutations reside within the GAP domain of tuberin that spans exons 36 to 40 of the TSC2 gene. Approximately half of the GAP domain mutations are MS or in-frame deletion mutations. We also calculated mutation frequency per nucleotide for all coding exons and found that exon 16, with a rate of 0.13 mutations per nucleotide, had the highest rate, followed by rates of 0.09 for exon 40 and 0.07 for exon 23 of TSC2. Exons 3, 26, 30, 34, 35, and 39 of TSC2 and exons 8 and 10 of TSC1 have mutation frequencies of approximately 0.05 per nucleotide. We did not find any mutations in coding exons 3, 4, 7, 12, 22, and 23 of the TSC1 gene or mutations in exons 6, 25, or 31 of the TSC2 gene.
The single most common site for mutation, accounting for 6.2% of the total in this study, was exon 16 on codon R611 of TSC2 gene with R611W (c.1831C>T) found in 10 cases and R611Q (c.1832G>A) in 5 cases. A common in-frame deletion involving amino acids 1746_1751 (HIKRLR; c.5238_5255del) in exon 40 of TSC2 gene reported by others is seen in five independent families (2.1%) in this study.
Overall clinical features observed
The overall frequencies of observed clinical features for all patients with TSC in our study are consistent with previous observations (Table 3). Table 3 lists all abbreviations for phenotypic features used throughout the rest of the article. We also observed some features that were not reported in the two previous studies:13,14 confetti skin lesions (58%), cerebral white matter radial migration lines (28%), rectal polyps (10%), and bone cysts (11%). In addition, our study showed many features with frequencies lower than in the two previous studies (FA, SP, FFP, AP, Tub, SEN, MR, SZ, DEP, and GF).
Phenotype comparisons
For phenotype comparison, we have clinical information collected on 325 definite, 8 probable, and 21 possible diagnosed TSC index patients. We compared phenotypes of these patients by gender and their mutations (Tables 4 and 5). Of the 14 patients with no clinical information available, we identified pathogenic mutations predicted to cause premature protein termination for seven. Two mutations were found in TSC1 gene (c.231_232delTC and c.1669 delC), and five were found in TSC2 gene (c.226 -2A>G, c.268C>T, c.1513C>T, c.4971delC and c.5259 + 1 delG). A mutation was identified in DNA from a fetus with a cardiac rhabdomyoma classified as having a possible diagnosis (c.4115_4116delTG). Another patient with a probable TSC diagnosis at 1 month of age with cortical tubers and retinal achromic patches was found to have the c.1832G>A mutation.
Male versus female patients
We compared male patients (163) with female patients (196) in our cohort to identify whether TSC features differ between genders. The median age for male patients (8 years) is not significantly different from that of the female patients (10.6 years) (P = .6438). The average ages are 11.1 and 12.8 years for male and female patients, respectively. There are no significant differences in diagnostic criteria (P = .0521), ratio of TSC1 to TSC2 mutated (P = .3508), or mode of inheritance (P = .3700) between genders. Overall, our male patients exhibited significantly more neurologic findings of cortical tubers (89.7% vs. 78.9%), SEN (88.9% vs. 78.4%), MR (52.8% vs. 40.0%), and SZ (82.6% vs. 66.9%) than the female patients (Tables 4 and 5). In addition, male patients also showed a nonsignificant increase of retinal phakoma compared with female patients.
Familial versus de novo patients
To investigate the phenotypic effects of mutation between the TSC1 gene and the TSC2 gene, TSC features for 70 familial index patients and 297 de novo patients were analyzed according to the modes of inheritance and effects of gene mutated. The median age was 10.5 years for familial index patients and 9 years for de novo patients with average ages of 13.4 and 11.8 years, respectively. Comparison of the disease features of these two groups indicated that familial patients exhibit significantly less frequent SEN, RA, and RC, but more frequent HM. Frequencies of other disease features do not show any significant differences. We also noted that familial patients have a significantly higher proportion of TSC1 gene mutations than TSC2 gene mutations compared with de novo patients (P < .001). Familial patients were significantly more likely (P < .001) than de novo patients to have a definite diagnosis, with the de novo patients more likely to be in the possible or probable diagnostic categories.
Because the percentage of de novo patients with a definite diagnosis was significantly less than that of familial patients, we further restricted our analysis to patients with mutations identified in the TSC1 or TSC2 genes to account for the effect of diagnostic category (P = .5932). A total of 52 familial and 182 de novo index patients were included in this analysis. The median ages were 11 and 9.25 years for familial and de novo patient groups with average ages of 13.5 and 11 years, respectively (P = .7237). After the removal of any effect of diagnostic category, two disease features (SEN and RA) remained higher in de novo patients. Two disease features (RH and MR) reached significance in patients with de novo TSC.
Gene mutation effect on tuberous sclerosis complex features
We examined the effect of gene mutation on TSC disease features by comparing patients with a definite diagnosis, including 59 patients with TSC1 mutations and 177 patients with TSC2 mutations. The median ages were 10.67 and 9 years (P = .8509), and the average ages were 12.5 and 11.2 years, respectively. A significant difference in the ratio of MS mutation versus PT mutation type between TSC1 and TSC2 was observed (P < .001). Patients with TSC2 mutations had significantly higher frequencies of SEN, MR, LD, HM, FA, FFP, RA, RC, and RH. A trend of a higher frequency of behavioral problems associated with TSC1 mutation was observed (P = .0570).
To determine whether gene mutation (TSC1 versus TSC2) showed different effects in familial TSC cases, TSC disease features from a total of 52 familial index patients, including 25 patients with mutations in TSC1 and 27 patients with mutations in TSC2, were analyzed. The median ages were 12 and 14 years (P = .2252), and the average ages were 15.64 and 15.58 years, respectively. A slightly higher frequency of SEGA, Beh, Con, UF, SP, AP, DEP, and GF was found in familial index patients with TSC1 mutation, whereas features including Tub, SEN, CRML, MR, LD, IS, SZ, HM, FA, FFP, RA, RC, Ham, and retinal tumors were more frequent in familial patients with TSC2 mutation. However, no features reached significance because of the small numbers in this analysis.
When comparing de novo case patients only, we analyzed the disease features of 35 de novo patients with TSC1 mutation compared with 150 de novo patients with TSC2 mutation. The median ages were 10.3 and 9 years (P = 1.00), and the average ages were 11.61 and 10.84, respectively. A significant difference in the ratio of MS versus PT mutation type was observed (P < .001). The results were similar to the combined familial and de novo index patient analyses. De novo patients with TSC2 mutations showed significantly higher frequencies of SEN, MR, LD, HM, FA, FFP, RA, RC, and RH than de novo patients with TSC1 mutations. The trend of higher frequency of behavioral problems associated with TSC1 mutation remained.
Mutation type effect
The type of mutations in many single gene disorders affects disease severity. To evaluate the effect of the type of mutations on the presence of TSC features, we compared features of patients by grouping them into two main categories: mutations predicted to cause PT (including nonsense, out-of-frame insertion/deletion, and cryptic splice sites) and mutations predicted to cause amino acid substitution (MS mutation and in-frame insertion/deletion).
Our analyses showed that patients with TSC2 PT mutation are more likely to have SEN, MR, LD, RA, RC, HM, FA, FFP, and retinal tumor compared with patients who have TSC1 PT mutations. In addition, nonrenal hamartoma occurrence increased among patients with TSC2 PT mutation (7/9 vs. 0/7, P = .036). A trend of higher seizure occurrence associated with TSC2 PT mutation was also observed (91/108 vs. 38/53, P = .060). The median age for patients with TSC1 or TSC2 PT mutation were both 10.71 years (P = .8), and the average ages were 12.7 and 12.2 years, respectively.
MS mutations in the TSC2 gene seem to cause similar disease phenotypes as PT mutation in the TSC2 gene. All features are equally presented between the group of patients with TSC2 MS mutation versus TSC2 PT mutation except that the MS mutation group has less UF and Ham. Patients with TSC2 MS mutations are younger, with a median age of 7 and 10.71 years for patients with TSC2 PT mutation, but the difference is not significant (P = .9416).
MS mutation in the TSC2 gene resulted in more severe disease than PT mutations in the TSC1 gene. Patients with MS mutations in the TSC2 gene have a higher risk for more severe phenotypes of SEN, MR, RA, RC, CRM, FA, FFP, and retinal tumors. More behavioral problems seem to be associated with TSC1 PT mutation (7/8 vs. 7/16, P = .0270), a trend that was consistent when comparing all patients with TSC1 mutation with those with TSC2 mutation.
Patients with no mutation identified and patients with mutation identified
Because of the mutation screening method, the TSC NMI patient group is likely to be enriched with patients having large gene deletion mutations of the TSC2 gene. The median age for patients with NMI is 9.5 years, the same as for the group of patients with mutations identified in the TSC1 and TSC2 genes (P = .4973), and the average ages are 11.6 and 13.4 years, respectively. However, a significant difference in definite diagnostic status between the two groups was observed (P < .0001), and more female patients were present in the NMI group (68/105 vs. 116/237, P = .0068). Features that are significantly more frequent in the mutation identified groups include Tub, SEN, IS, SZ, HM, CON, UF, SP FFP, CRM, and retinal phakoma.
When the NMI group was compared with the group of patients with TSC1 mutation for all diagnostic criteria, we found higher frequencies of LD, RA, RC, and a trend of higher MR and FA in the NMI group. However, the TSC1 mutation group showed a higher occurrence of greater numbers of HM. Among those meeting definite diagnostic criteria, similar results were observed, suggesting that TSC features for patients with NMI are more severe than for patients with TSC1 mutations.
When the patients with NMI were compared with the patients with TSC2 mutations, we observed much milder phenotypes. There were significantly less tubers, SEN, MR, IS, SZ, CRM, RA, HM, FA, UF, SP, and FFP in the patients with NMI than in the patients with TSC2. Restricting the analysis of TSC2 patients to the group with PT mutation showed similar milder findings.
When the patients with NMI were compared with the patients with TSC2 MS mutation, lower frequencies of tubers, SEN, CRML, IS, SZ, CRM, HM, and FFP were observed in the patients with NMI. Adjustment for diagnostic status made tubers, SEN, and HM equally frequent between patients with NMI or TSC2 MS mutations.
DISCUSSION
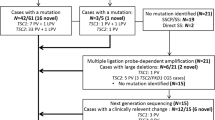
We began our screening by Southern blot testing for large gene deletions in TSC2 among 88 patients with TSC who were enrolled between 1987 and 1997; we identified two families with large deletions.15 We tested for small mutations in all coding exons of the TSC1 and TSC2 genes in DNA from 118 patients enrolled between 1987 and 1999 using SSCA; we identified 80 (66.7%) pathogenic mutations. Some of these mutations have been reported.16 Next, we used direct polymerase chain reaction and sequencing to search for etiologic mutations in the TSC1 and TSC2 genes for 40 patients with NMI screened by SSCA and tested an additional 246 independent patient families enrolled between 1999 and 2004. We found that SSCA missed 20 mutations that were subsequently identified by direct sequencing, increasing the detection rate to 83.3% (100/120) when using both SSCA and sequencing. By using polymerase chain reaction sequencing alone, we found 140 pathogenic and 17 putative mutations in the coding exons. Only 87% of the patients (214/246) enrolled between 1999 and 2004 have clinical information sufficient to make a definite diagnosis; therefore, the mutation detection rate was 72.4% with direct sequencing of patients with a definite diagnosis. Overall, our study observed a small mutation detection rate of 66% (243/368) regardless of diagnosis category and 72% (234/325) for patients with a definite diagnosis. Individual mutations and variants (Supplementary Tables 1 and 2) will be submitted to the TSC Variants Database curates by Povey and Ekong.7 Previous studies using a combination of three or more mutation screening methods to screen small mutations and large gene deletion resulted in a higher mutation detection rate of 70% to 85%.10,13,14 Neither SSCA nor direct sequencing methods will identify large gene deletion/insertion and low percentage mosaic mutations in 100% of cases. Large multi-exon deletion is rarely seen in TSC1 but accounted for approximately 7% of TSC2 mutations in one study.14 In another study, large TSC2 gene deletion was estimated as high as 14%.13 Less than one-third of our patients were screened for large deletions of the TSC2 gene using Southern blot, and this testing consumed large amounts of our patients' DNA. We therefore chose to delay screening for large gene deletions/insertion for the rest of our patients in the hope that different methods under development would use less DNA. Multiplex ligation-dependent probe amplification probes have been developed to identify large gene deletions for patients with multiple exons deleted. Our remaining patients with NMI are currently being tested for gene mutations with this method. In addition, we are developing a complete TSC exons microarray and comparative genomic hybridization method as another avenue for testing patients with NMI.
As noted in previous studies, the mutation detection rate varies from 50% to 62% for patients with no clinical information and from 5% to 27% for those patients without a definite diagnosis but who have TSC features. All studies show a fraction (15%–20%) of patients with TSC who have NMI and possibly have mosaicism for a mutation,17 a mutation in the noncoding but functional gene regions, or mutations in a gene (or genes) other than the two identified TSC genes. Mosaicism among parents of patients with de novo TSC is suggested to be rare when lymphoblast DNAs were examined.18 Similar results have been observed for germline mosaic cases.19 However, an effective method to detect mosaic mutations in de novo patients is not yet available, making it difficult to estimate the frequency of mosaicism in de novo TSC cases.
The types of mutations observed in our study do not differ from other previous studies. Incidentally, few or no mutations were found in exons 22 and 23 of the TSC1 gene and exons 6, 25, 31, and 41 of the TSC2 gene in all three studies after approximately 1000 samples from patients with TSC were examined. Although most of the mutations identified have been spread throughout different exons of both genes, approximately 70% of TSC1 mutations are located in or near exons 8, 9, 10, 15, 17, and 18, and approximately 70% of TSC2 mutations are located in or near exons 9, 13, 14, 16, 23, 24, 29, 30, 33, and 35 to 40.
More than 30% of TSC2 gene mutations are MS, whereas the others are predicted to cause PT. MS and in-frame deletion mutations were found in similar exons (7, 10, 16, 23, 27, 29, and 35–40) for all three studies. Although the functional RHEB-GAP domain is located in exons 35 to 40 of TSC2, the consequences of MS changes in other exons remain unknown. Nellist and coworkers20,21 have begun to elucidate the functions of these other regions. One of the most frequently mutated codons, R611 of TSC2 (accounting for 6% of all mutations) has been demonstrated to be important in regulating mTOR/pS6K function. The phenotypes of 15 patients in our study with R611 mutated varied from mild to severe, suggesting that specific individual factors may interact and modify the effect of defective tuberin. It will be interesting to perform a meta-analysis for all patients with R611 mutation. MS mutations in the TSC2 GAP-domain exons only accounted for approximately 6% of all mutations in our study, in contrast with previous studies suggesting that the GAP domain exons are a major target for MS mutation.22 MS mutation in TSC1 is rare. Sancak et al.14 reported one MS mutation in exon 7. We identified two independent families with MS variants for the same codon G305 (G305R and G305W) in exon 9 in only the affected individuals. The functional significance of these changes is not known.
A significantly higher frequency of TSC2 mutations was identified in de novo cases (TSC1:TSC2 = 1:4) compared with 1:1.1 in familial cases. Previous reports on de novo cases varied with TSC2 mutations reported from 2 to 10 times more commonly and familial cases with approximately equal frequencies.9,11,13,14,23 In general, we observed milder TSC phenotypes among familial cases than among de novo patients, but we did observe a few more severe phenotypes among familial patients with TSC2 mutations in our meta-analyses. Although regional genomic structural differences of the TSC1 and TSC2 genes could significantly contribute to the mutation ratio differences, environmental factors, such as higher morbidity and mortality among patients with more severe TSC phenotypes, also play a part in the observed lower TSC1:TSC2 mutation ratios in familial cases.
In our study, we report the occurrence of common diagnostic features among patients with TSC similar in frequency to other reports, but we also report on several other features that have been less commonly studied (Table 3). An increasing number of studies have linked mutation of TSC genes with new clinical findings that are consistent with the now known multisignaling pathway involvement of tuberin and hamartin.24–26 We observed only 10% of our patients (4/40) to have rectal polyps, in contrast with an earlier report of 78% (14/18) in a gastrointestinal surgery setting.27 Bone cysts, although rare, were found in approximately 11% of our patients (5/47), and we also observed nonrenal hamartomas in 22% of patients (11/51). Approximately 28% of our patients (9/32) showed cerebral white matter radial migration lines associated with cortical tubers. Loss of function of tuberin through mutation has been shown to decrease the quantity and affect the function of the cell cycle kinase inhibitor p27Kip1. Functions of p27Kip1 include promotion of neuron differentiation and migration to the cerebral cortex.28,29 Consistent with other neuropsychiatric studies of patients with TSC,30 approximately 76% of patients (139/183) who have an intelligence quotient greater than 70 were reported to have learning difficulties, and approximately 60% (39/66) showed behavioral problems. Autism, pervasive developmental delay, attention deficit disorder/attention deficit-hyperactivity disorder, obsessive compulsive disorder, and sleep disturbance were all grouped together into the category “behavioral problems” in this study. Systematically reporting the occurrence of all features seen among patients with TSC should help geneticists and clinicians diagnose and plan treatment for patients with TSC.
In comparing male and female patients, we found male patients to have more phenotypic features than female patients, similar to the findings of Sancak et al.14 However, in our study the specific types of features differed from those in the study by Sancak and colleagues. We performed a meta-analysis of our study and Sancak et al.'s, illustrating the features more commonly observed in male patients. Males have more neurologic features in our study, and after we combined both datasets, this led to increased morbidity over that observed in females. The odds for male patients to have these neurologic features were approximately twice that of female patients (Table 6). Male patients also had a higher risk for other features, including retinal phakomas, ungual fibromas, and renal cysts in the meta-analysis. There is no known reason for these observed differences. One possible explanation could be modifier genes coded for on the X chromosome. Another possibility would be a protective effect of hormonal influences between genders.31–33 Future research directions will be to sort out these differences for both provisions of prognostic information and therapeutic interventions.
One of the focuses of this study is to compare these findings with those previously published. In addition, we combined the strength of our study with other studies by analyzing combined data with two previous large genotype/phenotype association studies13,14 by a meta-analysis method. Analysis using pooled data will increase the power of analysis for small-number subgroups in the familial cases and the cases with TSC1 mutations. In general, our results are similar to the two previous genotype/phenotype associations. Our sample, however, does differ slightly from the previous studies in that some skin features (FA, SP, and FFP) and oral features (GF and DEP) are lower. Our patients have a median age (10 years) and an average age (12.4 years) and range (0–64 years) similar to that in Dabora et al.'s study,13 but approximately 3 years younger than that in Sancak et al.'s study14 (median age 13.0 years).
Almost all of the neurologic disease phenotype frequencies are lower than in both of the other studies. This finding is most likely attributable to the ascertainment strategies of the different studies. Both studies by Dabora et al.13 and Sancak et al.14 had ascertainment of patients primarily through neurologists. In contrast, our participants were recruited from diverse sources, including neurologists, pediatric geneticists, genetic counselors, and dermatologists. By limiting recruitment to neurologic practices, the other studies may have enriched the sample for individuals with the neurologic sequelae of TSC. In our patient population, the frequencies of the remaining major and minor diagnostic features of TSC were similar to frequencies reported previously. In addition, we observed behavioral problems and learning disabilities that are also consistent with previous reports.30
We performed a meta-analysis of our study and the other two large studies comparing phenotypes in TSC2 versus TSC1 mutations stratified by gender and mode of inheritance (Tables 6, 7, and 8). Overall, neurologic, renal, and some skin findings were more prominent with the TSC2 mutation in our study and the other studies. With the neurologic and renal features causing the highest morbidity and mortality associated with TSC, this highlights the value of molecular testing for provision of prognostic information.
Both Sancak et al.'s study14 and our study came to the same conclusion that male patients with TSC have a higher risk for MR. Gender information for Dabora et al.'s study13 is not available. Other features, including cortical tubers, SEN, seizures, retinal phakomas, ungual fibromas, and renal cysts, began to show significance when combining both datasets in the meta-analysis. Although the results for retinal achromic patches, facial angiofibromas, and gingival fibromas found by Sancak et al.14 are not shown in the combined data, we noted that the median ages of our patients were 3 years less than those of the patients in Sancak et al.'s study. It is known that many features such as facial angiofibromas become more prominent as patients age.3 Observations from the meta-analysis support the age-related observation and suggest that the age of patients may not contribute to the gender differences we observed in neurologic features together with tumors in the retina and nails.
We wanted to define those features that differ by age groups in this patient population. To do this, we created strata of patients aged 7 years or less and 12 years or more. In general, almost all tumor types increase in frequencies with age except for CRM, which decreased in the older age group. We found approximately equal frequencies of cardiac rhabdomyoma between genders when we looked at the patients aged 7 years or less. Older patients (aged > 12 years) have a much lower frequency of cardiac rhabdomyoma, most likely because of the natural history of these lesions in TSC.34 Skin lesions (FA, UF, RA, and DEP) are significantly higher in the older age group regardless of gender; SP was significantly higher in the older patients for males only. Retinal phakoma was slightly higher in older female patients. Both SP and RH showed similar frequencies between the genders in the younger group. The frequency of HM did not increase with age in both male and female patients. Tubers, MR, LD, IS, and SZ are found less frequently in the older age group when compared with the younger age group. We suggest that this may be attributable to differential survival because severe MR is the leading cause of premature death in TSC.35
Differences between familial probands and de novo patients were minimal, with de novo patients having a few features more commonly than familial patients. Familial patients did have hypomelanotic macules at a higher frequency than de novo patients. A comparison between familial cases and de novo cases is also limited by the number of familial index patients present in all three studies. In meta-analysis, SEN and retinal phakoma are consistently more common in de novo patients, and MR showed marginal significance. Features including seizures and renal AML were observed significantly more frequently in de novo patients only in the combined dataset, whereas no significant difference can be concluded for other features (renal cysts and hypomelanotic macules), as concluded by individual studies.
The milder disease presentations and small number of familial cases in individual studies also make it difficult to perform a genotype/phenotype analysis in this patient group, although a trend remained for patients with TSC2 mutation tending to have more features. By pooling our familial case data and the other two large studies, we demonstrated that four features (MR, renal AML, renal cysts, and retinal phakoma) are more likely to occur in familial patients with TSC2 mutations (Table 8). From individual and combined data analyses, patients with TSC2 mutations regardless of their mode of inheritance are at a higher risk (2–9 times) of having renal AML, retinal phakoma, renal cysts, and MR.
In addition, our NMI group displayed a phenotype intermediate between our TSC1 mutation group and our TSC2 mutation group (Table 5). As in the study by Sancak et al.,14 the patients with NMI showed more severe renal abnormalities than patients with TSC1 mutations, whereas several other features are less frequent than in patients with both mutation types of TSC2. This is not surprising because our NMI group should have a percentage of patients who have large deletions and rearrangements in the TSC2 gene because we did not test for this category of mutation in our sample. Other categories of mutations we did not test because of the lack of a simple direct screening protocol include mosaicism and mutations in the noncoding TSC gene region. In addition, it is unlikely to distinguish unique noncoding polymorphisms from mutation without a robust functional assay in place for verification.
We also compared mutation type in our sample set. The findings were similar to the comparison of the TSC2 mutation with the TSC1 mutation: The TSC2 PT mutations were associated with a more severe phenotype than the TSC1 PT mutations. It has been shown that certain TSC2 MS mutations retained some functions of tuberin that possibly contribute to milder phenotypes.20 In our study, the TSC2 PT mutations did not produce a more severe phenotype than the TSC2 MS mutations, indicating that prognostic information regarding TSC2 MS mutations will be specific. Discovering this information will take additional research.
Some TSC features are reported to be found together.13,14,36 We assessed whether specific TSC disease features were associated with each other by comparing frequencies of all other features between groups of patients with the absence and presence of the finding. Patients who have a history of seizures (n = 243) are more likely to also have a higher frequency of tubers (P < .0001), subependymal nodules (P < .0001), cerebral white matter migration lines (P = .035), MR (P < .0001), learning disabilities (P < .0001), infantile spasms (P < .0001), and behavioral problems (P = .0001). Similarly, patients who have tubers (n = 220) are significantly more likely to have SEN (P < .0001), MR (P < .0001), LD (P < .0001), IS (P = .0025), SZ (P < .0001), and facial angiofibromas (P = .0136). Hypomelanotic macules (P < .001) are significantly associated with the presence of tubers or seizures. When comparing patients with and without MR, we found that almost all neurologic findings except SEGA are significantly associated with the presence of MR (P < .001). In addition, MR is associated with HM (P = .0022), FA (P = .0024), renal AMLs (P < .0001), and more than two renal cysts (P = .024) among these patients. When patients with and without FA were compared, FA was often significantly associated with HM (P = .038), ungual fibromas (P = .0016), shagreen patches (P = .0025), fibrous facial plaques (P = .0196), tubers (P = .0177), retinal phakomas (P = .0201), RA (P = .0103), and renal cysts (P = .0014). Patients with RA are more likely to have RC (P < .0001) and other tumors, including FA (P < .0001), FFP (P = .0001), RH (P = .0031), dental enamel pits (P = .0057), gingival fibromas (P = .0039) and nonrenal hamartomas (P = .0007), and brain-related findings, including SEN (P = .0009), MR (P < .0001), and LD (P = .0004). When analyzed for the presence of clusters of TSC features, no specific smaller clusters of major and minor diagnostic features can be identified. We conclude that the neurocutaneous features of TSC present together as part of the natural history of the disease.
In summary, the overall small mutation detection rate for patients with TSC with a definite diagnosis was 72% in our study. TSC-causing mutations were dispersed throughout the 61 coding exons of the TSC1 and TSC2 genes with no specific mutation hot spot. The two most common mutations identified were substitution mutations in R611 and an in-frame deletion of amino acid 1746-11 (HIKRLR), both in TSC2 and both nonprotein truncating. The proportion of TSC1 to TSC2 mutation is approximately one to one for TSC families with multiple affected individuals. In de novo cases, TSC1 mutation accounted for only 20% and TSC2 mutations accounted for 80%. Despite the highly variable expressivity of TSC phenotypes,37 our study indicated that male patients have more severe neurologic phenotypes than female patients. As other studies have shown, our study demonstrated that major diagnostic features, including facial angiofibromas, forehead plaques, SENs, renal AMLs and cysts, retinal phakomas, and MR, are significantly associated with mutations in the TSC2 gene. The trend holds true for familial cases with TSC2 mutations associated with a higher chance of having renal and retinal abnormalities.
References
Northrup H, Au KS . Tuberous sclerosis complex. GeneReviews at GeneTests: Medical Genetics Information Resource [database online http://www.genetests.org ]. Seattle, WA: University of Washington, 2005.
Roach ES, Gomez MR, Northrup H . Tuberous sclerosis complex consensus conference: revised clinical diagnostic criteria. J Child Neurol 1998; 13: 624–628.
Roach ES, Sparagana SP . Diagnosis of tuberous sclerosis complex. J Child Neurol 2004; 19( 9): 643–649.
The European Chromosome 16 Tuberous Sclerosis Consortium. Identification and characterization of the tuberous sclerosis gene on chromosome 16. Cell 1993; 75: 1305–1315.
Xu L, Sterner C, Maheshwar MM, Wilson PJ, et al. Alternative splicing of the tuberous sclerosis 2 (TSC2) gene in human and mouse tissues. Genomics 1995; 27: 475–480.
van Slegtenhorst M, de Hoogt R, Hermans C, Nellist M, et al. Identification of the tuberous sclerosis gene TSC1 on chromosome 9q34. Science 1997; 277: 805–808.
TSC variants database at http://chromium.liacs.nl/lovd/index.php?select_db=TSC1 and http://chromium.liacs.nl/lovd/index.php?select_db=TSC2. Curators: Povey S, Ekong R.
van Slegtenhorst M, Verhoef S, Tempelaars A, Bakker L, et al. Mutational spectrum of the TSC1 gene in a cohort of 225 tuberous sclerosis complex patients: no evidence for genotype-phenotype correlation. J Med Genet 1999; 36: 285–289.
Niida Y, Lawrence-Smith N, Banwell A, Hammer E, et al. Analysis of both TSC1 and TSC2 for germline mutations in 126 unrelated patients with tuberous sclerosis. Hum Mutat 1999; 14: 412–422.
Jones AC, Daniells CE, Snell RG, Tachataki M, et al. Molecular genetic and phenotypic analysis reveals differences between TSC1 and TSC2 associated familial and de novo tuberous sclerosis. Hum Mol Genet 1997; 6: 2155–2161.
Jones AC, Shyamsundar MM, Thomas MW, Maynard J, et al. Comprehensive mutation analysis of TSC1 and TSC2-and phenotypic correlations in 150 families with tuberous sclerosis. Am J Hum Genet 1999; 64: 1305–1315.
Lewis JC, Thomas HV, Murphy KC, Sampson JR . Genotype and psychological phenotype in tuberous sclerosis. J Med Genet 2004; 41: 203–207.
Dabora SL, Jozwiak S, Franz DN, Roberts PS, et al. Mutational analysis in a cohort of 224 tuberous sclerosis patients indicates increased severity of TSC2, compared with TSC1, disease in multiple organs. Am J Hum Genet 2001; 68: 64–80.
Sancak O, Nellist M, Goedbloed M, Elfferich P, et al. Mutational analysis of the TSC1 and TSC2 genes in a diagnostic setting: genotype-phenotype correlations and comparison of diagnostic DNA techniques in Tuberous Sclerosis Complex. Eur J Hum Genet 2005; 13( 6): 731–741.
Au KS, Rodriguez JA, Rodriguez E Jr, Dobyns JWB, et al. Mutations and polymorphisms in the tuberous sclerosis complex gene on chromosome 16. Hum Mutat 1997; 9( 1): 23–29.
Au KS, Rodriguez JA, Finch JL, Volcik KA, et al. Germ-line mutational analysis of the TSC2 gene in 90 tuberous-sclerosis patients. Am J Hum Genet 1998; 62( 2): 286–294.
Verhoef S, Bakker L, Tempelaars AM, Hesseling-Janssen AL, et al. High rate of mosaicism in tuberous sclerosis complex. Am J Hum Genet 1999; 64: 1632–1637.
Roberts PS, Dabora S, Thiele EA, Franz DN, et al. Somatic mosaicism is rare in unaffected parents of patients with de novo tuberous sclerosis. J Med Genet 2004; 41: e69.
Rose VM, Au KS, Pollom G, Roach ES, et al. Germ-line mosaicism in tuberous sclerosis: how common?. Am J Hum Genet 1999; 64( 4): 986–992.
Nellist M, Sancak O, Goedbloed MA, Rohe C, et al. Distinct effects of single amino-acid changes to tuberin on the function of the tuberin-hamartin complex. Eur J Hum Genet 2005; 13( 1): 59–68.
Nellist M, Verhaaf B, Goedbloed MA, Reuser AJ, et al. TSC2 missense mutations inhibit tuberin phosphorylation and prevent formation of the tuberin-hamartin complex. Hum Mol Genet 2001; 10: 2889–2898.
Maheshwar MM, Cheadle JP, Jones AC, Myring J, et al. The GAP-related domain of tuberin, the product of the TSC2 gene, is a target for missense mutations in tuberous sclerosis. Hum Mol Genet 1997; 6: 1991–1996.
Langkau N, Martin N, Brandt R, Zugge K, et al. TSC1 and TSC2 mutations in tuberous sclerosis, the associated phenotypes and a model to explain observed TSC1/ TSC2 frequency ratios. Eur J Pediatr 2002; 161: 393–402.
Yeung RS . Multiple roles of the tuberous sclerosis complex genes. Genes Chromosomes Cancer 2003; 38( 4): 368–375.
Au KS, Williams AT, Gambello MJ, Northrup H . Molecular genetic basis of tuberous sclerosis complex: from bench to bedside. J Child Neurol 2004; 19( 9): 699–709.
Jozwiak J, Jozwiak S, Grzela T, Lazarczyk M . Positive and negative regulation of TSC2 activity and its effects on downstream effectors of the mTOR pathway. Neuromolecular Med 2005; 7( 4): 287–296.
Gould SR . Hamartomatous rectal polyps are common in tuberous sclerosis. Ann N Y Acad Sci 1991; 615: 71–80.
Soucek T, Yeung RS, Hengstschlager M . Inactivation of the cyclin-dependent kinase inhibitor p27 upon loss of the tuberous sclerosis complex gene-2. Proc Natl Acad Sci U S A 1998; 95: 15653–15658.
Nguyen L, Besson A, Heng JI, Schuurmans C, et al. p27kip1 independently promotes neuronal differentiation and migration in the cerebral cortex. Genes Dev 2006; 20( 11): 1511–1524.
Prather P, de Vries PJ . Behavioral and cognitive aspects of tuberous sclerosis complex. J Child Neurol 2004; 19( 9): 666–674.
Smalley SL, Tanguay PE, Smith M, Gutierrez G . Autism and tuberous sclerosis. J Autism Dev Disord 1992; 22: 339–355.
Kwiatkowski DJ, Zhang H, Bandura JL, Heiberger KM, et al. A mouse model of TSC1 reveals sex-dependent lethality from liver hemangiomas, and up-regulation of p70S6 kinase activity in TSC1 null cells. Hum Mol Genet 2002; 11: 525–534.
Yu J, Astrinidis A, Howard S, Henske EP . Estradiol and tamoxifen stimulate lymphangiomyomatosis-associated angiomyolipoma cell growth and activate both genomic and non-genomic signaling pathways. Am J Physiol Lung Cell Mol Physiol 2004; 286( 4): L694–L700.
DiMario FJ, Dianna D, Leopold H, Chameides L . Evolution of cardiac rhabdomyoma in tuberous sclerosis complex. Clin Pediatr 1996; 35: 615–619.
Shepherd CW, Gomez MR . Mortality in the Mayo Clinic Tuberous Sclerosis Complex Study. Ann N Y Acad Sci 1991; 615: 375–377.
O'Callaghan FJ, Noakes M, Osborne JP . Renal angiomyolipomata and learning difficulty in tuberous sclerosis complex. J Med Genet 2000; 37: 156–157.
Northrup H, Wheless JW, Bertin TK, Lewis RA . Variability of expression in tuberous sclerosis. J Med Genet 1993; 30: 41–43.
Acknowledgements
This research was funded by generous support from the Tuberous Sclerosis Alliance with grants to H. N. and K. S. A., the Treasure Street of the Texas Scottish Rite Hospital, and the National Institute of Neurological Disorders and Stroke (National Institutes of Health) grant NS32300-02 to H. N. We thank the many wonderful families affected by tuberous sclerosis who participated in this research because it would not have been possible without their help.
Author information
Authors and Affiliations
Corresponding author
Additional information
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Au, K., Williams, A., Roach, E. et al. Genotype/phenotype correlation in 325 individuals referred for a diagnosis of tuberous sclerosis complex in the United States. Genet Med 9, 88–100 (2007). https://doi.org/10.1097/GIM.0b013e31803068c7
Received:
Accepted:
Issue Date:
DOI: https://doi.org/10.1097/GIM.0b013e31803068c7
Keywords
This article is cited by
-
Tsc2 mutation rather than Tsc1 mutation dominantly causes a social deficit in a mouse model of tuberous sclerosis complex
Human Genomics (2023)
-
Neurofibromatosis type1, type 2, tuberous sclerosis and Von Hippel-Lindau disease
Child's Nervous System (2023)
-
Treatment of Pediatric Low-Grade Gliomas
Current Neurology and Neuroscience Reports (2023)
-
Comment on Balsamo et al.: Birt-Hogg-Dubé syndrome with simultaneous hyperplastic polyposis of the gastrointestinal tract: case report and review of the literature
BMC Medical Genomics (2022)
-
Renal phenotypes correlate with genotypes in unrelated individuals with tuberous sclerosis complex in China
Orphanet Journal of Rare Diseases (2022)