Key Points
-
Shows that periodontitis patients, especially smokers, have significantly lower plasma vitamin C levels than healthy subjects.
-
Vitamin C is involved in immunological functions which make it relevant for periodontal therapy and prevention.
-
This study shows that the recommendation of vitamin C rich foods could support the management of periodontal disease.
Abstract
Objective Previous studies demonstrate a relationship between a lack of vitamin C and increased risk of periodontal disease. In the present study we examine the vitamin C plasma levels and inflammatory measures in periodontitis patients before and after the consumption of grapefruit.
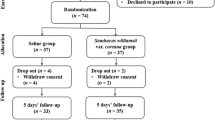
Subjects and methods Fifty-eight patients with chronic periodontitis were assigned to the test group (non-smokers n=21, smokers n=17) and a diseased control group (non-smokers n=11, smokers n=9). Furthermore, 22 healthy subjects were recruited to compare vitamin C plasma levels between periodontally diseased and healthy subjects. Clinical evaluations, including plaque index (PI), sulcus bleeding index (SBI), probing pocket depths (PPD) and plasma vitamin C levels, were performed at baseline, and after two weeks of grapefruit consumption.
Results At baseline, we observed significantly reduced plasma vitamin C levels in the test group and diseased controls in comparison with the healthy controls. On principle, smokers showed lower levels of vitamin C (mean 0.39 ± 0.17 mg dl−1) than non-smokers (mean 0.56±0.29 mg dl−1). After grapefruit consumption, the mean plasma vitamin C levels rose significantly in the test group compared to the diseased controls (non-smokers: 0.87±0.39 mg dl−1, smokers: 0.74±0.30 mg dl−1). Furthermore the SBI was reduced in the test group (non-smokers: from 1.68±0.6 to 1.05±0.6, p<0.001), whereas PI and PPD were unaffected.
Conclusion The present results show that periodontitis patients are characterised by plasma vitamin C levels below the normal range, especially in smokers. The intake of grapefruit leads to an increase in plasma vitamin C levels and improves sulcus bleeding scores. Longer term studies are necessary to determine whether other periodontal outcomes improve with such supplementation especially in smokers.
Similar content being viewed by others
Introduction
Periodontal disease is an inflammatory disorder that leads to tissue damage and bone loss as a result of complex interactions between pathogenic bacteria and the host's immune response. The majority of periodontal treatment modalities attempt to arrest the progression of periodontal destruction in order to avoid tooth loss. But there are some situations when periodontal therapy is not effective despite the provision of proper treatment. Therefore, periodontal research should attempt to identify background factors that may explain the response to therapy. Systemic factors such as a balanced nutrition or nutritional supplementation have not been thoroughly evaluated in periodontal research, although reports of the possible effects of nutrient deficiency and supplementation have appeared early in the periodontal literature.1,2,3,4
The relationship between vitamin C and periodontal disease has been of interest ever since it was observed that people with vitamin C deficiencies have loose teeth and red swollen gingiva. Former studies have dealt with the effect of vitamin C supplementation in the treatment of periodontitis.1,5,6 But there are no relevant studies evaluating increased vitamin C consumption as part of a vitamin C rich fruit diet.
It is known that vitamin C is involved in the synthesis of intercellular substances and collagen fibres of various forms of connective tissues, for example tendinous and fascial tissue and the matrix of calcified tissues such as alveolar bone and teeth. Therefore it is possible that an insufficient vitamin C supply could aggravate established periodontitis.7 Unlike most animals, humans are unable to synthesise vitamin C and must rely upon dietary intake to provide for their physiological needs. Being water-soluble, vitamin C is not retained well in the body and requires a continuous intake to maintain an adequate bodily pool.
In industrialised countries, inadequate dietary vitamin C intake is no longer considered a public health priority. But recently investigators observed inadequate vitamin C intakes in the general population and described the consequences for human health.8,9 Nishida et al.9 demonstrated, that a decreased vitamin C intake is a contributing risk factor for periodontal disease, especially in smokers. Numerous epidemiological studies have shown that smokers have a higher prevalence and severity of periodontitis when compared to non-smokers.10,11,12 The components of tobacco smoke influence directly the periodontal tissue and the immunological and inflammatory processes.13,14
The aim of this longitudinal, single-blinded randomised study was to evaluate the effects of increasing vitamin C intake through natural dietary sources upon measures of periodontal inflammation in periodontitis patients (smokers and non-smokers) before and after the consumption of two grapefruits per day.
Material and methods
Patient selection
Fifty-eight patients (mean age of 45.0 ranging from 22–75 years old), 21 males and 37 females, with chronic periodontitis were consecutively selected from the dental clinic population of the Friedrich Schiller University of Jena, Conservative Dentistry, Department of Periodontology. All patients were systemically healthy and none had received antibiotics, dietary supplements or undergone periodontal treatment in the previous six months. Thirty-eight patients (mean age of 45.3), 21 non-smokers and 17 smokers, were allocated to the test group, in which their diet was supplemented with two grapefruits daily for a period of two weeks. The grapefruits were acquired in the supermarket and all fruits had an approximate weight of 300g. Patients were instructed about the storage (cool and dark) and the consumption time (after a main meal) of the grapefruits. Furthermore, we recommended that the patients rinsed with water or milk, but did not perform toothbrushing after the grapefruit consumption to avoid enamel erosions.
The remaining subjects formed a diseased control group of 20 patients (mean age of 44.7), nine non-smokers and 11 smokers, who did not consume grapefruits. During the test period the patients received no periodontal therapy or professional cleaning.
The smoking history was checked according to a standardised questionaire. Former smokers who had quit smoking were excluded. All smokers were cigarette smokers with a median cigarette consumption of 20 cigarettes a day.
Furthermore, 22 subjects (mean age of 42.0, ranging from 24–65), eight males and 14 females, with a clinically healthy periodontium were used to compare the vitamin C plasma levels between healthy and periodontally diseased subjects. The study design is shown in Figure 1.
Informed consent was obtained from all subjects and the study was approved by the Ethic Committee of the Friedrich Schiller University of Jena.
Clinical examinations
At baseline the clinical evaluation of all study participants (test group, diseased controls and healthy controls) were carried out to characterise their periodontal conditions. Clinical measurements consisted of plaque index,15 sulcus bleeding index,16 and probing pocket depths. All teeth were evaluated at six sites per tooth.
Probing pocket depth (PPD) was assessed with a 15 mm periodontal probe (UNC-PC15) to the nearest mm. All data describing the clinical characteristics were collected by the same examiner, who was blinded with respect to the group membership of the participants.
Plasma vitamin C levels
Venous blood samples were obtained from each subject between 8:00-12:00 AM at baseline and after the observation period. The blood was collected into vacuum tubes containing EDTA. Within one hour the plasma was separated by centrifugation (4000 rpm min−1 for 10 min). Samples were stored at −80°C for a maximum of two weeks. Vitamin C levels were determined by a photometrical method as described by Terada et al.17 This method is based on the oxidation of ascorbic acid (AA) to dehydroascorbic acid (DAA) in a copper-catalyzed reaction. The addition of 2.4-dinitrophenylhydrazine is necessary for the photometric measurement. Reference values are shown in Table 2. Plasma levels below 0.65 mg dl−1 indicate a marginal deficiency without clear clinical symptoms. Plasma levels below 0.2 mg dl−1 lead to scorbutic symptoms. Vitamin C plasma levels over 0.8 mg dl−1 may help to prevent the development of cardiovascular diseases and cancer.18,19
Statistical analysis
Descriptive statistics (means of subject means) were used for mean plaque and bleeding indices and for probing pocket depths. Between group differences were examined using the Mann-Whitney U test and longitudinal changes within individual patients were analysed by paired t-test for probing pocket depth and vitamin C levels and by Wilcoxon sign rank test for indices.
Results
Clinical examinations
Table 1 provides a summary of the clinical characteristics in the test group, the diseased controls and the healthy controls. At baseline, there were no significant differences between the plaque index, sulcus bleeding index and probing pocket depths for test subjects and diseased controls. Data stratification for smoking status revealed no differences for any clinical measures between non-smokers and smokers (Table 1). The PI was significantly different between the periodontitis patients and the healthy controls (p<0.05).
Grapefruit consumption had no significant influence on PI or PPD (Table 1), but SBI scores were reduced in the test group after the intervention period (AGC). The reduction was only significant for the non-smokers.
Plasma vitamin C levels
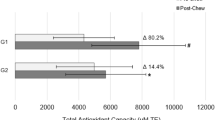
At the initial examination the majority of the periodontitis patients had plasma ascorbic acid levels below the normal range and the values of the healthy controls (Table 2 and Fig. 2). The periodontitis patients (test group and diseased controls) showed mean levels of 0.47 and 0.49 mg dl−1, while the healthy subjects expressed mean levels of 1.07 mg dl−1 (p<0.01). The comparison between non-smokers and smokers showed about 29% lower levels in smokers at baseline (Fig. 3).
Plasma ascorbic acid levels reflect the vitamin C supply to the tissues of an individual subject. Using the reference values for plasma vitamin C we compared each patient with the vitamin C supply reference level (severe undersupplied, undersupplied, normal supplied, optimal supplied; Table 2) and ascertained the percentage that fell into each category. At baseline in periodontally diseased non-smokers 71% of the patients were undersupplied and 5% were severely undersupplied with vitamin C (Fig. 4). Only 24% of the non smoking patients showed a 'sufficient' vitamin C supply. In the periodontally diseased smokers we identified 88% as undersupplied and 12% as severely undersupplied with vitamin C. None of the smoking patients had plasma ascorbic acid levels within the normal range. In the healthy controls no participant was undersupplied with vitamin C. The healthy subjects showed mean values > 0.8 mg dl−1, which indicated an optimal supply (Fig. 2).
The consumption of grapefruit over two weeks increased the ascorbic acid plasma levels in the test group independently of smoking habit of the participants (Figs 3 and 4). In non-smokers the mean values rose significantly from 0.56 mg dl−1 to 0.87 mg dl−1 (p<0.001; Fig. 3). The smoking patients showed a significant increase from 0.39 mg dl−1 to 0.74 mg dl−1 (p<0.05; Fig. 3), but they were unable to attain the same plasma levels as non-smokers. In the diseased controls (no grapefruit consumption) the ascorbic acid levels did not change significantly (Fig. 2). Re-assessment of the percentage of each group falling within the normal range for vitamin C showed a better vitamin C supply after grapefruit consumption. Forty-eight per cent of the non-smokers attained plasma levels of > 0.8 mg dl−1 (Fig. 4).
Discussion
There are many studies that have examined the association of vitamin C with periodontal disease.1,2,3,4,5,6,7 One of the important roles of vitamin C in metabolic function is collagen synthesis, particularly in the course of wound healing. This is relevant for the maintenance of oral tissues such as the periodontal ligament, the formation of bone matrix and the integrity of blood vessel walls.
The present study examined plasma vitamin C levels in periodontitis patients. At baseline, the periodontitis patients showed significantly lower plasma levels than healthy controls (with no signs of gingivitis or periodontitis). According to Nakamoto et al.2 vitamin C deficiency is a conditioning factor in the development of gingivitis. Changes in the periodontal tissues associated with vitamin C deficiency have been described as oedema, haemorrhage, osteoporosis of alveolar bone, tooth mobility and alterations of ligament fibres.
Furthermore we observed significant differences in plasma ascorbic acid levels between non-smokers and smokers. While 12% of smokers showed plasma levels below 0.2 mg dl−1 indicating severe vitamin C deficiency, only 5% of non-smokers had levels below this value (Fig. 4). These results are consistent with the recent findings of Nishida et al.9 who observed that smokers had a lower dietary vitamin C intake when compared with non-smokers. The authors presumed that smokers, for this reason, had a significantly greater incidence of periodontal disease. On the other hand the consumption of cigarettes could decrease the vitamin C pool within the body. Cigarette smoke is known to contain numerous reactive oxygen species causing tissue damage through a variety of mechanisms, including stimulation of proinflammatory cytokine release by monocytes and macrophages. Vitamin C is known as one of several compounds that form part of the body's antioxidant defence system. It has been reported that vitamin C directly neutralises free radicals, scavenges hydroxyl radicals which mediate tissue damage, and suppresses macrophage secretion of superoxide anions. The inverse relationship between smoking and plasma vitamin C levels is well reported, even for passive smoking.20 Schectman et al.21 suggested that smokers need more vitamin C to reach the same plasma levels as non-smokers. Vegetables and fruits serve as primary contributors to total vitamin C intake,22 whereas dietary supplements of vitamin C and other antioxidants have failed to demonstrate consistent therapeutic benefits,23 therefore grapefruit was choosen to influence vitamin C status. Furthermore, the integration of grapefruit in the diet is easy as the fruit is available to everyone. One grapefruit contains approximately 92.5 mg vitamin C.24 Thus two grapefruit per day supply approximately 185 mg vitamin C in addition to other micronutrients. A recent report suggests that women should consume 75 mg of vitamin C and men 90 mg daily. With two grapefruits per day the vitamin C intake in our test group increased above recommended values. The improved vitamin C intake led to increased plasma ascorbic acid levels after the intervention period of two weeks in the test group. However, the levels attained by smokers were still lower than those of non-smokers. One further study dealt also with the consumption of citrus fruits, especially oranges, to improve the oral health in children.4 The authors also measured increased plasma ascorbic acid levels after a daily consumption of three oranges. However, any comparison with our results is difficult, because the study population were children without periodontitis.
The influence of grapefruit consumption on clinical periodontal parameters was also investigated. Our results demonstrate that grapefruit consumption did not significantly influence plaque accumulation. Dilley et al.4 also observed no effect on the plaque indices after the consumption of three oranges per day in children. Further studies observed positive effects of apple consumption on plaque accumulation.25,26 The authors presumed that the fibrous texture of apples acts like a toothbrush during the act of chewing. But it is well known that appropriate hygienic measures can significantly reduce plaque levels.27
Probing pocket depths were not influenced by the grapefruit consumption in our study. A recent study tested the effect of a nutritional supplement (vitamin tablets) on the pocket formation in periodontitis patients.28 After 60 days of vitamin tablet application the pocket depths were reported to be significantly reduced. However, our study test period was too short for such effects to be expected and it is most likely that antioxidant effects on periodontal inflammation act in a preventative manner, rather than by improved healing. The shorter-term effects on gingival bleeding are more likely structural due to ascorbates role in collagen metabolism.
We observed a significant reduction of the sulcus bleeding index after grapefruit consumption. The main cause for this effect seems likely to be the improved vitamin C supply as this was the only intervention. Vitamin C plays an essential role in the collagen synthesis. It acts as a co-factor for proline and lysine-hydroxylases and influences gene transcription.29,30 A deficient collagen production causes a higher permeability of gingival tissue, which was observed in vitamin C deficient individuals. Legott et al.5 also found that vitamin C supplementation of 250 mg d−1 leads to decreased bleeding scores, which may be related to the role of vitamin C in maintaining the microvasculature structure within the sulcus. Another mechanism of vitamin C or other compounds in grapefruit could be based on antioxidant effects. Phagocytes produce reactive oxygen species (ROS) as part of their antibacterial function in response to infection with periodontopathogenic bacteria. Recent studies have shown that periodontitis subjects produce excess ROS in what is though to be a hyper-inflammatory response.31 Furthermore, studies have demonstrated compromised antioxidant defence systems in the plasma and crevicular fluid of periodontitis subjects, relative to controls.32,33 Grapefruit consumption may serve to increase the antioxidant defence system of the oral tissues and reduce periodontal inflammation in this manner.
In conclusion, the results of this study demonstrate that periodontitis patients have reduced plasma ascorbic acid levels, especially if they smoke. The consumption of two grapefruit per day improved vitamin C supply significantly and had positive effects on gingival bleeding. Increased dietary intake of vitamin C rich foods may be useful as an adjunctive measure in the management of periodontal disease. Further studies are required over more protracted periods of time and using vitamin C as an adjunt to traditional non-surgical therapy in further randomised controlled trials.
References
Aurer-Kozelj J, Kralj-Klobucar N, Buzina R, Bacic M . The effect of ascorbic acid supplementation on periodontal tissue ultrastructure in subjects with progressive periodontitis. Int J Vitam Nutr Res 1982; 52: 333–341.
Nakamoto T, McCroskey M, Mallek HM . The role of ascorbic acid deficiency in human gingivitis- a new hypothesis. J Theor Biol 1984; 108: 163–171.
Alvares O, Siegel I . Permeability of gingival sulcular epithelium in the development of scorbutic gingivitis. Oral Pathol 1981; 10: 40–48.
Dilley JG, Koerber LG, Roche JR . The effects of dietary supplement of fresh oranges on the oral health of children. ASDC J Dent Child 1977; 44: 35–41.
Leggott PJ, Robertson PB, Jacob RA, Zambon JJ, Walsh M, Armitage GC . Effects of ascorbic acid depletion and supplementation on periodontal health and microflora in humans. J Dent Res 1991; 70: 1531–1536.
Jacob RA, Omaye ST, Skala JH, Leggott PJ, Rothman DL, Murray PA . Experimental vitamin C depletion and supplementation in young men. Ann NY Acad of Sci 1987; 498: 333–346.
Väänänen MK, Markkanen HA, Tuovinen VJ, Kulaa AM, Karinpää AM, Kumpusalo EA . Periodontal health related to plasma ascorbic acid. Proc Finn Dent Soc 1993; 89: 51–59.
Taylor CA, Hampl JS, Johnston CS . Low intakes of vegetables and fruits, especially citrus fruits, lead to inadequate vitamin C intakes among adults. Eur J Clin Nutr 2000; 54: 573–578.
Nishida M, Grossi SG, Dunford RG, Ho AW, Trevisan M, Genco RJ . Dietary vitamin C and the risk of periodontal disease. J Periodontol 2000; 71: 1215–1223.
Haber J, Wattles J, Crowley M, Mandell R, Joshipura K, Kent R . Evidence for cigarette smoking as a major risk factor for periodontitis. J Periodontol 1993; 64: 16–23.
Grossi SG, Zambon JJ, Ho AW, Koch G, Dunford RG, Machtei EE, Norderyd OM Genco RJ . Assessment of risk for periodontal disease. I. Risk indicators for attachment loss. J Periodontol 1994; 65: 260–267.
Martinez-Canut P, Lorca A, Magan R . Smoking and periodontal disease severity. J Clin Periodontol 1995; 22: 743–749.
Pabst MJ, Pabst KM, Collier JA, Coleman TC, Lemons-Prince ML, Godat MS, Waring MB, Babu JP . Inhibition of neutrophil and monocyte defensive functions by nicotine. J Periodontol 1995; 66: 1047–1055.
Tappia PS, Troughton KL, Langley-Evans SC, Grimble RF . Cigarette smoking influences cytokine production and antioxidant defences. Clin Sci 1995; 88: 485–489.
Silness J, Löe H . Periodontal disease in pregnancy. II. Correlation between oral hygiene and periodontal condition. Acta Odontol Scand 1964; 22: 121–125.
Mühlemann HR, Son S . Gingival sulcus bleeding-a leading symptom in initial gingivitis. Helv Odont Acta 1971; 15: 107–113.
Terada M, Watanabe Y, Kunitomo M, Hayashi E . Differencial rapid analysis of AA and AAS by diphenyl hydrazine method. Anal Biochem 1978; 84: 604–608.
Kurl S, Tuomainen TP, Lankkanen JA, Nyyssonen K, Lakka T, Sivenius J, Salonen JT . Plasma vitamin C modifies the association between hypertension and risk of stroke. Stroke 2002; 33: 1568–1573.
Luben R, Khaw KT, Welch A, Bingham S, Wareham N, Oakes S, Day NE . Plasma vitamin C, cancer mortality and incidence in men and woman: a prospective study. IARC Sci Publ 2002; 156: 117–118.
Stefanadis C, Vlachopoulas C, Tsiamis E . Unfavourable effects of passive smoking on aortic function in men. Ann Intern Med 1998; 124: 426–434.
Schectman G, Byrd JC, Hoffmann R . Ascorbic acid requirements for smokers: analysis of a population survey. Am J Clin Nutr 1991; 53: 1466–1470.
Johnston CS, Thompson, LL . Vitamin C status of an outpatient population. J Am Coll Nutr 1998; 17: 366–370.
Wise JA, Morin RJ, Sanderson R . Changes in plasma carotenoids, alpha tocopherol and lipid peroxide levels in response to supplementation with concentrated fruit and vegetable extracts: A pilot study. Current Therapeutic Res 1996; 57: 445–461.
Sun J, Chu YF, Wu X, Liu RH . Antioxidant and antiproliferative activities of common fruits. J Agric Food Chem 2002; 50: 7449–7454.
Schneider HG, Knieknecht I: Reduction of dental plaque by apples and chewing gum. Nahrung 1986; 30: 907–912.
Harris R : Editorial: Apples and plaque. Aust Dent J 1975; 20: 43–45.
Singh SM, Rustogie KN, McCool JJ, Petrone M, Volpe AR, Korn LR, Petrone D . Clinical studies regarding plaque removal efficiancy of manual toothbrushes. J Clin Dent 1992; 3: 21–28.
Munoz CA, Kiger RD, Stephens JA, Kim J, Wilson A C: Effects of a nutritional supplement on periodontal status. Compend Contin Educ Dent 2001; 22: 425–428.
Kurata S, Senoo H, Hata R . Transcriptional activation of type I collagene genes by ascorbic acid 2-phosphate in human skin fibroblasts and its failure in cells from a patient with alpha 2 (I)-chain-defective Ehlers-Danlos syndrome. Exp Cell Res 1993; 206: 63–71.
Navas P, Villalba JM, Cordoba, F . Ascorbate functions at the plasma membrane. Biochem Biophys Acta 1994; 1197: 1–13.
Gustafsson A, Asman B, Bergstrom K . Priming response to inflammatory mediators in hyperreactive peripheral neutrophils from adult periodontitis. Oral Diseases 1997; 3: 167–171.
Chapple ILC, Brock G, Eftimiadi C, Matthews JB . Glutathione in gingival crevicular fluid and its relation to local antioxidant capacity in periodontal health and disease. J Clin Pathol: Mole Pathol 2003; 78: 367–373.
Brock G, Matthews JB, Butterworth CJ, Chapple ILC . Local and systemic total antioxidant capacity in periodontitis and health. J Clin Periodontol 2004; 31: 515–521.
Author information
Authors and Affiliations
Corresponding author
Additional information
Refereed paper
Rights and permissions
About this article
Cite this article
Staudte, H., Sigusch, B. & Glockmann, E. Grapefruit consumption improves vitamin C status in periodontitis patients. Br Dent J 199, 213–217 (2005). https://doi.org/10.1038/sj.bdj.4812613
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.bdj.4812613
This article is cited by
-
Efficacy of vitamin C supplementation as an adjunct in the non-surgical management of periodontitis: a systematic review
Systematic Reviews (2021)
-
Consumer response to media information: the case of grapefruit-medicine interaction
Health Economics Review (2015)
-
Einfluss spezieller Mikronährstoffe auf die Parodontitis
Stomatologie (2015)
-
Attitudes and practices of dentists with respect to nutrition and periodontal health
British Dental Journal (2008)
-
Lipid peroxidation and antioxidant activity in saliva of periodontitis patients: effect of smoking and periodontal treatment
Clinical Oral Investigations (2008)