Key Points
-
Describes the use of ceramic inserts in posterior teeth.
-
Cerana inserts performed well in class I and class II cavities over eight years.
-
These inserts improve the properties of composite resin restorations.
Abstract
Background Single-visit system ceramic restorations are now in use to provide an alternative to resin-based materials. Inserts have been shown to improve characteristics of composite restorations. Objective To investigate the longevity of Cerana (Nordiska Dental, Sweden) in a prospective clinical trial. Methods Cerana restorations use matched drills with pre-etched and silanated leucite inserts cemented using a conventional restorative composite resin material. The results of 33 Cerana restorations up to eight years (25 Class I, eight class II) are presented. Restorations were reviewed and assessed by two examiners using modified USPHS criteria for anatomical form (AF) A-C, marginal adaptation (MA) A-D, surface roughness (SR) A-D, marginal discoloration (MD) A-C, colour match (CM) A-C and discomfort (DT) A-D as well as retention. Results The percentage of A scores for AF, MA, SR, MD, CM and DT at baseline (n = 33) were: 100, 100, 79, 100, 21, 100; after two years (n = 27) 100, 85, 33, 100, 19, 100 and after four years (n = 24) 96, 75, 17, 96, 25, 100. At six years (n = 20) 95, 70, 10, 95, 15, 100 and finally at the eight year recall (n = 18) 94, 61, 0, 94, 6, 100. AF was maintained in all except for one fractured marginal ridge. MA of the insert was good but composite was lost where exposed. SR increased to a B score for all inserts. MD at B grade was observed in 6% between composite and tooth but none between insert and composite. CM was stable in all cases. DT nil in all. There were no scores less than B. All reviewed restorations were retained, clinically acceptable and in function except for two lost for reasons not directly related to the Cerana insert. One class II restoration had a fractured marginal ridge but otherwise remains satisfactory. Conclusions The results suggest that these restorations can be expected to perform well. Cerana is acceptable in terms of aesthetics, patient acceptance, occlusal wear and ease of use and is a good alternative for a single-visit, tooth coloured restoration in suitable cavity shapes.
Similar content being viewed by others
Introduction
There is an increasing demand from patients for aesthetic restorations, including those in posterior teeth. Direct placement composite resin is often used but is associated with polymerisation shrinkage which can result in marginal failure, gap formation,1 microleakage,2 post-operative sensitivity and cuspal flexion.3,4 These problems may not be overcome by incremental placement.5 Obtaining good proximal contacts is also difficult with directly placed composite resin. Polyacid modified composite resins (compomers) and glass ionomers do not offer such suitable long-term wear resistance as composite or ceramic materials.6
Attempts to overcome the problems of direct placement composite resin have included the use of an indirect technique.7 However, indirect restorations of composite resin require two visits and the placement of a temporary restoration. Furthermore, they incur laboratory fees and require increased chairside time resulting in a higher cost to the patient than for a directly placed composite resin. The direct indirect ('chairside') composite inlay technique is time-consuming and technique sensitive.8,9
Other methods aimed at reducing polymerisation shrinkage have included the use of inserts.10,11,12,13 Beta-quartz inserts have been shown to reduce polymerisation shrinkage14 which has resulted in reduced marginal gaps,15 acceptable margins16 and less microleakage.17 Improved occlusal wear rates have also been reported in some studies18 but not in others19 and inserts have been considered useful as a means of maintaining a functional occlusion19 and improved proximal contacts.20 In general, the effects of the insert seem to be beneficial, largely due to the increase in the filler:resin ratio.
More recently leucite inserts, which have more enamel-like properties than beta-quartz, have been produced. The resulting restoration has the potential to offer the favourable properties of leucite ceramic yet allow a simple and quick placement technique in a single visit.13,21 The reduction in volume of polymerisable resin will result in less overall shrinkage and reduced marginal leakage.22 Such single-visit ceramic systems provide aesthetic, easy to place yet hard wearing restorations with the aesthetic qualities of ceramic. The present longitudinal clinical evaluation investigates Cerana (Nordiska Dental, Sweden), a single-visit ceramic inlay system. The technique is based on a ceramic insert with the optional use of a size-matched bur for cavity preparation. Odman et al.23 studied 60 inlays and showed promising results over a mean evaluation period of one and a half years.
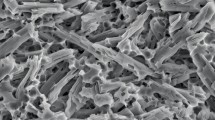
The Cerana restorations are formed from pressed leucite and are surface-treated ready for bonding. Leucite has been identified as having suitable qualities including thermal coefficients and Cerana shown to be more resistant to marginal leakage than beta-quartz.24 Leucite crystals (K2O Al2O3 4SiO2) can be etched with HF and silanised. The Cerana inserts are hydrofluoric acid etched and surface treated with methacryloxypropyl-trimethoxy-silane, with a shelf-life of over five years, before being sealed into a sterile blister pack.
The Cerana system is designed for use for class I, II (conventional and tunnel design), III, and IV cavities but is expected to have its main application in class I and class II cases. The Cerana technique is also well-suited to the closure of endodontic access cavities.25 Cerana offers an attractive option to composite resin and compomer and is less time-consuming than indirect techniques or CAD-CAM fabricated restorations. Cerana conforms to ISO6872:1995, has a CE mark [NIOM; 0510] and became available in Europe during 1995 and in the UK from 1997.
The technique, details of which have been described,13,21 uses a prefabricated ceramic insert, previously etched and silane coated, to accurately fit a cavity prepared with matching burs. The beta-quartz system does not have size-matched burs. The use of the size-matched Cerana burs will reduce the area of exposed marginal composite. An alternative technique is to avoid using the Cerana size-matched burs to shape the cavity and instead place the insert directly into the cavity following composite resin placement. Any differences in cavity outline form from the round inlay shape are restored by a conventional restorative material such as a filled composite resin, not a luting resin. Therefore, there are two techniques for using Cerana depending on the pre-exisiting cavity shape and the operator's decision.
The advantage in the technique using the matched burs is ideal for small round lesions where the occlusal surface will be almost entirely replaced by the ceramic. For more complex cavity shapes an overlap technique can be used where additional inlays can be placed adjacent to, and replacing part of, other Cerana inlays.
Cerana, like the other direct systems including CAD-CAM restorations, requires occlusal grinding adjustments and polishing after cementation. The ceramic inserts and inlays are able to create optimal approximal contacts20 because of their ability to hold the matrix in position against the adjacent tooth during curing of the composite resin.
The Cerana system has been in use for over 10 years by the authors and with undergraduate and postgraduate dental students with success. The aim of this study was to document the longevity of Cerana restorations in a prospective longitudinal trial.
Methods
A prospective longitudinal study was initiated in 1996 to investigate the use and longevity of Cerana restorations. The data obtained from eight years of recalls are presented reporting on 33 Cerana restorations (25 class I, eight class II). All restorations were placed by one operator using a single technique throughout the study. The technique was found to be simple to learn and to integrate into current treatment regimes with a minimum outlay for new equipment. The technique has been used by undergraduates and clinical staff for a range of cavity types.
The cavities were prepared in the usual way by gaining access to the carious lesion and removal of carious tooth material. Conical Cerana diamonds were used to finalise the cavity shape without increasing the cavity outline unnecessarily. An enamel-etch or total-etch technique was used and the composite resin restorative material was placed in the cavity. The Cerana insert, which matches the drill, was removed from its blister pack (Fig. 1), coated in bonding resin and placed into the cavity with a rotatory action.
If large undercut areas are present then a size-matched curing cone made of clear acetate can be used to light-cure materials in these regions while creating a suitable shape for the Cerana inlay. The inlay does not require any surface treatment as it has been etched and silanated during manufacture. Once seated the composite resin was light-cured and excess inlay material projecting above the cavity outline was removed. Final contouring was carried out to create a suitable occlusal surface which was then polished. A typical class I cavity can be restored with this system in the same time as an incrementally placed composite resin. The enamel-like aesthetic properties of the inlay assist in the colour matching. Four sizes of inlay are currently available in two shapes designed for Class I and Class II cavity forms.
An example of the treatment for a Class II cavity is illustrated in Figure 2 (a-d). It was also found to be a rapid means of sealing minimal fissure class I cavities following the opening of a fissure to investigate a small dentinal lesion as well as for larger class I cavities, including larger endodontic access cavities (Figs 3a–c) where the occlusal contacts could be placed on the ceramic inlay rather than on composite resin. Figure 4 illustrates a 4-year-old single Cerana inlay in a class I cavity and Figure 5 shows an 8-year-old Cerana restoration sealing an access cavity cut through a metal-ceramic crown. Figure 6 illustrates a 4-year-old single inlay placed in a box design class II and Figures 7a and 7b show a larger class II cavity restored with two overlapping Cerana inserts.
In the present study the burs were not used to complete the entire cavity outline to eliminate the marginal composite resin. It was accepted that the bulk of the restoration would be Cerana, including occlusal stops and contact areas. This approach was adopted to avoid unnecessary overcutting of tooth tissue.
Restorations were scored initially and at each annual review by two examiners for retention and assessed using modified USPHS criteria for:
1. anatomical form (AF) A-C 2. marginal adaptation (MA) A-D 3. surface roughness (SR) A-D 4. marginal discolouration (MD) A-C 5. colour match (CM) A-C 6. discomfort (DT) A-D A = excellent, no correction required
B = satisfactory, minor defects present, no need for replacement C/D = need for replacement
Grades A and B together represent clinical success and C and D represent a failed restoration.
Addition cured silicone impressions and photographs were also recorded for future analysis.
Results
The patients were recalled as close to the review date as possible and were assessed by two trained examiners who then agreed a score. The percentage of scores for retention and each criteria at baseline is given in Table 1. Table 2 shows the data at four years and Table 3 at eight years. There were no C or D scores awarded. The percentage of alpha scores over the eight year trial period can be seen in Figure 8.
Anatomical form was maintained in all restorations except for one fractured marginal ridge. Marginal adaptation of the inserts was excellent particularly where the ceramic fitted up to the enamel margin. Composite wear was apparent in restorations where composite resin was exposed between inlay and tooth.
Surface roughness increased to a B score for all inserts by the eighth year recall. None were grade C or D. This was considered to be similar to the loss of surface lustre which becomes apparent on hybrid composite restorations as observed in our parallel studies.26
Marginal discolouration remained A for 94% of Cerana restorations. Grade B was observed in the remainder due to staining between composite resin and enamel. There was no staining between insert and composite and no restorations were graded C or D.
Colour match was stable in all cases. There was no colour change in any of the Cerana restorations. The B grades given at baseline and subsequently reflect that the Cerana inserts used in the trial were all a single shade and therefore not colour-matched to the tooth. However, the colour was acceptable to all patients and remained stable throughout the study period. There was no surface staining of any Cerana restoration. Discomfort remained nil in all cases for all restorations over the whole study period.
Figure 9 illustrates a case where loss of composite resin has occurred over eight years to leave the ceramic insert and enamel margins proud of the composite resin surface. Three 10-year-old Cerana restorations can be observed in Figure 10 showing loss of composite resin around the intact Cerana inserts. These restorations were placed without the use of the size-matched Cerana burs and so the marginal composite had been exposed to wear.
One restoration was lost from the study as the tooth was later prepared for a crown with the Cerana forming part of the core. Another restoration was lost due to the fracture of an adjacent cusp and replacement with a complete new restoration. One Cerana restoration exhibited a fracture of the distal marginal ridge (Fig. 11) between the second and third year recalls. This restoration continues in function and is now in its eighth year.
Discussion
The main advantage of Cerana is that it provides a rapid and simple method of achieving a ceramic restoration in a posterior tooth in a single visit. This avoids two appointments, two anaesthetics and temporisation. The problems associated with bulk curing of composite resin are also reduced. The occlusal surface can be highly polished and the occlusal contacts can be placed on ceramic rather than composite resin. Proximal contact areas can be achieved by using the inlay to push the matrix against the adjacent tooth as can be seen in Figure 2b.
The observations to date are in agreement with the findings of others23 who followed 38 patients with 60 Cerana inlays over a mean period of 1.5 years in a retrospective study. In the present study it was found that all of the inlays were 'excellent' or 'acceptable' for marginal adaptation, colour and surface roughness. No patients reported post-operative pain and only one restoration 'failed' due to a fractured marginal ridge. Therefore, Cerana restorations compare favourably with direct composite, amalgam and GIC derivative materials.6
As with other inlay systems it is important that the cavity is not enlarged unnecessarily in order to accommodate a particular size or shape of inlay. Clinicians can opt to restore the cavity with a smaller Cerana inlay and fill the area between the inlay and the adjacent tooth tissue with a filled composite restorative, as was the technique used in this study. However, if the size-matched burs had been used to create prescribed cavities then the fit of the insert would have improved and less composite wear would be observed.
In this study the Cerana restorations performed better than beta-quartz glass-ceramic insert restorations at the three year recall stage using similar criteria27 in which a 3.5 year survival rate was determined to be 59%. The results from the present study compares favourably to a similar eight year trial using the same criteria by the same authors with composite resin.26
The failure rate (ie C and D scores) over the study period was 0% for the Cerana restorations which compares favourably with Cerana in another study,23 direct composite 0-9%, amalgam 0-7%, glass ionomer 1.4-14.4%, gold inlays 0-5.9%, indirect composite inlays 0-11.8% and indirect ceramic inlays 0-11.8%.28 Survival of class II Cerec inlays has been reported as 89% at 10 years29 and the success of composite inlays has been reported as 89% at three years and Empress ceramic inlays, which like Cerana are leucite-based, have been reported as having a success rate of 100% at three years.30
The success can, in part, be attributed to the close marginal fit and the effect of a 'megafiller' on composite shrinkage and is in agreement with the concept of the use of inserts.31 An investigation of marginal gap width32 showed indirect porcelain inlays to have an enamel marginal gap of 468±63 μm before adjustment and 126±19 μm after adjustment. This gap would normally be closed with a luting composite resin which may wear more quickly than the more highly filled restorative composite resin around a Cerana restoration. Cerana inserts have been shown to have margins as acceptable as indirect ceramic inlays.33 Another study34 has shown Cerana to have a high percentage of perfect margins and reports a marginal fit of 58±21 μm.
In the present study the Cerana restorations were cemented with a restorative composite resin at room temperature. However, given recent awareness35 about the advantages of pre-heated composite on curing time, depth of cure, hardness, degree of polymerisation and microleakage and flow properties, this technique is now used by the authors. It has been recommended that polyacid-modified composite cements are not used for cementation.33
In conclusion, Cerana offers a leucite ceramic restoration as a cost-effective alternative to direct placement composite resin, indirect composite resin inlays, conventional indirect ceramic inlays and CAD-CAM inlays. It is particularly suited to the restoration of class 1 cavities, the closing of endodontic cavities and some class 2 lesions. Further longitudinal assessment is underway.
References
Ciucchi B, Bouillaguet S, Delaloye M, Holz J . Volume of the internal gap formed under composite restorations in vitro. J Dent 1997; 25: 305–312.
Derhami K, Coli P, Brannstrom M . Microleakage in Class 2 composite resin restorations. Oper Dent 1995; 20: 100–105.
Causton B, Millar B J, Sefton J . The deformation of cusps by bonded posterior composite restorations: An in vitro study. Br Dent J 1985; 159: 397–400.
Suliman A A, Boyer D B, Lakes R S . Cusp movement in premolars resulting from composite polymerization shrinkage. Dent Mater 1993; 9: 6–10.
Versluis A, Douglas W H, Cross M, Sakaguchi R L . Does an incremental filling technique reduce polymerization shrinkage stresses? J Dent Res 1996; 75: 871–878.
Hickel R, Manhart J . Longevity of restorations in posterior teeth and reasons for failure. J Adhes Dent 2001; 3: 45–64.
Altshuler JL, Jacobs D . Financial considerations regarding the acquisition of the Siemens Cerec computer reconstruction system. J Esthet Dent 1992; 41: 12–15.
Dickerson WG, Hastings JH . Indirect composite restorations. Curr Opin Cosmet Dent 1995; 51–56.
Burke FJT, Watts DC, Wilson NHF, Wilson MA . B Dent J 1991; 170: 269–273.
Bowen R L, Eichmiller F C, Marjenhoff W A . Glass-ceramic inserts anticipated for 'megafilled' composite restorations. Research moves into the office. J Am Dent Assoc 1991; 122: 71–75.
Bott B, Hannig M . Optimizing Class II composite resin esthetic restorations by the use of ceramic inserts. J Esthet Dent 1995; 7: 110–117.
Eichmiller F C . Clinical use of Beta-Quartz Glass-Ceramic Inserts. Compendium 1992; 13: 568–572.
Millar B J . Cerana – a direct ceramic inlay technique. Primary Dental Care 1999; 6: 59–62.
Tani Y, Nambu T, Ishikawa A, Katsuyama S . Polymerization shrinkage and contraction force of composite resin restorative inserted with 'Megafiller'. Dent Mater J 1993; 12: 182–189.
George L A, Richards N D, Eichmiller F C . Reduction of marginal gaps in composite restorations by use of glass-ceramic inserts. Oper Dent 1995: 20: 151–154.
Ozcan M, Pfeiffer P, Nergiz I . Marginal adaptation of ceramic inserts after cementation. Oper Dent 2002; 27: 132–136.
Godder B, Zhukovsky L, Trushkowsky R, Epelboym D . Microleakage reduction using glass-ceramic inserts. Am J Dent 1994; 7: 74–76.
Tani Y, Togaya T, Ishikawa A et al. Effect of 'Megafiller' insertion on the wear of composite resins. Dent Mater J 1994; 13: 174–181.
Kawai K, Leinfelder K F . Effect of glass inserts on resin composite wear. Am J Dent 1995; 8: 249–252.
El-Badrawy W A et al. Evaluation of proximal contacts of posterior composite restorations with 4 placement techniques. J Can Dent Assoc 2003; 69: 162–167.
Odman P, Nilsson E, Pietruszka K . Cerana. A new method for the restoration of teeth with prefabricated ceramic inlays. J Oral Rehab 1998; 25: 340–347.
Olmez A, Oztas N, Bilici S . Microleakage of resin composite restortations with glass-ceramic inserts. Quint Int 1998; 29: 725–729.
Odman P . A 3-year clinical evaluation of Cerana prefabricated ceramic inlays. Int J Prosthodont 2002; 15: 79–82.
Tan C L, Santini A . Marginal leakage around class V cavities restored with glass ceramic inserts of different coefficients of thermal expansion. J Clin Dent 2005; 16: 26–31.
Millar B J, Robinson P B . Initial observations with a ceramic inlay technique for sealing endodontic access cavities. Proceedings European Society Endodontics, Gothenberg, June 1997.
Millar B J, Robinson P B, Inglis A T . Clinical evaluation of an anterior hybrid composite resin over eight years. Br Dent J 1997; 182: 26–30.
Sjogren G, Hedlund S O, Jonsson C . Sandstrom A. A 3-year follow-up study of preformed beta-quartz glass-ceramic insert restorations. Quint Int 2000; 31: 25–31.
Hickel R . Manhart J . Longevity of restorations in posterior teeth and reasons for failure. J Adhesive Dent 2001; 3: 45–64.
Sjogren G, Molin M, van Dijken J W . A 10-year prospective evaluation of CAD/CAM-manufactured (Cerec) ceramic inlays cemented with a chemically cured or dual-cured resin composite. Int J Prosthod 2004; 17: 241–246.
Manhart J, Chen H Y, Neuerer P et al. Three-year clinical evaluation of composite and ceramic inlays. Am J Dent 2001; 14: 95–99.
Federlin M, Thonemann B, Schmalz G . Inserts – megafillers in composite restorations: a literature review. Clin Oral Investig 2000; 4: 1–8.
Sorenson J A . Improved seating of ceramic inlays with a silicone fit-checking medium. J Prosthet Dent 1991; 65: 646–649.
Hahn P, Schaller G, Mullner U, Hellwig E . Marginal leakage in class II-restorations after use of ceramic-inserts luted with different materials. J Oral Rehab 1998; 25: 567–574.
Bott B, Hannig M . Effect of luting materials on the marginal adaptation of Class I ceramic inlay restorations in vitro. Dental Materials 2003; 19: 264–269.
Freedman G F, Krejci I . Warming up to composites. Compendium 2004; 25: 95–98.
Author information
Authors and Affiliations
Corresponding author
Additional information
Refereed Paper
Rights and permissions
About this article
Cite this article
Millar, B., Robinson, P. Eight year results with direct ceramic restorations (Cerana). Br Dent J 201, 515–520 (2006). https://doi.org/10.1038/sj.bdj.4814159
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.bdj.4814159