Key Points
-
Inflammatory dentigerous cyst are found in mixed dentition.
-
They are associated with the roots of non-vital primary teeth and the crown of unerupted permanent successors.
-
Their roentgenographic appearance is characteristic and the nature is uncomplicated.
-
Extraction of a non-vital primary tooth and decompression of the cyst is indicated. Conservative management limits associated morbidity.
Abstract
Inflammatory dentigerous cysts are only found in the mixed dentition. The four cases presented here illustrate the uncomplicated behavior of these cysts when properly treated. By extracting the infected primary teeth, opening the cyst and ensuring continuous drainage, it is possible to achieve spontaneous eruption of the involved permanent teeth into the dental arch even if they are badly dislocated. Simultaneous with the eruption of the permanent teeth, ossification of the bony defect can take place. The reparatory process is completed in one to two years.
Similar content being viewed by others
Main
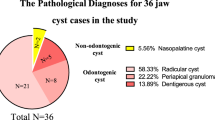
In children the frequency of odontogenic cysts is relatively low. Shear1 has estimated that about 9% of dentigerous and 1% of radicular cysts occur in the first decade of life, while according to Donath,2 about 4% of dentigerous and less than 1% of radicular cysts appear in this life period. Radicular cysts involving the primary dentition are extremely rare. Only 28 such cases were reported from 1898 to 1985, and Lustmann and Shear3 identified 23 additional cases in 1985. There are reports of children with cysts associated with carious primary teeth and the crowns of more or less dislocated permanent successors.4,5,6 Benn and Altini7 suggest that periapical inflammation from a non-vital primary tooth may spread to involve the follicle of the permanent successor. The inflammatory exudate leads to the formation of a dentigerous cyst. Main8 designated such cysts as inflammatory follicular cysts.
As evident from the literature, an inflammed follicular cyst occurs more frequently in boys than girls. It occurs between from 6–12 years of age and is ten times more likely to occur in the lower jaw than the upper.
Cysts occur most frequently in the premolar region, while primary molars are destroyed by caries and non-vital. As long as the cyst remains small it is asymptomatic and usually only found by chance, for example, during routine radiography for orthodontic reasons. Generally, a large cyst causes an intraoral buccal swelling, while at the same time it may cause a springiness of the bone. It has the potential to expand the bone, displacing adjacent teeth and may cause root deformation of developing permanent teeth.
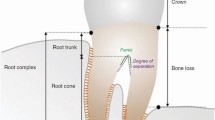
Radiographically, inflammatory denti- gerous cysts appears as a round or void, well demarcated unilocular radiolucency within the corpus of the mandible. A cyst is usually associated with the roots of a non-vital primary tooth and the crown of an unerupted permanent successor. The border is sclerotic.
In differential diagnosis, an odontogenic keratocyst and unicystic ameloblastoma must be considered. Most freq- uently, they both occur in the molar region of the lower jaw during the second and third decade of life, i.e. more distally and later in life than an inflamed follicular cyst. The radiography does not show radiolucency associated with the roots of a non-vital primary tooth and the crown of an unerupted permanent one.
Since the development of the cyst is connected with inflammation arising in a non-vital primary tooth, removal of the source of inflammation, i.e. extraction of the tooth, is logically the basic therapeutic procedure. The next step comprises opening and draining the cystic cavity. This paper describes four dentigerous inflammatory cysts that were treated by extraction of the non-vital primary tooth and decompression of the cyst. The outcome of treatment is presented.
Report of Cases
Case 1
In January 1990, a 12-year-old boy was referred to our out-patient clinic for treatment of a cyst in the left side of the mandible found on a panoramic radiograph taken three months earlier (Fig. 1a). There was a unilocular radiolucent area with sclerotic border associated with the crown of an unerupted first premolar and unresorbed roots of a primary first molar. The first premolar was dislocated caudally and medially. On discovering the cyst, the boy's dentist had extracted both left lower primary molars. Initial examination at our clinic showed that the edges of the extraction wounds had epithelialized and the cyst was draining well. Repeated radiography revealed that the cyst had already decreased in size, so that a surgical procedure was not required. The patient had had a panoramic radiograph taken in October 1986 for orthodontic reasons. The radiograph showed that the crown of the developing left first premolar was surrounded by a radiolucency broader than a normal follicle (Fig. 1b). At that time the first primary molar already had an extensive amalgam restoration. Nobody paid attention to these changes, and over the next three years the cyst reached a diameter of 3 cm. In April 1990, we extracted the left lower primary canine and after two months the permanent successor erupted. In October 1990, the crown of the first lower premolar was at the level of the alveolar arch. Because of lack of space in the dental arch we removed this tooth under local anaesthesia. The cyst was attached to the neck of the crown. Two years after the boy's first visit to our clinic, the radiolucency in the mandible completely disappeared. With orthodontic treatment the teeth came into good occlusion (Fig. 1c).
b, Already three years earlier, a radiolucency broader than a normal follicle was visible around the crown of the first lower premolar on the left. Comparison between the radiographs presented in Figs. 1a and b indicates the growth rate of the cyst. c, Final result four years after the extraction of the primary teeth. Three first premolars were extracted for orthodontic reasons. The radio-opaque element disto-apical to the left lower canine need to be radiographically followed to exclude supernumerary dentiele.
Case 2
A 10-year-old girl was referred to our out-patient clinic in September 1993 because of a painless swelling on the left side of the mandible. On the buccal surface of the mandible, the bone was thin and exhibited springiness. A panoramic radiograph showed a radiolucency into which the roots of the primary second molar and the crown of the second premolar extended. The premolar was shifted to the lower edge of the mandible. The primary second molar had an extensive amalgam restoration (Fig. 2a). At the first visit both non-vital primary molars on the left were extracted. This opened the cyst, and its liquid content leaked out. In two months the position of the second premolar improved and the radiolucency diminished. A year after extraction of the non-vital primary molars, the second premolar was about to erupt and the defect in the bone was ossified. All the teeth came into good occlusion without orthodontic treatment (Fig. 2a).
Case 3
In May 1994, a 9-year-old boy was referred to our out-patient clinic by his orthodontist, who had been consulted by the parents because of poor alignment of the lower permanent incisors. Radiography revealed a large radiolucency, extending from the premolar region on the left to that of the second incisor on the opposite side. The crown of the unerupted first premolar was tilted, and the developing canine was dislocated under the roots of the incisors (Fig. 3a). The primary molars were non-vital. On the buccal surface of the mandible, there was swelling without springiness. At the boy's first visit to our clinic, the primary canine and molars on the left side were extracted under local anaesthesia. The extraction alone did not open the cyst, but it was possible to palpate its wall. The cyst was opened by incision and the fluid leaked out. A part of the wall was sent for histopathological examination, but the specimen did not contain an epithelial component. The cavity was carefully packed with gauze soaked in Chlumsky solution. The gauze was changed every second day and removed after a week. Three and a half months later the position of the canine was improved considerably. After a year the first premolar was palpable through the drainage opening. For the next two and half years we had no contact with the patient. When seen again in March 1997, he had an ossified defect and normally erupted teeth (Fig. 3b).
Case 4
An 8-year-old girl was referred to the Department of Maxillofacial and Oral Surgery in October 1996 because of a swelling on the left side of the mandible and purulent leakage into the vestibulum. The parents had observed the changes for three months but they had not sought help as the girl did not feel any pain. On admission there was a left-sided swelling on the buccal surface of the mandible but no springiness. A panoramic radiograph showed a well-defined radiolucency of the left mandible, extending from the midline to the developing second permanent molar. The permanent canine and first premolar were displaced medially and caudally, the second incisor was shifted distally (Fig. 4a). As the first primary molar was destroyed by caries, it was extracted under general anesthesia. This opened the pus-filled cyst wide, which was then carefully packed with iodoform gauze. The girl was discharged on the third day after the operation. A tissue specimen that had been sent for histopathological examination was found to contain granulation tissue with foreign body granulomas and a solitary cyst lined by non-keratinized squamous epithelium. After a week she was provided with an acrylic plug. This was subsequently reduced in the depth once a month until May, when it was removed. In June, the cystic cavity was ossified, the left permanent canine and first premolar were about to erupt (Fig. 4b). Because of lack of space for the first premolar orthodontic treatment was started in October 1997.
a, The cyst extends nearly over the entire body of the left mandible. The canine and first premolar are severely dislocated. The cyst caused root deformation mildly affecting the second incisor and severelyaffecting the first molar. The second premolar is rotated. b, Eight months after extraction and extensive decompression of the cyst, the permanent teeth are about to erupt. The bone defect is ossified. Had the primary canine been extracted at the beginning of treatment, the permanent successor would have erupted in its proper position.
Discussion
About 70% of six-year-old children in Slovenia have one or more decayed primary teeth,9 but only a small proportion of them develop inflammatory dentigerous cysts. It seems that pulp treatment cannot prevent the development of these cysts as they have been noted to occur both after pulp treatment5,10 and in the absence of it.4
It is generally accepted that extraction of a non-vital primary tooth and marsupialization will allow rapid healing of the lesion and eruption of the permanent tooth, provided that these procedures are performed at the normal time of eruption.5,7,11,12,13 The removal of the permanent tooth may be necessary if it has suffered arrested development or is hopelessly displaced.14 Arita et al.10 have recommended enucleation of the cyst wall without removal of the permanent tooth and the use of a lingual-arch space maintainer.
All our cases, regardless of the dimension of the cyst, were treated with extraction of the non-vital primary tooth. When this failed to open the cyst, its wall was incised and iodoform gauze was inserted into the opening to provide continuous drainage. In most cases, the procedure could be performed under local anaesthesia on an out-patient basis.
The leaking out of the cyst's fluid during an extraction of a primary tooth or during a decompression, respectively, confirms the clinical impression of the cyst. If during the therapeutic procedure it is possible to gather enough tissue for a histopathological examination, it is worth undertaking it. When treating the described cases, we got the tissue of two children, but only once it was sufficient for a histopathological examination.
The permanent successors, even when badly dislocated, erupted into the dental arch, provided that there was enough space. For this reason, two children (Case 1 and Case 4) were in need of additional orthodontic treatment. Such treatment could not be avoided, even if we had inserted a space maintainer. It is our opinion, that its routine usage is not necessary. Each case should be assessed individually.
In all four patients, the bone defect ossified without complications. None of the patients showed signs of persistence or recurrence of the cyst. These results suggest that it is worth starting the treatment by decompressing the cyst even when the permanent teeth are severely displaced.
Case 1 provides information on the growth rate of inflammatory dentigerous cysts: in a three- year period the cyst reached a diameter of 3 cm (Figs 1a, b). Shear1 has shown radiologically that dentigerous cysts measuring 4–5 cm in diameter may develop in 3–4 years.
Conclusions
Inflammatory dentigerous cysts can be treated successfully by extraction of the non-vital or carious primary tooth and decompression of the cystic cavity. The procedure can be done under local anaesthesia. However, the patient must be followed up until eruption of the displaced permanent teeth and bony consolidation of the cyst.
References
Shear M. Cysts of the oral regions. (3rd ed). Oxford: Write, 1992.
Donath K . Odontogene und nicht-odontogene Kieferzysten. Dtsch Zahnärztl Z 1985; 40: 502–509.
Lustmann J, Shear M . Radicular cysts arising from deciduous teeth. Int J Oral Surg 1985; 14: 153–161.
Azaz B, Shteyern A . Dentigerous cyst associated with second mandibular bicuspids in children: Report of five cases. J Dent Child 1973; 40: 29–31.
Shaw W, Smith M, Hill F . Inflammatory follicular cysts. J Dent Child 1980; 47: 97–101.
Benn A, Ackermann G L, Altini M . The role of deciduous teeth in the pathogenesis of odontogenic cysts. J Dent Res 1990; 69: 1092.
Benn A, Altini M . Dentigerous cysts of inflammatory origin. A clinicopathogenic study. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 1996; 81: 203–209.
Main D M G . Epithelial jaw cysts: 10 years of the WHO classification. J Oral Pathology 1985; 14, 1–7.
Vrbiè V . Periodièna obdobna raziskava oralnega zdravja doloèenih starostnih skupin. In Vrbiè V (ed). Oralno zdravje v Sloveniji. 1995; p 21. Ljubljana: Medicinska fakulteta.
Arita K, Amo M, Kamada K, Yanagawa T, Nishino M . Dentigerous cysts of children treated by cyst wall enucleation. Report of eleven cases. Shoni Shikagaku Zasshi 1989; 27: 197–207.
Horch H H, (ed) Zahnärztliche Chirurgie. 2nd ed. München: Urban & Schwarzenberg, 1989.
Ellis III E . Surgical management of oral pathologic lesions. Contemporary Oral and Maxillofacial Surgery. 3rd ed. In Peterson L J, Ellis III E, Hupp J R, Tucker M R (eds). 1998. pp 533–545. St Louis: Mosby.
Takagi S, Koyama S . Guided eruption of an impacted second premolar associated with a dentigerous cyst in the maxillary sinus of a 6-year-old child. J Oral Maxillofac Surg 1998; 56: 237–239.
Brook A H, Winter G B . Development arrest of permanent tooth germs following pulpal infection of deciduous teeth. Br Dent J 1975; 139: 9–11.
Author information
Authors and Affiliations
Additional information
Refereed paper
Rights and permissions
About this article
Cite this article
Koželj,, V., Sotošek,, B. Inflammatory dentigerous cysts of children treated by tooth extraction and decompression—report of four cases. Br Dent J 187, 587–590 (1999). https://doi.org/10.1038/sj.bdj.4800339
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.bdj.4800339
This article is cited by
-
Coincidental Overlapping Cystic Pathological Changes: A Case against Marsupialisation
Journal of Maxillofacial and Oral Surgery (2013)
-
Odontogenic Cysts: Analysis of 680 Cases in Brazil
Head and Neck Pathology (2008)