Abstract
MicroRNAs (miRNAs) are short, noncoding RNAs that function as posttranscriptional regulators of gene expression by controlling translation of mRNAs. A subset of miRNAs may be critical for the control of cell death, including the p53-regulated miRNA, miR-34a. Because seizures activate p53, and p53-deficient mice are reportedly resistant to damage caused by prolonged seizures, we investigated the role of miR-34a in seizure-induced neuronal death in vivo. Status epilepticus was induced by intra-amygdala microinjection of kainic acid in mice. This led to an early (2 h) multifold upregulation of miR-34a in the CA3 and CA1 hippocampal subfields and lower protein levels of mitogen-activated kinase kinase kinase 9, a validated miR-34a target. Immunoprecipitation of the RNA-induced silencing complex component, Argonaute-2, eluted significantly higher levels of miR-34a after seizures. Injection of mice with pifithrin-α, a putative p53 inhibitor, prevented miR-34a upregulation after seizures. Intracerebroventricular injection of antagomirs targeting miR-34a reduced hippocampal miR-34a levels and had a small modulatory effect on apoptosis-associated signaling, but did not prevent hippocampal neuronal death in models of either severe or moderate severity status epilepticus. Thus, prolonged seizures cause subfield-specific, temporally restricted upregulation of miR-34a, which may be p53 dependent, but miR-34a is probably not important for seizure-induced neuronal death in this model.
Similar content being viewed by others
Main
MicroRNAs (miRNAs) are an expanding class of small noncoding RNAs that function as posttranscriptional regulators of gene expression. They are critical for embryogenesis, development and normal cell physiology.1 miRNAs are processed from primary transcripts to pre-miRNA, exported from the nucleus, processed further by Dicer, after which a single strand is uploaded to the RNA-induced silencing complex (RISC).2 Here, approximately seven-nucleotide seed regions within the 5′ portion of the miRNA associate with complementary regions within the 3′ untranslated region of the mRNA, along with additional base pairing, resulting in translational repression or mRNA decay.3 miRNAs have been shown to regulate cell cycle and cell death, and miRNA dysfunction has been implicated in neurodegenerative diseases.4 Acute neurological insults also alter expression of miRNAs, and emerging data show that prolonged seizures (status epilepticus (SE)) regulate miRNA expression in the brain.5, 6, 7
The p53 transcription factor is an important regulator of cell cycle, DNA repair and apoptosis. When activated, p53 transcribes several genes that promote either DNA repair (e.g., Gadd45α), cell cycle arrest (Cdc25c) or apoptosis (Puma, Bax).8 Prolonged seizures lead to accumulation of p53 in the neurons and induction of Puma.9, 10, 11 Pharmacological or genetic inhibition of p53 or loss of Puma is protective in in vivo models of seizure-induced neuronal death,11, 12, 13, 14, 15 although the genetic background has been shown to be an important influence on whether p53 deficiency is protective in seizure models.16
miR-34a belongs to one of several evolutionarily conserved families of miRNAs and is a p53-regulated miRNA that is constitutively expressed in the brain.17 Welch et al.18 were the first to demonstrate pro-apoptotic functions of miR-34a, followed thereafter by a series of reports confirming and extending this evidence.19, 20, 21, 22 Overexpression of miR-34a was shown to induce caspase-dependent apoptosis in cells,18 whereas inactivation of miR-34a inhibited p53-dependent apoptosis.19 Nevertheless, miR-34a may be necessary but not sufficient to account for p53-dependent apoptosis. miR-34a may also have p53-independent pro-apoptotic mechanisms,20 and miR-34a was recently reported to influence neuronal morphology and function23 and attenuate p53 regulation of induced pluripotent stem cell generation.24
Several targets of miR-34a have been identified, including Bcl-2,17 E2F318 and mitogen-activated protein kinase kinase kinase 9 (MAP3K9; MLK1).25 Overexpression of miR-34a in cells is capable, however, of altering expression of over 100 proteins.20, 26 Thus, the pro-apoptotic mechanism and full repertoire of miR-34a effects remain to be cataloged.
Given the evidence that p53 contributes to seizure-induced neuronal death in vivo and emerging data supporting a role for miRNAs in the pathophysiology of epilepsy, we hypothesized that miR-34a would be upregulated by seizures and contribute to seizure-induced neuronal death. Our results show that seizures strongly upregulate miR-34a, and that this is p53 regulated, but silencing miR-34a in vivo does not prevent seizure-induced neuronal death.
Results
Rapid upregulation of miR-34a after SE
We have previously shown that protein levels of p53 begin to increase in the cornu ammonis (CA) 3 subfield of the hippocampus within 1 h of SE.11 As miR-34a is a p53-regulated miRNA, we examined whether seizures also upregulate miR-34a. SE was induced by unilateral microinjection of kainic acid (KA, 1 μg) into the amygdala of mice, as described earlier.14 Electroencephalogram (EEG) recordings from skull-mounted electrodes confirmed seizures, in the form of high-amplitude high-frequency discharges (HAHFDs), emerging within 5–10 min of KA injection (Supplementary Figure 1a). Electrographic seizures continued, becoming near continuous over the next 40 min. Histopathological inspection of the hippocampus 24 h later revealed seizure-induced neuronal death as detected by Fluoro-Jade B (FJB) staining within the ipsilateral CA3 subfield (Supplementary Figure 1b). Damage to the ipsilateral hilus was also present, along with lesser injury to area CA1 (Supplementary Figure 1b).
Using real-time (RT)-PCR, we measured expression of mature miR-34a within the CA3 and CA1 subfields of the ipsilateral hippocampus at various time points, and compared levels with samples from time-matched, vehicle-injected non-seizure controls (Figures 1a and b). A large increase in miR-34a expression was detected 2 h following SE in the CA3 subfield (Figure 1a). Expression of miR-34a in CA3 returned to a similar level to controls at 6 and 24 h, and levels of miR-34a were also not different from that of controls at 3 and 7 days, which corresponds to the time when the first spontaneous (i.e., epileptic) seizures occur in the model.11, 15 Expression of miR-34a also increased in the less damaged CA1 subfield after SE, beginning at 2 h but peaking later, at 6 h, and at much higher levels than in CA3 (Figure 1b). Levels of miR-34a in CA1 were similar to controls at 1, 3 and 7 days after SE (Figure 1b).
Increased binding of miR-34a to Argonaute-2 after SE
miRNA function requires their uploading into the RISC, where Argonuate-2 (Ago-2) contributes to miRNA-induced silencing of mRNAs.3 To determine whether increased miR-34a levels after seizures result in a corresponding increased loading of the miRNA into the RISC, we immunoprecipitated Ago-2 from control and seizure hippocampus at 2 h and used PCR to detect miR-34a. Western blot analysis did not detect a significant difference in Ago-2 levels between controls and KA-injected mice at 2 h (data not shown). Levels of Ago-2-bound miR-34a were increased over 3.5-fold in seizure samples compared with controls (Figure 2a).
RISC loading of miR-34a, downregulation of target Map3k9 and p53 dependence. (a) Graph showing miR-34a levels eluted by immunoprecipitation of Ago-2 from non-seizure controls (Con) and mice 2 h after SE. ***P<0.001 compared with control (n=3 per group). (b) Representative western blot (n=1 per lane) showing protein levels of the miR-34a target Map3k9 in Con and 2, 4 or 24 h after SE. β-Actin is included as a guide to protein loading. Molecular weight markers depicted to the right. Time in hours after KA is shown above. (c) Semiquantification of Map3k9 levels after seizures. *P<0.05 compared with control (n=4 per group). (d) RT-PCR measurement of p53-target gene p21WAF/Cip1 expression in seizure mice at 2 h showing reduced expression of the p53-regulated gene in mice treated with pifithrin-α (PFT) compared with vehicle (Veh, DMSO; *P<0.05 compared with vehicle; n=5 per group). (e) Graph showing RT-PCR measurement of miR-34a in animals given PFT or Veh before SE. **P<0.01 compared with vehicle (n=3–4 per group)
We next examined whether a recently experimentally validated miR-34a target, Map3k9,25 showed the predicted downregulation at the protein level shortly after the time when miR-34a was upregulated. Western blot analysis found a significant reduction in hippocampal Map3k9 protein levels at 2 and 4 h after SE (Figures 2b and c). Map3k9 levels returned to control levels at 24 h after SE (Figures 2b and c).
miR-34a induction by seizures is blocked by pifithrin-α
To explore whether miR-34a was under p53 control during seizure-induced neuronal death, we treated mice with pifithrin-α, a p53 inhibitor,27 before SE. Seizure severity was not significantly different between mice injected with pifithrin-α or vehicle (data not shown). To confirm that pifithrin-α had blocked p53 transcriptional activity, we measured expression of p21WAF/Cip1, a known p53-regulated gene encoding a cyclin-dependent kinase inhibitor.11, 19, 22 Hippocampal levels of p21WAF/Cip1 were significantly lower in mice treated with pifithrin-α (4 mg/kg, twice) before SE compared with vehicle controls after seizures (Figure 2d).
Next, we measured miR-34a levels in CA3 samples from vehicle- and pifithrin-α-injected seizure mice. Administration of pifithrin-α significantly reduced hippocampal miR-34a expression 2 h after SE relative to vehicle-injected seizure controls (Figure 2e). To evaluate the specificity of this effect, we measured miR-92a, which may be under p53 control in some systems.22 Levels of miR-92a were not reduced in pifthrin-α-treated mice (P=0.09, data not shown). Similarly, expression of miR-134, which has not been associated with p53 regulation, was not reduced by pifithrin-α (P=0.15, data not shown).
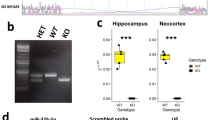
In vivo depletion of miR-34a using antagomirs
We recently reported that miR-132 expression could be reduced in vivo by intracerebroventricular (i.c.v.) injection of sub-nanomolar doses of locked nucleic acid--modified, cholesterol-tagged antagomirs.7 We therefore used i.c.v. injections of antagomirs targeting miR-34a (Ant-34a) to reduce brain levels of miR-34a in vivo. Injection of 0.1 nmol Ant-34a did not significantly change hippocampal miR-34a levels when assessed 24 h later relative to a nontargeting scrambled control (Figure 3a). In contrast, miR-34a levels were significantly reduced in mice injected with 0.5 nmol Ant-34a (Figure 3a). Expression of miR-134 was not significantly altered by injection of either dose of antagomir (Figure 3b). Further increases of antagomirs/scrambled doses were not attempted because of possible off-target effects on other miRNAs above 0.5 nmol.7
Effect of antagomirs on brain levels of miR-34a and seizure EEG. (a and b) Effect of antagomirs targeting miR-34a (Ant-34a) and scrambled (Scram) on hippocampal CA3 expression of A, miR-34a, and B, miR-134, measured 24 h after injection. Expression levels were corrected to RNU6B. *P<0.05 compared with Scram (n=3 per group). (c) Representative EEG spectrogram during SE in mice given either Scram or Ant-34a. (d) Graphs showing semiquantification of seizure parameters between treated mice subjected to SE (n=7–8 per group). Differences were not statistically significant
We next subjected mice to intra-amygdala KA-induced SE 24 h after i.c.v. injection of 0.5 nmol of either Ant-34a or scrambled (Figure 3c). Seizure severity as assessed by durations of HAHFDs or total EEG power analysis was not significantly different between mice given Ant-34a compared with scrambled-injected mice (P=0.11 for HAHFDs; P=0.41 for total power, Figures 3c and d).
Inhibition of miR-34a does not prevent seizure-induced neuronal death in vivo
We next compared damage within dorsal (septal) hippocampus between Ant-34a- and scrambled-treated mice 24 h after SE. In rostral sections, seizure-induced neuronal death in scrambled-injected mice exhibited typical damage within CA3, hilus and CA1 subfields (Figure 4a, and compare to Supplementary Figure 1b). Seizure-induced neuronal death was not different in mice injected with antagomirs targeting miR-34a (Figures 4a and b); that is, Ant-34a-injected animals displayed similar CA3 lesions to scrambled mice, and counts of FJB-positive CA3 neurons found no difference between the groups at this stereotaxic level (Figure 4b). Results were similar when medial sections were analyzed, with similar distribution of hippocampal damage and no difference in FJB counts between the groups (Figures 4a and c). We also stained additional sections for DNA fragmentation using terminal deoxynucleotidyl dUTP nick end labeling (TUNEL). TUNEL counts were not different between scrambled- and antagomir-treated mice (data not shown).
No effect of antagomirs targeting miR-34a on seizure-induced neuronal death. (a) Representative photomicrographs of the ipsilateral hippocampus at two levels of the dorsal hippocampus from mice 24 h after SE given either 0.5 nmol Scram or Ant-34a. Black dots are FJB-positive cells. Scale bars; rostral, 550 μm; medial, 600 μm. (b and c) Graphs showing FJB counts in ipsilateral CA3 and CA1 at rostral and medial levels of the dorsal hippocampus 24 h after SE (n=7–8 per group). Differences were not statistically significant
To exclude the possibility that seizure-induced neuronal death triggered by 1 μg KA was too severe to protect against, we undertook a second series of experiments in mice given a lower dose of KA. This produces a focal lesion, mainly within the CA3 subfield, with only occasional neuronal death in the hilus.14 Seizure severity was again comparable between mice injected with scrambled or Ant-34a and then subjected to seizures by 0.3 μg intra-amygdala KA (Figures 5a and b). Analysis of seizure-induced neuronal death found a typical CA3-dominant lesion in scrambled-injected mice subjected to SE via intra-amygdala injection of 0.3 μg KA (Figure 5c). Mice injected with Ant-34a also displayed a similar CA3 lesion, and there was no significant difference between groups (Figures 5c and d).
Antagomirs targeting miR-34a do not prevent neuronal death caused by moderate severity SE. (a) Representative seizure EEG spectrogram showing amplitude and frequency during SE in mice that received either targeting (Ant-34a) or non-targeting (Scram) antagomirs (0.5 nmol each) 24 h before intra-amygdala microinjection of 0.3 μg KA. Note more delayed emergence and lesser amplitude/frequency of seizures relative to 1 μg KA model. (b) Graphs showing similar seizure parameters between Ant-34a and Scram-injected mice subjected to 0.3 μg KA-induced SE (n=3 per group). (c) Representative photomicrographs of the FJB stained ipsilateral hippocampus at two levels of dorsal hippocampus of mice 24 h after SE induced by 0.3 μg KA and given either Scram or Ant-34a. Scale bar, 575 μm. (d) Graphs showing FJB counts in ipsilateral CA3 24 h after 0.3 μg KA-induced SE (n=3 per group)
Modulation of apoptosis signaling pathways following inhibition of miR-34a
Although inhibition of miR-34a did not alter seizure-induced neuronal death, we hypothesized that miR-34a reduction might still have effects on the signaling pathways underlying apoptosis. Accordingly, we undertook western blot analysis of proteins from the temporal portion of the hippocampus of scrambled and Ant-34a mice 24 h after seizures. Levels of the cleaved p19 fragment of caspase-3, but not p17 fragment, were significantly lower in samples from mice injected with miR-34a-targeting antagomirs compared with animals given the scrambled sequence (Figures 6a and b and data not shown). Levels of pro-caspase-3 were not different between groups (Figures 6a and b). We also looked at protein levels of Bax because the mRNA for Bax may contain a potentially complementary 7- to 9-nt seed match for miR-34a (see Materials and Methods). Levels of full-length Bax were, surprisingly, significantly higher in antagomir-treated mice than scrambled animals (Figures 6b and c). Levels of a p18 fragment of Bax, reported to be a more pro-apoptotic truncated form,28 were also increased in antagomir-injected mice (Figures 6c and d).
Modulation of apoptosis-associated signaling after antagomirs targeting miR-34a. (a) Levels of cleaved and full-length (fl) caspase-3 (Casp3) protein in hippocampal samples from Scram- or Ant-34a-injected mice 24 h after SE (n=8 per group). Protein levels were corrected to β-actin. (b) Representative western blots (n=1 per lane) showing hippocampal levels of Casp3, p17/19 cleaved Casp3 (cCasp3, arrows) and β-actin as a loading control. (c) Levels of Bax and p18 Bax in each group (n=8 per group). (d) Representative western blots (n=1 per lane) showing hippocampal levels of Bax and p18 Bax. **P<0.01, *P<0.05 compared with Scram
Discussion
In this study, we report that miR-34a is rapidly upregulated in the hippocampus following experimental SE in mice. Levels of miR-34a were also increased within the RISC, and a known target, Map3k9, showed the expected downregulation at a protein level. Results with pifithrin-α suggest that the control of miR-34a is p53 dependent. However, reducing miR-34a expression in vivo using antagomirs failed to alter seizure-induced neuronal death. These studies identify miR-34a as a seizure-regulated miRNA, although the in vivo significance of seizure-induced miR-34a upregulation remains uncertain.
Emerging data point to important roles for miRNAs in the pathogenesis of seizure-induced neuronal death and epilepsy. Indeed, miRNA profiling has detected expression changes for multiple miRNAs following experimentally evoked seizures,6, 7 and miRNA regulation in experimental and human epilepsy.5, 29 The in vivo targets and functional significance of most of these miRNAs remain undetermined, but identification of miRNAs regulating seizure-induced neuronal death could lead to novel targets for neuroprotection and, possibly, anti-epileptogenesis.7, 30 This study explored the role of miR-34a because it had been implicated in p53-dependent control of apoptosis.17 We used intra-amygdala microinjection of KA to trigger focal-onset SE, which produces unilateral hippocampal damage and the subsequent emergence of epileptic seizures.31 Apoptotic pathways contribute to seizure-induced neuronal death in the model, as evidenced by significantly altered hippocampal damage in animals lacking apoptosis-associated genes, including p53, and pharmacological manipulations of core apoptotic components.11, 14, 15, 32 We report for the first time that miR-34a is upregulated after SE in mice. Our data extend earlier profiling work in rats treated with pilocarpine6 and featured individual RT-PCR measurement of mature miR-34a levels, subfield-specific information as opposed to whole hippocampus and a complete temporal profile. Ago-2 pull-down experiments showed that miR-34a was uploaded to the RISC where miRNA-based RNA silencing occurs, and we detected the downregulation of Map3k9 protein, a miR-34a target.25 Some miRNA profiling studies did not detect changes to miR-34a in seizure models.6, 29 This may be because single or later time point sampling would miss the abrupt induction and subsequent restitution of miR-34a levels we observed here. The large-scale upregulation of miR-34a was unexpected, particularly in CA1, exceeding that reported for the pilocarpine model.6 The increase is also greater than in most reports on miR-34a upregulation in non-neuronal tissue.19, 21, 24 Thus, SE, particularly when induced via intra-amygdala KA, is a potent inducer of miR-34a.
miR-34a-induced cell death is caspase dependent,18 and the pro-apoptotic effects of miR-34a may derive from inhibiting translation of anti-apoptotic proteins, such as Bcl-2.17 The observed upregulation of miR-34a in CA3 after SE coincides with the earliest events in the cell death process in this model and precedes post-mitochondrial events such as caspase processing.11, 32 Although the caspase dependence of neuronal death in this model has not been tested directly, the seizure-induced damage is both p53- and Bcl-2 family protein dependent.11, 15, 32 The larger and more sustained increase in miR-34a levels detected in CA1 was unexpected because the CA1 subfield is less damaged in the model.14, 32 If miR-34a is activity regulated, then it could reflect preserved function of this neuron population to transcribe the gene compared with the more damaged CA3. This pattern would also be consistent with miR-34a functions besides control of cell death.23, 24, 33
By comprehensively covering the temporal profile of miR-34a expression after seizures, we found an unusually restricted period of induction. It is unknown why miR-34a levels returned to control in both CA1 and CA3. Indeed, p53 expression remains elevated until at least 24 h in this model.11 Rapid turn-on/turn-off transitions were not noted in the original work linking miR-34a to p53.19, 20, 21, 22 This may be specific, therefore, to the tissue and model. It is possible that p53 targeting of the miR34a gene after seizures is transient and specific to the early transcriptional functions of p53 in the cell death process. Alternatively, p53 may be transcriptionally active for only short periods in the model, perhaps undertaking transcription-independent functions later.34
A number of miRNAs have been shown to be regulated in experimental and human epilepsy.5, 29 Here, we looked for miR-34a regulation in the first week following SE, by which time epileptic seizures would occur.11, 31 Expression of miR-34a was not upregulated in these mice, consistent with profiling work in rat experimental epilepsy, which did not find changes to miR-34a.29 Thus, spontaneous seizures appear insufficient to induce miR-34a despite p53 being upregulated in epilepsy.35, 36 Taken together, these data suggest that miR-34a is particularly associated with the early pathological changes associated with seizure-induced neuronal death but not epilepsy. This contrasts certain other miRNAs that have been shown to be regulated both after SE and in chronic epilepsy.5, 29
Our findings with pifithrin-α, an inhibitor of p53,13, 27 suggest that miR-34a upregulation during seizure-induced neuronal death is under the control of p53. The specificity of this approach was confirmed by the knockdown of p21, a well-characterized target of p53 and index of its transcriptional activity.22 However, pifithrin-α has been found to have anti-apoptotic effects in p53-deficient cells.37 Although miR-34a is perhaps the most significant known miRNA under p53 control,17 it is not the only miRNA regulated by p53. Several other miRNAs identified as p53 regulated19, 20, 22 are also regulated after seizures in our model, including miRs -21, -29a and -132.7 Other factors may also maintain or regulate miR-34a expression, and recent work has identified p53-independent mechanisms of miR-34a control via ELK138 and p73.39
There is strong evidence that miR-34a can promote apoptosis.17 However, the degree to which miR-34a can induce apoptosis varies between studies, being as little as a few percent in some reports19 to ∼20% in others.20 At present, we found that reducing miR-34a levels in vivo using antagomirs did not protect against seizure-induced neuronal death. We used two models, varying the KA dose to alter the amount of cell death.14 Although modulating miR-34a can affect inhibitory currents in neurons,23 seizures were not affected by miR-34a inhibition in either model. Reducing miR-34a levels had no noticeable effect on damage, but antagomirs did cause a small change to apoptosis signaling, a reduction in cleaved caspase-3, consistent with studies showing that miR-34a promotes caspase-dependent apoptosis.18 The relatively small amount of cleaved caspase-3 in the scrambled-treated seizure animals is consistent with the limited apoptotic component in the high-dose KA model.14 Thus, miR-34a inhibition may have affected apoptosis signaling but below a level capable of influencing neuronal death. We must also consider that some miR-34a may escape inactivation by antagomirs, leaving some residual miR-34a in the target tissue. Unexpectedly, we detected higher levels of Bax in antagomir-treated animals. This may be an indirect effect of inhibiting miR-34a,40 or even a nonspecific toxic effect of antagomirs. The result could also be explained if Bax is a miR-34a target, as suggested by bioinformatics, although this requires experimental validation. We might speculate that higher Bax would exert a pro-apoptotic effect, countering any potentially protective influence of reduced caspase-3 cleavage. Regardless, genetic deletion of Puma, a pro-apoptotic Bcl-2 family protein under p53 control, is strongly protective in both models,11, 14 demonstrating that the models are capable of detecting functional contributions of p53-regulated pro-apoptotic genes to neuronal death. Other processes besides control of apoptosis have been reported to be regulated by miR-34a, including neuronal function23 and amygdala-mediated anxiety-like behavior.33 Indeed, combined proteomics–microarray analysis reveal that miR-34a downregulates dozens of protein-coding genes and likely influences diverse processes including metabolism, Wnt signaling and invasion/migration.26 The recent description of miR-34a-deficient mice23, 24 provides the means to assess the impact of complete miR-34a deficiency, not achievable with antagomirs, which may clarify outstanding questions on the contribution of miR-34a to neuronal death after seizures and, perhaps, other neuronal functions.23, 33, 39
In summary, this study contributes to an emerging focus on miR-34a in the brain, demonstrating that miR-34a is upregulated by prolonged seizures in vivo. This occurred in a spatio-temporally specific manner that appears to be p53 regulated. Studies using antagomirs to reduce miR-34a expression in vivo suggest, however, that miR-34a is not functionally significant for seizure-induced neuronal death in this model.
Materials and Methods
Animal model
Animal procedures were reviewed and approved by the Research Ethics Committee of the Royal College of Surgeons in Ireland, under license from the Department of Health, Dublin, Ireland, and were in accordance with the European Communities Council Directive (86/609/EEC). Adult male C57BL/6 mice (20–22 g) were obtained from Harlan (Oxon, Bicester, UK) and housed in a climate-controlled biomedical research facility on a 12 h light/dark cycle with food and water provided ad libitum. All efforts were made to minimize the number of animals used, and to avoid pain and suffering. Focal-onset SE was induced by intra-amygdala stereotaxic microinjection of KA, as described previously.11, 14 Briefly, mice were first anesthetized (5% isoflurane in oxygen; maintenance 1.5–2%) and placed in a stereotaxic frame. Body temperature was maintained within the normal physiological range with a rectal thermometer and a feedback-controlled heat pad (Harvard Apparatus, Kent, UK). Following a midline scalp incision, Bregma was located. Three partial craniectomies were then performed for placement of skull-mounted recording screws (Bilaney Consultants, Sevenoaks, Kent, UK). A complete craniectomy was then drilled for placement of a guide cannula (Coordinates from Bregma; AP=−0.94 mm, L=−2.85 mm based on a mouse brain stereotaxic atlas). The cannula and electrode assembly was then fixed with dental cement, anesthesia was discontinued and the animal was removed from the frame. Next, mice were placed in an open Perspex box and electrodes connected to a Grass Comet XL lab-based EEG via swivel a commutator (Bilaney Consultants). Baseline EEG was recorded and then the animal was lightly restrained while an injection cannula was lowered 3.75 mm below the brain surface to the basolateral amygdala nucleus for injection of KA (Sigma-Aldrich Ireland Ltd, Arklow, Ireland). The injected dose was either 0.3 or 1 μg in 0.2 μl volume to elicit either a moderate or a prolonged SE, respectively.14 Non-seizure control mice underwent the same surgical procedures but received intra-amygdala vehicle (PBS, 0.2 μl). The injection cannula was carefully withdrawn and EEG recordings continued. Following EEG recordings, animals were disconnected and placed in a warmed recovery chamber until recovery.
Mice were killed 2, 4, 6 and 24 h, or 3 and 7 days, after intra-amygdala injections. Animals were given a pentobarbital overdose and perfused with ice-cold saline to remove intravascular blood components. For molecular and biochemical work, brains were microdissected on ice blocks under a microscope and the hippocampus subdivided to obtain the CA3- and CA1-enriched portions. For histology, whole brains were flash-frozen in 2-methylbutane and then sectioned on a cryostat.
Drug injections
Animals were randomized between treatment groups. Pifithrin-α (4 mg/kg, intraperitoneal, in DMSO) was given as a double injection, first 24 h and then 1 h before intra-amygdala KA, as described previously.11 For i.c.v. injections of antagomirs, mice were affixed with a cannula ipsilateral to the side of KA injection (coordinates from Bregma: AP=−0.4 mm, L=−1.15 mm, V=−2.0 mm). Mice received a 2-μl infusion of miR-34a-silencing antagomir (Exiqon, Vedbaek, Denmark) or scrambled antagomir (0.1 or 0.5 nmol), in artificial cerebrospinal fluid (Harvard Apparatus).
EEG analysis
EEG was recorded and analyzed using the TWin software. Two parameters were determined. The duration of high-amplitude (>2 × baseline), high-frequency (>1 Hz) discharges was manually counted. Automated EEG total power analysis was also performed, using the LabChart Pro v7 software (ADInstruments Ltd, Oxford, UK).7
RT-q (quantitative) PCR analysis of miRNA expression
Reverse transcription for individual qPCRs was carried out as described,7 using 250 ng of total RNA and the High-Capacity Reverse Transcription Kit (Applied Biosystems, Paisley, UK). RT-specific primers for mouse miRNAs miR-34a, miR-92a and miR-134 (Applied Biosystems) were used for all miRNA reverse transcription. Individual qPCRs were carried out on the 7900HT Fast Realtime System (Applied Biosystems) using miR-34a-, miR-92a- and miR-134-specific Taqman miRNA assays (Applied Biosystems). RNU6B was used for normalization of miRNA expression levels. A relative fold change in expression of the target gene transcript was determined using the comparative cycle threshold method (2−ΔΔCT).
The presence of a potential miR-34a consensus site (7 mer) in the 3′ UTR of the Bax mRNA was established using independent bioinformatic alignment tools (http://www.microrna.org and http://www.targetscan.org).
Western blotting
Hippocampal CA3 subfields were homogenized in a lysis buffer, boiled in gel-loading buffer and separated on SDS-PAGE gels. Proteins were electroporated onto nitrocellulose membranes and incubated with antibodies against Argonaute-2, Caspase-3 (Cell Signaling Technology, Beverly, MA, USA), Map3k9 (a gift from R Stallings), β-actin and Bax (Santa Cruz Biotechnology, Santa Cruz, CA, USA). Membranes were then incubated with horseradish peroxidase-conjugated secondary antibodies (Jackson ImmunoResearch, Plymouth, PA, USA) and bands visualized using Supersignal West Pico chemiluminescence (Pierce, Rockford, IL, USA). Images were captured using a Fuji-Film LAS-300 (Fuji, Sheffield, UK) and densitometry performed using the AlphaEaseFC4.0 gel-scanning integrated optical density software (Alpha Innotech, San Leandaro, CA, USA).
Immunoprecipitation of Ago-2
The association between miRNAs and Ago-2 was investigated as described earlier.7 The CA3 subfields from three individual mice were pooled for each sample and homogenized in 0.7 ml of ice-cold immunoprecipitation buffer (300 mM NaCL, 5 mM MgCl2, 0.1% NP-40, 50 mM Tris HCl, pH 7.5). The homogenate was centrifuged at 16 000 × g for 15 min at 4 °C and the supernatant was retained. Antibodies against Ago-2 were added to 400 μg of lysate in a final volume of 1 ml, vortex-mixed and incubated overnight at 4 °C. Next, 20 μl of 50% Protein-A/G-agarose beads (Biotechnology) was added for 1 h at 4 °C and then bead complexes centrifuged at 16 000 × g for 15 min at 4 °C. The pellet was washed in immunoprecipitation buffer, and miRNA was extracted using the miRNeasy kit (Qiagen, West Sussex, UK). Stem–loop reverse transcription and RT PCR (Applied Biosystems) was performed as above to semiquantify the expression of the miRNA.
Histopathology
Cryosections (12 μm) were prepared at the level of either rostral (AP=−1.58 mm) or medial (AP=−1.82 mm) hippocampus. To assess neuronal death, sections were stained using FJB. Briefly, tissue sections were air-dried, postfixed in formalin (10%) and then immersed in 0.006% potassium permanganate solution. Sections were then rinsed and placed in 0.001% FJB solution in 0.1% acetic acid (Chemicon Europe Ltd, Chandlers Ford, UK). Sections were rinsed again, dried, cleared and mounted in DPX (Sigma-Aldrich). DNA damage was analyzed on fresh-frozen sections using a fluorescein-based TUNEL technique, according to the manufacturer's instructions (Promega, Madison, WI, USA), as described.11 Sections were examined using a Nikon 2000s epifluorescence microscope (Micron Optical Co. Ltd, Enniscorthy, Ireland) under Ex/Em wavelengths of 472/520 nm (green) and imaged using a Hamamatsu Orca 285 camera (Micron Optical Co. Ltd). Images were processed using Adobe Photoshop 6.0 (Adobe Systems Software Ireland Limited, Dublin, Ireland). Cell counts were performed for the entire CA3 subfield, beginning at the border with CA2 through to the end of CA3c/CA4 within the hilus of the dentate gyrus. Counts were the average of two adjacent sections assessed by an observer blinded to the experimental group/condition.
Data analysis
All data are presented as mean±S.E.M. Two group comparisons were made using Student's t-test, whereas multigroup comparisons were made using analysis of variance followed by appropriate post hoc testing. Significance was accepted at P<0.05.
Abbreviations
- CA:
-
cornu ammonis
- EEG:
-
electroencephaologram
- FJB:
-
Fluoro-Jade B
- i.c.v.:
-
intracerebroventricular
- KA:
-
kainic acid
- HAHFDs:
-
high-amplitude high-frequency discharges
- MAP3K9:
-
mitogen-activated protein kinase kinase kinase 9
- miRNAs:
-
MicroRNAs
- miR:
-
MicroRNA
- RT-qPCR:
-
real-time quantitative
- RISC:
-
RNA-induced silencing complex
- TUNEL:
-
terminal deoxynucleotidyl dUTP nick end labeling
References
Bartel DP . MicroRNAs: genomics, biogenesis, mechanism, and function. Cell 2004; 116: 281–297.
Kim VN, Han J, Siomi MC . Biogenesis of small RNAs in animals. Nat Rev Mol Cell Biol 2009; 10: 126–139.
Peters L, Meister G . Argonaute proteins: mediators of RNA silencing. Mol Cell 2007; 26: 611–623.
Eacker SM, Dawson TM, Dawson VL . Understanding microRNAs in neurodegeneration. Nat Rev Neurosci 2009; 10: 837–841.
Aronica E, Fluiter K, Iyer A, Zurolo E, Vreijling J, van Vliet EA et al. Expression pattern of miR-146a, an inflammation-associated microRNA, in experimental and human temporal lobe epilepsy. Eur J Neurosci 2010; 31: 1100–1107.
Hu K, Zhang C, Long L, Long X, Feng L, Li Y et al. Expression profile of microRNAs in rat hippocampus following lithium-pilocarpine-induced status epilepticus. Neurosci Lett 2011; 488: 252–257.
Jimenez-Mateos EM, Bray I, Sanz-Rodriguez A, Engel T, McKiernan R, Mouri G et al. MicroRNA expression profile after status epilepticus and hippocampal neuroprotection by targeting miR-132. Am J Pathol 2011; 179: 2519–2532.
Riley T, Sontag E, Chen P, Levine A . Transcriptional control of human p53-regulated genes. Nat Rev Mol Cell Biol 2008; 9: 402–412.
Sakhi S, Bruce A, Sun N, Tocco G, Baudry M, Schreiber SS . p53 induction is associated with neuronal damage in the central nervous system. Proc Natl Acad Sci USA 1994; 91: 7525–7529.
Liu W, Rong Y, Baudry M, Schreiber SS . Status epilepticus induces p53 sequence-specific DNA binding in mature rat brain. Brain Res Mol Brain Res 1999; 63: 248–253.
Engel T, Murphy BM, Hatazaki S, Jimenez-Mateos EM, Concannon CG, Woods I et al. Reduced hippocampal damage and epileptic seizures after status epilepticus in mice lacking proapoptotic Puma. FASEB J 2010; 24: 853–861.
Morrison RS, Wenzel HJ, Kinoshita Y, Robbins CA, Donehower LA, Schwartzkroin PA . Loss of the p53 tumor suppressor gene protects neurons from kainate- induced cell death. J Neurosci 1996; 16: 1337–1345.
Culmsee C, Zhu X, Yu QS, Chan SL, Camandola S, Guo Z et al. A synthetic inhibitor of p53 protects neurons against death induced by ischemic and excitotoxic insults, and amyloid beta-peptide. J Neurochem 2001; 77: 220–228.
Engel T, Hatazaki S, Tanaka K, Prehn JH, Henshall DC . Deletion of puma protects hippocampal neurons in a model of severe status epilepticus. Neuroscience 2010; 168: 443–450.
Engel T, Tanaka K, Jimenez-Mateos EM, Caballero-Caballero A, Prehn JH, Henshall DC . Loss of p53 results in protracted electrographic seizures and development of an aggravated epileptic phenotype following status epilepticus. Cell Death Dis 2010; 1: e79.
Schauwecker PE, Steward O . Genetic determinants of susceptibility to excitotoxic cell death: implications for gene targeting approaches. Proc Natl Acad Sci USA 1997; 94: 4103–4108.
Hermeking H . The miR-34 family in cancer and apoptosis. Cell Death Differ 2010; 17: 193–199.
Welch C, Chen Y, Stallings RL . MicroRNA-34a functions as a potential tumor suppressor by inducing apoptosis in neuroblastoma cells. Oncogene 2007; 26: 5017–5022.
Raver-Shapira N, Marciano E, Meiri E, Spector Y, Rosenfeld N, Moskovits N et al. Transcriptional activation of miR-34a contributes to p53-mediated apoptosis. Mol Cell 2007; 26: 731–743.
Chang TC, Wentzel EA, Kent OA, Ramachandran K, Mullendore M, Lee KH et al. Transactivation of miR-34a by p53 broadly influences gene expression and promotes apoptosis. Mol Cell 2007; 26: 745–752.
He L, He X, Lim LP, de Stanchina E, Xuan Z, Liang Y et al. A microRNA component of the p53 tumour suppressor network. Nature 2007; 447: 1130–1134.
Tarasov V, Jung P, Verdoodt B, Lodygin D, Epanchintsev A, Menssen A et al. Differential regulation of microRNAs by p53 revealed by massively parallel sequencing: miR-34a is a p53 target that induces apoptosis and G1-arrest. Cell Cycle 2007; 6: 1586–1593.
Agostini M, Tucci P, Steinert JR, Shalom-Feuerstein R, Rouleau M, Aberdam D et al. microRNA-34a regulates neurite outgrowth, spinal morphology, and function. Proc Natl Acad Sci USA 2011; 108: 21099–21104.
Choi YJ, Lin CP, Ho JJ, He X, Okada N, Bu P et al. miR-34 miRNAs provide a barrier for somatic cell reprogramming. Nat Cell Biol 2011; 13: 1353–1360.
Tivnan A, Tracey L, Buckley PG, Alcock LC, Davidoff AM, Stallings RL . MicroRNA-34a is a potent tumor suppressor molecule in vivo in neuroblastoma. BMC Cancer 2011; 11: 33.
Kaller M, Liffers ST, Oeljeklaus S, Kuhlmann K, Roh S, Hoffmann R et al. Genome-wide characterization of miR-34a induced changes in protein and mRNA expression by a combined pulsed SILAC and microarray analysis. Mol Cell Proteomics 2011; 10: M111. 010462.
Komarov PG, Komarova EA, Kondratov RV, Christov-Tselkov K, Coon JS, Chernov MV et al. A chemical inhibitor of p53 that protects mice from the side effects of cancer therapy. Science 1999; 285: 1733–1737.
Wood DE, Newcomb EW . Cleavage of Bax enhances its cell death function. Exp Cell Res 2000; 256: 375–382.
Song YJ, Tian XB, Zhang S, Zhang YX, Li X, Li D et al. Temporal lobe epilepsy induces differential expression of hippocampal miRNAs including let-7e and miR-23a/b. Brain Res 2011; 1387: 134–140.
Saugstad JA . MicroRNAs as effectors of brain function with roles in ischemia and injury, neuroprotection, and neurodegeneration. J Cereb Blood Flow Metab 2010; 30: 1564–1576.
Mouri G, Jimenez-Mateos E, Engel T, Dunleavy M, Hatazaki S, Paucard A et al. Unilateral hippocampal CA3-predominant damage and short latency epileptogenesis after intra-amygdala microinjection of kainic acid in mice. Brain Res 2008; 1213: 140–151.
Murphy B, Dunleavy M, Shinoda S, Schindler C, Meller R, Bellver-Estelles C et al. Bcl-w protects hippocampus during experimental status epilepticus. Am J Pathol 2007; 171: 1258–1268.
Haramati S, Navon I, Issler O, Ezra-Nevo G, Gil S, Zwang R et al. microRNA as repressors of stress-induced anxiety: the case of amygdalar miR-34. J Neurosci 2011; 31: 14191–14203.
Green DR, Kroemer G . Cytoplasmic functions of the tumour suppressor p53. Nature 2009; 458: 1127–1130.
Engel T, Murphy BM, Schindler CK, Henshall DC . Elevated p53 and lower MDM2 expression in hippocampus from patients with intractable temporal lobe epilepsy. Epilepsy Res 2007; 77: 151–156.
Xu S, Pang Q, Liu Y, Shang W, Zhai G, Ge M . Neuronal apoptosis in the resected sclerotic hippocampus in patients with mesial temporal lobe epilepsy. J Clin Neurosci 2007; 14: 835–840.
Sohn D, Graupner V, Neise D, Essmann F, Schulze-Osthoff K, Janicke RU . Pifithrin-alpha protects against DNA damage-induced apoptosis downstream of mitochondria independent of p53. Cell Death Differ 2009; 16: 869–878.
Christoffersen NR, Shalgi R, Frankel LB, Leucci E, Lees M, Klausen M et al. p53-independent upregulation of miR-34a during oncogene-induced senescence represses MYC. Cell Death Differ 2010; 17: 236–245.
Agostini M, Tucci P, Killick R, Candi E, Sayan BS, Rivetti di Val Cervo P et al. Neuronal differentiation by TAp73 is mediated by microRNA-34a regulation of synaptic protein targets. Proc Natl Acad Sci USA 2011; 108: 21093–21098.
Sotillo E, Laver T, Mellert H, Schelter JM, Cleary MA, McMahon S et al. Myc overexpression brings out unexpected antiapoptotic effects of miR-34a. Oncogene 2011; 30: 2587–2594.
Acknowledgements
We thank Isabella Bray for helpful advice and Raymond L Stallings for the gift of the Map3k9 antibody. This work was supported by the Science Foundation Ireland grant 08/IN1/B1875, the Health Research Board PHD/2007/11 and a postdoctoral fellowship from the Irish Research Council for Science Engineering and Technology (to E J-M).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Additional information
Edited by A Verkhratsky
Supplementary Information accompanies the paper on Cell Death and Disease website
Supplementary information
Rights and permissions
This work is licensed under the Creative Commons Attribution-NonCommercial-No Derivative Works 3.0 Unported License. To view a copy of this license, visit http://creativecommons.org/licenses/by-nc-nd/3.0/
About this article
Cite this article
Sano, T., Reynolds, J., Jimenez-Mateos, E. et al. MicroRNA-34a upregulation during seizure-induced neuronal death. Cell Death Dis 3, e287 (2012). https://doi.org/10.1038/cddis.2012.23
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/cddis.2012.23
Keywords
This article is cited by
-
Increased hippocampal excitability in miR-324-null mice
Scientific Reports (2021)
-
A microRNA signature of toxic extrasynaptic N-methyl-D-aspartate (NMDA) receptor signaling
Molecular Brain (2020)
-
MicroRNAs as regulators of brain function and targets for treatment of epilepsy
Nature Reviews Neurology (2020)
-
Signature of Aberrantly Expressed microRNAs in the Striatum of Rotenone-Induced Parkinsonian Rats
Neurochemical Research (2018)
-
2R,4R-APDC, a Metabotropic Glutamate Receptor Agonist, Reduced Neuronal Apoptosis by Upregulating MicroRNA-128 in a Rat Model After Seizures
Neurochemical Research (2018)