Abstract
Non-small cell lung cancers (NSCLC), in particular adenocarcinoma, are often mixed with normal cells. Therefore, low sensitivity of direct sequencing used for K-Ras mutation analysis could be inadequate in some cases. Our study focused on the possibility to increase the detection of K-Ras mutations in cases of low tumour cellularity. Besides direct sequencing, we used wild-type hybridisation probes and peptide-nucleic-acid (PNA)-mediated PCR clamping to detect mutations at codons 12 and 13, in 114 routine consecutive NSCLC frozen surgical tumours untreated by targeted drugs. The sensitivity of the analysis without or with PNA was 10 and 1% of tumour DNA, respectively. Direct sequencing revealed K-Ras mutations in 11 out of 114 tumours (10%). Using PNA-mediated PCR clamping, 10 additional cases of K-Ras mutations were detected (21 out of 114, 18%, P<0.005), among which five in samples with low tumour cellularity. In adenocarcinoma, K-Ras mutation frequency increased from 7 out of 55 (13%) by direct sequencing to 15 out of 55 (27%) by clamped-PCR (P<0.005). K-Ras mutations detected by these sensitive techniques lost its prognostic value. In conclusion, a rapid and sensitive PCR-clamping test avoiding macro or micro dissection could be proposed in routine analysis especially for NSCLC samples with low percentage of tumour cells such as bronchial biopsies or after neoadjuvant chemotherapy.
Similar content being viewed by others
Main
Malignant transformations are the result of an accumulation of carcinogenesis steps corresponding to activation of oncogenes and inactivation of tumour suppressor genes (Bishop, 1991). Among the available candidates, the K-Ras proto-oncogene is the most well-studied cellular gene whose alterations seem to have an important role in the pathogenesis of human cancer. K-Ras oncogene is a known downstream signaling molecule in the EFGR-signaling pathway. K-Ras gene encodes a 21 kDa GTP-binding protein, which controls the mechanisms of cell growth and differentiation. Point mutations in the K-Ras gene lead to uncontrolled stimulation of Ras-related functions by altered p21ras protein, locking it in the ‘on’ position for signal transduction (Adjei, 2001; Molina and Adjei, 2007).
Non-small cell lung cancers (NSCLC) represent more than 80% of lung cancers and are subgrouped in squamous cell carcinomas (SCC), adenocarcinoma (ADC) and large cell carcinoma (Travis et al, 2004). K-Ras mutations are found in 10–20% of NSCLC and have been described in approximately 30% of ADC (Ahrendt et al, 2001). About 92% of K-Ras mutations occur in codon 12 (Huncharek et al, 1999). K-Ras mutations are most closely associated with a history of cigarette smoking and are more common in women (Ahrendt et al, 2001; Broermann et al, 2002; Sugio et al, 2006; Tam et al, 2006). Oncogenic activation of K-Ras has been reported as a prognostic marker of poor outcome in NSCLC patients and K-Ras mutations seemed to be associated with a shorter survival in early-stage and locally advanced NSCLC (Fukuyama et al, 1997; Huncharek et al, 1999). A recent meta-analysis of K-Ras mutations in lung cancer showed that these mutations appeared to be associated with shorter survival in NSCLC (Mascaux et al, 2005). It was also suggested that K-Ras mutations could be predictive of chemotherapy resistance, in metastatic disease rather in adjuvant situation (Eberhard et al, 2005; Tsao et al, 2007). Although meta-analyses has indicated that K-Ras gene mutations are weak prognostic markers of poorer outcome in NSCLC, results from individual studies have been inconsistent (Huncharek et al, 1999; Mascaux et al, 2005; Tsao et al, 2007).
At first, EGFR status is a decisive molecular factor for using EGFR-targeted therapies in NSCLC (Lynch et al, 2004; Paez et al, 2004; Pao et al, 2004). K-Ras and EGFR mutations were shown to be mutually exclusive in lung ADC (Kosaka et al, 2004). Mutations in K-Ras are found more frequently in patients who develop disease progression upon gefinitib or erlotinib therapy (Pao et al, 2005). Both the time to disease progression and the median survival were significantly worse in patients with K-Ras mutations when they were treated with erlotinib in combination with chemotherapy compared with those receiving chemotherapy alone (Eberhard et al, 2005). It was suggested that one potential mechanism for primary resistance to EGFR-TKI may be the presence of K-Ras mutations (Massarelli et al, 2007). These recent advances within molecular biology may facilitate treatment selection based on potential predictive molecular markers such as K-Ras.
Direct sequencing is considered as the gold standard and has allowed comprehensive knowledge of mutations (Lynch et al, 2004; Paez et al, 2004; Pao et al, 2004, 2005; Massarelli et al, 2007). Direct sequencing is still widely employed to discover ‘new’ mutations. But the sensitivity of direct sequencing depends on the percentage of tumour cells in the analysed sample. A percentage of more than 50% of tumour cells is usually requested and the threshold of detection is around 25% of mutant DNA into a wild-type environment (Pao and Ladanyi, 2007; Eberhard et al, 2008). If a low percentage of tumour cells is present in some samples, direct sequencing could lead to false-negative results. Thus, direct sequencing considered as the gold standard could be inadequate in such cases, even in surgical specimens, resulting in differences in K-Ras mutations frequencies and in prognostic/predictive values of such mutations. Besides classical sequencing, K-Ras mutations could be detected by mutation-specific oligonucleotide hybridisation, PCR followed by restriction fragment length polymorphisms analysis, single-strand conformation polymorphisms analysis or mutant allelic-specific amplification. These procedures involve multiple steps and/or are time-consuming. Therefore, they are impracticable for routine clinical use.
To detect a minimal amount of mutant DNA in clinical samples, peptide-nucleic-acid (PNA) oligomers have been developed (Orum et al, 1993). PNAs are non-extendable oligonucleotides in which the ribose-phosphate backbone is replaced by 2-aminoethyl glycine units linked by amide bonds. In PNA-mediated PCR clamping, PNA oligomers suppress the amplification of the complementary sequence confined by a pair of DNA oligonucleotide primers because PNA are not substrate for DNA polymerase. The PNA-clamped probe assay is more sensitive than direct sequencing, with the ability to detect mutations in samples containing less than 1% mutant alleles (Nagai et al, 2005; Pao and Ladanyi, 2007). Using this method, c-Kit point mutations have been detected in skin biopsy samples from patients with urticaria pigmentosa (Sotlar et al, 2003). Such a technique has been applied to search for K-Ras mutations in various tumour samples (Sun et al, 2002; Chen et al, 2004; Taback et al, 2004; Däbritz et al, 2005; Luo et al, 2006; Miyake et al, 2007). This method was also used to detect EGFR mutations in NSCLC (Nagai et al, 2005; Soh et al, 2006; Sutani et al, 2006; Tanaka et al, 2007; Miyanaga et al, 2008).
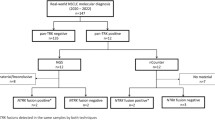
As NSCLC, in particular adenocarcinoma, could often be mixed with normal cells, the aim of this study was to estimate the possibility to increase the sensitivity of the detection of K-Ras mutations on an EGFR-targeted naive NSCLC cohort, even in cases of low tumour cellularity and to evaluate its routine clinical usefulness. To be able to compare the results of detection of K-Ras mutations by a sensitive technique and by direct sequencing, we chose to work on frozen samples of NSCLC. We conducted this study to establish a one-step real-time PCR method that combines fluorescent hybridisation probes PCR without or with competing wild-type PNA 17-mer and melting curve analysis for the detection of K-Ras mutations at codon 12 and 13, in a cohort of 114 consecutive surgical frozen NSCLC tumour tissues.
Materials and methods
Patients
Anonymised frozen samples from 114 routine consecutive NSCLC patients surgically treated were obtained from the Biological Resource Center of the University Hospital of Strasbourg, in protocols approved by the institutional review board. Stage was defined as recommended (Moutain, 1997). All patients are chemo- and targeted drug naive at the time of surgery. All the patients are non-Asian. The patients included 91 men and 23 women. Only seven (6%) of the patients were never smokers. The observation period ranged from 1 to 82 months, with a median follow-up of 26 months. Patients’ characteristics are summarized in Table 1. Tumour and paired normal lung peripheral tissue samples obtained at the time of surgery, were immediately stored at −80°C. Tumours were histologically classified according to the World Health Organization guidelines and scored for differentiation (Travis et al, 2004). Three haematoxylin and eosin-stained sections of frozen tissues were reviewed by a pathologist to evaluate the percentage of tumour cells, at the beginning, middle and end of the frozen tissues. The percentage of tumour cells corresponds to the number of tumour cells reported to the number of all the cells (tumour and non-tumour cells) analysed on a slide. Almost half of the patients presented less than 50% of tumour cells. Histological characteristics are summarized in Table 1.
DNA extraction from frozen lung cancer tumours
Genomic DNA was isolated using conventional techniques with QIAamp DNA kit (Qiagen, Courtaboeuf, France). To validate the percentage of tumour cells assessed by the pathologist in the frozen samples, paired tumour and normal DNA were amplified by fluorescent polymerase chain reaction (PCR) for microsatellite (MS) analysis with a panel of markers distributed among the genome on 13 chromosomes frequently altered in NSCLC (data not shown). Detailed MS and PCR conditions are available upon request.
DNA sequencing analysis
The mutational status of K-Ras (codon 12,13) was performed using 40 ng of genomic DNA amplified by PCR in 25 μl reaction mix containing 1.25 U Fast Start High Fidelity Taq (Roche), 0.2 mM dNTP, 1.5 mM MgCl2, and 0.2 μm of K-Ras F and K-Ras R I primers (Table 2). After an initial denaturation (2 min at 94°C), a touch down protocol was used as follows: 10 cycles with a decreased hybridisation temperature from 61 to 58°C every two cycles. The subsequent 35 cycles were performed as follows: 50 s at 93°C, 50 s at 55°C, and 1 min 30 s at 72°C, followed by a final extension period of 10 min at 72°C. All PCR products were verified by electrophoresis on agarose gels. After purification (Microcon-PCR Filter Unit, Millipore, Paris, France), the PCR products were sequenced (Big Dye Terminator v1.1 Cycle sequencing kit, Applied Biosystems, Forster City, CA, USA) and analysed on ABI PRISM 3100 Genetic Analyser (Applied Biosystems). The GB sequence of human K-Ras (L00045) was used as a reference for sequence analysis (Seqscape v2.5, Applied Biosystems). All sequencing reactions were performed in both forward and reverse directions, and all mutations were confirmed by sequencing a second independent PCR product. As expected, by direct sequencing technique for K-Ras mutation analysis, K-Ras mutations were reproducibly detectable at a dilution of 25% of mutated DNA into normal DNA (data not shown). All the mutated K-Ras DNA were also sequenced for EGFR mutation analysis as described earlier (Beau-Faller et al, 2008).
Real-time PCR and melting curve analysis, clamped-probe assay
Primers were chosen to amplify a specific 243-bp genomic fragment from K-Ras codon 12 and 13. Hybridisation FRET probes were designed complementary to wild-type sequence of codon 12 and 13. The anchor probe was 5′-labeled with LC-Red 640 and 3′ phosphorylated, and the sensor probe was 3′-labeled with fluorescein. The PNA oligomer covered codons 10–14 wild-type sequence. Sequences of primers (Eurogentec, Liège, Belgium), probes (Timolbiol, Berlin, Germany), and 17 mer-PNA (Eurogentec, Liège, Belgium) are listed in Table 2. They are represented in Figure 1. Real-time PCR was performed with 20 ng of genomic DNA, in a final volume of 20 μl containing Light Cycler Fast Start DNA Master Hyb Probe (Roche Diagnostics, Mannheim, Germany), 3 mM MgCl2, 0.4 μ M of each primers K-Ras, 0.4 μ M of K-Ras hybridisation sensor probe and 0.2 μ M of K-Ras hybridisation anchor probe, without or with 0.1 μ M PNA oligomer. After the initial denaturation step at 95°C for 10 min, a touch down amplification was performed consisting of a denaturation at 95°C for 10, 7 s at 76°C, then 10 cycles with touchdown annealing for 15 s from 65 to 55°C (decreasing 2°C/two cycles) and elongation at 65°C for 20 s. This step was followed by 28 cycles: 95°C for 10 s, 76°C for 7 s, 50°C for 15 s, 65°C for 20 s. Melting curve analysis was performed by increasing temperature from 40 to 95°C with a transition rate of 0.25°Cs−1. Fluorescence data were analysed using the Light Cycler software (software version 3.5, Roche Diagnostics). Mutation analysis for each tumour sample was performed at least two times. PNA–PCR products from all samples that gave positive results by the clamped-probe assay was sequenced to confirm and precise the type of K-Ras mutation.
Controls
DNA from a lung cancer cell line A549 with a homozygous K-Ras codon 12 mutation (c.34G>A, G12S) was used for homozygous K-Ras mutation positive control. One negative control (DNA from colon cancer cell line HT29 of colon carcinoma with wild-type K-Ras sequence) and a no template negative control (as control for contamination) were processed in parallel. We evaluate the sensitivity of the developed alternative methods by serially diluting DNA from A549 mutated K-Ras cell line in the DNA of wild-type K-Ras HT29 cell line (Figure 2).
Serial dilution experiments showing the sensitivity of the alternative techniques for K-Ras mutation detection: hybridisation assay without PNA (A) and PNA-clamped probe assay (B). DNA from A549 (lung adenocarcinoma) cell line, which harbours an homozygous K-Ras mutation (G12S), was diluted into DNA from a wild-type K-Ras HT29 cell line.
Statistical analysis
A total number of patients to be tested by PNA–PCR clamp was decided to be more than 100 patients because about 15–20% of NSCLC patients were reported to have K-Ras mutations in previous articles (Mascaux et al, 2005). Statistical analysis using χ2 test or exact test (type Fisher's test) if appropriate with exact P-values was used to compare the qualitative data. Where appropriate, continuous variables were categorized before analysis. The date of point was 30 April 2008. The Kaplan–Meier method was used to estimate the probability of event-free survival and the log-rank test to detect the difference in survival curves. Cox's proportional hazard models were used to determine the impact of patient characteristics on event-free survival. All statistical calculations were performed with the Statistical Package for the Social Science (SPSS) (number 15.0) statistical software.
Results
Sequence analysis of NSCLC samples
We first analysed the 114 routine samples by direct sequencing for K-Ras mutation detection. By this technique, 11 (10%) of the 114 cases showed a K-Ras mutation at codon 12 or 13, represented by five mutations G12C, two mutations G12D, two mutations G12V, one mutation G12R and one mutation G12A (Tables 3 and 4).
Determination of the sensitivity of the hybridisation-probe assay and clamped-probe assay
The tumour cell count was lower than 50% in 52 patients, and among them lower than 25% in 15 patients (Table 1). To further improve the detection of K-Ras mutations in comparison with direct sequencing, we developed real-time PCR with wild-type hybridisation probes without or with PNA-mediated clamped PCR. We assessed the sensitivity of these assays by testing homozygous G12S K-Ras mutated A549 cell line DNA serially diluted into DNA from wild-type K-Ras HT29 cell line DNA. By hybridisation-probe assay, the mutations were reproducibly detectable at a dilution of 10% of mutated DNA into wild-type DNA and by the clamped-probe assay, at a dilution of 1% of mutated DNA into wild-type DNA (Figure 2). Indeed, in our conditions, addition of PNA allows to increase the threshold detection of K-Ras mutation by a magnitude of 10.
Hydridisation-probe and clamped-probe assays for detecting K-Ras mutations. Comparison with direct sequencing
All the 114 patients were then analyzed for K-Ras mutations by hybridisation-probe assay and clamped-probe assay (Table 2). As expected, the 11out of 114 (10%) tumours with a K-Ras mutation at codon 12 or 13 detected by direct sequencing, were also detected by hybridisation-probe/clamped-probe assays. However, five tumours with wild-type K-Ras assessed by direct sequencing presented K-Ras mutations when using the hybridisation-probe assay. Remarkably, five other tumours with wild-type K-Ras assessed by direct sequencing and by the hybridisation-probe assay presented K-Ras mutations when using clamped-probe assay alone. As expected, all the positive samples detected by hybridisation-probe assay were also positive for clamped-probe assay. Thus, these sensitive techniques allowed an increase in detection of K-Ras mutations from 11 out of 114 patients (10%) by direct sequencing to 21 out of 114 (18%) (P<0.005). To confirm the mutations in the 10 tumours only detected by these sensitive techniques and to identify precisely the type of K-Ras mutation, all PNA–PCR products were directly sequenced for codon 12 and 13 of K-Ras. We identified five mutations G12C, three mutations G12D, one mutation G12S and one mutation G13C with hybridisation-probe/clamped-probe assays (Tables 3 and 4, Figure 3).
Representative melting curves obtained by hybridisation and clamped-probe assays. On the right side, paired electropherograms obtained by sequencing of a PCR product, without and with PNA. (A) K-Ras mutation (G12D) diagnosed by the two alternative techniques: hybridisation probe and clamped-PCR assays (No. 63). (B) K-Ras mutation (G12D) only diagnosed by the most sensitive technique: clamped-PCR (No. 1103).
Among the K-Ras mutated tumours diagnosed only by hybridisation/PNA techniques, five had a percentage of tumour cells effectively lower than required for classical sequencing. The tumour cellularity of these tumours was 15% (one patient), 10% (one patient) and less than 10% (three patients). K-Ras mutations in two of these tumours were detected by hybridisation-probe assay and three others by clamped-probe assay only. In another hand, five K-Ras mutated tumours diagnosed only by hybridisation/PNA techniques, presented a percentage of tumour cells usually sufficient for direct sequencing, suggesting the presence of mutated tumour subclones.
Clinical data and K-Ras mutations detected by the different methods
Then, we asked for the clinical usefulness of K-Ras mutations detected by these sensitive techniques. Our cohort of 114 surgically treated NSCLC patients were represented by 55 ADC and 59 SCC (Table 1). The 11 K-Ras mutations detected by direct sequencing were found in seven ADC (two with BAC features) and in four SCC (Tables 1 and 4). The 10 additional K-Ras mutations detected by hybridisation/PNA methods were observed in eight ADC and in two SCC. Overall, the 21 K-Ras mutated patients, 16 males and five females, 15 ADC and six SCC, have tumours from all stages and from current/former smokers. In adenocarcinoma, K-Ras mutation frequency increased from 7 out of 55 (13%) by direct sequencing to 15 (27%) by clamped-PCR (P<0.005). If there is no correlation between K-Ras mutation frequency detected by direct sequencing and histological subtypes, a correlation was found between K-Ras mutation frequency detected by hybridisation/PNA methods and ADC histological subtype (P=0.01). Survival analysis showed that the presence of K-Ras mutations diagnosed by direct sequencing are a weak prognostic marker of poorer outcome (median EFS 14 months vs 47 months, HR=1.57, CI 95%: 0.77–3.84, P=0.08). By contrast, when taking into account all the K-Ras mutations detected by the three techniques, our results failed to confirm K-Ras oncogenic activation as a significant marker of poor prognosis after surgery for NSCLC (median EFS 16 months vs 47 months, HR=1.19, CI 95%: 0.61–2.32, NS) (Figure 4).
Kaplan–Meier curves for event-free survival (months) of 114 NSCLC tumours. (A) Stratified according to K-Ras mutation analysed by direct sequencing (median EFS 14 months vs 47 months, HR=1.57, CI 95%: 0.77–3.84). (B) Stratified according to K-Ras mutation analysed by PCR clamp assay (median EFS 16 months vs 47 months, HR=1.19, CI 95%: 0.61–2.32).
Discussion
Surgical tumour specimens of NSCLC may contain a lot of normal/inflammatory cells. The presence of a high percentage of normal/inflammatory cells could lead to ‘false-negative’ results when mutations were detected by direct sequencing. A recent commentary synthetically addresses the question of the ideal method for EGFR mutation testing in lung cancer (Pao and Ladanyi, 2007), but no such data are available for K-Ras. We developed a quick, cheap and sensitive method for detecting K-Ras mutations from routine surgical specimens of NSCLC without removing contaminating normal cells by macro/micro dissection.
PNA–PCR clamp method can rapidly (within 2 h) detect K-Ras mutations using a low quantity of DNA. By contrast to other PNA studies, we used wild-type fluorescent-labelled hybridisation probes allowing rapid and high-sensitive detection of all the K-Ras mutations (Sun et al, 2002; Chen et al, 2004; Taback et al, 2004; Däbritz et al, 2005; Luo et al, 2006; Miyake et al, 2007). Only one pair of primers and one pair of probes are required to detect all possible mutations in codons 12 and 13 of the K-Ras gene. The detected fluorescence signal corresponds to the amplified mutant DNA and can be analysed by a subsequent melting curve analysis. If requested, the PNA–PCR products are available to precisely identify the mutated nucleotide. All these advantages greatly simplify the manipulating procedure.
The sensitivity of direct sequencing depends on the percentage of tumour cells in the analysed sample, generally up to 50% tumour cells is requested with a detection threshold of 25% mutant DNA into a wild-type environment (Pao and Ladanyi, 2007; Eberhard et al, 2008). The sensitivity of our assays is 10 and 1% of mutant DNA for hybridisation-probe assay and for clamped-probe assay, respectively, and might correspond to a more sensitive test, applicable for routine purposes without macro or micro dissection. Another new rapid method for mutated EGFR and K-Ras detection by high resolution melting analysis (HRM) has been recently reported (Do et al, 2008). Even HRM is a promising method, it can be compromised by a low proportion of tumour cells in the analysed sample and by the difficulty to detect homozygous mutations, as the sensitivity of K-Ras mutations detection was only 5–10%. Among the 10 new K-Ras mutated patients detected by these most sensitive methods, half presented a percentage of tumours cells under the level usually required for direct sequencing. Thus, even in a surgical cohort of NSCLC tumour samples, there is a risk of false-negative K-Ras mutated patients when they were analysed by direct sequencing. The rapidity and sensitivity of our sensitive technique could lead us to propose this test for routine K-Ras mutation detection, that is, bronchial biopsies in NSCLC.
In our study, the 10 new K-Ras-mutated cases presented clinical/biological characteristics usually associated with K-Ras mutations in NSCLC (Ahrendt et al, 2001; Broermann et al, 2002; Sugio et al, 2006; Tam et al, 2006). Remarkably, none of the five new K-Ras mutated patients with more than 50% of tumour cells, presented an EGFR mutation (exon 18, 19, 20, 21) (data not shown). Interestingly, if K-Ras mutations diagnosed by direct sequencing appeared to be a prognostic marker of poorer outcome in our cohort of surgically treated NSCLC patients, this tendency is not more observed when we considered K-Ras mutations diagnosed by the two other techniques (hybridisation probe alone, or with clamped-PCR). Our survival analysis is nevertheless limited by the relatively short follow-up with fewer than half of the patients having relapsed or died. Accordingly, a recent study (JBR.10) showed that mutations of K-Ras gene were neither prognostic for survival nor predictive of a differential benefit from adjuvant chemotherapy in stage IB and II NSCLC (Tsao et al, 2007). In this study, the tumour cellularity was enriched by microdissection, and using allelic-specific oligonucleotide hybridisation, they failed to confirm K-Ras oncogenic activation as a significant marker of poor prognosis after surgery for NSCLC. The lack of prognostic value of all the K-Ras mutated cases could be explained by the fact that in cases of mutation detected by sensitive techniques, the real percentage of K-Ras mutated cells could be too low, under a threshold with immediate clinical significance. Further studies are required to precisely determinate the significant prognostic threshold of K-Ras mutated cells.
In our study, half of the new K-Ras mutated cases diagnosed only by sensitive techniques, presented a percentage of tumour cells above the threshold usually required for direct sequencing. These results suggest the presence of mutated subclones in the tumour. In fact, direct sequencing could fail to detect mutated subclones (Pao and Ladanyi, 2007). Some EGFR-mutated subclones were already detected in NSCLC when EGFR T790M mutations have been analysed with sensitive techniques (Inukai et al, 2006). It was suggested that the possible presence of such mutations at a low frequency in NSCLC tumours before EGFR-targeted therapy might affect the tumour response or the event-free survival after targeted treatments. Recently, K-Ras mutations detected by allelic discrimination on tumour DNA, have been demonstrated to be an independent prognostic factor in patients with advanced colorectal cancer treated with cetuximab (Lièvre et al, 2008). To our knowledge, no predictive studies have been realised to identify K-Ras mutated subclones in NSCLC, but the presence of such mutated subclones could explain some cases of secondary EGFR-targeted therapy resistance. Therefore, it would be important to evaluate the predictive value of such K-Ras mutated tumour subclones, particularly in stabilised or progressive cases treated by targeted EGFR therapy.
Consequently, the percentage of tumour cells in the analyzed sample as well as the threshold of mutation detection of the currently molecular test appeared to be two essential data to better understand the significance (i.e., prognostic or predictive factor) of the detected mutation. Indeed, in our cohort of surgical specimen, 53 (46.5%) of our routine consecutive patients presented a percentage of tumour cells under the value (50%) classically required for direct sequencing; and in addition, some patients with a percentage of tumour cells sufficient for direct sequencing, appeared to have K-Ras mutations at a low frequency. In the first type of tumours, a sensitive technique will detect low level of K-Ras mutations with finally a number of K-Ras mutated tumour cells which could have clinical usefulness; in the second type of tumours, sensitive technique will detect K-Ras-mutated subclones of which clinical usefulness has still to be explored.
In conclusion, our study allows us to propose an easy and sensitive method for rapid analysis of K-Ras mutations in NSCLC tumours. This sensitive technique could be helpful for specimens of lung cancer without removing contaminating normal cells, mostly in the setting of NSCLC, in which diagnoses are often based on bronchial biopsies or cytologic specimens. The prognostic value of such sensitive detected K-Ras mutations when tacking into account the tumour cellularity, has still to be evaluated on an increased number of surgically treated lung cancer patients, taking into account the frequency of mutated allele in the sample depending on the tumour cellularity. Furthermore, predictive value of low represented K-Ras mutations need to be assessed in lung cancer patients treated by targeted anti-EGFR treatments, to optimise such treatments in NSCLC patients.
Accession codes
Change history
16 November 2011
This paper was modified 12 months after initial publication to switch to Creative Commons licence terms, as noted at publication
References
Adjei AA (2001) Blocking oncogenic Ras signalling for cancer therapy. J Natl Cancer Inst 93 (14): 1062–1074
Ahrendt SA, Decker PA, Alawi EA, Zhu Yr YR, Sanchez-Cespedes M, Yang SC, Haasler GB, Kajdacsy-Balla A, Demeure MJ, Sidransky D (2001) Cigarette smoking is strongly associated with mutation of the K-ras gene in patients with primary adenocarcinoma of the lung. Cancer 92 (6): 1525–1530
Beau-Faller M, Ruppert AM, Voegeli AC, Neuville A, Meyer N, Guerin E, Legrain M, Mennecier B, Wihlm JM, Massard G, Quoix E, Oudet P, Gaub MP (2008) MET gene copy number in non-small cell lung cancer: molecular analysis in a targeted tyrosine kinase inhibitor naïve cohort. J Thorac Oncol 3 (4): 331–339
Bishop JM (1991) Molecular themes in oncogenesis. Cell 64 (2): 235–248
Broermann P, Junker K, Brandt BH, Heinecke A, Freitag L, Klinke F, Berdel WE, Thomas M (2002) Trimodality treatment in Stage III nonsmall cell lung carcinoma: prognostic impact of K-ras mutations after neoadjuvant therapy. Cancer 94 (7): 2055–2062
Chen C-Y, Shiesh SC, Wu SJ (2004) Rapid detection of K-ras mutations in bile by peptide nucleic acid-mediated PCR clamping and melting curve analysis: comparison with restriction fragment length polymorphism analysis. Cl Chemistry 50 (3): 481–489
Däbritz J, Hänfler J, Preston R, Stieler J, Oettle H (2005) Detection of Ki-ras mutations in tissue and plasma samples of patients with pancreatic cancer using PNA-mediated PCR clamping and hybridisation probes. Br J Cancer 92 (2): 405–412
Do H, Krypuy M, Mitchell PL, Fox SB, Dobrovic A (2008) High resolution melting analysis for rapid and sensitive EGFR and KRAS mutation detection in formalin fixed paraffin embedded biopsies. BMC Cancer 8 (142): 1–14
Eberhard DA, Giaccone G, Johnson BE (2008) Non-Small-Cell Lung Cancer Working Group Biomarkers of response to epidermal growth factor receptor inhibitors in Non-Small-Cell Lung Cancer Working Group: standardization for use in the clinical trial setting. J Clin Oncol 26 (6): 983–994
Eberhard DA, Johnson BE, Amler LC, Goddard AD, Heldens SL, Herbst RS, Ince WL, Jänne PA, Januario T, Johnson DH, Klein P, Miller VA, Ostland MA, Ramies DA, Sebisanovic D, Stinson JA, Zhang YR, Seshagiri S, Hillan KJ (2005) Mutations in the epidermal growth factor receptor and in KRAS are predictive and prognostic indicators in patients with non-small-cell lung cancer treated with chemotherapy alone and in combination with erlotinib. J Clin Oncol 23 (25): 5900–5909
Fukuyama Y, Mitsudomi T, Sugio K, Ishida T, Akazawa K, Sugimachi K (1997) K-ras and p53 mutations are an independent unfavourable prognostic indicator in patients with non-small-cell lung cancer. Br J Cancer 75 (8): 1125–1130
Huncharek M, Muscat J, Geschwind JF (1999) K-ras oncogene mutation as a prognostic marker in non-small cell lung cancer: a combined analysis of 881 cases. Carcinogenesis 20 (8): 1507–1510
Inukai M, Toyooka S, Ito S, Asano H, Ichihara S, Soh J, Suehisa H, Ouchida M, Aoe K, Aoe M, Kiura K, Shimizu N, Date H. (2006) Presence of epidermal growth factor receptor gene T790 M mutation as a minor clone in non-small cell lung cancer. Cancer Res 66 (16): 7854–7858
Kosaka T, Yatabe Y, Endoh H, Kuwano H, Takahashi T, Mitsudomi T (2004) Mutations of the epidermal growth factor receptor gene in lung cancer: biological and clinical implications. Cancer Res 64 (24): 8919–8923
Lièvre A, Bachet J-B, Boige V, Cayre A, Le Corre D, Buc E, Ychou M, Bouché O, Landi B, Louvet C, André T, Bibeau F, Diebold MD, Rougier P, Ducreux M, Tomasic G, Emile JF, Penault-Llorca F, Laurent-Puig P (2008) KRAS mutations as an independent prognostic factor in patients with advanced colorectal cancer treated with cetuximab. J Clin Oncol 26 (3): 374–379
Luo J-D, Chan EC, Shih CL, Chen TL, Liang Y, Hwang TL, Chiou CC (2006) Detection of rare mutant K-ras DNA in a single-tube reaction using peptide nucleic acid as both PCR clamp and sensor probe. Nucleic Acid Res 34 (2): e12
Lynch TJ, Bell DW, Sordella R, Gurubhagavatula S, Okimoto RA, Brannigan BW, Harris PL, Haserlat SM, Supko JG, Haluska FG, Louis DN, Christiani DC, Settleman J, Haber DA. (2004) Activating mutations in the epidermal growth factor receptor underlying responsiveness of non-small-cell lung cancer to gefitinib. N Engl J Med 350 (21): 2129–2139
Mascaux C, Iannini N, Martin B, Paesmans M, Berghmans T, Dusart M, Haller A, Lothaire P, Meert AP, Noel S, Lafitte JJ, Sculier JP (2005) The role of RAS oncogene in survival of patients with lung cancer: a systematic review of the literature with meta-analysis. Br J Cancer 92 (1): 131–139
Massarelli E, Varella-Garcia M, Tang X, Xavier AC, Ozburn NC, Liu DD, Bekele BN, Herbst RS, Wistuba (2007) KRAS mutation is an important predictor of resistance to therapy with epidermal growth factor receptor tyrosine kinase inhibitors in non-small-cell lung cancer. Clin Cancer Res 13 (10): 2890–2896
Miyake M, Sugano K, Kawashima K, Ichikawa H, Hirabayashi K, Kodama T, Fujimoto H, Kakizoe T, Kanai Y, Fujimoto K, Hirao Y (2007) Sensitive detection of FGFR3 mutations in bladder cancer and urine sediments by peptide nucleic acid-mediated real-time PCR clamping. Biochem Biophys Res Commun 362 (4): 865–871
Miyanaga A, Gemma A, Ando M, Kosaihira S, Noro R, Minegishi Y, Kataoka K, Nara M, Okano T, Miyazawa H, Tanaka T, Yoshimura A, Kobayashi K, Iwanami H, Hagiwara K, Tsuboi E, Kudoh S (2008) E-cadherin expression and epidermal growth factor receptor mutation status predict outcome in non-small cell lung cancer patients treated with gefitinib. Oncol Rep 19 (2): 377–383
Molina JR, Adjei AA (2007) The Ras/Raf/MAPK pathway. J Thorac Oncol 1 (1): 7–9
Moutain CF (1997) Revisions in the International System for Staging Lung Cancer. Chest 111 (6): 1710–1717
Nagai Y, Miyazawa H, Huqun, Tanaka T, Udagawa K, Kato M, Fukuyama S, Yokote A, Kobayashi K, Kanazawa M, Hagiwara K (2005) Genetic heterogeneity of the epidermal growth factor receptor in non-small cell lung cancer cell lines revealed by a rapid and sensitive detection system, the peptide nucleic acid-locked nucleic acid PCR clamp. Cancer Res 65 (16): 7276–7282
Orum H, Nielsen PE, Egholm M, Berg RH, Buchardt O, Stanley C (1993) Single base pair mutation analysis by PNA directed PCR clamping. Nucleic Acid Res 21 (23): 5332–5336
Paez JG, Jänne PA, Lee JC, Tracy S, Greulich H, Gabriel S, Herman P, Kaye FJ, Lindeman N, Boggon TJ, Naoki K, Sasaki H, Fujii Y, Eck MJ, Sellers WR, Johnson BE, Meyerson M (2004) EGFR mutations in lung cancer: correlation with clinical response to gefitinib therapy. Science 304 (5676): 1497–1500
Pao W, Ladanyi M (2007) Epidermal growth factor receptor mutation testing in lung cancer: searching for the ideal method. Clin Cancer Res 13 (17): 4954–4955
Pao W, Miller V, Zakowski M, Doherty J, Politi K, Sarkaria I, Singh B, Heelan R, Rusch V, Fulton L, Mardis E, Kupfer D, Wilson R, Kris M, Varmus H (2004) EGF receptor gene mutations are common in lung cancers from ‘never smokers’ and are associated with sensitivity of tumors to gefitinib and erlotinib. Proc Natl Acad Sci USA 101 (36): 13306–13311
Pao W, Wang TY, Riely GJ, Miller VA, Pan Q, Ladanyi M, Zakowski MF, Heelan RT, Kris MG, Varmus HE (2005) KRAS mutations and primary resistance of lung adenocarcinomas to gefitinib or erlotinib. PLoS Med 2 (1): e17
Soh J, Tokooya S, Aoe K, Asano H, Ichihara S, Katayama H, Hiraki A, Kiura K, Aoe M, Sano Y, Sugi K, Shimizu N, Date H (2006) Usefulness of EGFR mutation screening in pleural fluid to predict the clinical outcome of gefitinib treated patients with lung cancer. Int J Cancer 119 (10): 2353–2358
Sotlar K, Escribano L, Landt O, Möhrle S, Herrero S, Torrelo A, Lass U, Horny HP, Bültmann B (2003) One-step detection of c-kit point mutations using peptide nucleic acid-mediated polymerase chain reaction clamping and hybridization probes. Am J Pathol 162 (3): 737–746
Sugio K, Uramoto H, Ono K, Oyama T, Hanagiri T, Sugaya M, Ichiki Y, So T, Nakata S, Morita M, Yasumoto K (2006) Mutations within the tyrosine kinase domain of EGFR gene specifically occur in lung adenocarcinoma patients with a low exposure of tobacco smoking. Br J Cancer 94 (6): 896–903
Sun X, Hung K, Wu L, Sidransky D, Guo B (2002) Detection of tumor mutations in the presence of excess amounts of normal DNA. Nat Biotechnol 20 (2): 186–189
Sutani A, Nagai Y, Udagawa K, Uchida Y, Koyama N, Murayama Y, Tanaka T, Miyazawa H, Nagata M, Kanazawa M, Hagiwara K, Kobayashi K (2006) Gefitinib for non-small-cell lung cancer patients with epidermal growth factor receptor gene mutations screened by peptide nucleic acid-locked nucleic acid PCR clamp. Br J Cancer 95 (11): 1483–1489
Taback B, Bilchik AJ, Saha S, Nakayama T, Wiese DA, Turner RR, Kuo CT, Hoon DS (2004) Peptide nucleic acid clamp PCR: a novel K-ras mutation detection assay for colorectal cancer micrometastases in lymph nodes. Int J Cancer 111 (3): 409–414
Tam IY, Chung LP, Suen WS, Wang E, Wong MC, Ho KK, Lam WK, Chiu SW, Girard L, Minna JD, Gazdar AF, Wong MP (2006) Distinct epidermal growth factor receptor and KRAS mutation patterns in non-small cell lung cancer patients with different tobacco exposure and clinicopathologic features. Clin Cancer Res 12 (5): 1647–1653
Tanaka T, Nagai Y, Miyazawa H, Koyama N, Matsuoka S, Sutani A, Huqun, Udagawa K, Murayama Y, Nagata M, Shimizu Y, Ikebuchi K, Kanazawa M, Kobayashi K, Hagiwara K (2007) Reliability of the peptide nucleic acid-locked nucleic acid polymerase chain reaction clamp-based test for epidermal growth factor receptor mutations integrated into the clinical practice for non-small cell lung cancers. Cancer Sci 98 (2): 246–252
Travis WD, Brambilla E, Muller-Hermelink HK (2004) World Health Organization Classification of Tumours, Pathology and Genetics: Tumours of the Lung, Pleura, Thymus and Heart. IARC Press: Lyon. pp 9–124
Tsao M, Aviet-Ronen S, Ding K, Lau D, Liu N, Sakurada A, Whitehead M, Zhu CQ, Livingston R, Johnson DH, Rigas J, Seymour L, Winton T, Shepherd FA (2007) Prognostic and predictive importance of p53 and RAS for adjuvant chemotherapy in non small-cell lung cancer. J Clin Oncol 25 (33): 5240–5247
Acknowledgements
We thank Julie Kretz, Valérie Mangin, Véronique Kussaibi and Florence Guenard, for excellent technical work. This work was supported by the Ligue Régionale contre le Cancer (Haut-Rhin Comity), the Canceropole du Grand Est, the Hôpitaux Universitaires de Strasbourg and the Faculté de Médecine de Strasbourg.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
From twelve months after its original publication, this work is licensed under the Creative Commons Attribution-NonCommercial-Share Alike 3.0 Unported License. To view a copy of this license, visit http://creativecommons.org/licenses/by-nc-sa/3.0/
About this article
Cite this article
Beau-Faller, M., Legrain, M., Voegeli, AC. et al. Detection of K-Ras mutations in tumour samples of patients with non-small cell lung cancer using PNA-mediated PCR clamping. Br J Cancer 100, 985–992 (2009). https://doi.org/10.1038/sj.bjc.6604925
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.bjc.6604925
Keywords
This article is cited by
-
Current therapy of advanced colorectal cancer according to RAS/RAF mutational status
Cancer and Metastasis Reviews (2020)
-
Circulating tumor DNA in patients with colorectal adenomas: assessment of detectability and genetic heterogeneity
Cell Death & Disease (2018)
-
Monitoring the Transcriptional Activity of Human Endogenous Retroviral HERV-W Family Using PNA Strand Invasion into Double-Stranded DNA
Molecular Biotechnology (2018)
-
Co-dependency of PKCδ and K-Ras: inverse association with cytotoxic drug sensitivity in KRAS mutant lung cancer
Oncogene (2017)
-
Prognostic value of the KRAS G12V mutation in 841 surgically resected Caucasian lung adenocarcinoma cases
British Journal of Cancer (2015)