Abstract
Antitumor necrosis factor-α (TNF-α) is used for treatment of severe cases of inflammatory bowel diseases (IBD), including Crohn’s disease (CD) and ulcerative colitis (UC). However, one-third of the patients do not respond to the treatment. Genetic markers may predict individual response to anti-TNF therapy. Using a candidate gene approach, 39 mainly functional single nucleotide polymorphisms (SNPs) in 26 genes regulating inflammation were assessed in 738 prior anti-TNF-naive Danish patients with IBD. The results were analyzed using logistic regression (crude and adjusted for age, gender and smoking status). Nineteen functional polymorphisms that alter the NFκB-mediated inflammatory response (TLR2 (rs3804099, rs11938228, rs1816702, rs4696480), TLR4 (rs5030728, rs1554973), TLR9 (rs187084, rs352139), LY96 (MD-2) (rs11465996), CD14 (rs2569190), MAP3K14 (NIK) (rs7222094)), TNF-α signaling (TNFA (TNF-α) (rs361525), TNFRSF1A (TNFR1) (rs4149570), TNFAIP3(A20) (rs6927172)) and other cytokines regulated by NFκB (IL1B (rs4848306), IL1RN (rs4251961), IL6 (rs10499563), IL17A (rs2275913), IFNG (rs2430561)) were associated with response to anti-TNF therapy among patients with CD, UC or both CD and UC (P⩽0.05). In conclusion, the results suggest that polymorphisms in genes involved in activating NFκB through the Toll-like receptor (TLR) pathways, genes regulating TNF-α signaling and cytokines regulated by NFκB are important predictors for the response to anti-TNF therapy among patients with IBD. Genetically strong TNF-mediated inflammatory response was associated with beneficial response. In addition, the cytokines IL-1β, IL-6 and IFN-γ may be potential targets for treating patients with IBD who do not respond to anti-TNF therapy. These findings should be examined in independent cohorts before these results are applied in a clinical setting.
Similar content being viewed by others
Introduction
Inflammatory bowel diseases (IBD), including Crohn’s disease (CD) and ulcerative colitis (UC), are characterized by a dysregulated inflammatory response.1 The transcription factor NFκB is a central regulator of inflammation and regulates the expression of more than 150 genes including TNFA, TNFAIP3, TLR2, TLR9, CD14, NFKBIA, NFKB1, IL1B, IL1RN, IL6, IL10, IL17A and IFNG.2 NFκB can be activated by Toll-like receptors (TLRs), which recognize molecules that are broadly shared by pathogens but distinguishable from host molecules, such as bacterial or viral DNA, flagellin or lipopolysaccharide (LPS). For example, LPS from Gram-negative bacterial cell membranes can be bound by CD14 in the presence of LPS-binding protein, which together with MD-2 interacts with TLR4. TLR4 is a membrane-bound protein, which on LPS stimuli forms homodimers and activates an intracellular kinase cascade. This kinase cascade ultimately activates the IKK complex, which phosphorylates and degrades the NFκB inhibitor IκBα.3 NFκB is shuttled from the cytosol to the nucleus where it initiates expression of pro- and anti-inflammatory cytokines (Figure 1).
Simplified overview of the NFκB pathway highlighting the genes that were studied. Polymorphisms in genes associated or not associated with response to anti-TNF therapy among patients with IBD are written in white and red, respectively. Genes not studied are written in black. Increased gene/protein activity was associated with beneficial response (green) or nonresponse (purple). The biological effect was unclear (TLR4, TLR9, NIK) or showed opposite direction of effect among patients with CD and UC (MD-2) (blue). A significant association was only seen in CD14 and IL-1RA (inhibitor of IL-1β signaling) among patients with UC. CD, Crohn’s disease; IBD, inflammatory bowel disease; UC, ulcerative colitis.
One of the pro-inflammatory cytokines activated by NFκB is tumor necrosis factor-α (TNF-α), whose feedback stimulates NFκB by binding to TNF receptors (TNFR1 or TNFR2), resulting in a kinase cascade similar to, but distinct from, the canonical pathway induced by TLRs.3
The TNF-α level is increased in the blood, stool and intestinal tissue from patients with CD and UC, and therefore it has been a target for medical treatment.4, 5, 6 Infliximab and adalimumab are therapeutic antibodies that block the binding of TNF-α to its cell-surface receptors and limit downstream cell signaling pathways.7 These antibodies are used for the treatment of severe cases of IBD, but approximately one-third of the patients benefit minimally or not at all from the treatment.8, 9
We wanted to investigate whether there were genetic differences between responders and nonresponders to anti-TNF therapy among patients with IBD. Therefore, we assessed 39 mainly functional polymorphisms in genes involved in inflammation, in particular the NFκB pathway, in a cohort of 738 Danish IBD patients previously naive to anti-TNF therapy. Knowing the biological effect of the studied polymorphisms allows a biological interpretation of the associations in the candidate genes. The genes studied are involved in regulation of the NFκB pathway (TLR2, TLR4, TLR5, TLR9, LY96, CD14, MAP3K14, SUMO4, NFKBIA and NFKB1), TNF-α signaling (TNFA, TNFRSF1A and TNFAIP3), cytokines regulated by NFκB (IL1B, IL1RN, IL6, IL10, IL17A and IFNG) and other genes involved in regulation of inflammation (IL4R, IL6R, IL23R, TGFB1, PTPN22, PPARG and NLRP3).
Materials and methods
Cohort
A prior anti-TNF-naive Danish cohort of patients with IBD was established. Blood samples retrieved as part of the routine screening for latent Mycobacterium tuberculosis at Statens Serum Institut (SSI, Copenhagen, Denmark) and the Department of Respiratory Diseases B, and the Department Clinical Microbiology, Aarhus University Hospital (Aarhus, Denmark) were collected from 01 September 2009 to 30 March 2011 (9217 patients). Patients with intestinal diseases (ICD-10 code K50–K63) were identified by linking the unique personal identification number of Danish citizens (CPR number) from each blood sample with the National Patient Registry (2659 patients). Patient records from 18 medical departments were examined (1378 patients) and identified 738 previously anti-TNF-naive ethnic Danish patients with IBD. Treatment efficacy using the simple three-step scale10, 11, 12 reflected the maximum response within 22 weeks after initiation.
Genotyping
DNA was extracted from cryopreserved blood clots by using the Maxwell 16 Blood purification kit (Promega, Madison WI, USA) according to the manufacturers’ instructions with a median yield of 4.90 μg (range 0.8–25 μg) per 300 μl total blood.13 Competitive Allele-Specific Polymerase chain reaction (KASP), an end-point PCR technology, was used by LGC Genomics for genotyping (LGC Genomics, Hoddesdon, UK) (http://www.lgcgenomics.com/).
The single nucleotide polymorphisms (SNPs) studied were TLR2 (rs4696480, rs1816702, rs11938228, rs3804099), TLR4 (rs12377632, rs5030728, rs1554973), TLR5 (rs5744168), TLR9 (rs187084, rs352139), LY96 (MD-2) (rs11465996), CD14 (rs2569190), MAP3K14 (NIK) (rs7222094), SUMO4 (rs237025), NFKBIA (IκBα) (rs696, rs17103265), NFKB1 (NFκB1) (rs28362491), TNFA (TNF-α) (rs1800629, rs1800630, rs1799724, rs361525), TNFRSF1A (TNFR1) (rs4149570), TNFAIP3 (A20) (rs6927172), IL1B (IL-1β) (rs1143623, rs4848306, rs1143627), IL1RN (IL-1RA) (rs4251961), IL4R (rs1805010), IL6 (rs10499563), IL6R (rs4537545), IL10 (rs1800872, rs3024505), IL17A (rs2275913), IL23R (rs11209026), IFNG (IFN-γ) (rs2430561), TGFB1 (TGF-β1) (rs1800469), PTPN22 (rs2476601), PPARG (PPAR-γ) (rs1801282) and NLRP3 (rs4612666).
Genotyping of TNFA (TNF-α) –857 C>T (rs1799724) and –863 C>A (rs1800630) failed due to their close proximity to each other. All genotyping of –857 C>T (rs1799724) either failed or were erroneously genotyped as homozygous wild type when the patients were carriers of the AA genotype of –863 C>A (rs1800630) due to genotyping bias.
The 39 SNPs were replicated in 94 randomly selected samples and yielded >99% identical genotypes. The studied SNPs had a minor allele frequency of 0.05–0.48.
Linkage disequilibrium was calculated using the Genome-wide LInkage DisEquilibrium Repository and Search Engine (GLIDER) software (http://www.sanger.ac.uk/resources/software/gliders/). Haplotypes were inferred manually.
Ethical considerations
The study was conducted in accordance with the Declaration of Helsinki and was approved by the local regional ethics committees (M20100153 and S-20120113) and the Danish Data Protection Agency (J. 2010-41-4719 and 2008-58-035).
Power analysis
The Genetic Power Calculator was utilized for power analysis of discrete traits.14 The ‘high-risk allele frequency’ was set to 0.05, 0.25 and 0.48, the ‘prevalence’ was set to 0.33, D-prime was set to 1, type I error rate was set to 0.05 and number of cases and control:case ratio was based on Table 1. This cohort study had more than 80% chance of detecting a dominant effect with an odds ratio (OR) of 1.9, 1.5 and 1.6 for CD, 2.1, 1.7 and 1.9 for UC and 1.6, 1.4 and 1.5 for IBD with high-risk allele frequencies of 0.05, 0.25 and 0.48, respectively.
Statistical analysis
Logistic regression, crude and adjusted for age, gender and smoking status, was used to compare genotypes among responders versus nonresponders and responders versus non- and partial responders to anti-TNF therapy (Supplementary Tables 1–3).
A χ2-test or unpaired t-test was used to test for statistically significant difference in response between patients with CD and UC, for difference in secondary parameters between responders and nonresponders (Table 1), and for haplotype analysis (Supplementary Tables 4–7).
To achieve more statistical power, analyses for associations between polymorphisms and treatment response in relation to IBD and for haplotype analyzed were performed with the combined CD and UC data set.
Statistical analyses were performed using STATA version 11 (STATA, College Station, TX, USA).
Results
Study population
The clinical and demographic characteristics of the 482 and 256 prior anti-TNF-naive patients with CD and UC, respectively, are shown in Table 1. More females (17%) than males (9%) were nonresponders among patients with CD (OR: 2.05, 95% CI: 1.16–3.64, P=0.01) and a decrease in CRP level by more than 25% was associated with beneficial response among patients with IBD when only considering CRP⩾20 mg l−1 pretreatment (OR: 2.01, 95% CI: 1.09–3.72, P=0.02). Furthermore, 14% (66 patients) and 24% (62 patients) were nonresponders among patients with CD and UC, respectively (OR: 0.48, 95% CI: 0.33–0.72, P=0.001). Young age at diagnosis was borderline associated with beneficial response (P=0.06).
Polymorphisms associated with response in CD
In a dominant model, the homozygous variant genotype of TNFRSF1A –609G>T (rs4149570) (ORadj: 2.39, 95% CI: 1.03–5.57, P=0.04), the heterozygous genotype of TLR4 G>A (rs5030728) (ORadj: 3.34, 95% CI: 1.32–8.47, P=0.01) and both the homozygous and the heterozygous variant genotypes of TLR2 597T>C (rs3804099) (ORadj: 2.02, 95% CI: 1.17–3.49, P=0.01), TLR2 C>T (rs1816702) (ORadj: 2.02, 95% CI: 1.04–3.95, P=0.04), LY96 (MD-2) –1625 C>G (rs11465996) (ORunadj: 1.73, 95%CI: 1.01–2.95, P=0.04) and IFNG 874T>A (rs2430561) (ORadj: 1.97, 95% CI: 1.13–3.42, P=0.02) were associated with beneficial response among patients with CD (Supplementary Table 1).
In a recessive model, the homozygous variant genotypes of TLR4 G>A (rs5030728) (ORadj: 0.38, 95% CI: 0.15–0.96, P=0.04) and TLR9 1174G>A (rs352139) (ORadj: 0.38, 95% CI: 0.16–0.94, P=0.04) were associated with nonresponse and the homozygous variant genotype of TNFRSF1A –609G>T (rs4149570) (ORadj: 5.16, 95% CI: 1.14–23.39, P=0.03) was associated with beneficial response among patients with CD (Supplementary Table 1).
The variant allele of the polymorphisms has been shown to decrease TNF-α, IL-1β and IL-6 levels (TLR2 597T>C (rs3804099)), increase TLR2 (TLR2 C>T (rs1816702)), MD-2 and TNF-α levels (LY96 –1625 C>G (rs11465996)), increase TNFRSF1A expression (TNFRSF1A –609G>T (rs4149570)) and decrease IFN-γ level (IFNG 874T>A (rs2430561)) (Table 2).
The biological effect of the polymorphism TLR4 G>A (rs5030728) and TLR9 1174G>A (rs352139) was unknown.
Thus, genetically determined increased TLR2 level (rs1816702), MD-2 level (rs11465996), TNFRSF1A (TNFR1) expression (rs4149570) and genetically determined decreased IL-1β (rs3804099), IL-6 (rs3804099) and IFN-γ (rs2430561) levels were associated with beneficial response among patients with CD. The genetically determined effect of TNF-α was inconclusive among patients with CD, as one polymorphism indicated that genetically determined increased TNF-α level (rs11465996) and another polymorphism indicated that decreased TNF-α level (along with decreased IL-1β and IL-6 levels) (rs3804099) were associated with beneficial response.
Polymorphisms associated with response in UC
In a dominant model, the homozygous variant genotype of TLR4 G>A (rs5030728) (ORunadj: 2.89, 95% CI: 1.17–7.12, P=0.02) and both the homozygous and the heterozygous variant genotypes of IL1B –3737G>A (rs4848306) (ORadj: 2.69, 95% CI: 1.04–6.94, P=0.04) and IL6 –6331T>C (rs10499563) (ORadj: 3.60, 95% CI: 1.39–9.29, P=0.01) were associated with beneficial response among patients with UC. The homozygous variant genotype of TLR2 A>T (rs4696480) (ORunadj: 0.47, 95% CI: 0.23–0.95, P=0.04) and both the homozygous and the heterozygous variant genotypes of TLR2 C>A (rs11938228) (ORunadj: 0.49, 95% CI: 0.26–0.90, P=0.02), LY96 (MD-2) –1625 C>G (rs11465996) (ORadj: 0.32, 95% CI: 0.14–0.75, P=0.01), CD14 –159G>A (rs2569190) (ORunadj: 0.54, 95% CI: 0.30–0.98, P=0.04), TNFAIP3 (A20) C>G (rs6927172) (ORadj: 0.34, 95% CI: 0.13–0.90, P=0.03), IL1RN T>C (rs4251961) (ORadj: 0.42, 95% CI: 0.18–0.98, P=0.04) and IL17A 197G>A (rs2275913) (ORadj: 0.42, 95% CI: 0.18–1.00, P=0.05) were associated with nonresponse (Supplementary Table 2).
In a recessive model, the homozygous variant genotype of TLR2 597T>C (rs3804099) (ORunadj: 2.47, 95% CI: 0.98–6.23, P=0.05) and the homozygous variant genotype of TLR4 G>A (rs5030728) (ORunadj: 2.59, 95% CI: 1.08–6.18, P=0.03) were associated with beneficial response among patients with UC. The homozygous variant genotype of TLR2 C>A (rs11938228) (ORadj: 0.26, 95% CI: 0.08–0.92, P=0.04) and the homozygous variant genotype of TLR2 A>T (rs4696480) (ORadj: 0.29, 95% CI: 0.12–0.70, P=0.01) were associated with nonresponse (Supplementary Table 2).
The variant allele of the polymorphisms has been shown to decrease TNF-α, IL-1β and IL-6 levels (TLR2 597T>C (rs3804099)), increase MD-2 and TNF-α levels (LY96 –1625 C>G (rs11465996)), CD14 level (CD14 –159G>A (rs2569190)), increase TNFAIP3 expression (TNFAIP3 C>G (rs6927172)), decrease IL1B transcription (IL1B –3737G>A (rs4848306)), decrease IL-1RA level (IL1RN T>C (rs4251961)), decrease IL6 expression (IL6 –6331T>C (rs10499563)) and increase IL17A expression (IL17A 197G>A (rs2275913)) (Table 2). The biological effect of the polymorphisms TLR2 A>T (rs4696480), TLR2 C>A (rs11938228) and TLR4 G>A (rs5030728) was unknown.
Thus, genetically determined increased MD-2 level (rs11465996), CD14 level (rs11465996), TNF-α level (rs11465996), TNFAIP3 (A20) expression (rs6927172) and IL-17 expression (rs2275913) were associated with nonresponse and genetically determined decreased IL1B (rs4848306 and rs3804099) and IL6 expressions (rs10499563 and rs3804099) were associated with beneficial response among patients with UC. One polymorphism indicated that decreased TNF-α level (along with decreased IL-1β and IL-6 levels) (rs3804099) was associated with beneficial response. Finally, genetically determined decreased IL-1RA level (rs4251961) was associated with nonresponse.
Polymorphisms associated with response in CD and UC combined (IBD)
The polymorphisms generally showed the same direction of effect in both diseases, except for the polymorphisms in LY96 (rs11465996) (Supplementary Tables 1 and 2).
In a dominant model, the homozygous variant genotype of TNFRSF1A –609G>T (rs4149570) (ORadj: 2.07, 95% CI: 1.03–4.15, P=0.04), the heterozygous genotypes of TLR9 –1486T>C (rs187084) (ORadj: 1.99, 95% CI: 1.04–3.82, P=0.04) and MAP3K14 T>C (rs7222094) (ORadj: 1.92, 95% CI: 1.00–3.68, P=0.05) and both the homozygous and the heterozygous variant genotypes of TLR2 597T>C (rs3804099) (ORadj: 1.80, 95% CI: 1.15–2.81, P=0.01), TLR4 G>A (rs5030728) (ORunadj: 1.45, 95% CI: 1.06–2.00, P=0.02), LY96 (MD-2) –1625 C>G (rs11465996) (ORunadj: 1.48, 95% CI: 1.00–2.19, P=0.05), IL1B –3737G>A (rs4848306) (ORadj: 1.85, 95% CI: 1.05–3.27, P=0.03), IL6 –6331T>C (rs10499563) (ORadj: 2.26, 95% CI: 1.18–4.32, P=0.01) and IFNG 874T>A (rs2430561) (ORadj: 1.66, 95% CI: 1.05–2.62, P=0.03) were associated with beneficial response among patients with IBD. The heterozygous genotype of TNFA –238G>A (rs361525) (ORadj: 0.43, 95% CI: 0.19–0.97, P=0.04) and both the homozygous and the heterozygous variant genotypes of TLR2 C>A (rs11938228) (ORadj: 0.63, 95% CI: 0.41–0.98, P=0.04), TLR4 T>C (rs1554973) (ORunadj: 0.72, 95% CI: 0.52–0.99, P=0.04) and TNFAIP3 (A20) C>G (rs6927172) (ORadj: 0.62, 95% CI: 0.42–0.92, P=0.02) were associated with nonresponse (Supplementary Table 3).
In a recessive model, the homozygous variant genotype of TLR2 597T>C (rs3804099) (ORadj: 2.52, 95% CI: 1.08–5.87, P=0.03) and the homozygous variant genotype of TNFRSF1A –609G>T (rs4149570) (ORadj: 2.65, 95% CI: 1.00–6.97, P=0.05) were associated with beneficial response. The homozygous variant genotype of TLR9 1174G>A (rs352139) (ORadj: 0.48, 95% CI: 0.24–0.96, P=0.04) and the homozygous variant genotype of IL17A 197G>A (rs2275913) (ORadj: 0.47, 95% CI: 0.21–1.01, P=0.05) were associated with nonresponse (Supplementary Table 3).
The variant allele of the polymorphisms has been shown to decrease TNF-α, IL-1β and IL-6 levels (TLR2 597T>C (rs3804099)), increase MD-2 and TNF-α levels (LY96 –1625 C>G (rs11465996)), decrease TNFA expression (TNFA –238G>A (rs361525)), increase TNFRSF1A (TNFRSF1A –609G>T (rs4149570)), TNFAIP3 expressions (TNFAIP3 C>G (rs6927172)), decrease IL1B transcription (IL1B –3737G>A (rs4848306)), decrease IL6 expression (IL6 –6331T>C (rs10499563)), increase IL17A expression (IL17A 197G>A (rs2275913)) and decrease IFN-γ level (IFNG 874T>A (rs2430561)) (Table 2). The polymorphisms –1486T>C (rs187084) and 1174G>A (rs352139) in TLR9 have only been shown to have a biological effect in a haplotype context and the biological effect of the heterozygous variant of MAP3K14 T>C (rs7222094) was unknown. The biological effect of the polymorphisms TLR2 C>A (rs11938228), TLR4 G>A (rs5030728) and TLR4 T>C (rs1554973) was unknown.
Thus, genetically determined increased MD-2 level (rs11465996) and TNFRSF1A (TNFR1) expression (rs4149570) and genetically determined decreased TNFAIP3 (A20) expression (rs6927172), IL-1β (rs3804099 and rs4848306), IL-6 (rs3804099 and rs10499563), IL-17 (rs2275913) and IFN-γ (rs2430561) levels were associated with beneficial response among patients with IBD. Again, the effect of TNF-α was less clear, as two polymorphisms indicated that genetically determined increased TNF-α level (rs11465996 and rs361525) and one polymorphism indicated that decreased TNF-α level (rs3804099) (along with decreased IL-1β and IL-6 levels) were associated with beneficial response.
Haplotype analysis
Haplotype analysis of TLR2, TLR4, TLR9 and IL1B among patients with IBD is shown in Supplementary Tables 4–7, respectively. Rs11938228 and rs3804099 in TLR2 were in linkage disequilibrium with r2=0.34 and D'=1.00. In TLR9, the linkage disequilibrium for rs187084 and rs352139 was r2=0.55 and D'=1.00.
Four haplotypes in TLR2, three in TLR4 and IL1B and two in TLR9 described 85, 95, 99 and 97% of the genotypes observed, respectively. The TLR2 haplotype 22 (rs4696480TT, rs1816702CC, rs11938228AA and rs3804099TT) (OR: 0.41, 95% CI: 0.19–0.86, P=0.02) and the haplotype 12 (rs4696480TA, rs1816702CC, rs11938228CA and rs3804099CT) (OR: 0.48, 95% CI: 0.24–0.95, P=0.04) were associated with nonresponse. Haplotype combination 33 was also associated with nonresponse, although not statistically significant. Both haplotypes 2 and 3 encompass the wild-type allele of rs3804099, and thus the haplotype analysis supports the found association between the variant allele of rs3804099 and beneficial response. No associations were found for TLR4,TLR9 or IL1B.
Discussion
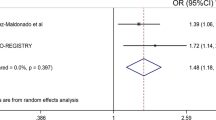
In the inflammatory pathways, 37 SNPs in 26 genes were successfully genotyped and 19 of the functional polymorphisms in 14 genes were associated with response to anti-TNF therapy among patients with CD, UC, or CD and UC combined (IBD) as shown in Figure 2.
Polymorphisms associated with response to anti-TNF. Thirty-seven functional single nucleotide polymorphisms (SNPs) in 26 genes were successfully genotyped and 19 SNPs in 14 genes were associated with response to antitumor necrosis factor-α (TNF-α) therapy among patients with Crohn’s disease (CD), ulcerative colitis (UC) or CD and UC combined. The 19 SNPs associated with response were in genes involved in regulation of NFκB through the Toll-like receptor (TLR) pathways (TLR2, TLR4, TLR9, LY96 (MD-2), CD14 and MAP3K14 (NIK)), TNF-α signaling (TNFA (TNF-α), TNFRSF1A (TNFR1) and TNFAIP3 (A20)) or cytokines regulated by NFκB (IL1B, IL1RN, IL6, IL17A and IFNG).
As illustrated in Figure 1, genetically determined increased levels of TLR2 (rs1816702) and MD-2 (LY96) (rs11465996) (required for TLR2 and TLR4 to respond to LPS)15, 16 were associated with beneficial response among patients with CD, indicating that a higher activity of TLR2 was associated with a beneficial response among patients with CD. Among patients with UC, genetically determined increased levels of MD-2 (LY96) (rs11465996) and CD14 (rs2569190)15, 17, 18 were associated with nonresponse, indicating that a high activity of TLR4 was associated with nonresponse among patients with UC. In addition, two SNPs in TLR2 (rs4696480 and rs11938228) and two SNPs in TLR4 (rs5030728 and rs1554973) with unknown biological effects were associated with response among patients with CD, UC or IBD as shown in Table 2. The TLR9 heterozygous genotype of –1486T>C (rs187084) and the homozygous variant genotype of TLR9 1174G>A (rs352139) were associated with beneficial response and nonresponse among patients with IBD, respectively. The 1486T>C and 1174G>A polymorphisms in TLR9 have only been shown to have a biological effect in haplotype context,19, 20 however, the haplotype analysis of TLR9 did not reveal any associations. Thus, the results indicate that TLR activity is important in determining response to anti-TNF therapy among patients with IBD.
Regarding the canonical and noncanonical NFκB pathway, functional polymorphisms in SUMO4, NFKBIA (IκBα) and NFKB1 (p50-RelA) were not found to be associated with response. However, the heterozygous genotype of rs7222094 T>C in MAP3K14 (NIK) was associated with beneficial response among patients with IBD. The biological effect of the heterozygous genotype is unknown,21 which makes it difficult to interpret the association in MAP3K14 from a biological perspective. Further studies of the noncanonical NFκB pathway, for example, by studying functional polymorphisms in LTA or TNFSF11 (RANKL),22, 23, 24 could shed more light on any possible involvement of this pathway in anti-TNF therapy response.
The TNF-α signaling pathway showed that a genetically determined decreased expression of TNFA (TNF-α) (rs361525)25 was associated with nonresponse among patients with IBD. Furthermore, a genetically determined increased expression of the TNF receptor 1 (TNFRSF1A) (rs4149570)26 was associated with beneficial response among patients with CD and IBD. In addition, a genetically determined increased expression of TNFAIP3 (A20) (rs6927172)27 was associated with nonresponse among patients with IBD. A20, encoded by TNFAIP3, is known to inhibit NFκB activation as well as TNF-α-mediated apoptosis.
Thus, the results indicate that polymorphisms in TNFA (TNF-α), TNFRSF1A (TNFR1) and TNFAIP3 (A20), which upregulate TNF-α signaling, were associated with beneficial response to anti-TNF therapy among patients with IBD.
Among cytokines regulated by NFκB, a genetically determined decreased expression of IL1B (rs4848306), IL6 (rs10499563) and IFNG (rs2430561)28, 29, 30 were associated with beneficial response among patients with CD, UC and IBD. Furthermore, a polymorphism in IL1B (rs1143627), which has been shown to increase IL-1β level,31, 32 was borderline significantly associated with nonresponse among patients with IBD. In addition, a genetically determined decreased IL-1 receptor antagonist (IL-1RA) level (rs4251961)33 was associated with nonresponse among patients with UC. IL-1RA binds to the IL-1 receptor and inhibits IL-1β signaling.3 The IL-6 receptor is not regulated by NFκB and no association was found with the SNP studied in IL6R.34
This could indicate that among patients with IBD, nonresponders to anti-TNF therapy are more likely to have an inflammatory response mediated by other early pro-inflammatory cytokines than TNF-α, such as IL-1β, IL-6 and IFN-γ. This suggests that drugs targeting IFN-γ, IL-1β or IL-6 could potentially be useful for treating patients who do not respond to anti-TNF therapy. This interpretation is supported by the polymorphism in IL1RN, where a genetically determined high inhibition of IL-1β signaling (high IL-1RA level) was associated with beneficial response. Furthermore, this interpretation is also supported by another study that has reported an association between the C-allele of rs1143634 in IL1B and higher serum IL-1β level and a lower response rate to infliximab therapy among patients with CD.35
The variant allele of the 597T>C polymorphism in TLR2 (rs3804099) was associated with beneficial response among patients with CD, UC and IBD. The polymorphism has been shown to decrease TNF-α level by ∼50%, IL-1β level by 75% and IL-6 level by 150%.36 In the light of the other results, we expected an increased TNF-α level to be associated with beneficial response and an increased IL-1β and IL-6 levels to be associated with nonresponse. This indicates that the relative levels of the cytokines TNF-α, IL-1β and IL-6 are important in determining response to anti-TNF.
The variant allele of the 197G>A polymorphism in IL17A was associated with nonresponse among patients with UC and IBD. The polymorphism has been shown to increase expression of IL-17,37 indicating that high level of this cytokine may also be associated with nonresponse.
The functional SNPs studied in IL4R, IL10, IL23R, TGFB1, PTPN22, PPARG and NLRP3 were not associated with response to anti-TNF therapy.
Overall, the results indicate that patients with genetically determined high TNF-driven inflammatory response benefit the most from anti-TNF therapy. Conversely, patients with genetically determined IL1B, IL6 and IFNG-driven inflammatory response seem to benefit the least from anti-TNF therapy. These patients might benefit from biological drugs targeting other cytokines such as IL-1β, IL-6 or IFN-γ or from a cocktail of several antibodies.
The results in this exploratory study should be interpreted with care. Additional confirmation of these findings in independent cohorts should be performed before our results are applied in the clinic. In the light of the obtained P-values and the number of statistical tests performed, we cannot exclude that some of our positive findings may be due to chance. We successfully genotyped 37 polymorphisms. Of these, two polymorphisms would be expected to be associated with treatment outcome by pure chance assuming a 5% acceptance level. We found numerous associated polymorphisms. Furthermore, most of the found associations were biologically plausible. The study generally did not have enough power to detect a recessive effect and the associations were predominantly found to show gene-dose effects. We cannot exclude that associations were not identified due to insufficient statistical power. On the other hand, this study is rather large including 738 IBD patients treated with anti-TNF, giving the cohort study >80% power to detect an OR of 1.6 assuming a minor allele frequency of 0.05. In addition, blood and clinical data from these patients were collected at 18 large gastroenterological centers at basic and specialized hospitals in Denmark. Thus, the patients are representative of Danish patients with severe IBD.
In conclusion, the results suggest that genes involved in the regulation of NFκB through the TLR pathways, genes regulating TNF-α signaling and cytokines regulated by NFκB are important predictors for the response to anti-TNF therapy among patients with IBD. Genetically strong TNF-mediated inflammatory response was associated with beneficial response to anti-TNF therapy. In addition, patients with genetically determined high IL-1β, IL-6 or IFN-γ levels were less likely to respond, perhaps because the colonic inflammation was primarily driven by these pro-inflammatory cytokines. This could indicate that the cytokines IL-1β, IL-6 and IFN-γ may be potential targets for treating patients with IBD who do not respond to anti-TNF therapy. Before the genetic markers found in this study are applied in a clinical setting, they should be confirmed in independent cohorts.
References
Podolsky DK . Inflammatory bowel disease. N Engl J Med 2002; 347: 417–429.
Verstrepen L, Bekaert T, Chau TL, Tavernier J, Chariot A, Beyaert R . TLR-4, IL-1R and TNF-R signaling to NF-kappaB: variations on a common theme. Cell Mol Life Sci 2008; 65: 2964–2978.
Komatsu M, Kobayashi D, Saito K, Furuya D, Yagihashi A, Araake H et al. Tumor necrosis factor-alpha in serum of patients with inflammatory bowel disease as measured by a highly sensitive immuno-PCR. Clin Chem 2001; 47: 1297–1301.
Dionne S, Hiscott J, D'Agata I, Duhaime A, Seidman EG . Quantitative PCR analysis of TNF-alpha and IL-1 beta mRNA levels in pediatric IBD mucosal biopsies. Dig Dis Sci 1997; 42: 1557–1566.
Meena NK, Verma R, Verma N, Ahuja V, Paul J . TLR4 D299G polymorphism modulates cytokine expression in ulcerative colitis. J Clin Gastroenterol 2013; 47: 773–780.
Knight DM, Trinh H, Le J, Siegel S, Shealy D, McDonough M et al. Construction and initial characterization of a mouse-human chimeric anti-TNF antibody. Mol Immunol 1993; 30: 1443–1453.
Rutgeerts P, Sandborn WJ, Feagan BG, Reinisch W, Olson A, Johanns J et al. Infliximab for induction and maintenance therapy for ulcerative colitis. N Engl J Med 2005; 353: 2462–2476.
Mascheretti S, Hampe J, Kuhbacher T, Herfarth H, Krawczak M, Folsch UR et al. Pharmacogenetic investigation of the TNF/TNF-receptor system in patients with chronic active Crohn's disease treated with infliximab. Pharmacogenomics J 2002; 2: 127–136.
Ljung T, Karlen P, Schmidt D, Hellstrom PM, Lapidus A, Janczewska I et al. Infliximab in inflammatory bowel disease: clinical outcome in a population based cohort from Stockholm County. Gut 2004; 53: 849–853.
Caspersen S, Elkjaer M, Riis L, Pedersen N, Mortensen C, Jess T et al. Infliximab for inflammatory bowel disease in Denmark 1999-2005: clinical outcome and follow-up evaluation of malignancy and mortality. Clin Gastroenterol Hepatol 2008; 6: 1212–1217.
Cohen RD, Tsang JF, Hanauer SB . Infliximab in Crohn's disease: first anniversary clinical experience. Am J Gastroenterol 2000; 95: 3469–3477.
Bank S, Nexo BA, Andersen V, Vogel U, Andersen PS . High-quality and -quantity DNA extraction from frozen archival blood clots for genotyping of single-nucleotide polymorphisms. Genet Test Mol Biomarkers 2013; 17: 501–503.
Gu W, Shan YA, Zhou J, Jiang DP, Zhang L, Du DY et al. Functional significance of gene polymorphisms in the promoter of myeloid differentiation-2. Ann Surg 2007; 246: 151–158.
Bielinski SJ, Hall JL, Pankow JS, Boerwinkle E, Matijevic-Aleksic N, He M et al. Genetic variants in TLR2 and TLR4 are associated with markers of monocyte activation: the Atherosclerosis Risk in Communities MRI Study. Hum Genet 2011; 129: 655–662.
Baldini M, Lohman IC, Halonen M, Erickson RP, Holt PG, Martinez FD . A Polymorphism* in the 5' flanking region of the CD14 gene is associated with circulating soluble CD14 levels and with total serum immunoglobulin E. Am J Respir Cell Mol Biol 1999; 20: 976–983.
Mertens J, Bregadze R, Mansur A, Askar E, Bickeboller H, Ramadori G et al. Functional impact of endotoxin receptor CD14 polymorphisms on transcriptional activity. J Mol Med (Berl) 2009; 87: 815–824.
Tao K, Fujii M, Tsukumo S, Maekawa Y, Kishihara K, Kimoto Y et al. Genetic variations of Toll-like receptor 9 predispose to systemic lupus erythematosus in Japanese population. Ann Rheum Dis 2007; 66: 905–909.
Omar AH, Yasunami M, Yamazaki A, Shibata H, Ofori MF, Akanmori BD et al. Toll-like receptor 9 (TLR9) polymorphism associated with symptomatic malaria: a cohort study. Malar J 2012; 11: 168.
Thair SA, Walley KR, Nakada TA, McConechy MK, Boyd JH, Wellman H et al. A single nucleotide polymorphism in NF-kappaB inducing kinase is associated with mortality in septic shock. J Immunol 2011; 186: 2321–2328.
Knight JC, Keating BJ, Kwiatkowski DP . Allele-specific repression of lymphotoxin-alpha by activated B cell factor-1. Nat Genet 2004; 36: 394–399.
Migita O, Noguchi E, Koga M, Jian Z, Shibasaki M, Migita T et al. Haplotype analysis of a 100 kb region spanning TNF-LTA identifies a polymorphism in the LTA promoter region that is associated with atopic asthma susceptibility in Japan. Clin Exp Allergy 2005; 35: 790–796.
Tan W, Wu H, Zhao J, Derber LA, Lee DM, Shadick NA et al. A functional RANKL polymorphism associated with younger age at onset of rheumatoid arthritis. Arthritis Rheum 2010; 62: 2864–2875.
Kaluza W, Reuss E, Grossmann S, Hug R, Schopf RE, Galle PR et al. Different transcriptional activity and in vitro TNF-alpha production in psoriasis patients carrying the TNF-alpha 238A promoter polymorphism. J Invest Dermatol 2000; 114: 1180–1183.
Chen H, Wilkins LM, Aziz N, Cannings C, Wyllie DH, Bingle C et al. Single nucleotide polymorphisms in the human interleukin-1B gene affect transcription according to haplotype context. Hum Mol Genet 2006; 15: 519–529.
Elsby LM, Orozco G, Denton J, Worthington J, Ray DW, Donn RP . Functional evaluation of TNFAIP3 (A20) in rheumatoid arthritis. Clin Exp Rheumatol 2010; 28: 708–714.
Pravica V, Perrey C, Stevens A, Lee JH, Hutchinson IV . A single nucleotide polymorphism in the first intron of the human IFN-gamma gene: absolute correlation with a polymorphic CA microsatellite marker of high IFN-gamma production. Hum Immunol 2000; 61: 863–866.
Yoshida M, Shiroiwa K, Mouri K, Ishiguro H, Supriyanto I, Ratta-Apha W et al. Haplotypes in the expression quantitative trait locus of interleukin-1beta gene are associated with schizophrenia. Schizophr Res 2012; 140: 185–191.
Smith AJ, D'Aiuto F, Palmen J, Cooper JA, Samuel J, Thompson S et al. Association of serum interleukin-6 concentration with a functional IL6 -6331T>C polymorphism. Clin Chem 2008; 54: 841–850.
Lind H, Haugen A, Zienolddiny S . Differential binding of proteins to the IL1B -31 T/C polymorphism in lung epithelial cells. Cytokine 2007; 38: 43–48.
Wen AQ, Gu W, Wang J, Feng K, Qin L, Ying C et al. Clinical relevance of IL-1beta promoter polymorphisms (-1470, -511, and -31) in patients with major trauma. Shock 2010; 33: 576–582.
Rafiq S, Stevens K, Hurst AJ, Murray A, Henley W, Weedon MN et al. Common genetic variation in the gene encoding interleukin-1-receptor antagonist (IL-1RA) is associated with altered circulating IL-1RA levels. Genes Immun 2007; 8: 344–351.
Rafiq S, Frayling TM, Murray A, Hurst A, Stevens K, Weedon MN et al. A common variant of the interleukin 6 receptor (IL-6r) gene increases IL-6r and IL-6 levels, without other inflammatory effects. Genes Immun 2007; 8: 552–559.
Lacruz-Guzman D, Torres-Moreno D, Pedrero F, Romero-Cara P, Garcia-Tercero I, Trujillo-Santos J et al. Influence of polymorphisms and TNF and IL1beta serum concentration on the infliximab response in Crohn's disease and ulcerative colitis. Eur J Clin Pharmacol 2013; 69: 431–438.
Zhang F, Gao XD, Wu WW, Gao Y, Zhang YW, Wang SP . Polymorphisms in toll-like receptors 2, 4 and 5 are associated with Legionella pneumophila infection. Infection 2013; 41: 941–948.
Espinoza JL, Takami A, Nakata K, Onizuka M, Kawase T, Akiyama H et al. A genetic variant in the IL-17 promoter is functionally associated with acute graft-versus-host disease after unrelated bone marrow transplantation. PLoS One 2011; 6: e26229.
Gast A, Bermejo JL, Claus R, Brandt A, Weires M, Weber A et al. Association of inherited variation in Toll-like receptor genes with malignant melanoma susceptibility and survival. PLoS One 2011; 6: e24370.
Hawn TR, Verbon A, Lettinga KD, Zhao LP, Li SS, Laws RJ et al. A common dominant TLR5 stop codon polymorphism abolishes flagellin signaling and is associated with susceptibility to legionnaires' disease. J Exp Med 2003; 198: 1563–1572.
Guo D, Li M, Zhang Y, Yang P, Eckenrode S, Hopkins D et al. A functional variant of SUMO4, a new I kappa B alpha modifier, is associated with type 1 diabetes. Nat Genet 2004; 36: 837–841.
Song S, Chen D, Lu J, Liao J, Luo Y, Yang Z et al. NFkappaB1 and NFkappaBIA polymorphisms are associated with increased risk for sporadic colorectal cancer in a southern Chinese population. PLoS One 2011; 6: e21726.
Wang S, Zhang M, Zeng Z, Tian L, Wu K, Chu J et al. IkappaBalpha polymorphisms were associated with increased risk of gastric cancer in a southern Chinese population: a case-control study. Life Sci 2011; 88: 792–797.
Park JY, Farrance IK, Fenty NM, Hagberg JM, Roth SM, Mosser DM et al. NFKB1 promoter variation implicates shear-induced NOS3 gene expression and endothelial function in prehypertensives and stage I hypertensives. Am J Physiol Heart Circ Physiol 2007; 293: H2320–H2327.
Udalova IA, Richardson A, Denys A, Smith C, Ackerman H, Foxwell B et al. Functional consequences of a polymorphism affecting NF-kappaB p50-p50 binding to the TNF promoter region. Mol Cell Biol 2000; 20: 9113–9119.
Lv K, Chen R, Cai Q, Fang M, Sun S . Effects of a single nucleotide polymorphism on the expression of human tumor necrosis factor-alpha. Scand J Immunol 2006; 64: 164–169.
Karimi M, Goldie LC, Cruickshank MN, Moses EK, Abraham LJ . A critical assessment of the factors affecting reporter gene assays for promoter SNP function: a reassessment of -308 TNF polymorphism function using a novel integrated reporter system. Eur J Hum Genet 2009; 17: 1454–1462.
Wang GB, Li CR, Yang J, Wen PQ, Jia SL . A regulatory polymorphism in promoter region of TNFR1 gene is associated with Kawasaki disease in Chinese individuals. Hum Immunol 2011; 72: 451–457.
Carrol ED, Payton A, Payne D, Miyajima F, Chaponda M, Mankhambo LA et al. The IL1RN promoter rs4251961 correlates with IL-1 receptor antagonist concentrations in human infection and is differentially regulated by GATA-1. J Immunol 2011; 186: 2329–2335.
Wallis SK, Cooney LA, Endres JL, Lee MJ, Ryu J, Somers EC et al. A polymorphism in the interleukin-4 receptor affects the ability of interleukin-4 to regulate Th17 cells: a possible immunoregulatory mechanism for genetic control of the severity of rheumatoid arthritis. Arthritis Res Ther 2011; 13: R15.
Rees LE, Wood NA, Gillespie KM, Lai KN, Gaston K, Mathieson PW . The interleukin-10-1082 G/A polymorphism: allele frequency in different populations and functional significance. Cell Mol Life Sci 2002; 59: 560–569.
Andersen V, Ernst A, Christensen J, Ostergaard M, Jacobsen BA, Tjonneland A et al. The polymorphism rs3024505 proximal to IL-10 is associated with risk of ulcerative colitis and Crohns disease in a Danish case-control study. BMC Med Genet 2010; 11: 82.
Oosting M, ter HH, van de Veerdonk FL, Sturm P, Kullberg BJ, van der Meer JW et al. Role of interleukin-23 (IL-23) receptor signaling for IL-17 responses in human Lyme disease. Infect Immun 2011; 79: 4681–4687.
Shah R, Hurley CK, Posch PE . A molecular mechanism for the differential regulation of TGF-beta1 expression due to the common SNP -509C-T (c. -1347C > T). Hum Genet 2006; 120: 461–469.
Kariuki SN, Crow MK, Niewold TB . The PTPN22 C1858T polymorphism is associated with skewing of cytokine profiles toward high interferon-alpha activity and low tumor necrosis factor alpha levels in patients with lupus. Arthritis Rheum 2008; 58: 2818–2823.
Aoyagi Y, Nagata S, Kudo T, Fujii T, Wada M, Chiba Y et al. Peroxisome proliferator-activated receptor gamma 2 mutation may cause a subset of ulcerative colitis. Pediatr Int 2010; 52: 729–734.
Hitomi Y, Ebisawa M, Tomikawa M, Imai T, Komata T, Hirota T et al. Associations of functional NLRP3 polymorphisms with susceptibility to food-induced anaphylaxis and aspirin-induced asthma. J Allergy Clin Immunol 2009; 124: 779–785.
Acknowledgements
The work was funded by Health Research Fund of Central Denmark Region, Colitis-Crohn Foreningen and University of Aarhus (PhD grant).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Additional information
Supplementary Information accompanies the paper on the The Pharmacogenomics Journal website
PowerPoint slides
Rights and permissions
This work is licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 3.0 Unported License. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in the credit line; if the material is not included under the Creative Commons license, users will need to obtain permission from the license holder to reproduce the material. To view a copy of this license, visit http://creativecommons.org/licenses/by-nc-sa/3.0/
About this article
Cite this article
Bank, S., Andersen, P., Burisch, J. et al. Associations between functional polymorphisms in the NFκB signaling pathway and response to anti-TNF treatment in Danish patients with inflammatory bowel disease. Pharmacogenomics J 14, 526–534 (2014). https://doi.org/10.1038/tpj.2014.19
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/tpj.2014.19
This article is cited by
-
Inflammation suppresses DLG2 expression decreasing inflammasome formation
Journal of Cancer Research and Clinical Oncology (2022)
-
Tumor necrosis factor induced protein 3 gene polymorphism and the susceptibility to chronic primary immune thrombocytopenia in Egyptian children: a case-control study
Egyptian Journal of Medical Human Genetics (2021)
-
Association of TLR 9 gene polymorphisms with remission in patients with rheumatoid arthritis receiving TNF-α inhibitors and development of machine learning models
Scientific Reports (2021)
-
Genetic variation in toll like receptors 2, 7, 9 and interleukin-6 is associated with cytomegalovirus infection in late pregnancy
BMC Medical Genetics (2020)
-
TLR4 896A/G and TLR9 1174G/A polymorphisms are associated with the risk of infectious mononucleosis
Scientific Reports (2020)