Abstract
Discovery of clinical and genetic predictors of exemestane pharmacokinetics was attempted in 246 postmenopausal patients with breast cancer enrolled on a prospective clinical study. A sample was collected 2 h after exemestane dosing at a 1- or 3-month study visit to measure drug concentration. The primary hypothesis was that patients carrying the low-activity CYP3A4*22 (rs35599367) single-nucleotide polymorphism (SNP) would have greater exemestane concentration. Additional SNPs in genes relevant to exemestane metabolism (CYP1A1/2, CYP1B1, CYP3A4, CYP4A11, AKR1C3/4, AKR7A2) were screened in secondary analyses and adjusted for clinical covariates. CYP3A4*22 was associated with a 54% greater exemestane concentration (P<0.01). Concentration was greater in patients who reported White race, had elevated aminotransferases, renal insufficiency, lower body mass index and had not received chemotherapy (all P<0.05), and CYP3A4*22 maintained significance after adjustment for covariates (P<0.01). These genetic and clinical predictors of exemestane concentration may be useful for treatment individualization in patients with breast cancer.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 6 print issues and online access
$259.00 per year
only $43.17 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
References
Coombes RC, Hall E, Gibson LJ, Paridaens R, Jassem J, Delozier T et al. A randomized trial of exemestane after two to three years of tamoxifen therapy in postmenopausal women with primary breast cancer. N Engl J Med 2004; 350: 1081–1092.
Pagani O, Regan MM, Walley BA, Fleming GF, Colleoni M, Láng I et al. Adjuvant exemestane with ovarian suppression in premenopausal breast cancer. N Engl J Med 2014; 371: 107–118.
Henry NL, Azzouz F, Desta Z, Li L, Nguyen AT, Lemler S et al. Predictors of aromatase inhibitor discontinuation as a result of treatment-emergent symptoms in early-stage breast cancer. J Clin Oncol 2012; 30: 936–942.
Henry NL, Giles J, Ang D, Mohan M, Dadabhoy D, Robarge J et al. Prospective characterization of musculoskeletal symptoms in early stage breast cancer patients treated with aromatase inhibitors. Breast Cancer Res Treat 2008; 111: 365–372.
Early Breast Cancer Trialists' Collaborative Group (EBCTCG) Early Breast Cancer Trialists' Collaborative Group (EBCTCG) Dowsett M, Forbes JF, Bradley R, Ingle J, Aihara T et al. Aromatase inhibitors versus tamoxifen in early breast cancer: patient-level meta-analysis of the randomised trials. Lancet 2015; 386: 1341–1352.
Jannuzzo MG, Poggesi I, Spinelli R, Rocchetti M, Cicioni P, Buchan P . The effects of degree of hepatic or renal impairment on the pharmacokinetics of exemestane in postmenopausal women. Cancer Chemother Pharmacol 2004; 53: 475–481.
King PD, Perry MC . Hepatotoxicity of chemotherapy. Oncologist 2001; 6: 162–176.
Helsby NA, Lo WY, Sharples K, Riley G, Murray M, Spells K et al. CYP2C19 pharmacogenetics in advanced cancer: compromised function independent of genotype. Br J Cancer 2008; 99: 1251–1255.
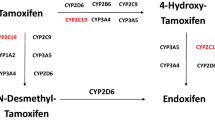
Kamdem LK, Flockhart DA, Desta Z . In vitro cytochrome P450-mediated metabolism of exemestane. Drug Metab Dispos 2011; 39: 98–105.
Elens L, Nieuweboer A, Clarke SJ, Charles KA, de Graan AJ, Haufroid V et al. CYP3A4 intron 6 C>T SNP (CYP3A4*22) encodes lower CYP3A4 activity in cancer patients, as measured with probes midazolam and erythromycin. Pharmacogenomics 2013; 14: 137–149.
Elens L, van Gelder T, Hesselink DA, Haufroid V, van Schaik RH . CYP3A4*22: promising newly identified CYP3A4 variant allele for personalizing pharmacotherapy. Pharmacogenomics 2013; 14: 47–62.
Diekstra MH, Klumpen HJ, Lolkema MP, Yu H, Kloth JS, Gelderblom H et al. Association analysis of genetic polymorphisms in genes related to sunitinib pharmacokinetics, specifically clearance of sunitinib and SU12662. Clin Pharmacol Ther 2014; 96: 81–89.
Teft WA, Gong IY, Dingle B, Potvin K, Younus J, Vandenberg TA et al. CYP3A4 and seasonal variation in vitamin D status in addition to CYP2D6 contribute to therapeutic endoxifen level during tamoxifen therapy. Breast Cancer Res Treat 2013; 139: 95–105.
Desta Z, Kreutz Y, Nguyen AT, Li L, Skaar T, Kamdem LK et al. Plasma letrozole concentrations in postmenopausal women with breast cancer are associated with CYP2A6 genetic variants, body mass index, and age. Clin Pharmacol Ther 2011; 90: 693–700.
Henry NL, Jacobson JA, Banerjee M, Hayden J, Smerage JB, Van Poznak C et al. A prospective study of aromatase inhibitor-associated musculoskeletal symptoms and abnormalities on serial high-resolution wrist ultrasonography. Cancer 2010; 116: 4360–4367.
Hertz DL, Kidwell KM, Thibert JN, Gersch C, Regan MM, Skaar TC et al. Genotyping concordance in DNA extracted from formalin-fixed paraffin embedded (FFPE) breast tumor and whole blood for pharmacogenetic analyses. Mol Oncol 2015; 9: 1868–1876.
Tobin J . Estimation of relationships for limited dependent variables. Econometrica 1958; 26: 24–36.
Hillis SL . Residual plots for the censored data linear regression model. Stat Med 1995; 14: 2023–2036.
Cockcroft DW, Gault MH . Prediction of creatinine clearance from serum creatinine. Nephron 1976; 16: 31–41.
Werk AN, Cascorbi I . Functional gene variants of CYP3A4. Clin Pharmacol Ther 2014; 96: 340–348.
Westlind-Johnsson A, Hermann R, Huennemeyer A, Hauns B, Lahu G, Nassr N et al. Identification and characterization of CYP3A4*20, a novel rare CYP3A4 allele without functional activity. Clin Pharmacol Ther 2006; 79: 339–349.
Wilkinson GR . Drug metabolism and variability among patients in drug response. N Engl J Med 2005; 352: 2211–2221.
Lee S, Goldstein JA . Functionally defective or altered CYP3A4 and CYP3A5 single nucleotide polymorphisms and their detection with genotyping tests. Pharmacogenomics 2005; 6: 357–371.
Sanghavi K, Brundage RC, Miller MB, Schladt DP, Israni AK, Guan W et al. Genotype-guided tacrolimus dosing in African-American kidney transplant recipients. Pharmacogenomics J; advance online publication, 15 December 2015; doi:10.1038/tpj.2015.87 [e-pub ahead of print].
Sawesi S, Carpenter JS, Jones J . Reasons for nonadherence to tamoxifen and aromatase inhibitors for the treatment of breast cancer: a literature review. Clin J Oncol Nurs 2014; 18: E50–E57.
Flegal KM, Carroll MD, Ogden CL, Johnson CL . Prevalence and trends in obesity among US adults, 1999-2000. JAMA 2002; 288: 1723–1727.
Moy B, Tu D, Pater JL, Ingle JN, Shepherd LE, Whelan TJ et al. Clinical outcomes of ethnic minority women in MA.17: a trial of letrozole after 5 years of tamoxifen in postmenopausal women with early stage breast cancer. Ann Oncol 2006; 17: 1637–1643.
Harmsen S, Meijerman I, Beijnen JH, Schellens JHM . Nuclear receptor mediated induction of cytochrome P450 3A4 by anticancer drugs: a key role for the pregnane X receptor. Cancer Chemother Pharmacol 2009; 64: 35–43.
Ingle JN, Kalari KR, Buzdar AU, Robson ME, Goetz MP, Desta Z et al. Estrogens and their precursors in postmenopausal women with early breast cancer receiving anastrozole. Steroids 2015; 99 (Pt A): 32–38.
Ingle JN, Schaid DJ, Goss PE, Liu M, Mushiroda T, Chapman JA et al. Genome-wide associations and functional genomic studies of musculoskeletal adverse events in women receiving aromatase inhibitors. J Clin Oncol 2010; 28: 4674–4682.
Henry NL, Skaar TC, Dantzer J, Li L, Kidwell K, Gersch C et al. Genetic associations with toxicity-related discontinuation of aromatase inhibitor therapy for breast cancer. Breast Cancer Res Treat 2013; 138: 807–816.
Fontein DB, Houtsma D, Nortier JW, Baak-Pablo RF, Kranenbarg EM, van der Straaten TR et al. Germline variants in the CYP19A1 gene are related to specific adverse events in aromatase inhibitor users: a substudy of Dutch patients in the TEAM trial. Breast Cancer Res Treat 2014; 144: 599–606.
Colomer R, Monzo M, Tusquets I, Rifa J, Baena JM, Barnadas A et al. A single-nucleotide polymorphism in the aromatase gene is associated with the efficacy of the aromatase inhibitor letrozole in advanced breast carcinoma. Clin Cancer Res 2008; 14: 811–816.
Garcia-Casado Z, Guerrero-Zotano A, Llombart-Cussac A, Calatrava A, Fernandez-Serra A, Ruiz-Simon A et al. A polymorphism at the 3'-UTR region of the aromatase gene defines a subgroup of postmenopausal breast cancer patients with poor response to neoadjuvant letrozole. BMC Cancer 2010; 10: 36.
Ferraldeschi R, Arnedos M, Hadfield KD, A'Hern R, Drury S, Wardley A et al. Polymorphisms of CYP19A1 and response to aromatase inhibitors in metastatic breast cancer patients. Breast Cancer Res Treat 2012; 133: 1191–1198.
Liu L, Bai YX, Zhou JH, Sun XW, Sui H, Zhang WJ et al. A polymorphism at the 3'-UTR region of the aromatase gene is associated with the efficacy of the aromatase inhibitor, anastrozole, in metastatic breast carcinoma. Int J Mol Sci 2013; 14: 18973–18988.
Wang L, Ellsworth KA, Moon I, Pelleymounter LL, Eckloff BW, Martin YN et al. Functional genetic polymorphisms in the aromatase gene CYP19 vary the response of breast cancer patients to neoadjuvant therapy with aromatase inhibitors. Cancer Res 2010; 70: 319–328.
Ramsey LB, Panetta JC, Smith C, Yang W, Fan Y, Winick NJ et al. Genome-wide study of methotrexate clearance replicates SLCO1B1. Blood 2013; 121: 898–904.
Hesselink DA, van Schaik RH, van der Heiden IP, van der Werf M, Gregoor PJ, Lindemans J et al. Genetic polymorphisms of the CYP3A4, CYP3A5, and MDR-1 genes and pharmacokinetics of the calcineurin inhibitors cyclosporine and tacrolimus. Clin Pharmacol Ther 2003; 74: 245–254.
Sun D, Chen G, Dellinger RW, Sharma AK, Lazarus P . Characterization of 17-dihydroexemestane glucuronidation: potential role of the UGT2B17 deletion in exemestane pharmacogenetics. Pharmacogenet Genomics 2010; 20: 575–585.
Acknowledgements
This research was supported by Pharmacogenetics Research Network Grant No. U-01 GM61373 (to DAF) and Clinical Pharmacology Training Grant No. 5T32-GM08425 (to DAF) from the National Institute of General Medical Sciences, National Institutes of Health (NIH), Grant Nos. M01-RR000042 (University of Michigan), M01-RR00750 (Indiana University) and M01-RR00052 (Johns Hopkins University) from the National Center for Research Resources (NCRR), a component of the NIH, the Breast Cancer Research Foundation (BCRF) (N003173 to JMR and DFH), the National Cancer Institute (5T32CA083654), the National Institute of General Medical Sciences (GM099143 to JMR) and the National Institutes of Health through the University of Michigan’s Cancer Center Support Grant (P30 CA046592) by the use of the following Cancer Center Core: University of Michigan DNA Sequencing Core. In addition, these studies were supported by grants from Pfizer (to DFH), Novartis Pharma AG (to DFH) and the Fashion Footwear Association of New York/QVC Presents Shoes on Sale (to DFH). Drugs were supplied by Novartis and Pfizer.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
Dr Stearns has received research funding from Abbvie, Celgene, Merck, Novartis, Medimmune, Pfizer and Puma. NLH had research funding from AstraZeneca, Eli Lilly, BioMarin Pharmaceuticals, Celldex Pharmaceuticals, and Sanofi Aventis. VS had research funding from Abbvie, Abraxis (Celgene), Medimmune, Merck, Novartis, Pfizer, Puma. DFH has consulted for Pfizer and Lilly Oncology, and had research funding from Janssen R&D, Puma Biotechnology, Pfizer, and Astra Zeneca. DFH also has personal financial interest in Oncimmune and Inbiomotion and has royalties from Janssen R&D. DAF had research funding from Pfizer and Novartis and sat on the Scientific Board for Quest Diagnostics. The other authors declare no conflict of interest.
Additional information
This work was presented in part at the 2015 San Antonio Breast Cancer Symposium.
Supplementary Information accompanies the paper on the The Pharmacogenomics Journal website
Supplementary information
PowerPoint slides
Rights and permissions
About this article
Cite this article
Hertz, D., Kidwell, K., Seewald, N. et al. Polymorphisms in drug-metabolizing enzymes and steady-state exemestane concentration in postmenopausal patients with breast cancer. Pharmacogenomics J 17, 521–527 (2017). https://doi.org/10.1038/tpj.2016.60
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/tpj.2016.60
This article is cited by
-
Therapeutic drug monitoring of oral targeted antineoplastic drugs
European Journal of Clinical Pharmacology (2021)
-
Association of CYP gene polymorphisms with breast cancer risk and prognostic factors in the Jordanian population
BMC Medical Genetics (2019)
-
Therapeutic Drug Monitoring of Oral Anti-Hormonal Drugs in Oncology
Clinical Pharmacokinetics (2019)
-
Variable aromatase inhibitor plasma concentrations do not correlate with circulating estrogen concentrations in post-menopausal breast cancer patients
Breast Cancer Research and Treatment (2017)
-
Prospective assessment of patient-reported outcomes and estradiol and drug concentrations in patients experiencing toxicity from adjuvant aromatase inhibitors
Breast Cancer Research and Treatment (2017)