Key Points
-
'Laser' is an acronym for 'light amplification by the stimulation emission of radiation'. Its theoretical basis was postulated by Albert Einstein.
-
The first tooth exposed to laser light was in 1960.
-
Lasers can be applied to almost any clinical situation.
-
Laser light in dentistry is a unique, non-ionising form of electromagnetic radiation that can be employed as a controlled source of tissue stimulation, cutting or ablation, depending on specific parameters of wavelength, power and target tissue.
Key Points
Lasers in dentistry
-
1
Introduction, history of lasers and laser light production
-
2
Laser-tissue interaction
-
3
Low-level laser use in dentistry
-
4
Lasers and soft tissue: 'loose' soft tissue surgery
-
5
Lasers and soft tissue: 'fixed' soft tissue surgery
-
6
Lasers and soft tissue: periodontal therapy
-
7
Surgical laser use in implantology and endodontics
-
8
Surgical lasers and hard dental tissue
-
9
Laser regulation and safety in general dental practice
Abstract
The word laser conjures in the mind's eye many aspects of what might be described as 'modern' life. The words 'powerful', 'precise' and 'innovative' complement our conception of the world in terms of technology, whereas patients often associate the words 'magical' and 'lightening quick' with the use of lasers in medical practice. The purpose of this series of articles is to explore the history and development of lasers, the integration of lasers into clinical dentistry and the safeguards as to their regulated use.
Similar content being viewed by others
Introduction
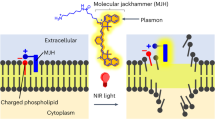
The theoretical basis of laser light production was developed some 90 years ago; the first laser was used on an extracted tooth 47 years ago. It is perhaps somewhat surprising that commercially available lasers have only been used in dental practice during the past 18 years. Associated with the launch of the first 'dental' laser, there was a level of hype that quickly led to a combination of frustration for dentists and research that discredited or minimised many of the claims for clinical use (Fig. 1).
Unlike many fields of medicine and surgery, where laser treatment represents a sole source of remedy, in dentistry the use of a laser is considered adjunctive in delivering a stage of tissue management conducive to achieving a completed hard or soft tissue procedure.
To the dental professional in general practice, the delivery of dental treatment can be compromised by the willingness of the patient to accept a procedure that is often erroneously associated with painful stimuli. Most patients recoil at the thought of a high or low-speed drill and those exposed to surgery find associated bleeding and tissue bruising interferes with normal speech and eating functions. As much as any wish to explore the envelope of possible laser-tissue interaction, much of the hype surrounding laser use in dentistry has centred on the possibility to encourage patient uptake through the avoidance of peri- and post-operative pain and discomfort. Certainly, however, today's lasers offer an opportunity to deliver hard and soft-tissue treatments that, at least in outline, make the patient experience somewhat easier (Figs 2, 3, 4, 5, 6, 7, 8, 9, 10).
As will be seen in later articles in this series, considerable research has been carried out ostensibly to validate the innovative use of lasers in all branches of dentistry. At worst, claims to beneficial use in some areas have been discredited; often, other usage has been shown to overcome deficiencies in more conventional therapies. Lasers can be applied to almost any clinical situation, but their efficacy versus conventional techniques in many cases is unknown, with the exception of anecdotal reports.
Essentially, the adjunctive use of surgical lasers in dentistry has sought to address efficient cutting of dental hard tissue, haemostatic ablation of soft tissue and also the sterilising effect through bacterial elimination. Less powerful, non-surgical lasers have been shown to modify cellular activity and enhance biochemical pathways associated with tissue healing, aid in caries detection and assist in the curing of composite restorative materials. The decision to include lasers in everyday dental care will depend not least upon financial considerations as to how their use may enhance practice profitability; the greatest factor in making that decision will be an understanding of how laser wavelengths interact with oral tissue, together with an appreciation of how such use can improve patient management.
History of Lasers and Their Use in Clinical Medicine and Dentistry
The theoretical basis that postulated the production of intense light of a specific configuration, pre-dated the development of the first laser by over forty years.
In 1704, Newton1 characterised light as a stream of particles. The Young's interference experiment in 1803 and the discovery of the polarity of light convinced other scientists of that time that light was emitted in the form of waves. The concept of electromagnetic radiation, of which 'light' is an example, had been described in mathematical form by Maxwell, in 1880. Maxwell's electromagnetic (EM) theory explained light as rapid vibrations of EM fields due to the oscillation of charged particles. At the turn of the 20th century, the black body radiation phenomenon challenged the waveform light theory. Atomic structures would absorb incident EM energy and become excited to an upper level, which would subsequently decay to a lower, stable state, with the release of emissive energy. According to Maxwell's EM theory, the energy intensity of EM emissions with a given frequency is proportional to the square of this frequency.
Additional work undertaken by Hertz on the 'photoelectric effect' (a pioneering study into cathode ray emission), and Planck on the formulation of the distribution of the radiation emitted by a black body or perfect absorber of radiant energy, complemented further the understanding of light propagation. The significance of Planck's constant in this context is that radiation such as light, is emitted, transmitted and absorbed in discrete energy packets or quanta, determined by the frequency of the radiation and the value of Planck's constant.
The observations that the number of electrons released in the photoelectric effect is proportional to the intensity of the light and that the frequency, or wavelength, of light determines the maximum kinetic energy of the electrons, indicated a kind of interaction between light and matter that could not be explained in terms of classical physics. The search for an explanation led in 1905 to Albert Einstein's fundamental theory that light can be regarded alternatively as composed of discrete particles (photons), equivalent to energy quanta.
In explaining the photoelectric effect, Einstein (Fig. 11) assumed that a photon could penetrate matter, where it would collide with an atom. Since all atoms have electrons, an electron would be ejected from the atom by the energy of the photon, with great velocity. Einstein also predicted in 1917 in Zur Theorie der Strahlung2 (Theory of Wavelength), that when there exists the population inversion between the upper and lower energy levels among the atom systems, it was possible to realise amplified stimulated radiation, ie laser light. Stimulated electromagnetic radiation emission has the same frequency (wavelength) and phase (coherence) as the incident radiation.
Maser
The electromagnetic spectrum is a comparative arrangement of electromagnetic energy (photonic quanta) relative to wavelength, spanning ultra-short gamma and X-radiation, through visible light, to ultra-long micro- and radio-waves. In 1953, Charles Townes, experimenting with microwaves,3 produced a device whereby this radiation could be amplified by passing it through ammonia gas. This was the first MASER (microwave amplification by the stimulated emission of radiation) and was developed as an aid to communication systems and time-keeping (the 'atomic clock'). It was realised that only a fraction of the incident energy was converted into maser energy, the greater emission being in the form of heat; the output power of the early masers was of the order of a few micro-watts.
Experimental work undertaken by other workers into various incident energy wavelengths and target materials, resulted in the invention of the first LASER (light amplification by the stimulated emission of radiation) by Theodore Maiman,4 at the Hughes Aircraft Company USA, in 1960.
Laser
The experimental work into the physics of laser light production highlighted the attraction of the use of intense radiation energy, of single wavelength, in many military and communications applications. Maiman's laser used a solid ruby as an 'active medium', which was energised or 'pumped' by an electrical source (Fig. 12).
Many other kinds of laser were invented soon after the solid ruby laser – the first uranium laser by IBM Laboratories (in November 1960), the first helium-neon laser by Bell Laboratories in 1961 and the first semiconductor laser by Robert Hall at General Electric Laboratories in 1962; the first working neodymium-doped yttrium aluminium garnet (Nd:YAG) laser and CO2 laser by Bell Laboratories in 1964, argon ion laser in 1964, chemical laser in 1965 and metal vapour laser in 1966. In each case, the 'name' of the laser was annotated with regard to the active medium (source of laser photons) used.
Laser use in medicine and surgery
As will be seen in later articles in this series, there is a specific and fundamental relationship between light wavelength and absorption by an 'illuminated' target material. Thus, the unique nature of laser light and its specific absorption, led to an expansion of its use in medicine. Within a year of the invention, pioneers such as Dr Leon Goldman began research on the interaction of laser light on biologic systems, including early clinical studies on humans.5 Interest in medical applications was intense, but the difficulty controlling the power output and delivery of laser energy, together with the relatively poor absorption of these red and infrared wavelengths, led to inconsistent and disappointing results in early experiments. The exception was the application of the ruby laser in retinal surgery in the mid-1960s. In 1964, the argon ion laser was developed. This continuous wave 488 nm (blue-green) gas laser was easy to control and its high absorption by haemoglobin made it well suited to retinal surgery; clinical systems for treatment of retinal diseases were soon available.
In 1964, the Nd:YAG and CO2 lasers were developed at Bell Laboratories in the USA. The CO2 laser is a continuous wave gas laser and emits infrared light at 10,600 nm in an easily manipulated, focused beam that is well absorbed by water. Because soft tissue consists mostly of water, researchers found that a CO2 laser beam could cut tissue like a scalpel, but with minimal blood loss. The surgical uses of this laser were investigated extensively from 1967-1970 by pioneers such as Dr Thomas Polanyi and Geza Jako and in the early 1970s, use of the CO2 laser in ENT and gynaecologic surgery became well established, but was limited to academic and teaching hospitals.
In the early 1980s, smaller but more powerful lasers became available. Most of these systems were CO2 lasers used for cutting and vaporising tissue and argon lasers for ophthalmic use. These 'second generation' lasers were all continuous wave or CW systems which tend to cause non-selective heat injury, and proper use required a long 'learning curve' and experienced laser surgeons.
The single most significant advance in the use of medical lasers was the concept of 'pulsing' the laser beam, which allowed selective destruction of abnormal or diseased tissue, while leaving surrounding normal tissue undisturbed. The first lasers to fully exploit this principal of 'selective thermolysis' were the pulsed dye lasers introduced in the late 1980s for the treatment of port wine stains in children and shortly after, the first 'Q-switched' (ultra-short pulsed) lasers for the treatment of tattoos. Another major advance was the introduction of scanning devices in the early 1990s, enabling precision computerised control of laser beams. Scanned, pulsed lasers revolutionised the practice of plastic and cosmetic surgery by making safe, consistent laser re-surfacing possible, as well as increasing public awareness of laser medicine and surgery.
Laser use in dentistry
Although Maiman had exposed an extracted tooth to his ruby laser in 1960, the possibilities for laser use in dentistry did not occur until 1989, with the production of the American Dental Laser for commercial use. This laser, using an active medium of Nd:YAG, emitted pulsed light and was developed and marketed by Dr Terry Myers, an American dentist. Though low-powered and due to its emission wavelength, inappropriate for use on dental hard tissue,6 the availability of a dedicated laser for oral use gained popularity amongst dentists. This laser was first sold in the UK in 1990 (Fig. 13).
Other laser wavelengths, using machines that were already in use in medicine and surgery and only slightly modified, became available for dental use in the early 1990s. Being predominately argon, Nd:YAG, CO2 and semiconductor diodes, all these lasers failed to address a growing need amongst dentists and patients for a laser that would ablate dental hard tissue. In 1989, experimental work by Keller and Hibst7 using a pulsed erbium YAG (2,940 nm) laser, demonstrated its effectiveness in cutting enamel, dentine and bone. This laser became commercially available in the UK in 1995 and, shortly followed by a similar Er,Cr:YSGG (erbium chromium: yttrium scandium gallium garnet) laser in 1997, amounted to a laser armamentarium that would address the surgical needs of clinical dentistry in general practice (Figs 14 and 15).
Light (photonic) production and emission
Ordinary light
'Ordinary' light refers to the close band of wavelengths in the electromagnetic spectrum that is visible to the human retina. In nature, its origin is in the cosmic stream from space and a common source of man-made ordinary light is the incandescent filament of a light bulb. 'White' light is the sum of all component wavelengths of the visual spectrum. The waveform of ordinary light is non-coherent, in that there is a confused overlap of successive waves. The spread of such waves results in scattering of light with distance and the multi-direction and interference of successive waves gives rise to divergence and dimming with distance. The wavelength of any light beam is measured in metres, with typical values being expressed as nanometres (10−9 metres).
The unit of light energy is the photon and the relationship of energy with frequency can be expressed as:

where v = frequency (number of wave oscillations with time) and h = Planck's constant.
In addition, the relationship of frequency to wavelength λ can be expressed as:

where c is the speed of light (a constant).
Substituting wavelength for frequency:

This relationship thereby establishes an inverse relationship between wavelength and photonic energy. With reference to the electromagnetic spectrum, this accounts for why X-rays, at the ultra-short wavelength end of the spectrum have deep penetrating energy, whilst long wavelength radio waves require a specific receiver.
Quantum nature of light – absorption & emission
The expression of quantum physics in terms of atomic structure was defined by Bohr in 1922.8 Incident light energy, absorbed by a target atom, will result in an electron moving to a higher energy shell. This unstable state will result in the emission of photonic energy relative to the stable energy state of the target, with excess energy being produced as heat. This is known as spontaneous emission. If an already energised atom is bombarded with a second photon, this will result in the emission of two, coherent photons of identical wavelength. This was postulated by Einstein as stimulated emission2 (Fig. 16).
The simple process represented by Figure 16 demonstrates a three-level concept of energy values, ie ground state → excited state → ground state.
Laser light
Laser light occurs through the amplification of stimulated emission. Since the emission energy is unique relative to its source and of known measurable quantity, the light will be of a single wavelength (monochromatic). The high-energy, single wavelength light is produced in a spatially stable form (collimated or non-divergent), with successive waveforms that are in phase (coherent). In consequence, the coherence and collimation of the light results in high energy density and the mono-chromatic wavelength will define specific target absorption. These fundamental qualities will be considered in the article on laser-tissue interaction.
Dental laser wavelengths
With respect to the monochromatic nature of laser light, a number of emission wavelengths have been developed that, for the purposes of current clinical dentistry, span the visible to the far infrared portions of the electromagnetic spectrum (approximately 400-10,600 nm) (Fig. 17).
Components of a typical laser (Fig. 18)
The component parts of a typical laser are:
1. Active medium
A material, either naturally occurring or man-made that when stimulated, emits laser light. This material may be a solid, liquid or gas. The first 'dental' laser used a crystal of neodymium-doped yttrium aluminium garnet (Nd:YAG) as its active medium. 'YAG' is a complex crystal with the chemical composition Y3Al5O12. During crystal growth, 1% neodymium (Nd3+) ions are doped into the YAG crystal (Fig. 19).
Other lasers of significance in dentistry use rare earth and other metal ions within a 'doped' YAG crystal lattice, eg erbium (Er:YAG) and holmium (Ho:YAG), together with another erbium and chromium-doped garnet of yttrium, scandium and gallium (Er,Cr:YSGG).
The active medium is positioned within the laser cavity, an internally-polished tube, with mirrors co-axially positioned at each end and surrounded by the external energising input, or pumping mechanism.
The 'active medium', eg CO2, Nd:YAG, defines the type of laser and the emission wavelength of the laser (10,600 nm and 1,064 nm respectively). Atoms of the active medium are absorbed by the process of light emission.
2. Pumping mechanism
This represents a man-made source of primary energy that excites the active medium. This is usually a light source, either a flashlight or arc-light, but can be a diode laser unit or an electromagnetic coil. Energy from this primary source is absorbed by the active medium, resulting in the production of laser light. This process is very inefficient, with only some 3-10% of incident energy resulting in laser light,9 the rest being converted to heat energy.
The dynamics of incident energy with time has a fundamental bearing on the emission mode characteristics of a given laser. A continuous-feed electrical discharge will result in a similar continuous feed of laser light emission (see below, laser light emission modes).
3. Optical resonator
Laser light produced by the stimulated active medium is bounced back and forth through the axis of the laser cavity, using two mirrors placed at either end, thus amplifying the power. The distal mirror is totally reflective and the proximal mirror is partly transmissive, so that at a given energy density, laser light will escape to be transmitted to the target tissue (Fig. 20).
4. Delivery system
Dependant upon the emitted wavelength, the delivery system may be a quartz fibre-optic, a flexible hollow waveguide, an articulated arm (incorporating mirrors), or a hand-piece containing the laser unit (at present only for low-powered lasers). Early attempts to produce delivery systems relied upon the use of fixed mirror and/or lens apparatus. It was soon apparent that the use of a fine, silica quartz fibre-optic cable maximised the feasibility for medical and dental lasers to reach their target site. However, the suitability of this delivery system is conditional upon the emission wavelength being poorly absorbed by water (hydroxyl groups), present in the quartz fibre. Therefore, shorter wavelengths such as argon, diodes and Nd:YAG can enjoy such fibre delivery, whereas longer wavelengths (Er,Cr:YSGG, Er:YAG and carbon dioxide) give rise to severe power losses through quartz fibre and hence require alternative delivery systems (Fig. 21).
Examples of such alternatives are articulated arms incorporating internal mirrors and prisms, and hollow waveguides, where the light is reflected along internally-polished tubes. Newer, water-free fibre compounds, eg zirconium fluoride, are being developed to overcome this problem.10,11,12,13
5. Cooling system
Heat production is a by-product of laser light propagation. It increases with the power output of the laser and hence, with heavy-duty tissue cutting lasers, the cooling system represents the bulkiest component. Co-axial coolant systems may be air- or water-assisted.
6. Control panel
This allows variation in power output with time, above that defined by the pumping mechanism frequency. Other facilities may allow wavelength change (multi-laser instruments) and print-out of delivered laser energy during clinical use.
Diode lasers
The development of micro-structure diode cells that are capable of laser light production has dramatically reduced the bulk of laser machines (Fig. 22).
The limitation of the physics involved has restricted the span of spectral emissions to a relatively narrow band (approx 400-1,000 nm) at the present time. Only solid material active media are used in these lasers.
In a diode laser, the active medium is sandwiched between silicon wafers (Fig. 23). Due to the crystalline nature of the active medium, eg GaAlAs, it is possible to selectively polish the ends of the crystal relative to internal refractive indices to produce totally and partially reflective surfaces, thus replicating the optical resonators of larger lasers. The discharge of current from one silicon wafer to the other, across the active medium, releases photons from the active medium. Individual diode 'chips' produce relatively low-energy output and so current surgically-appropriate diode lasers employ banks of individual diode chips in parallel to achieve a desired power capability.
Energy exchange and wavelength emission
As was seen earlier, the ideal quantum exchange in an absorption/emission system is through a three-level transfer (ground – excited – ground). Although many lasers exhibit this (eg HeNe, N2), several important dental laser active mediums suffer some time delay, whereby energy decay exists over a range of values, giving rise to an upper and lower lasing level of emission. This exposes the active medium to multi-wavelength emission spectra. As such, these lasers are known as four-level lasers (Fig. 24) and their relevance is such that there is a potential for a non-specific, multi-wavelength emission. However, through a choice of reflecting mirrors as optical resonators (plain, concave, convex), it is possible to create wave interference and cancellation within the laser cavity, to leave a desired emission single wavelength. This explanation accounts for the existence of, for example, a CO2 laser at 9,300, 9,600 and 10,600 nm (Fig. 25).
The active medium of a CO2 laser is a mixture of CO2, helium and nitrogen gases, in proportions 8:7:1. Pumping is through an electric coil discharge. Initially, most of the electrical discharge energy is absorbed by nitrogen gas and only a small part of the energy is absorbed by CO2 molecules directly to raise them from a ground state to the upper lasing level. Large amounts of CO2 molecules collide with the nitrogen molecules and gain the excitation energy. Energy decay occurs over time, to a lower lasing level, thus giving out laser light at frequency 9,300 nm, 9,600 nm or 10,600 nm respectively. Remaining decay to ground state will dissipate energy in the form of heat instead of light.
Laser light beam dynamics
Collimation, one of the prime properties of laser light, is in practice a theoretical concept, in that its acceptance is based upon transmission through a vacuum. The passage of laser light through any other medium will result in some divergence with distance, which can be of the order of 15-30 degrees when using an optical fibre delivery system or a diode active medium.14 As such, in order to be controlled, an emission beam is often passed through a focal medium, eg a bi-convex lens.
If the primary output laser beam is intersected and the transverse beam cross-section studied, the light intensity can be of different distributions (patterns), consistent with the reflective dynamics of the optical resonators. These are called transverse electromagnetic modes (TEM). Three indices are used to indicate the modes – TEM plq, where p is the number of radial zero fields, l is the number of angular zero fields and q is the number of longitudinal fields. The first two indices are usually used to specify a TEM mode, eg TEM00, TEM10, etc. Clearly, the higher the order of the modes the more difficult it is to focus the beam to a fine spot. TEM00 mode, or Gaussian beam as it is commonly known, is preferred in order to achieve desired accuracy in treatment procedures. The ability to produce a focussed beam together with the controlled application of light power over a small area, has a fundamental bearing on the concept of delivering ablation energy to a target tissue.
Laser light emission modes
Often, a clinical laser is referred to as 'continuous wave' (CW), 'gated pulsed' (GP) or 'free-running pulsed' (FRP). Although this might appear confusing, it relates to the rate of emission of laser light with time. The inherent benefit of the concept of pulsed flow over average continuous flow is that, assuming the average delivery of energy with time might be low, the peak-energy of each 'pulse' can be significantly higher. In dentistry, this is seen where an Er:YAG laser is used to cut enamel; the average power (energy rate with time) is low, but the peak power levels are sufficiently high to dislocate hydroxyapatite crystals, through the instantaneous, explosive vaporisation of interstitial water.15 Commercial lasers for surgical dental use are commonly annotated '5 Watts', '10 Watts', etc – this relates to the maximal average power output. The emission mode epithet, eg 'CW', 'FRP' will alert the clinician to the potential peak power capacity of the laser.
In practice, the emission mode for any given laser can be either 'inherent' or 'acquired'. Inherent emission modes are related to the nature of the excitation source:
-
a
Free-running pulsed, where laser emission occurs over a pulse width of 100-200 microseconds
-
b
Continuous wave.
Acquired emission modes are due to a modifying effect (electrical, mechanical, electro-optical or acousto-optical) acting upon the inherent delivery:
-
a
Chopped or gated CW, where laser emission occurs over tenths (0.1-0.5) of a second
-
b
Q-switched, mode-locked (not applicable in dental lasers)
-
c
Super-pulsed, where laser emission occurs over 300-400 microseconds.
With relevance to the clinical application of any laser with any target oral tissue, it is important to consider the potential transfer of energy from the laser beam, converted to heat energy in the target, in order that only a sufficient transfer to execute designated tissue change is achieved. For a simple, low power CO2 laser, the average power output of a CW machine is readily understood – four Watts of CW output = four Watts average power. With a FRP laser, eg Er:YAG, output is often expressed as energy per pulse and the operator can determine the number of pulses. As such, the energy per pulse, eg 200 mJ, must be multiplied by the number of pulses, eg 20 pulses per second (0.2 J × 20) to give an average power delivery of four Watts (Joules per second). The prime benefit of a pulsed delivery mode will be the capacity of the target tissue to cool between successive pulses. However, when considering a FRP laser, the peak power per pulse can be considerable. An energy-per-pulse value of 200 mJ (200 × 10−3 J) with a pulse duration of 100 μs (100 × 10−6 s) can give rise to a peak power of 2,000 Watts for that fraction of time (J ÷ s).
The electromagnetic forces produced during a peak power energy discharge can be sufficient to create a plasma ball of energy,16 sufficient to destroy molecular structure in a target tissue.
The majority of commercial lasers for use in clinical dentistry incorporate such information within the control panel display. What is of concern is that many lasers in use in dental practice are derivatives of machines that are designed primarily for general surgical use and as such, possess power parameters that could be considered potentially damaging for use in an intra-oral setting.
In summary, emission mode will have a direct effect in the following ways:
-
a
The average power (rate of energy with time) being delivered to the target
-
b
The peak power value of laser light being delivered to the target (observed with FRP modes)
-
c
The thermal relaxation effect (ability to cool) of the target.
The thermal relaxation potential is greatest in FRP emission and least in CW emission. This has a profound bearing on the tissue management during laser-tissue interaction.
References
Newton I. Opticks: or, a treatise of the reflections, refractions, inflexions and colours of light. Also two treatises of the species and magnitude of curvilinear figures. London, 1704.
Einstein A. Zur quantentheorie der strahlung. Physiol Z 1917; 18: 121–128.
Townes C H. Making waves. New York: Springer-Verlag, 1994.
Maiman T H. Stimulated optical radiation in ruby. Nature 1960; 187: 493–494.
Goldman L, Ingelman J M, Richfield D F. Impact of the laser on nevi and melanomas. Arch Dermatol 1964; 90: 71–75.
Myers T D, Myers W D, Stone R M. First soft tissue study utilising a pulsed Nd YAG dental laser. Northwest Dent 1989; 68: 14–17.
Hibst R, Keller U. Experimental studies of the application of the Er YAG laser on dental hard substances: 1. Measurement of ablation rate. Lasers Surg Med 1989; 9: 338–344.
Bohr N. The theory of spectra and atomic constitution. 2nd ed. Cambridge: Cambridge University Press, 1922.
Prakash O, Ram R S. Simple designs to measure efficiency of different types of monochromators. J Opt 1996; 27: 241–245.
Inberg A, Oksman M, Ben-David M, Croitoru N. Hollow waveguide for mid and thermal infrared radiation. J Clin Laser Med Surg 1998; 16: 127–133.
Yang Y, Chaney C A, Fried N M. Erbium:YAG laser lithotripsy using hybrid germanium/silica optical fibers. J Endourol 2004; 18: 830–835.
Konorov S O, Mitrokhin V P, Fedotov A B et al. Hollow-core photonic-crystal fibres for laser dentistry. Phys Med Biol 2004; 49: 1359–1368.
Merberg G N. Current status of infrared fiber optics for medical laser power delivery. Lasers Surg Med 1993; 13: 572–576.
Moseley H, Davison M, Allan D. Beam divergence of medical lasers. Phys Med Biol 1985; 30: 853–857.
Apel C, Franzen R, Meister J, Sarrafzadegan H, Thelen S, Gutknecht N. Influence of the pulse duration of an Er:YAG laser system on the ablation threshold of dental enamel. Lasers Med Sci 2002; 17: 253–257.
Hillenkamp F. Laser radiation tissue interaction. Health Phys 1989; 56: 613–616.
Author information
Authors and Affiliations
Corresponding author
Additional information
Refereed Paper
Rights and permissions
About this article
Cite this article
Parker, S. Introduction, history of lasers and laser light production. Br Dent J 202, 21–31 (2007). https://doi.org/10.1038/bdj.2006.113
Published:
Issue Date:
DOI: https://doi.org/10.1038/bdj.2006.113
This article is cited by
-
Long-term clinical outcomes of Er:YAG or Er,Cr:YSGG lasers utilized as monotherapy or as adjuncts to mechanical therapy in the treatment of chronic periodontitis: a systematic review
Lasers in Dental Science (2023)
-
Lasers in prosthodontics — An overview part 1: Fundamentals of dental lasers
The Journal of Indian Prosthodontic Society (2010)