Abstract
We evaluated the impact of genomic polymorphisms in folate-metabolizing, DNA synthesis and DNA repair enzymes on the clinical outcome of 108 patients with myelodysplastic syndromes (MDS) receiving best supportive care (BSC) or azacitidine. A statistically significant association between methylenetetrahydrofolate reductase (MTHFR) 677T/T, thymidylate synthase (TS) 5′-untranslated region (UTR) 3RG, TS 3′-UTR −6 bp/−6 bp, XRCC1 399G/G genotypes and short survival was found in patients receiving BSC by multivariate analysis (P<0.001; P=0.026; P=0.058; P=0.024). MTHFR 677T/T, TS 3′-UTR −6 bp/−6 bp and XRCC1 399G/G genotypes were associated with short survival in patients receiving azacitidine by multivariate analysis (P<0.001; P=0.004; P=0.002). We then performed an exploratory analysis to evaluate the effect of the simultaneous presence of multiple adverse variant genotypes. Interestingly, patients with ⩾1 adverse genetic variants had a short survival, independently from their International Prognostic Scoring System (IPSS) and therapy received. To our knowledge, this is the first study showing that polymorphisms in folate-metabolizing pathway, DNA synthesis and DNA repair genes could influence survival of MDS patients.
Similar content being viewed by others
Introduction
Myelodysplastic syndromes (MDS) are a heterogeneous group of hematological malignancies characterized by ineffective hematopoiesis and risk for progression to acute myeloid leukemia (AML). Similar to other malignant diseases, myelodysplasia and its progression to AML is a genomic instability disorder, resulting from a stepwise accumulation of genetic abnormalities, probably because of an increased DNA damage burden and/or reduced ability to deal with the damage.1, 2
Folate is an important nutrient required for DNA synthesis and methylation because it provides one-carbon donor for the synthesis of de novo purines and pyrimidines, and remethylation of homocysteine for methylation reaction of protein, DNA and RNA. Its deficiency has been associated with various vascular and neurological diseases, as well as with diabetes, psoriasis and malignancies and acute lymphoblastic leukemia.3 Both genetic stability of the cell and DNA methylation could be modulated by folate level. An imbalance between entities in folic acid metabolism can adversely affect nucleotide synthesis, DNA repair and methylation systems, leading to impairments in chromosome segregation, abnormal expression of pro-oncogenes and inactivation of tumor suppressor genes.4 As a consequence, an alteration in folic acid metabolism could have an effect on DNA repair efficiency and genomic stability.
Thymidylate synthase (TS) catalyzes the conversion of deoxyuridine monophosphate to deoxythymidine monophosphate using 5,10-methylenetetrahydrofolate, a substrate of methylenetetrahydrofolate reductase (MTHFR) enzyme, during DNA synthesis. Impairment in the TS enzyme has been associated with chromosomal damage and fragile site induction.5 The role of the TS polymorphisms remains unclear and it may influence TS mRNA stability in vitro and its expression in vivo.6, 7 It has been shown that TS could be involved in the etiopathogenesis of AML and chronic myeloid leukemia.5
The base excision repair pathway is responsible for the repair of little DNA lesions, as single-strand lesions, oxidative damage, alkylation or methylation. The base excision repair pathway is a multistep process that requires the activation of several proteins and the functional polymorphism in these genes may be responsible for an altered DNA repair capacity.2, 8
It is well known that the presence of functional polymorphisms in genes affects, in general, the respective enzyme activities. As an example, two known polymorphisms in the MTHFR gene, C677T and A1298C, lead to a 30–60% reduction in enzyme activity.9, 10, 11
Population-based studies have shown an association between genetic polymorphisms in folate-metabolizing pathway, DNA synthesis and DNA repair and solid and hematological diseases.12, 13, 14, 15, 16, 17, 18, 19, 20, 21 Some of these studies also showed an association between specific polymorphisms and decreased of survival after chemotherapy.8 As an example, Kim et al.5 reported that (1) MTHFR 677TT genotype is associated with a significantly increased risk for adult acute lymphoblastic leukemia, (2) TS polymorphisms are involved in the etiopathogenesis of AML and (3) both DNA synthesis and methylation play important roles in the pathogenesis of AML and MDS.
The impact of genomic polymorphisms of folate-metabolizing, DNA synthesis and DNA repair enzymes on risk and clinical outcome in patients with hematological disease has been previously reported, but there are no data on MDS. Moreover, because of the large clinical use of hypomethylating agents that modulate the methylation of patients with MDS, in the absence of a marker predictive of response, it sounds scientifically good to us to evaluate genetic variants of genes involved not only in the methylation pathway, but also in important metabolic checkpoints relevant for DNA synthesis and repair.
Therefore, we conducted a study to examine the relationship between nine polymorphisms in five genes (MTHFR, TS, XRCC1, XRCC3 and APE1) and survival in patients with MDS. We started by analyzing patients receiving azacitidine, and therefore we studied the same genetics variants in patients receiving supportive care only.
Materials and methods
Study population
The study was approved by the reference ethics committee and was carried out in accordance with the International Conference on Harmonization Good Clinical Practice Guidelines, the Declaration of Helsinki (1996) and local regulatory requirements and laws. All patients signed informed consent before entering the study. The characteristics of the 108 patients enrolled between September 2009 and March 2015 (age, diagnosis, International Prognostic Scoring System (IPSS) risk category and so on) are listed in Table 1.
Genotype analysis
We performed analyses of nine genetic variants, single-nucleotide polymorphism and variable number tandem repeat on five genes as follows: genomic DNA was isolated from 1 ml of peripheral blood by means of commercially available kit (QIAamp DNA Blood Midi kit, Hilden, Germany) according to the manufacturer’s instructions. The laboratory analyses were performed blind to the patients’ treatment and clinical outcomes. All samples were genotyped for the following polymorphisms: MTHFR C677T (Ala222Val; rs1801133) and A1298C (Glu429Ala; rs801131), TS 5′- untranslated region (UTR) (rs183205964 2R/3R and rs 2853542 3R G/C) and 3′-UTR (rs11280056 −6 bp/+6T/T bp), XRCC1 Arg194Trp (rs1799782 C/T) and Arg399Glu (rs25487 G/A), XRCC3 Thr241Met (rs861539 C/T) and APE1 Asp148Glu (rs1130409 T/G).
Polymorphisms were detected by PCR high-resolution melting assay, restriction fragment length polymorphism of PCR products and PCR-pyrosequencing assay. PCR conditions and additional details are listed in Table 2.
The PCR for restriction fragment length polymorphism and pyrosequencing analyses were performed in a volume of 25 μl using 2 × PCR Master Mix kit (Diatheva, Fano, Italy), 25 ng of genomic DNA and 200 nM of each primer. Primer sequences and preparative PCR conditions are reported in Table 2. The PCR high-resolution melting assays were performed by using commercial kits according to the manufacturer’s instructions (Diatheva).22
Statistical analysis
We checked whether the polymorphisms showed any deviations from Hardy–Weinberg equilibrium. The frequencies of each polymorphism in the cohort of patients were compared with the general Italian population (TSI, Tuscany http://www.ensembl.org/info/genome/variation/index.html).
We separately analyzed two groups of patients according to IPSS stage and therapy administered. The first group consisted of 54 patients with intermediate-2 and high IPSS treated with azacitidine (AZA group), whereas the second group consisted of 54 patients with low and intermediate-1 IPSS receiving only best supportive care (BSC group).
Demographic (age, sex), clinical (hemoglobin level, IPSS) and biological (karyotype) prognostic features were compared across genotypes, using Pearson’s χ2 tests (for categorical variables) and Mann–Whitney test and Kruskal–Wallis tests (for continuous variables), where appropriate.
Additive, dominant (major homozygous plus heterozygous vs minor homozygous) and recessive (major homozygous vs heterozygous plus minor homozygous) models were applied to detect associations between genotypes and overall survival (OS). OS was calculated from the data of diagnosis to last known date alive, or death. The association between the cumulative probability of OS among genotypes or haplotypes was calculated according to the Kaplan–Meier method, whereas significant differences between survival curves were evaluated with log-rank test. Multivariable analysis was performed by stepwise logistic regression model, describing as the hazard ratio and 95% confidence interval. Statistical significance was set at P<0.05. All statistical testing was done using Statistical Package for the Social Sciences SPSS version 20 (SPSS, Chicago, USA).
Results
Genotype frequencies
The genotype frequencies for each polymorphism are presented in Table 2; they are not significantly different than what would be expected if the population was in Hardy–Weinberg equilibrium. No statistically significant association was found between demographic, clinical or prognostic features and all the studied polymorphisms (data not shown). The frequencies of genotypes identified in this study were similar to those reported in the TSI population.
Survival and genotypes
We evaluated the impact of the genetic variants in MTHFR, TS, XRCC1, XRCC3 and APE1 genes on the survival of the two groups of MDS patients enrolled in the study.
In univariate analysis, the comparison of genotypes in the BSC group showed that patients with homozygous MTHFR 677T/T, TS 5′-UTR 3RG, TS 3′-UTR −6 bp/−6 bp and XRCC1 399G/G had a shorter survival when compared with patients with the other variant (heterozygous plus the other homozygous). Multivariate stepwise regression model confirmed these genotypes to be strong independent prognostic factors, significantly associated with short survival (Table 3).
Interestingly, the comparison of genotypes in the AZA group confirmed that patients with homozygous MTHFR 677T/T, TS 3′-UTR −6/−6 and XRCC1 399G/G had a shorter survival when compared with patients with the other variant (heterozygous plus the other homozygous) in both univariate and multivariate analyses (Table 4).
No significant association was found between other enzymatic polymorphisms and MDS subtypes (data not shown). In particular, we did not observe any effect of adverse cytogenetics aberration, when tested alone, on survival. Regarding novel molecular mutations, we did not evaluate their possible adverse effect on OS due to the fact that this group of patients was enrolled and treated in a pre-NGS era, and we do not have residual genetic samples to test molecular mutations now.
Combination of variant genotypes and survival
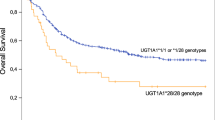
We then performed an exploratory analysis to evaluate which impact could have the simultaneous presence of multiple adverse variant genotypes on survival in both groups (BSC and AZA groups). Patients were stratified according to the number of adverse genotypes. A strong, negative effect on OS was observed in patients with multiple adverse genotypes. In the BSC group, the 3-year OS was 33% for patients with ⩾2 variant alleles as compared with 62.5% and 100%, respectively, for those with 2 or 0/1 variant alleles (Figure 1a). The predictive role of the combination of adverse genotypes on survival was also confirmed in the AZA group (Figure 1b), suggesting that patients with a higher number of genetic variants in genes involved in DNA synthesis, repair and in folate pathway had a short survival, independently from their IPSS score and therapy received.
Combined effects of adverse genotypes. (a) Overall survival of myelodysplastic syndrome (MDS) patients with low/intermediate-1 (int-1) International Prognostic Scoring System (IPSS) treated with best supportive care, according to the number of adverse genotypes simultaneously occurring. (b) Overall Survival of MDS patients with intermediate-2 (int-2)/high-risk IPSS treated with azacitidine, according to the number of adverse genotypes simultaneously occurring.
Discussion
MDS have been presumed to be stem cell disorders, and it has been suspected that the development of MDS results from accumulation of multiple gene abnormalities, similar to solid cancer. Elucidation of associations between gene mutations and clinical phenotypes has advanced rapidly in MDS, whereas the molecular pathogenesis based on the function of each variant has not been fully clarified yet.23 Several studies have previously demonstrated the importance of genetic background on individual risk of developing cancer, drug sensitivity and patient survival.24, 25 Moreover, these studies showed that genetic susceptibility to develop cancer could be the result of the net effect of multiple single-nucleotide polymorphisms in genes implicated in various molecular pathways.26 Accordingly, single-nucleotide polymorphisms could possibility upset the balance between the most important metabolic pathways and therefore influence the development and progression of cancer by modifying the activity, stability and level of the corresponding enzymes. Moreover, it has been postulated5 that hematological malignancies are associated with alterations of plasma folate levels or DNA repair genes, but the number of patients studied, difference genotype frequencies and different ethnicities may influence the results.
In this study, we demonstrated, for the first time, that MTHFR 677TT, TS 3′-UTR −6/−6 and XRCC1 399GG genetic polymorphisms are associated with statistically significant short survival in MDS patients in both univariate and multivariate analyses. These findings are true either for patients with low-risk MDS, receiving supportive care only, or for high-risk MDS, receiving hypomethylating therapy with azacitidine. This latter finding, if confirmed in larger series, could be of particular interest, because so far there is no validated marker predictive of response to azacitidine, and the role of global gene-specific methylation is not well defined.
Starting from this, we then evaluated whether the negative effect on survival of MTHFR 677TT, TS 3′-UTR −6/−6 and XRCC1 399GG genetic polymorphisms could increase when multiple adverse variants simultaneously occur. When we performed an exploratory analysis to test this hypothesis, we found that patients with a higher number of variant alleles had a worse survival outcome (Figure 1a and b).
We know that the two cohorts of patients are not comparable, and we did not want to directly compare them. However, our study showed that patients with ⩾1 adverse genetic variants had a short survival, independently from their IPSS score and therapy received. In other words, even if low-risk patients receiving BSC only and high-risk patients receiving azacitidine are not comparable because of clinical characteristics, IPSS score and therapy received, the presence of ⩾1 adverse genetic variants in any of these cohorts seems to independently affect survival. Indeed, the simultaneous presence of similar, adverse genotypes influences survival in both cohorts of patients. Last but not least, azacitidine does not perform well in patients with IPSS intermediate-2 or high bearing ⩾1 adverse genotypes. This finding, if confirmed in larger series, should be taken in account in order to avoid toxicity in patients who have a low probability to respond. On the contrary, azacitidine should be prospectively tested in patients with IPSS low or intermediate-1 bearing ⩾1 adverse genotypes, who had a dismal survival with BSC only.
We do not know whether the underlying mechanism of MDS or its progression to AML could be the result of a defect in one or more pathways involved in methylation and/or DNA repair. At present, clinical prognostic scores, such as IPSS, WHO Prognostic Scoring System (WPSS) or Revised-IPSS (R-IPSS), seem to be the most powerful tools to predict survival time for MDS patients, together with adverse mutation of few genes detected with NGS techniques. Even if we do not have next-generation sequencing data to evaluate the presence of adverse mutation, such as ASLX1 and SRSF2, in our cohort of patients, our results show that MDS patients with one or more unfavorable genotype(s) in the studied pathways have a worse survival, independently from their risk score at diagnosis. Therefore, it will be necessary, in the future, to validate our results and correlate them with the presence or not of driver mutation together with adverse genetic polymorphisms.
In any case, a possible explanation for the discrepancy between survival expected from clinical prognostic score and OS resulting from the presence of multiple adverse genetic variants could be attributed to the perturbation of folate and methionine status because of the presence of polymorphisms in the metabolizing enzyme genes. Folate is an important nutrient required for DNA synthesis and methylation, because it provides one-carbon donors for the synthesis of de novo purines and pyrimidines and remethylation of homocysteine for methylation reaction of protein, DNA and RNA. Folate deficiency may cause DNA hypomethylation and pro-oncogene activation and/or uracil misincorporation during DNA synthesis, leading to catastrophic DNA repair, DNA strand breakage and chromosome damage. This process could be powered by the failure of the enzymatic activity of the enzymes of the DNA synthesis and repair that could lead to cell death by apoptosis or progression to AML.
Moving to DNA methylation, a well-recognized key regulatory of gene expression, few studies supported a crucial role of epigenetic changes in MDS and leukemia biology, as well as a potential impact in patient outcome.27 Using a supervised approach, Bullinger et al.27 demonstrated a significant association of altered DNA methylation and patient outcome (good or poor survival) of AML patients. Moreover, the authors were able to build a predictive model based on quantitative DNA methylation patterns.27
However, recent studies reported that there is little relation between the degree of demethylation following hypomethylating treatment and hematologic response in patients with MDS.28 In other words, methylation is not a predictive marker of response to hypomethylating agents for MDS patients, and therefore we cannot decide which patient can be a good candidate to receive these drugs taking only in account the degree of methylation. In this view, polymorphism in key genes regulating not only the metabolism of the cell, but also its sensitivity to certain type of drug, MDS specific, could represent a novel predictive marker that surely warrants further studies.
To the best of our knowledge, this is the first study showing that polymorphisms in folate-metabolizing pathway, DNA synthesis and DNA repair genes could affect survival outcome of patients with MDS. Additional studies, with a larger sample size, and able to correlate our pharmacogenomics data with novel next-generation sequencing data, are warranted. In this view, it is mandatory to further explore the associations between MTHFR, TS and XRCC1 genetic polymorphisms and survival of MDS patient treated with hypomethylating agents.
References
Zhou T, Hasty P, Walter CA, Bishop AJR, Scott LM, Rebel VI . Myelodypslastic syndrome: an inability to appropriately respond to damage DNA? Exp Hematol 2013; 41: 665–674.
Seedhouse C, Russell N . Susceptibility to MDS: DNA repair and detoxification genes. In: Várkonyi J (ed). The Myelodysplastic Syndromes 2011, XIII, 286p; 2 5–24.
Liew SC, Gupta DE . Methylenetetrahydrofolate reductase (MTHFR) C677T polymorphism: epidemiology, metabolism and associated diseases. Eur J Med Genet 2015; 58: 1–10.
Weiner AS, Beresina OV, Voronina EN, Voropaeva EN, Boyarskih UA, Pospelova TI et al. Polymorphisms in folate-metabolizing genes and risk of non-Hodgkin's lymphoma. Leuk Res 2011; 35: 508–515.
Kim HN, Kim YK, Lee IK, Yang DH, Lee JJ, Shin MH et al. Association between polymorphisms of folate-metabolizing enzymes and hematological malignancies. Leuk Res 2009; 33: 82–87.
Krajinovic M, Lemieux-Blanchard E, Chiasson S, Primeau M, Costea I, Moghrabi A . Role of polymorphisms in MTHFR and MTHFD1 genes in the outcome of childhood acute lymphoblastic leukemia. Pharmacogenomics J 2004; 4: 66–72.
Wang L, Ke Q, Chen W, Wan J, Tan Y, Zhou Y et al. Polymorphisms of MTHFD plasma homocisteine levels and risk of gastric cancer in a high-risk Chinese population. Clin Cancer Res 2007; 13: 2526–2532.
Bewick MA, Conlon MSC, Lafrenie RM . Polymorphisms in XRCC1 XRCC3, and CCND1 and survival after treatment for metastatic breast cancer. J Clin Oncol 2006; 24: 5645–5651.
Lucock M . Folic acid: nutritional biochemistry, molecular biology, and role in disease processes. Mol Genet Metab 2000; 71: 121–138.
Frosst P, Blom HJ, Milos R, Goyette P, Sheppard CA, Matthews RG et al. A candidate genetic risk factor for vascular disease: a common mutation in methylenetetrahydrofolate reductase. Nat Genet 1995; 10: 111–113.
Van der Put NM, Gabreëls F, Stevens EM, Smeitink JA, Trijbels FJ, Eskes TK et al. A second common mutation in the methylenetetrahydrofolate reductase gene: an additional risk factor for neural-tube defects? Am J Hum Genet 1998; 62: 1044–1051.
Wang L, Habuchi T, Mitsumori K, Li Z, Kamoto T, Kinoshita H et al. Increased risk of prostate cancer associated with AA genotype of cyclin D1 gene A870G polymorphism. Int J Cancer 2003; 103: 116–120.
Lockett KL, Snowhite IV, Hu JJ . Nucleotide excision repair and prostate cancer risk. Cancer Lett 2005; 220: 125–135.
Shen M, Hung RJ, Brennan P, Malaveille C, Donato F, Placidi D et al. Polymorphisms of the DNA repair genes XRCC1, XRCC3, XPD, interaction with environmental exposures, and bladder cancer risk in a case-control study in northern Italy. Cancer Epidemiol Biomarkers Prev 2003; 12 (11 Pt 1): 1234–1240.
Han J, Hankinson SE, Colditz GA, Hunter DJ . Genetic variation in XRCC1, sun exposure, and risk of skin cancer. Br J Cancer 2004; 91: 1604–1609.
Zhang X, Miao X, Liang G, Hao B, Wang Y, Tan W et al. Polymorphisms in DNA base excision repair genes ADPRT and XRCC1 and risk of lung cancer. Cancer Res 2005; 65: 722–726.
Porter TR, Richards FM, Houlston RS, Evans DG, Jankowski JA, Macdonald F et al. Contribution of cyclin d1 (CCND1) and E-cadherin (CDH1) polymorphisms to familial and sporadic colorectal cancer. Oncogene 2002; 21: 1928–1933.
Skibola CF, Smith MT, Kane E, Roman E, Rollinson S, Cartwright RA et al. Polymorphisms in the methylenetetrahydrofolate reductase gene are associated with susceptibility to acute leukemia in adults. Proc Natl Acad Sci USA 1999; 96: 12810–12815.
Skibola CF, Smith MT, Hubbard A, Shane B, Roberts AC, Law GR et al. Polymorphisms in the thymidylate synthase and serine hydroxymethyltransferase genes and risk of adult acute lymphocytic leukemia. Blood 2002; 99: 3786–3791.
Wiemels JL, Smith RN, Taylor GM, Eden OB, Alexander FE, Greaves MF, United Kingdom Childhood Cancer Study investigators. Methylenetetrahydrofolate reductase (MTHFR) polymorphisms and risk of molecularly defined subtypes of childhood acute leukemia. Proc Natl Acad Sci USA 2001; 98: 4004–4009.
Hur M, Park JY, Cho HC, Lee KM, Shin HY, Cho HI . Methylenetetrahydrofolate reductase A1298C genotypes are associated with the risks of acute lymphoblastic leukaemia and chronic myelogenous leukaemia in the Korean population. Clin Lab Haematol 2006; 28: 154–159.
Ruzzo A, Graziano F, Kawakami K, Watanabe G, Santini D, Catalano V et al. Pharmacogenetic profiling and clinical outcome of patients with advanced gastric cancer treated with palliative chemotherapy. J Clin Oncol 2006; 24: 1883–1891.
Harada H, Harada Y . Recent advances in myelodysplastic syndromes: molecular pathogenesis and its implications for targeted therapies. Cancer Sci 2015; 106: 329–336.
Voso MT, Fabiani E, D’Alo F, Guidi F, Di Ruscio A, Sica S et al. Increased risk of acute myeloid leukemia due to polymorphisms in detoxification and DNA repair enzymes. Ann Oncol 2007; 18: 1523–1528.
Kawakami K, Graziano F, Watanabe G, Ruzzo A, Santini D, Catalano V et al. Prognostic role of thymidylate synthase polymorphisms in gastric cancer patients treated with surgery and adjuvant chemotherapy. Clin Cancer Res 2005; 11: 3778–3783.
Weiner AS, Beresina OV, Voronina EN, Voropaeva EN, Boyarskih UA, Pospelova TI et al. Polymorphisms in folate-metabolizing genes and risk of non-Hodgkin's lymphoma. Leuk Res 2011; 35: 508–515.
Bullinger L, Ehrich M, Döhner K, Schlenk RF, Döhner H, Nelson MR et al. Quantitative DNA methylation predicts survival in adult acute myeloid leukemia. Blood 2009; 115: 636–642.
Voso MT, Santini V, Fabiani E, Fianchi L, Criscuolo M, Falconi G et al. Why methylation is not a marker predictive of response to hypomethylating agents. Haematologica 2014; 99: 613–619.
Acknowledgements
The study was supported in part by AIL Pesaro Onlus.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
PowerPoint slides
Rights and permissions
This work is licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International License. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in the credit line; if the material is not included under the Creative Commons license, users will need to obtain permission from the license holder to reproduce the material. To view a copy of this license, visit http://creativecommons.org/licenses/by-nc-sa/4.0/
About this article
Cite this article
Visani, G., Loscocco, F., Ruzzo, A. et al. MTHFR, TS and XRCC1 genetic variants may affect survival in patients with myelodysplastic syndromes treated with supportive care or azacitidine. Pharmacogenomics J 18, 444–449 (2018). https://doi.org/10.1038/tpj.2017.48
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/tpj.2017.48