Abstract
Aims
The purpose of this report is to demonstrate that a non-contact ultra-widefield dual wavelength laser camera (Optos) is able to capture high-quality images in retinopathy of prematurity (ROP).
Materials and methods
We conducted a retrospective review of patients attending the Oxford Eye Hospital with ROP between 1 August 2012 and 16 November 2012 that underwent standard clinical assessment. Anterior segment imaging, where relevant, was performed with Retcam. Retinal imaging was then performed with Optos, using a modified ‘flying baby position’.
Results
The Optos scanning laser ophthalmoscope was able to acquire ultra-widefield fundal images in nine ROP subjects. The images obtained show clear views of the different stages of ROP features at the posterior pole and peripheral retina. Regression of ROP features were identified, following laser and intravitreal bevacizumab treatment. Additionally, ‘skip areas’ missed by initial laser treatment could be identified in the peripheral retina.
Conclusion
The Optos ultra-widefield scanning laser ophthalmoscope is capable of acquiring clinically useful high-quality images of the fundus in ROP subjects. The imaging technique could potentially be used in monitoring ROP progression and documenting ROP regression following treatment.
Similar content being viewed by others
Introduction
Our centre uses Retcam (Clarity Medical Systems, Pleasanton, CA, USA) to monitor objectively the response to laser treatment of advanced retinopathy of prematurity (ROP) that is identified by indirect ophthalmoscopy during screening. Retcam imaging is useful for teaching and permits the detection of ‘skip areas’, which can be dealt with as a top-up treatment. As Retcam requires contact with the eye, we became concerned about increased infection risk when using it in the early postoperative period, following intravitreal injection of bevacizumab (Avastin; Roche, Grenzach, Germany) for high-risk posterior ROP.1 We had successfully obtained an oral fluorescein angiogram using a non-contact ultra-widefield scanning laser ophthalmoscope system in an infant referred for the management of incontinentia pigmenti and decided to use the ophthalmoscope to monitor the therapeutic response to intravitreal injection of bevacizumab.2 We felt that the quality of non-contact ultra-widefield imaging (NC-UWFI) was superior to Retcam in many ways. On the basis of these clinical experiences, we started using the ultra-widefield imaging device more frequently in babies that attended the Oxford Eye Hospital outpatient department for follow-up of ROP. We report our index case using NC-UWFI and describe the imaging characteristics of a cohort of patients with all stages of ROP, attending for the follow-up.
Materials and methods
All babies were examined by a consultant ophthalmologist (CKP) with 11 years experience in managing ROP at the Oxford University Hospitals NHS Trust, a large teaching hospital in the United Kingdom, specialising in tertiary management of advanced ROP and associated with a level-3 neonatal intensive care unit (NICU). Acute ROP was graded according to the modified ICROP classification.3
Technique
For cases 1–8, indirect ophthalmoscopy was undertaken, following instillation of topical proparacaine 0.5%, cyclopentolate 0.5%, and phenylephrine 2.5%. NC-UWFI was then performed using a scanning laser ophthalmoscope, the Optos Panoramic 200Tx imaging system (Optos PLC, Dunfermline, Scotland, UK) located in the Oxford Eye Hospital clinical imaging department. Babies resident in our NICU were monitored according to the standard NICU protocol. Under topical anaesthesia, a paediatric Lieberman eyelid speculum (Duckworth & Kent Ltd, Baldock, Hertfordshire, UK) was used, with the speculum stabilised by taping its handle to the baby’s cheek. The cornea was hydrated with saline drops and the infant held in the modified ‘flying baby position’ (Figure 1a), with one arm supporting the chest/chin and the other hand supporting the head. The head was moved towards the scanning laser ophthalmoscope, with visual feedback on the monitor guiding movement of the eye until the pupil was aligned. The photographers (LS, JB) captured the images when the eye was in the optimal position. Following satisfactory image acquisition, the process was repeated for the fellow eye. In babies attached to continuous positive airway pressure (CPAP), it was necessary to remove the protective cover of the Optos mirror that allowed the baby to move close enough to acquire images. Case 9 was nearly 7 years old and under annual review for ROP. She did not undergo indirect ophthalmoscopy and was able to cooperate with a routine examination using NC-UWFI with Optos. The images illustrated in this paper were processed using commercially available software (Photoshop CS5.5, Adobe, San Jose, CA, USA) to yield pseudo-colour images with adjustments to optimise the brightness, contrast, exposure, and colour balance.
(a) Modified ‘flying baby position’. (b) Pseudo-colour fundal Optos images of a CPAP baby’s right eye with APROP before Avastin injection: prominent plus disease with circumferential neovascular proliferation in zone 1 (white arrows) was noted. The CPAP is visible (yellow arrow). (c) Pseudo-colour fundal Optos images of a CPAP baby’s right eye with APROP after Avastin injection: improvement in plus disease was noted (d, e). Pseudo-colour fundal Optos images of a baby with resolved stage 3, zone-1 ROP. Scarring in zone 2 of the right eye and zone 3 of the left eye was noted (white arrows).
Results
A total of nine babies attended the Oxford Eye Hospital between 1 August and 15 November 2012 and underwent NC-UWFI. Their demographics and classification of acute ROP is summarised in Table 1. A wide spectrum of retinal changes representative of ROP is shown in one or both eyes of each baby, with a summary below each image.
Case 1: Aggressive posterior ROP
Pseudo-colour fundus images, obtained with NC-UWFI of the right eye of our index case, showing APROP (Figure 1b). The CPAP is visible (yellow arrow) and there is prominent plus disease, with circumferential neovascular proliferation in zone 1 (Figure 1b; white arrows). The baby was treated with an intravitreal injection of bevacizumab, and after 24 h the plus disease had improved significantly (Figure 1c).
Case 2: Resolved stage 3, zone-1 ROP
This baby developed zone 1, stage-3 ROP with pre-plus disease, and was treated with bilateral Avastin injection therapy at 34 weeks postnatal age (PNA). The baby was discharged to a nearby unit but returned for cleft palate repair to our hospital at 70 weeks PNA. At this visit, the NC-UWFI showed progression of retinal vascularisation with no evidence of retinal detachment (Figures 1d and e). There was however some scarring in zone 2 of the right eye and zone 3 of the left eye (Figure 1e; white arrows), which is being carefully monitored.
Case 3: Stage-1 ROP in zone 3
This baby was at a very low risk for developing sight-threatening retinopathy. NC-UWFI was able to capture the stage-1 ROP disease that was detected with indirect ophthalmoscopy in zone 3 of the right eye (Figure 2a).
(a) Pseudo-colour fundal Optos image of a baby’s right eye with stage 1, zone-3 ROP (white arrows). (b) Pseudo-colour fundal Optos image of a baby’s right eye with stage 2, zone-2 ROP (white arrows). (c) Pseudo-colour fundal Optos image of a baby’s left with stage 3, zone-2 ROP and multifocal retinal haemorrhages. Extra-retinal neovascularisation was seen (white arrows).
Case 4: Stage-2 ROP in zone 2
This is a very low birth-weight baby of mixed race in whom vascularisation from zone 2 into zone 3 took a long time, and remains incomplete. NC-UWFI shows a stage-2 ROP in zone 2, nasally in the right eye (Figure 2b).
Case 5: Stage-3 ROP in zone 2 with pre-plus disease
A baby with mild hydrocephalus that underwent ROP screening was found to have multiple bilateral intra-retinal haemorrhages. NC-UWFI of the left eye shows zone 2, stage-3 ROP with pre-plus disease, requiring weekly review. The extra-retinal neovascularisation is indicated by the white arrows in Figure 2c.
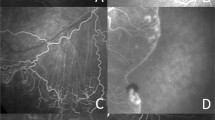
Case 6: Stage-3 ROP in zone 2 with plus disease
The NC-UWFI shows stage-3 ROP in zone 2 with plus disease. In both eyes, extra-retinal neovascularisation is associated with pre-retinal haemorrhage (Figures 3a and b; white arrows). In the right eye, there was a pre-existing corneal scar that did not appear to affect the quality of the retinal images (Figure 3a). Diode laser treatment was applied to both eyes, and we recorded the disease activity 1 week later (Figures 3c and d). Skip areas were seen supero-temporally in the right eye (yellow arrows in Figure 3c). The plus disease had however improved bilaterally.
(a–d) Pseudo-colour fundal Optos images of a baby with stage 3, zone-2 ROP with plus disease—extra-retinal neovascularisation (white arrows in (a, b)) was noted in both eyes. The quality of image obtained in the right eye was not affected by an existing corneal scar (blue arrow in (a)). One week after diode laser treatment, a skip area supero-temporally (yellow arrows in (c)) was seen. (e) Pseudo-colour fundal Optos image of a baby’s right eye with stage-4b ROP—fibrous tissue associated with a tractional retinal detachment (white arrows) was noted. Yellow arrow notes position of the optic disc. (f) Pseudo-colour fundal Optos image of a baby’s left eye after laser treatment of stage-4a ROP—skip areas were noted nasally.
Case 7: Stage-4b ROP right eye and stage-4a left eye
This baby underwent two episodes of bilateral laser treatment elsewhere, with subsequent progression to stage-4b and stage-4a ROP in the right and left eye, respectively (Figures 3e and f). The left eye had skip areas nasally that were treated with additional laser, and the right eye was managed conservatively.
NC-UWFI in the right eye showed fibrous tissue associated with a tractional retinal detachment involving the macula (white arrows in Figure 3e), with the optic disc indicated by the yellow arrow in Figure 3e. There was a peripheral retinal detachment seen infero-temporally in the left eye, which is not convincingly visualised in the Optos image.
Case 8: Stage-4a ROP in zone 2
A baby was referred after developing bilateral, threshold ROP in zone 2 (Figure 4a). Confluent bilateral laser photocoagulation was performed at 39 weeks PNA and the baby discharged for ophthalmic review elsewhere. She developed bilateral stage-4a retinal detachment and a heavy circumferential cicatrix 5 weeks later. The baby was re-admitted to our hospital, and treated with bilateral encirclement and left-sided lens sparing vitrectomy.
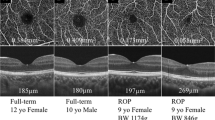
(a–c) Pseudo-colour fundal Optos images of a baby’s left eye with threshold ROP in zone 2 (white arrows in (a)). Extra-foveal retinal detachment infero-temporally (blue arrow in (b)) was noted. The residual circular cicatrix that required support from an encircling band was seen in (c). (d) Pseudo-colour fundal Optos image of a 7-year-old child’s left eye with a history of treated stage 3, zone-1 ROP. This case was imaged through a small pupil (bottom left picture).
The NC-UWFI from the left eye shows a double ridge of stage 3 before laser treatment (Figure 4a; white arrows). Following initial laser treatment, cicatrisation of the ridge developed, with a subsequent extra-foveal retinal detachment in the infero-temporal quadrant (Figure 4b; blue arrow). Lens-sparing vitrectomy to partially release traction has resulted in the resolution of retinal detachment, and it is possible to visualise the residual circular cicatrix that required support with an encircling band (Figure 4c).
Case 9: Treated stage-3 ROP in zone 1
A pseudo-colour fundal image of the left eye has been acquired through small bound-down pupil (Figure 4d) and cataract at 7 years of age. The child had had two lens-sparing vitrectomies and encirclement with silicone oil tamponade as a baby. Further surgery involved division of the buckle and removal of oil for a stage-4b ROP in the left eye. At the annual outpatient clinic review, the child cooperated with an Optos examination by fixating on the target shown by the device in the standard manner.
Discussion
The evaluation of retinal disease is undergoing a revolution with digital imaging at the core of improving the management of major blinding disease, such as age-related macular degeneration, glaucoma, and the spectrum of genetic and vitreoretinal disease. This report demonstrates that Optos ultra-widefield scanning laser ophthalmoscope is capable of acquiring clinically useful images, and documenting a wide spectrum of acute and chronic retinal features known to define ROP.
Digitised images from video-indirect ophthalmoscopes have been used to document disease features.4, 5 Narrow field devices have been used to document plus disease.6 The most popular digital widefield imaging device is Retcam that uses incandescent light for illuminating the retina. It requires apposition to the cornea and has the potential to yield high-quality images that can facilitate telemedicine screening.6 The field-of-view is around 130° and this requires 3–7 images to capture most of the peripheral features of ROP. In telemedicine screening the device has >90% sensitivity for detecting plus disease and referral-warranted ROP.6 This sensitivity drops significantly with decreasing PNA, when media clarity and the smaller palpebral aperture relative to camera size are barriers to the successful use of Retcam.
The major challenge of imaging non-sedated babies is that ocular movement can impair image acquisition. Retcam partly overcomes this by immobilising the eye through contact, although, in our experience, the eye may still rotate under the camera head. The Optos uses two wavelengths of laser and has a very fast image acquisition time once pupil alignment is achieved. It has been our experience that imaging with Optos was generally faster than with Retcam. Retcam assessment takes significantly longer than indirect ophthalmoscopy in experienced hands.7 Our experience is that Retcam is especially difficult to use in older babies because of excessive head movement. Case 2, who was 70 weeks PNA, underwent NC-UWFI with little difficulty. However, in younger sicker babies, for example, those with APROP, cardiac morbidity could be precipitated by the handling required for the ‘flying baby position’. We minimised such risk in our out-patient setting through the presence of neonatal staff who monitored vital signs. Optos therefore has the potential to alter the distress response, but this hypothesis requires scientific testing in a neonatal in-patient setting.
Our experience in the older children who attend for follow-up is that they will not cooperate with video-indirect ophthalmoscopy or Retcam sufficiently to obtain useful images. Older children like case 9 are able to cooperate with NC-UWFI, presumably because photophobia is less of an issue with a laser-based camera. This type of approach has the potential of reducing the need for examination under anaesthesia to ascertain retinal disease status.
Image quality in ROP is defined in terms of field; that is, coverage and clarity.8 NC-UWFI is potentially the best with regard to coverage. A single image in an adult covers 200° anteroposteriorly, while that of Retcam covers 130° and that of other modalities less.6 Using Optos, the horizontal meridians appear to be imaged further anteriorly compared with vertical meridians. In a single image (Figure 3c), one can visualise the circumferential extent of stage-3 disease in zone 2 (approximately 270°). This would not usually be expected with Retcam imaging.
Retcam can through excessive pressure on the eye affect the accurate diagnosis of plus disease, a problem that would not be expected of a non-contact system.9 Retinal image clarity associated with Retcam has been reviewed in detail and is reduced by several factors, including decreasing PNA, media opacity, anterior disease location, and darkly pigmented fundi.6 A corneal scar and mild vitreous haemorrhage (Figure 3a) did not appear to compromise retinal image quality, which is also maintained in the presence of cataract and a small pupil (case 9). Four out of nine of our patients had darkly pigmented fundi, and this did not compromise peripheral image clarity. Our experience is that imaging of anterior zone 2 and zone 3 with Retcam is poor. The likely explanation for improved image clarity relates to the confocal design of the Optos imaging device that is less prone to scatter than the incandescent illumination used by Retcam.
We found several limitations with the Optos system that requires further evaluation in a larger study. The lack of contact with the cornea using the Optos introduces variables that can degrade image clarity. On several images in the present series it can be seen that eye lashes are visible. We have been able to deal with this by taping the lashes down in some cases. The ability to image retinal detachment is the least impressive aspect of imaging with Optos. The left eye of case 7 had elevated retina infero-temporally, which was not convincingly seen in the image. It is possible that tear film changes, ocular alignment, or movement artefact are responsible.
NC-UWFI in cases 3 and 4 clearly show the presence of disease in zones 3 and 2, respectively. In order to discharge a baby from an ROP screening programme, vascularisation into zone 3 needs to be seen accurately on an imaging device. The Optos system opens up the possibility that telemedicine capability could be developed as a more comprehensive tool to manage exit from a hospital screening programme as well as to define disease severity that requires treatment.
In summary, our group has presented for the first time the use of Optos for NC-UWFI to document the acute and chronic features of ROP. The precise role of NC-UWFI in the management of ROP requires rigorous prospective scientific evaluation to evaluate the risk–benefit ratio, which will then inform whether the technique is worth considering for telemedicine paradigms.

References
Mintz-Hittner HA, Kennedy KA, Chuang AZ . Efficacy of intravitreal bevacizumab for stage 3+ retinopathy of prematurity. N Engl J Med 2011; 364 (7): 603–615.
Patel CK, Fung THM, Muqit MMK, Mordant DJ, Geh V . Non-contact ultra-wide field retinal imaging and fundus fluorescein angiography of a baby with incontinentia pigmenti without sedation in an ophthalmic office setting. JAAPOS 2013 (in press).
International Committee for the Classification of Retinopathy of Prematurity. The International Classification of Retinopathy of Prematurity revisited. Arch Ophthalmol 2005; 123 (7): 991–999.
Patel CK . Optical coherence tomography in the management of acute retinopathy of prematurity. Am J Ophthalmol 2006; 141 (3): 582–584.
Ahmad S, Wallace DK, Freedman S, Zhao Z . Computer-assisted assessment of plus disease in retinopathy of prematurity using video indirect ophthalmoscopy images. Retina 2008; 28 (10): 1458–1462.
Richter GM, Williams SL, Starren J, Flynn JT, Chiang MF . Telemedicine for retinopathy of prematurity diagnosis: evaluation and challenges. Surv Opthalmol 2009; 54 (6): 671–685.
Mukherjee AN, Watts P, Al-Madfai H, Manoj B, Roberts D . Impact of retinopathy of prematurity screening examination on cardiorespiratory indices: a comparison of indirect ophthalmoscopy and Retcam imaging. Ophthalmology 2006; 113 (9): 1547–1552.
Chiang MF, Wang L, Busuioc M, Du YE, Chan P, Kane SA et al. Telemedical retinopathy of prematurity diagnosis: accuracy, reliability, and image quality. Arch Ophthalmol 2007; 125 (11): 1531–1538.
Zepeda-Romero LC, Martinez-Perez ME, Ruiz-Velasco S, Ramirez-Ortiz MA, Gutierrez-Padilla JA . Temporary morphological changes in plus disease induced during contact digital imaging. Eye (Lond) 2011; 25 (10): 1337–1340.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Patel, C., Fung, T., Muqit, M. et al. Non-contact ultra-widefield imaging of retinopathy of prematurity using the Optos dual wavelength scanning laser ophthalmoscope. Eye 27, 589–596 (2013). https://doi.org/10.1038/eye.2013.45
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/eye.2013.45
Keywords
This article is cited by
-
Non-contact widefield neonatal retinal imaging for retinopathy of prematurity using the Clarus 700 high resolution true colour reflectance imaging
Eye (2023)
-
Evolving outcomes of surgery for retinal detachment in retinopathy of prematurity: the need for a national service in the United Kingdom
Eye (2022)
-
Smartphone based ROP (S-ROP) screening—opportunities and challenges
Eye (2020)
-
Wide-field imaging of sickle retinopathy
International Journal of Retina and Vitreous (2019)
-
Quantitative comparisons of ultra-widefield images of model eye obtained with Optos® 200Tx and Optos® California
BMC Ophthalmology (2019)