Abstract
Purpose: There is considerable information regarding the medical and cognitive aspects of Klinefelter syndrome yet little research regarding its psychosocial impact. This study investigates the personal impact of Klinefelter syndrome and the influence of age at diagnosis, clinical, social, and demographic factors on adult quality of life outcomes.
Methods: Men from across Australia, diagnosed with KS at different ages, were recruited through multiple sources. Participants completed a questionnaire assessing subjective well-being, body image, self-esteem, mental health, social support, and general health.
Results: Eighty-seven individuals self-completed the questionnaire. All outcomes were much poorer for the study population than for the general male population. Individuals diagnosed later in life reported many of the same symptoms as those diagnosed at younger ages. Employment status, social support, and phenotypic features were the strongest predictors of psychosocial outcomes. Age at diagnosis was not as influential because it did not correlate with phenotypic severity score.
Conclusion: This is the first quantitative study to show Klinefelter syndrome has a significant personal impact. Men diagnosed with Klinefelter syndrome later in life reported similar difficulties as those at younger ages, suggesting that they would benefit from early detection and intervention. Understanding factors influencing this can assist in providing adequate services to individuals with Klinefelter syndrome, their partners, families, and the health professionals caring for them.
Similar content being viewed by others
Main
Sometimes called “the forgotten syndrome,” Klinefelter syndrome (KS) remains a common yet underdiagnosed genetic condition, despite being first described almost 7 decades ago.1 Caused by an additional X chromosome in males (47XXY), the resulting phenotype is often highly variable between individuals and not always explicit in its clinical manifestation.2 Features of the condition almost always include testicular dysfunction leading to azoospermia and testosterone deficiency from puberty3; commonly include gynecomastia, decreased facial, body and pubic hair4; and can encompass a range of cognitive, speech, learning, and behavioral difficulties that may or may not be obvious from early childhood.5–8
The most recent studies estimate the live birth prevalence of KS at 1 in 4509 to 1 in 66010 males, with 50–70% cases remaining undiagnosed. For those who are diagnosed, postnatal detection most often occurs in the context of fertility investigations during the reproductive years.10,11 There is speculation as to whether undiagnosed men with KS experience difficulties associated with the condition that could be alleviated with treatment or are not detected because they in fact experience no related problems. Another possibility is that, these men are not detected through infertility investigations because they are not forming stable partnerships. This may be due to the less recognizable consequences of testosterone deficiency such as fatigue, low libido, poor concentration, and depression,12 in addition to currently poorly quantified psychosocial effects of the condition.
There is a growing body of research on the cognitive and neuropsychological profile of KS,2,7,13 including characterization of the specific deficits in comprehension, memory, language processing, and executive functioning that may contribute to these aspects of the condition.14–17 Speech, physical, educational, and other interventions are available for assisting with difficulties during the childhood years that may improve later outcomes.6,18,19 The personality and behavior of boys with KS has been described as shy, reserved, sensitive, and passive in childhood,20–22 which together with unattended learning difficulties may lead to secondary adaptation and behavioral problems in adolescence.23 Testosterone treatment from puberty may assist in psychosocial adaption during adolescence.24,25 For adults with KS, there is very little research regarding the personal impact of being diagnosed and living with KS.26,27 In addition, it remains to be elucidated as to how adult quality of life may be modified by age at diagnosis and whether earlier diagnosis and intervention results in better life outcomes in adulthood.
Despite the need for further research exemplifying that early intervention leads to better outcomes, earlier diagnosis has long been advocated,28,29 so that timely treatment and intervention can be implemented to ensure that each individual with KS reaches their potential. Population-based genetic screening is one means of achieving this but requires careful consideration of both the risks and benefits of diagnosis at different ages.30 This study aims to examine the psychosocial impact of being diagnosed with and living with KS. It explores the influence of age at diagnosis and other factors that may influence adult quality of life, including phenotypic severity, and treatments and interventions received.
SUBJECTS AND METHODS
Ethics approval
The study received ethics approval from the Southern Health Human Research and Ethics Committee and Monash University, Melbourne, Australia. All participants provided written informed consent for participating in the study, including permission to obtain a copy of their karyotype results from their doctor or testing laboratory.
Recruitment
Any Australian citizen aged 18 years and older, diagnosed with KS at any age (including prenatally), was eligible to participate. Inclusion criteria were a karyotype including more than one X chromosome and a single Y chromosome, excluding mosaics with a female cell line (e.g., 46,XX/47,XXY). Men with a 46,XX karyotype including a sex-determining region Y (SRY) gene were eligible as they were considered phenotypically similar enough to KS to experience comparable psychosocial issues. Initial study information was distributed to individuals who had been diagnosed with KS by health professionals, medical and hospital clinics, support organizations, other men's information groups, and through word of mouth. Individuals interested in participating could then provide their details to the research team by post, e-mail, phone, or fax. Multiple sources were used for distributing study information with the goal of obtaining a population-based sample. Participants were recruited between November 2008 and December 2009.
Data collection
After registering an interest in the study, individuals were sent a participant kit containing a questionnaire, an Oragene® DNA Self-Collection Kit for obtaining a saliva sample (optional), and consent forms. The completed questionnaire was returned with the saliva sample (if provided), and the participant was asked to indicate willingness to be involved in a future, separate, qualitative interview-based study. A reminder notice was sent or follow-up phone call made at 4 weeks after expected receipt of the participant kit. Individual karyotypes were confirmed with laboratory test results where available. Only the results from the questionnaire component of the study will be presented in this study. Results from the qualitative study undertaken as part of this project are currently in preparation.
Questionnaire
A comprehensive self-administered questionnaire was developed to assess key psychosocial areas that may be affected by symptoms of KS and contribute to adult quality of life. A number of validated measures were used to assess key domains and where possible, those for which Australian population normative data were available were selected (Table 1). The primary outcome measure was subjective well-being, as measured by the Personal Wellbeing Index (PWI).31 Individual and family sociodemographic information and details of diagnosis, specific for this study, were collected. The latter included age at diagnosis, age at which the participant was informed of the diagnosis and who the informant was, and the clinical indication that led to testing. In addition, participants were asked a series of questions regarding symptoms of KS they had experienced; what (if any) treatment had been received for this; and how much this symptom had concerned them on a 5-point response scale (ranging from “not at all” to “an extreme amount”). Another section, also designed specifically for this study, inquired about attitudes and opinions regarding KS diagnosis and impact on various aspects of life (e.g., family relationships, growing up, and stigmatization). Attitudes toward population-based genetic screening for KS were determined using a combination of multiple choice and open-ended questions but are not presented in this article.
Composite scores
Participant answers regarding symptoms of KS, treatments received for each symptom, and levels of concern about each symptom were used to create three separate composite scores. Symptoms were classified as either “primary” or “secondary” features of KS based on preliminary discussion with individuals with KS, clinicians with experience in KS (both pediatric and adult), and themes obtained from informal focus groups previously conducted by the Genetic Support Network of Victoria.
Symptoms considered as primary features of KS were those likely to have a strong psychosocial component: testosterone deficiency; breast development; infertility; physical development; and learning, behavioral, and communication difficulties. Secondary features were defined as health issues for which individuals with KS are at increased risk (although less common than primary features), which also affect the general population and may not have the same psychosocial impact as primary features. These included puberty (recalled commencement at a different time to peers); undescended testes; osteoporosis; diabetes; varicose veins; heart problems; thyroid disorders; cancer (of any type); other medical conditions; and psychiatric disorders. Psychiatric disorders (e.g., bipolar) were included as a secondary feature because all participants who had been diagnosed with a psychiatric disorder had also experienced common mental health issues such as depression, anxiety, or anger problems, and these were included under the primary feature of behavioral difficulties.
To create a composite score for the domain of phenotype, each primary feature listed by the participant was assigned a value of two and each secondary feature a value of one. For the domain of treatment of symptoms, a value of one was given for each feature for which treatment was received. For concern about symptoms, the level of concern about each primary feature was given a value between 0 “not at all concerned” and 4 “extremely concerned” (levels of concern were not ascertained for secondary features). In this way, three separate composite scores were calculated as estimations of phenotype, treatment, and concern. The “phenotypic severity score” was created by summing the primary (a possible maximum of seven items each scored 2) and secondary features (possible maximum of 10 items each scored 1) present, divided by the number of questions answered, and converted to a percent. This score was used as a proxy for phenotypic severity. The scores for each treatment received for primary and secondary characteristic (excluding puberty, total 16 items) were summed, divided by the number of questions answered (due to missing data), and converted to a percent to provide a “treatment score.” Scores for levels of concern (ascertained only for primary features with a possible total of seven items) were summed, divided by the number of questions answered, and converted to a percent to give a “concern score.”
The nine-item adapted Quality of Relationships Inventory (social support measure, Table 1) was repeated for mother, father, friends, and partner and a mean score obtained for each of these relationships. To obtain a general measure of social support, the mean of all four scores was calculated. For participants who did not have that person in their life (e.g., no partner and mother had passed away), a score of 0 was assigned for that relationship. Therefore, the final mean obtained is only a general indicator of current level of social support and does not apply to past relationships (although it may also be reflective of these).
Data analysis
All data were analyzed using Stata Statistical Software, Release 11.0 (College Station, TX: StataCorp LP, 2009). Scores for the validated measures listed in Table 1 were calculated according to manual instructions. Unless otherwise specified in the manual, mean replacement was used for all calculations if individual missing data were <10%, otherwise the case was excluded from that analysis.
Age at diagnosis was chosen as the primary grouping category for comparison of participant outcomes based on the original hypothesis of the study: “earlier age at diagnosis allows for timely intervention resulting in better outcomes in adulthood.” The age at diagnosis variable was categorized as there was a nonlinear relationship with the main outcome variable, subjective well-being (PWI). The age range for each age at diagnosis category was determined, taking into consideration the distribution of participants across each category, in addition to the likely clinical indication leading to diagnosis within each group (e.g., fertility investigations in those diagnosed between 25 and 39 years). The characteristics and outcomes of the study population were compared across age at diagnosis groups, using χ2 test for heterogeneity for categorical variables and the t test or one-way analysis of variance for continuous variables. For the analysis of variances, posthoc pairwise comparisons between age at diagnosis groups were examined using the Sidak test. Bivariable linear regression was used to explore associations of the outcome variables: subjective well-being (PWI); body image (Multidimensional Body-Self Relations Questionnaire Appearance Evaluation Subscale); self-esteem (Rosenberg Self-Esteem Scale); and psychological distress (K10); with age at diagnosis; individual and family sociodemographic characteristics; and phenotypic severity, treatment, and concern composite scores. Covariates associated with each outcome (P < 0.10) in bivariable analysis were included in a multivariable linear regression model.
RESULTS
Recruitment
Because of the anonymous nature of the initial recruitment step, it was not possible to determine the proportion of individuals with KS from across Australia who were informed of the study and then proceeded to register an interest to participate. However, 114 individuals registered interest and were sent a participant kit. Eighty-seven (76.3%) returned the completed questionnaire with consent forms: of which 79 (90.8%) provided a saliva sample and 77 (88.5%) indicated a willingness to partake in an interview at a future date (results not presented in this article).
Participants resided in all states and territories across Australia: 28% Victoria; 22% New South Wales; 16% Queensland; 9% South Australia; 8% Australian Capital Territory; 7% Western Australia; 2% Tasmania; and one participant resided overseas. Individuals with KS reported receiving information about the study from a wide range of sources including endocrinologists (33%); general or other health practitioners (25%); genetics services (16%); internet or general media (13%); hospital clinics (8%); family member or friend (8%); support groups (6%); or their partner's gynecologist (5%). Approximately 10% of participants received study information from more than one source and up to four sources.
Participant characteristics
The mean age of participants was 43 years and ranged from 19 to 76 years. Mean age did not vary significantly across the participant characteristics listed in Table 2, other than for time since diagnosis.
Associations with age at diagnosis
Mean age at diagnosis was calculated according to categories of various social, demographic, and other characteristics. The following variables were associated with age at diagnosis: age at study (F = 16.4, P < 0.001), time since diagnosis (F = 13.1, P < 0.001), relationship status (t = −2.0, P = 0.05), and karyotype (F = 2.7, P = 0.05). Participants who were currently partnered had a mean age at diagnosis of 28 years, compared with a mean age at diagnosis of 22 years for unpartnered participants. Mean age at diagnosis varied significantly between the different karyotypes: 26 years for 47,XXY; 36 years for 46,XY/47,XXY; 16 years for 46,XX men; and 19 years for those with an unconfirmed karyotype. The 46,XX men tended to be diagnosed earlier than those with a 47,XXY or mosaic karyotype; however, there were only two people in this group. Those with an unconfirmed karyotype also tended to have a younger age at diagnosis, but this was because many of these tests had been conducted so long ago that the results were no longer available, not necessarily because they had more symptoms leading to an earlier diagnosis. Posthoc analysis by Sidak test demonstrated the main differences in age at diagnosis across karyotype groups to lie between the mosaic group and the unconfirmed group (P = 0.07). A sensitivity analysis including and excluding karyotypes other than 47,XXY in bivariable analyses did not indicate any effect on the results, and therefore, all karyotypes were used as a single group.
There was a tendency for those diagnosed later in life to have completed a higher level of education (did not complete high school, 26 years; completed high school, 25 years; and further than high school, 32 years) and to be in a higher income bracket (less than AUS$30,000, 22 years; AUS$30,000 to AUS$69,999, 26 years; and AUS$70,000 and above, 30 years). In Australia, completion of high school refers to 12 years of education, usually completed at approximately 18 years of age. When asked about sexual preference, 84% of participants indicated heterosexual, 11% homosexual or bisexual, and 5% specified other (including asexual). The clinical indication for karyotyping leading to diagnosis was developmental delay or learning and behavioral difficulties (16%), physical or hormonal features (49%), fertility investigations (30%), or incidental finding (5%), with mean ages at diagnosis of 9, 28, 31, and 11 years, respectively.
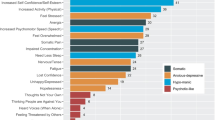
Phenotypic features, treatment, and levels of concern
Primary phenotypic features associated with KS, treatment received, and level of concern, reported by participants, were compared across age at diagnosis groups (Table 3). More than 90% of participants across all age at diagnosis groups reported being diagnosed with testosterone deficiency, and almost all had received testosterone treatment. Approximately half of participants had experienced breast development, although only some had received treatment (e.g., surgery) for this. For primary characteristics of KS involving development (i.e., learning, behavioral, communication, and physical difficulties), those diagnosed between 0 and 14 years experienced these the most. However, a notable proportion of the later diagnosed groups also reported difficulties with these characteristics while growing up. The 0–14-year age at diagnosis group received the most treatment for these features. Treatment levels for learning and communication difficulties were significantly lower in those diagnosed at later ages (P = 0.018 and P = 0.047, respectively). Almost all participants felt concerned about the phenotypic features they reported experiencing, in addition to a small number who felt concerned about a feature even if they had not experienced it.
Approximately half of participants reported commencing puberty at a different time to their peers (earlier or later) across the age at diagnosis groups, and similar proportions were concerned about their pubertal development. Forty-two percent of participants had accessed assisted reproductive technology, and 67% of these had one or more children resulting from the treatment, usually through donor sperm, with a large proportion being concerned about this aspect of the condition. When asked about how masculine or feminine they felt and looked, approximately three quarters of participants diagnosed in the 15–24-year age group reported the highest levels of masculinity, whereas the small number of participants who reported feeling and/or looking feminine were diagnosed beyond the age of 40 years.
The proportion of participants who experienced (and were treated for) secondary characteristics of KS is not presented in Table 3. The secondary characteristics experienced were psychiatric disorders 44% (38% treated), undescended testes 28% (9% treated), osteoporosis 23% (20% treated), heart problems 17% (13% treated), varicose veins 15% (3% treated), diabetes 10% (10% treated), cancer 9% (9% treated), and thyroid disease 5% (1% treated). Although there were no significant differences across age at diagnosis groups for any of these secondary features (data not shown), undescended testes were least prevalent in those diagnosed beyond the age of 40 years (8% vs. 31%), and osteoporosis and varicose veins were most frequent in this group (50% vs. 18% and 33% vs. 8%, respectively).
Phenotypic severity, treatment, and concern composite scores
Means of the composite scores for phenotypic features, treatment, and concern are listed in Table 4. No significant differences in mean scores were observed across age at diagnosis groups; however, a tendency for concern levels to increase with older age at diagnosis was observed.
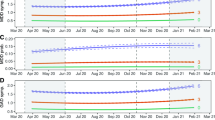
Psychosocial outcomes
Mean scores of measures of psychosocial well-being by age at diagnosis are presented in Table 5. The KS study population means were significantly poorer for all psychosocial outcomes measured, when compared with population normative data (P < 0.001). Means for all measures were compared across age at diagnosis groups (data not shown). Subjective well-being means were significantly different by age at diagnosis groups (F = 3.44, P = 0.02), with those diagnosed youngest showing lowest scores (48.8) and those diagnosed between 25 and 39 having highest scores (68.9). There was no significant difference for body image, self-esteem, or psychological distress, when compared across age at diagnosis groups.
Factors predicting psychosocial outcomes
Multiple linear regression was used to explore the contribution of a range of clinical, social, and demographic variables to the psychosocial domains explored. The results of the regression analyses are presented in Table 6. Only paternal education level was included in the analysis as maternal education level was highly correlated with this (r = 0.5, P < 0.001). Income was not included because it was highly correlated with employment status (r = 0.4, P < 0.001), which was more strongly associated with the outcomes. Karyotype, participant education level, and concern composite score were included in the initial bivariable analysis, however, were not associated with any of the outcomes and so were excluded from the final models. Regression analysis for the Appearance Orientation Subscale (Body Image) is not presented as it was not associated with any of the covariates studied.
Employment status, social support (Quality of Relationships Inventory), and phenotypic severity score showed the strongest association with subjective well-being, with scores increasing with active employment and more social support and decreasing with higher phenotypic severity scores. There was a trend for those diagnosed in the 25–29-year age group to have higher subjective well-being scores than those diagnosed between 0 and 14 years and for those whose fathers had completed education beyond the high school level, compared with those whose fathers had not completed high school.
The only factor strongly associated with body image (Multidimensional Body-Self Relations Questionnaire, Appearance Evaluation subscale) was phenotypic severity score, with feelings of attractiveness decreasing with higher scores. Self-esteem (Rosenberg Self-Esteem Scale) increased with level of social support and decreased with higher phenotypic severity scores. Psychological distress (K10) increased as phenotypic severity score increased but was lower in those employed, studying, or retired (active). Additionally, those with higher levels of social support showed less psychological distress, as did those whose fathers had completed education beyond that high school level.
DISCUSSION
This study provides the first quantitative evidence for a significant psychosocial impact of KS, as reported by adult individuals with KS representing the phenotypic and diagnostic spectrum of the condition. In a population-based sample of 87 men with KS, quality of life outcomes were noticeably poorer than the general male population for all domains evaluated, including subjective well-being, self-esteem, body image, mental health, and general health. The most consistent factor influencing these decreases in psychosocial health was phenotypic severity score.
It is often thought that individuals diagnosed early in life represent the more “severe” end of the phenotypic spectrum of KS and that those diagnosed during their reproductive years represent a “milder” phenotype. We found that age at diagnosis was not a major predictor of psychosocial outcomes in adulthood, as many of the phenotypic characteristics of KS thought to be more frequent in younger diagnosed individuals (e.g., learning and behavioral difficulties) were equally prevalent in participants diagnosed later in life. This challenges the commonly held belief that those diagnosed at older ages do not experience the symptoms of KS that often lead to a diagnosis earlier in life, such as learning, physical, or behavioral difficulties.45 This also suggests that presentation with typical symptoms of KS will not always lead to a timely diagnosis.
Across all age at diagnosis groups, a large proportion of participants reported experiencing features considered to be common features of KS. Interestingly, a higher proportion of those diagnosed in the 25–39-year age group reported having breast development than those diagnosed at younger ages. This may be the result of delayed testosterone treatment, which when given at the right time may prevent or reduce the development of breast tissue.46 Those diagnosed during the prepubescent years received more treatment than those diagnosed later in life, as would be expected, although our study did not measure the success or outcomes of such treatments or interventions, which may have a major influence on quality of life in adulthood. This is of particular concern when considering important developmental aspects of KS such as learning difficulties, which was experienced by the majority of participants regardless of age at diagnosis, but for which those diagnosed during or beyond adolescence were significantly less likely to have received treatment.
A large proportion of participants across all age at diagnosis groups reported that puberty commenced at a time later than their peers. Studies of puberty in adolescent boys with KS have shown that commencement is usually at the same times as peers.3 However, “progress” of puberty may not be as complete as peers (e.g., less hair and muscle development), and as such individuals with KS may perceive the timing as different. This is an interesting consideration in trying to elucidate psychosocial aspects of KS. Perceived pubertal timing is an influential factor in adolescent behavior, and earlier or later perceived timing has been linked to delinquency and other problematic behavior in adolescents.47 Implementation of testosterone treatment early in puberty for boys with KS has been proposed to ensure full virilization,46 even if testosterone levels are not yet low, as testosterone levels alone may not be the most accurate indicator of hypogonadism.48 Our findings support this recommendation, and a more normal pubertal development may reduce secondary behavioral problems from developing. Those diagnosed in the earlier two age groups were more likely to report experiencing puberty earlier than their peers. This could be an indication of implementation of testosterone treatment commencing early in puberty.
More than half of participants across all age groups reported feeling and looking masculine. A noticeable proportion, however, reported feeling and looking neither masculine nor feminine. Interestingly, a small number of those diagnosed later in life reported feeling and/or looking feminine. Given the role of testosterone in ensuring full development of muscle tone and body hair, these reports among older participants may reflect the impact of years of testosterone deficiency on their bodies and sense of gender identity. There may also have been issues around gender identity resulting from interpretation of genetic results (i.e., X chromosomes are often explained as the “female chromosome”). It is important to consider the impact of simplifying genetic information when explaining diagnosis of a sex chromosome abnormality such as KS. Development of methods for explaining the genetic basis of conditions involving the sex chromosomes that do not involve social concepts of gender and sexuality may be helpful for individuals with KS and their families.
When asked about sexual preference, the majority of participants indicated a preference for heterosexual relations, whereas 11% indicated same-sex attraction. Some older studies suggested a higher prevalence of homosexuality among individuals with KS,49 and this can be a concern for parents of a diagnosed boy.50 However, given the difficulties in measuring sexual preference at different times and in different cultures,51 the findings from this study do not indicate a deviation from the general population frequencies. In 2006, a large Australian study found 2–3% Australians identified as homosexual, whereas 20% reported having same-sex attractions.52
Composite scores were used in this study as an approximation of phenotypic severity, treatment, and levels of concern. It was expected that all scores would be highest in the youngest diagnosed group and lowest in those diagnosed late in life. Surprisingly, there were no significant differences in any of the three mean scores across age at diagnosis groups.
Although not significant, there was a small but consistent increase in concern levels with increasing age at diagnosis. This may suggest that the later in life an individual was diagnosed, the more they worried about the features of KS assessed in this study. Concern may increase over time because the symptoms exist, but there is a lack of explanation for them. Without diagnosis, treatment and understanding are less likely to be obtained, both of which can be important tools for ensuring the individual has the support needed to reach his potential.52 Men diagnosed beyond their mid-20s may represent those on a “diagnostic odyssey” albeit an unknown one. Another explanation is that later age at diagnosis allows for introspection and reflection, and it may be easier to identify concerns in retrospect, whereas the younger diagnosed group did not have this possibility. Those diagnosed early in life may indeed develop better coping mechanisms or different expectations (including those of their parents), or simply have more opportunity to integrate this knowledge into their developing self-identity (i.e., they are just more “used to it”). A final possible explanation is that, if those diagnosed at younger ages do in fact have more difficulties with behavior, learning, communication, or social processing, they may not be as aware of possible differences or problems as their later diagnosed counterparts, who may have more cognitive ability (not just time) to reflect and identify issues in their past.
It is not surprising that psychosocial outcomes were poorer for study participants, when compared with population norms, given the range of medical, cognitive, and psychological factors present with KS that may impact on these. Nonetheless, this finding is of considerable importance, as this is the first study to provide rigorous evidence of these aspects of KS in a population-based sample of individuals. With the exception of subjective well-being, no significant differences were observed in mean scores for the psychosocial measures used in this study across age at diagnosis groups.
The factors most influencing psychosocial outcomes were phenotypic severity score, employment status, and current level of social support. Phenotypic severity score remained a significant predictor of all outcomes, even after adjusting for treatment. This suggests that prevention (or amelioration) of KS symptoms, where possible, may be the best form of treatment. Early interventions for speech, motor, and learning difficulties associated with KS have been suggested even before such issues manifest explicitly,8 and our data support this. Interestingly, paternal education level had a significant impact on both subjective well-being (increasing with higher education level of father) and psychological distress (decreasing with higher education level of father). Previous studies have reported the concern of fathers whose children have been diagnosed with KS, worried about homosexuality, or femaleness of their son.49 Those with a lower education level may not have the resources to understand the genetic diagnosis as well as those with higher education levels.54 As discussed earlier with respect to gender identity, it is essential that accurate resources for understanding KS are available to individuals and families and that genetic counseling is accessed wherever possible.
Further evidence for effective interventions for KS may be best taken from studies of specific aspects of similar conditions, for example, the effectiveness of educational interventions for children with learning disabilities. Qualitative studies would also provide valuable insight into the experiences of individuals, and both the perceived and actual risks and benefits of diagnosis at different ages, including the modifying effects of environmental factors such as peer support and family functioning, and access to services and care.
Strengths and limitations
A major strength of this study is the population-based sample of participants. Recruitment through multiple sources, rather than a single clinic or support group, provided a sample of individuals from wide range of ages and socioeconomic backgrounds. This included participants receiving distinctly different levels of medical care, ranging from general to specialist, and including those not receiving active care at all. Only a small proportion of participants was recruited through a support group, providing a more representative population than studies where participants have been recruited through support groups alone. Almost all study participants were from a white background and, therefore, represent only one part of the general population. However, this allowed analysis to focus on other differences, without the added factor of cultural differences.
Nonetheless, this study only represents those men who have been diagnosed, the majority of whom were diagnosed as adults. Originally, we aimed to recruit a prenatally diagnosed subcohort to act as a reference group for comparisons. Unfortunately, because of ethical issues associated with contacting this group, it was not possible to conduct targeted recruitment for this small number of possible participants. As this was a written questionnaire, only those able to read, write, and comprehend to the level of the questionnaire were able to complete it. Telephone assistance was offered; however, only one participant took up this offer. Partners or parents may have also assisted in completing the questionnaire in some cases, but we were not privy to this information.
As this study aimed to address the psychosocial impact of KS, it was important to capture perceived symptomatology, together with levels of concern. Health issues assessed were general and self-reported, and so composite scores provided an approximation of phenotypic severity and treatment only; no clinical or biochemical measurements were taken for this study. Currently, no validated measure for quantitative assessment of KS phenotype exists. Although measures of this type are inevitably complex, and require careful and rigorous development, given the variability in clinical presentation of KS, such a tool would be invaluable for both research and clinical practice.
Although the measures designed for and used in this questionnaire provided a useful overview of the physical and psychosocial aspects of KS, more extensive development of these measures are needed to provide a level of information necessary to meaningfully assess such complex matters. For example, sexual function became apparent as an important issue for many participants, although this was not an area specifically covered in the questionnaire. Therefore, it would be useful to add a component inquiring about this to any future assessment tool. A combination of clinical, biochemical, and self-reported measures would provide the most comprehensive picture.
We were unable to confirm the karyotypes of a small proportion of participants as the test results were no longer held by the laboratory because of the length of time since diagnosis. However, the frequency of different KS karyotypes among study participants was similar to that found in prevalence studies.9 Assuming this is the only reason for a younger mean age at diagnosis for this group, it is expected that the distribution of karyotypes in this group would be similar to those whose karyotypes were confirmed. This idea was supported by analysis of the unconfirmed group compared with the confirmed 47,XXY group, for which the findings were very similar.
CONCLUSION
The findings from this study provide evidence for a negative psychosocial impact of KS and insight into some of the factors influencing this impact. Age at diagnosis is not necessarily an indicator of where an individual sits on the phenotypic spectrum of KS. Men diagnosed later in life report experiencing many of the same symptoms thought only to affect those diagnosed in childhood, suggesting all is “not well” as is often assumed. In fact, diagnosis of KS may be predominantly dependent on the health behavior of the parents or awareness of KS of the caring physician. This provides evidence for benefit of early diagnosis, which might only be achieved through population-based genetic screening of boys before puberty. Development of a validated measure for assessing phenotypic features and severity of KS is necessary, and clear identification of appropriate interventions and treatments for each biomedical and psychosocial aspect (in the form of guidelines) should be developed. Consistent and useful information for health professionals (doctors, allied health), family and partners, and community (e.g., teachers) would be beneficial to all parties.
References
Klinefelter H, Reifenstein E, Albright F . Syndrome characterized by gynecomastia, aspermatogenesis without a-leydigsm and increased secretion of follicle-stimulating hormone. J Clin Endocr Metab 1942; 2: 8.
Simpson JL, De La Cruz F, Swerdloff RS, et al. Klinefelter syndrome: expanding the phenotype and identifying new research directions. Genet Med 2003; 5: 460–468.
Salbenblatt JA, Bender BG, Puck MH, Robinson A, Faiman C, Winter JS . Pituitary-gonadal function in Klinefelter syndrome before and during puberty. Pediatr Res 1985; 19: 82–86.
Smyth CM, Bremner WJ . Klinefelter syndrome. Arch Intern Med 1998; 158: 1309–1314.
Ratcliffe S . Long-term outcome in children of sex chromosome abnormalities. Arch Dis Child 1999; 80: 192–195.
Rovet J, Netley C, Keenan M, Bailey J, Stewart D . The psychoeducational profile of boys with Klinefelter syndrome. J Learn Disabil 1996; 29: 180–196.
Leggett V, Jacobs P, Nation K, Scerif G, Bishop DV . Neurocognitive outcomes of individuals with a sex chromosome trisomy: XXX, XYY, or XXY: a systematic review. Dev Med Child Neurol 2010; 52: 119–129.
Samango-Sprouse C . Mental development in polysomy X Klinefelter syndrome (47,XXY; 48,XXXY): effects of incomplete X inactivation. Semin Reprod Med 2001; 19: 193–202.
Herlihy AS, Halliday JL, Cock ML, McLachlan RI . The prevalence and diagnosis rates of Klinefelter syndrome: An Australian comparison. Med J Aust 2011; 191: 24–28.
Bojesen A, Juul S, Gravholt CH . Prenatal and postnatal prevalence of Klinefelter syndrome: a national registry study. J Clin Endocr Metab 2003; 88: 622–626.
Abramsky L, Chapple J . 47,XXY (Klinefelter syndrome) and 47,XYY: estimated rates of and indication for postnatal diagnosis with implications for prenatal counselling [see comment]. Prenat Diagn 1997; 17: 363–368.
Nielsen J, Pelsen B, Sorensen K . Follow-up of 30 Klinefelter males treated with testosterone. Clin Genet 1988; 33: 262–269.
Bishop DV, Jacobs PA, Lachlan K, et al. Autism, language and communication in children with sex chromosome trisomies [published online ahead of print July 23, 2010]. Arch Dis Child doi: 10.1136/adc.2009.179747.
Fales CL, Knowlton BJ, Holyoak KJ, Geschwind DH, Swerdloff RS, Gaw Gonzalo I . Working memory and relational reasoning in Klinefelter syndrome. J Int Neuropsychol Soc 2003; 9: 839–846.
van Rijn S, Swaab H, Aleman A, Kahn RS . X Chromosomal effects on social cognitive processing and emotion regulation: a study with Klinefelter men (47,XXY). Schizophr Res 2006; 84: 194–203.
Van Rijn S, Aleman A, De Sonneville L, Swaab H . Cognitive mechanisms underlying disorganization of thought in a genetic syndrome (47,XXY). Schizophr Res 2009; 112: 91–98.
Verri A, Cremante A, Clerici F, Destefani V, Radicioni A . Klinefelter's syndrome and psychoneurologic function. Mol Hum Reprod 2010; 16: 425–433.
Samango-Sprouse C, Rogol A . XXY: the hidden disability and a prototype for an infantile presentation of developmental dyspraxia (IDD). Infants Young Child 2002; 15: 11–18.
Graham JM Jr, Bashir AS, Stark RE, Silbert A, Walzer S . Oral and written language abilities of XXY boys: implications for anticipatory guidance. Pediatrics 1988; 81: 795–806.
Bancroft J, Axworthy D, Ratcliffe S . The personality and psycho-sexual development of boys with 47 XXY chromosome constitution. J Child Psychol Psychiatry 1982; 23: 169–180.
Mandoki MW, Sumner GS, Hoffman RP, Riconda DL . A review of Klinefelter's syndrome in children and adolescents. J Am Acad Child Adolesc Psychiatry 1991; 30: 167–172.
Sorensen K . Physical and mental development of adolescent males with Klinefelter syndrome. Horm Res 1992; 37( suppl 3): 55–61.
Ross JL, Roeltgen DP, Stefanatos G, et al. Cognitive and motor development during childhood in boys with Klinefelter syndrome. Am J Med Genet A 2008; 146A: 708–719.
Simm PJ, Zacharin MR . The psychosocial impact of Klinefelter syndrome—a 10 year review. J Pediatr Endocrinol Metab 2006; 19: 499–505.
Maggi M, Schulman C, Quinton R, Langham S, Uhl-Hochgraeber K . The burden of testosterone deficiency syndrome in adult men: economic and quality-of-life impact. J Sex Med 2007; 4: 1056–1069.
Bender BG, Linden MG, Harmon RJ . Life adaptation in 35 adults with sex chromosome abnormalities. Genet Med 2001; 3: 187–191.
Geschwind DH, Dykens E . Neurobehavioral and Psychosocial issues in Klinefelter syndrome. Learn Disabil Res Pract Vol 2004; 19: 166–173.
Nielsen J, Sorensen K, The importance of early diagnosis of Klinefelter's syndrome. In: Bandman H, Breit R (eds) Klinefelter's syndrome. Berlin, Springer-Verlag, 1984; 170–187.
Mandoki MW, Sumner GS . Klinefelter syndrome: the need for early identification and treatment. Clin Pediatr 1991; 30: 161–164.
Herlihy AS, Halliday J, McLachlan RI, Cock M, Gillam L . Assessing the risks and benefits of diagnosing genetic conditions with variable phenotypes through population screening: Klinefelter syndrome as an example. J Community Genet 2010; 1: 6.
International Wellbeing Group. Personal Wellbeing Index, 2005. Available at: http://www.deakin.edu.au/research/acqol/instruments/wellbeing_index.htm. Accessed July 20, 2010.
Cummins RA, Eckersley R, Pallant J, van Vugt J, Misajon R . Developing a national index of subjective wellbeing: the Australian Unity Wellbeing Index. Soc Indicators Res 2003; 64: 31.
Cummins RA, Woerner J, Tomyn A, Gibson A, Knapp T The wellbeing of Australians, 2006. Available at: http://www.acqol.deakin.edu.au. Accessed July 20, 2010.
Cummins RA, Collard J, Woerner J, Weinberg M, Lorbergs M, Perera C . Australian Unity Wellbeing Index Survey 22: report 22.0. Melbourne, Deakin University, 2009.
Brown TA, Cash TF, Mikulka PJ . Attitudinal body-image assessment: factor analysis of the body-self relations questionnaire. J Pers Assess 1990; 55: 135–144.
Cash TF . The multidimensional body-self relations questionnaire user's manual. Norfolk, Old Dominion University, 2000.
Rosenberg M . Society and the adolescent self-image. Princeton, NJ, Princeton University Press, 1965.
Schmitt DP, Allik J . Simultaneous administration of the Rosenberg Self-Esteem Scale in 53 nations: exploring the universal and culture-specific features of global self-esteem. J Personality Social Psychol 2005; 89: 623–642.
Kessler RC, Andrews G, Colpe LJ, et al. Short screening scales to monitor population prevalences and trends in non-specific psychological distress. Psychol Med 2002; 32: 959–976.
Australian Bureau of Statistics National Health Survey: summary of results 2007–2008 (4364.0). Canberra, Australian Bureau of Statistics, 2009.
Australian Bureau of Statistics National Health Survey: users' guide 2007–2008 (4363.0). Canberra, Australian Bureau of Statistics, 2009.
Pierce GR, Sarason IG, Sarason BR, Solky-Butzel JA, Nagle LC . Assessing the quality of personal relationships. J Soc Personal Relationships 1997; 14: 339–356.
Vassallo S, Smart D, Price-Robertson R . The roles that parents play in the lives of their young adult children. Fam Matters 2009; 82: 8–14.
Stern BB, Barak B, Gould SJ . Sexual identity scale: a new self-assessment measure. Sex Roles 1987; 17: 503–519.
Radicioni AF, De Marco E, Gianfrilli D, et al. Strategies and advantages of early diagnosis in Klinefelter's syndrome. Mol Hum Reprod 2010; 16: 434–440.
Bojesen A, Gravholt CH . Klinefelter syndrome in clinical practice. Nat Clin Pract Urol 2007; 4: 192–204.
Williams JM, Dunlop LC . Pubertal timing and self-reported delinquency among male adolescents. J Adolesc 1999; 22: 157–171.
Aksglaede L, Andersson AM, Jorgensen N, et al. Primary testicular failure in Klinefelter's syndrome: the use of bivariate luteinizing hormone-testosterone reference charts. Clin Endocrinol 2007; 66: 276–281.
Schiavi RC, Theilgaard A, Owen DR, White D . Sex chromosome anomalies, hormones, and sexuality. Arch Gen Psychiatry 1988; 45: 19–24.
Borelli JB, Bender BG, Puck MH, Salbenblatt JA, Robinson A . The meaning of early knowledge of a child's infertility in families with 47,XXY and 45,X children. Child Psychiatry Hum Dev 1984; 14: 215–222.
Sell RL, Becker JB . Sexual orientation data collection and progress toward Healthy People 2010. Am J Public Health 2001; 91: 876–882.
McConaghy N, Hadzi-Pavlovic D, Stevens C, Manicavasagar V, Buhrich N, Vollmer-Conna U . Fraternal birth order and ratio of heterosexual/homosexual feelings in women and men. J Homosex 2006; 51: 161–174.
Bailey DB Jr, Skinner D, Warren SF . Newborn screening for developmental disabilities: reframing presumptive benefit. Am J Public Health 2005; 95: 1889–1893.
Gallo AM, Knafl KA, Angst DB . Information management in families who have a child with a genetic condition. J Pediatr Nurs 2009; 24: 194–204.
Acknowledgements
This work was supported by the National Health and Medical Research Council of Australia, Andrology Australia, Monash University, and Bayer Schering Pharma, who provided support for costs associated with the study in the form of an unrestricted educational grant. The authors thank all the study participants who shared their experiences so willingly, and the doctors and other health professionals who gave their time to assist in recruitment. Obioha Ukoumunne provided invaluable statistical advice.
Author information
Authors and Affiliations
Corresponding author
Additional information
Disclosure: The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Herlihy, A., McLachlan, R., Gillam, L. et al. The psychosocial impact of Klinefelter syndrome and factors influencing quality of life. Genet Med 13, 632–642 (2011). https://doi.org/10.1097/GIM.0b013e3182136d19
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1097/GIM.0b013e3182136d19
Keywords
This article is cited by
-
Subjective versus objective sleep in men with Klinefelter syndrome
Orphanet Journal of Rare Diseases (2023)
-
Healthcare and support experiences of adolescents and young adults diagnosed with 47,XXY, 47,XXX, and 48,XXYY
Journal of Community Genetics (2023)
-
Experiences of individuals receiving a sex chromosome multisomy diagnosis
Journal of Community Genetics (2022)
-
Quality of life in Klinefelter patients on testosterone replacement therapy compared to healthy controls: an observational study on the impact of psychological distress, personality traits, and coping strategies
Journal of Endocrinological Investigation (2021)
-
Participation of adults with disorders/differences of sex development (DSD) in the clinical study dsd-LIFE: design, methodology, recruitment, data quality and study population
BMC Endocrine Disorders (2017)