Abstract
The number of publications investigating heart rate variability (HRV) in psychiatry and the behavioral sciences has increased markedly in the last decade. In addition to the significant debates surrounding ideal methods to collect and interpret measures of HRV, standardized reporting of methodology in this field is lacking. Commonly cited recommendations were designed well before recent calls to improve research communication and reproducibility across disciplines. In an effort to standardize reporting, we propose the Guidelines for Reporting Articles on Psychiatry and Heart rate variability (GRAPH), a checklist with four domains: participant selection, interbeat interval collection, data preparation and HRV calculation. This paper provides an overview of these four domains and why their standardized reporting is necessary to suitably evaluate HRV research in psychiatry and related disciplines. Adherence to these communication guidelines will help expedite the translation of HRV research into a potential psychiatric biomarker by improving interpretation, reproducibility and future meta-analyses.
Similar content being viewed by others
Heart rate variability research in psychiatry
Heart rate variability (HRV) is the complex modification of the heart rate by the coordination of autonomic, respiratory, circulatory, endocrine and mechanical influences over time. Originally popularized as a research tool to detect fetal distress,1 and later to predict risk of mortality post-myocardial infarction using 24-h Holter recordings,2, 3, 4, 5 quantification of HRV has recently been more widely adopted to approximate autonomic control of the heart rate in the short term.6, 7, 8 The use of HRV as a transdiagnostic marker has a long research tradition in psychiatry9 that dovetails the recent push to establish neurobiological markers of psychiatric illness for improved nosology.10 Meta-analyses have established that individuals with a range of psychiatric disorders have reduced HRV, with the greatest reductions observed in psychotic disorders11, 12, 13, 14 (but see Stein et al.15 for situations where higher HRV is not necessarily better). The increased incidence of cardiovascular disease in psychiatric illnesses compared with healthy controls16, 17, 18 has also contributed to the increasing interest to better understand autonomic nervous system function in psychiatric illnesses. HRV has also been shown to covary with a range of psychological phenomena that are impaired in psychiatric illnesses such as social cognition19, 20 and executive function.21, 22 HRV is a central component of two prominent biobehavioral frameworks: the neurovisceral integration model, which highlights an inhibitory cortico-subcortical neural circuit to respond to environmental challenges23 and the Polyvagal theory, which adopts a phylogenetic approach.24 Both models emphasize how reduced HRV approximates a failure to inhibit maladaptive cardiac autonomic response to stress and perceived threats, whereas increased HRV promotes behavioral adaption and cognitive flexibility, all of which are inherent features to a number of psychiatric illnesses.
Considering the relationship between HRV and many core clinical features of psychiatric illness, the efficacy of novel treatments designed to increase HRV and, perhaps concordantly improve symptoms, is now being explored. HRV biofeedback has been shown to increase HRV by training resonance frequency breathing, which is typically 5.5 breaths per minute on average,25 but can vary from person to person.26 Early HRV biofeedback trials have demonstrated good tolerability and modest symptom improvements in anxiety, mood and substance-use disorders.27, 28, 29, 30, 31 Vagus nerve stimulation (VNS), which involves surgical implants of electrodes to the left vagus nerve, also increases HRV.32, 33 VNS has demonstrated effectiveness in treatment-resistant depression,34, 35, 36, 37 with the US Food and Drug Administration granting approval for such therapeutic use of VNS in 2005. Owing to the risks of surgery, however, VNS is only indicated for the most severe cases of depression. Non-invasive transcutaneous VNS that stimulates afferent vagus nerve fibers located in the ear38 has also demonstrated similar results,39, 40 which may open up such treatment to more individuals with depression.
Many HRV studies in psychiatry refer to a set of standards established almost two decades ago.7 While the general principles surrounding data collection, analysis and interpretation outlined in this report remain relatively unchanged (apart from novel HRV parameters41), coordinated efforts to improve research reporting and reproducibility have only recently emerged.42, 43 Given the absence of reporting standards specific to psychiatric research, it is therefore unsurprising that critical study details are inconsistently communicated.14, 44
The drawbacks of inconsistent study reporting
Inconsistent descriptions of study methodology present a significant problem for the scientific community at large. First, a lack of methodological detail may hinder or delay peer-review. Almost half of a large sample of researchers (n=4037) described the peer-review process as ‘slow’ or ‘very slow’.45 Appropriate reporting of HRV methods will reduce the need to request additional technical details, which then need to be gathered and structured by the original authors, benefitting both reviewers and editors. Standardized reporting of HRV methods will also benefit authors, assisting in the design of experiments and data collection.
Second, a lack of methodological detail hinders replication. A growing movement within the scientific community supports the standardization of reporting methodological details and providing transparent access to original data to improve the odds of replicability. Such large replication projects have described similar impediments because of a lack of methodological details in non-biological psychology,43, 46, 47, 48 neuroimaging49, 50 and drug discovery.51 Ostensibly, the goal of a methods section is the description of methodology such that findings may be replicated from written papers without clarification or reference to other sources. However, the reporting of methodological details required for replications is often inconsistent.
Third, unclear methodology presents inevitable and occasionally insoluble problems for performing meta-analyses; that is, the statistical combination of multiple studies to calculate a summary effect size for a given research question. Even combining effect sizes from two or three sets of data meaningfully increases statistical precision.52 However, the quality of data reporting in HRV research is mixed, if it is even available, and requests for additional data because of incomplete information often yield low response rates.14, 44 As large replication endeavors have often noted, retrospective requests for data or detailed protocols may be difficult to fulfill; for instance, data retention requirements for psychological or clinical data vary between institutions, the responsible students or staff may not be present at the time of the data request or data may be lost or corrupted because of older electronic data-storage systems. Moreover, the initial lead researcher may have no time for, or interest in, assisting with replication or meta-analyses. Researchers occasionally invoke the violation of privacy regulations, such as the Health Insurance Portability and Accountability Act, when declining data-sharing requests. Many methods have been developed that comply with Health Insurance Portability and Accountability Act-compliant de-identification.53, 54, 55 In cases where data cannot be appropriately de-identified (for example, participants all live in a specific geographical region), additional privacy safeguards, such as data-usage agreements, can be implemented.56, 57 To facilitate the sharing of data, consent processes can be updated to inform potential participants who de-identified study data may be shared.56, 58 Researchers may also associate direct replication with implicit criticism and may be uncomfortable with other laboratories pursuing their initial protocols as replication may miss the nuance of the original protocol.59 In short, insufficient reporting may slow, obstruct or even directly impede the calculation of meta-analytical effect sizes and related moderator analyses.
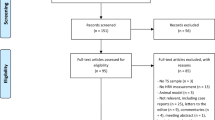
In consideration of these factors, we propose the Guidelines for Reporting Articles on Psychiatry and Heart rate variability—GRAPH. Research reported according to the 13-item GRAPH checklist (Figure 1 and Table 1; also see Supplementary Table 1 for a downloadable template) will help expedite translational research efforts by reducing the need for data and protocol requests for meta-analysis, replication and peer-review. Most importantly, the reader will have increased means to examine research in the field critically. We cover important considerations for HRV studies in psychiatry and biobehavioral research that include the following: selection of participants, interbeat interval (IBI) collection, data preparation and HRV calculation. Although we hasten to emphasize that we are not attempting to advocate a standard for HRV research—the breadth of research questions and methods renders this impractical—providing this information will help improve the interpretation of HRV research in psychiatry and related disciplines. Although not an exhaustive list of all the potential methodological considerations for the collection and analysis of HRV data, these guidelines are intended to provide a minimum set of criteria from which to design and report HRV studies in psychiatry.
Participant selection
The selection and description of study participants is an integral, but oft-under-reported aspect of HRV research in psychiatry. Proper appraisal requires a minimum standard of information on study populations, particularly for case–control designs. When studies include a psychiatric population, for example, the method of diagnosis is an important detail considering the variability of classification accuracy. Different classification systems are available for diagnosis (the Diagnostic and Statistical Manual for Mental Disorders and the International Classification of Diseases). These diagnoses can be determined via structured clinical assessments administered by specialists and non-specialists. Indeed, inexperienced interviewers, such as graduate students, can have difficulties classifying psychiatric illness.60, 61, 62
Diagnoses can also be gathered via self-report. Simple self-reported diagnoses are the least accurate means of collecting diagnostic information; as many as half of patients are unaware or unable to correctly identify their diagnosis.63 Data from self-report questionnaires may show satisfactory agreement with structured clinical interviews and clinician diagnoses. However, they cannot replace clinical interviews for diagnosis, a point emphasized by the authors of many of these screening instruments.64, 65, 66 An additional confound is the large range of available self-report questionnaires, with variable validity, rendering comparisons between studies difficult. Data from participants with subclinical symptomology, particularly ‘high-trait’ groups, based on these self-report questionnaires are still valuable, but such distinction needs to be explicit (for example, self-report questionnaire cutoffs). Disorder characteristics can also influence HRV. For instance, age of onset and illness severity are associated with HRV.13, 67 Finally, psychiatric comorbidities, which are common in psychiatric illness,68 also modify HRV in psychiatric populations.69
Healthy participants are often recruited to HRV studies to study behavioral or cognitive correlates, as a comparison with a clinical population, or a combination of both these goals. Bearing in mind the well-described association between mental illness and HRV, adequate descriptions (as detailed above) of how the absence of the condition was determined in controls are important. This is not only relevant in studies that compare HRV between a psychiatric population and controls but also studies that exclusively report the recruitment of healthy controls. Relatedly, the source of the healthy comparison group is also relevant. Many studies recruit ‘hypernormal’ controls (also referred to as ‘well’ controls) who are not representative of the general population.70, 71 Although it is ideal to recruit participants from the same sampled population as the clinical group, this may not always be possible or practical because of cost and time considerations (but see Schechter and Lebovitch72). Specific information about where control groups were selected from can provide a more accurate assessment of whether differences between groups may be exaggerated by potential control group population biases (for example, socioeconomic status and race).
Irrespective of the psychiatric status, reporting of pre-specified participant exclusion and inclusion criteria requires adequate description. Research indicates that demographic attributes, such as gender,73 physical activity levels74, 75 and habitual levels of alcohol,11, 76 and nicotine intake77 influence HRV. Age is of particular importance as it is inversely related to HRV78, 79 and patient groups are often older compared with the younger university/college students usually recruited to healthy sample studies. The occurrence of physiological conditions80, 81 and ectopic beats also increases with age.82, 83 In addition, physical health conditions such as cardiovascular,84, 85, 86 metabolic87 and renal diseases88, 89, 90 can have an impact on HRV and occur at increased frequency in psychiatric conditions. Relatedly, cardiovascular and psychotropic medications (especially, tricyclic antidepressants) also have an appreciable impact on HRV.13, 14, 91 Assessing for these factors is particularly important when comparing clinical and nonclinical groups, as they can often differ on many of these domains but may not be standardly assessed or reported.
IBI collection
Hardware
Interbeat interval data have traditionally been collected via electrocardiogram (ECG) or photopletysmography. These methods still represent the bulk of recordings, although more recent technologies are available or in development, such as smartphone-enabled optical pulse sensors,92 webcam video,93 ultrasounds to index fetal heart period,94 microwave radar,95 cushion-mounted ballistocardiogram96 and toilet seats.97 To assist interpretation and reproducibility, research should communicate details of the device (for example, manufacturer and model) along with the software used for IBI extraction or analysis. If the device is commercially unavailable, the researcher should provide more detailed information, including but not limited to the analog front-end, microcontroller unit, peripherals, electrodes and so on. Likewise, any data concerning explicit validation against existing measurement devices should be included. Many sports watch-monitor manufacturers offer models with sufficient sampling rates to calculate HRV (for example, Polar and Suunto). However, researchers do not have access to metrics about how these devices are identifying or correcting errors, consequently making the decision on the data quality sufficient for retention in analyses difficult. Error identification might be possible to some degree from RR intervals, but these devices do not provide the ECG trace, which can be used to better identify cardiac dysrhythmia. Thus, using these devices to investigate a condition or population characterized by above-average error or ectopy may be problematic.98
Recent advances in technology along with the rise of the ‘quantified self’ movement,99 where people track and monitor their own biometric data, have converged to create a new category of consumer devices purported to measure HRV. However, these devices are generally not formally validated against an ECG for accuracy. Moreover, these devices often (a) report a proprietary metric rather than a standard metric, (b) do not provide access to raw data and (c) do not offer technical details of correction methods (if any are present). Researchers should consider their own investigations into the validity of novel devices to determine their accuracy in the population of interest. Without a method of checking the original sinus rhythm there is no way to determine the accuracy of potential errors in a beat-to-beat series. That is, a proprietary device may return accurate beat information, but other device and individual patient factors may go undetected. For instance, vascular insufficiency may interfere with the collection of photopletysmography signals, and cardiac arrhythmia may interfere with the collection of ECG signals, both of which may be impossible to determine without inspection of the raw data.
Sampling rate
While the electrocardiographic P-wave is the direct representation of sinoatrial (SA) depolarization, and therefore the closest indication of the initiation of the cardiac cycle, the R-wave (which corresponds to ventricular depolarization) is used for convenience. As temporal accuracy is important to calculate the variance of a time series successfully, previous guidelines provided a minimum desirable sampling rate,7 with 500 Hz being the recommended threshold to accurately identify native fiducial points.100, 101 Having said that, 250 Hz may also be adequate when collecting data from healthy adults.102 It is still possible that Holter legacy data, which was typically recorded at 128 Hz, may be below this minimum. However, early data recorded at 128 Hz may still provide useful information if the error subsequent to the slower sample rate is recognized. Altogether, this consideration is only occasionally relevant to contemporary research, as hardware standards are often well in excess of minimum sampling rates—commercial devices are readily available with native sampling rates of 1–8 kHz. Moreover, it is clear that R-wave fiducial points can be easily reconstructed from lower-sampled signals as a 128-Hz signal contains enough data to improve the information in the signal. For instance, the reconstruction of R-waves even with a simple quadratic correction allows 128-Hz data to show equivalent accuracy to 512 Hz (Figure 2). As a consequence, research should state the native sampling rate of the hardware utilized, along with any details of signal reconstruction (if applicable).
Reconstruction of interbeat interval (IBI) signal. s.d. of errors compared with a natively sampled 2048-Hz signal in a single 15-min recording where all IBIs are identifiable; a simple quadratic correction to the peaks of the 128-Hz signal (c128) results in comparative accuracy to the natively sampled 512-Hz signal.
Time factors of recording
Whereas HRV has historically been calculated using 24-hour Holter monitoring—which offers superior prediction of future cardiovascular disease mortality103 and the opportunity to evaluate longer-term circadian HRV differences—the majority of HRV data within psychiatry and the behavioral sciences have been calculated using short-term recordings (durations between 1 and 5 min). The Task Force statement suggests a minimum of 60-s continuous recording to quantify high-frequency (HF) HRV,7 with recent work showing reasonable agreement between ultrashort-term HRV measures (<60 s) and 5-min periods.104 Two other recommendations for time periods are common (although neither appears to be strictly analytical): (a) 5 min of baseline recording, which is an overwhelmingly popular standard for most frequency domain HRV recordings,105 and likely a vestigial standard leftover from the original processing limits of the PDP-8 minicomputers originally used to collect ECG during the 1960s; and (b) 10 cycles of the lowest frequency of interest, or at least 250 s of recording in a standard frequency domain analysis reporting a low-frequency (LF) band with a lower bound of 0.04 Hz.
A related issue for consideration is acclimatization to the recording environment. Often this is accomplished by using an analysis period that begins subsequent to the start of recording, an approach used by ourselves19, 67, 92 and others.106, 107, 108 Acclimatization can help reduce any HRV changes because of posture, which may take time to adjust if the participant has just assumed a supine or seated position.109, 110, 111 Acclimatization may also reduce confounds subsequent to test anxiety in psychiatric populations. Considering the impact of attentive states on respiratory frequency,112 which subsequently influences the ECG recording,113 the beginning of the recording period should not be announced. As the comparison of HRV between different time periods is also problematic,114 the longer period should be reduced to match the shorter period.
Posture and procedures
Posture has a well-characterized effect on autonomic outflow, which is proportional to the shift of the body axis because of the primarily sympathetic response to venous pooling and consequent involvement of the baroreflex. The use of graded tilt—whereby an immobile participant’s posture is increased in progressive increments from supine to upright—reveals a strong curvilinear relationship between posture and HRV.109, 115 Consequently, direct equivalence between supine, seated and standing recording is not warranted, given these differences and wider dispersion of HRV during supine recordings compared with upright.
The instructions given for a task are also an important consideration. In some cases,116, 117, 118 researchers administer a low-demand cognitive ‘Vanilla’ Task,119 which may have some relevance for psychiatric populations that have difficulty sitting still or experience stress under experimental ‘resting-state’ conditions. Instructions with attentional demands may also modulate HRV, primarily because of changes in respiratory depth and frequency. Regardless, the instructions given to the participant should be stated. Some researchers have also attempted to blind participants to the purpose of the equipment that measures respiration to encourage true spontaneous breathing. For instance, Vlemincx et al.112 explained to participants that respiratory sensors built into a garment were collecting information on muscle tension. Thus, instructions given to participants for baseline recordings should be noted. Considering the influence of circadian rhythms and digestion on HRV,120, 121, 122, 123 time of day and time since last meal should also be noted and standardized where possible in short-term HRV recordings, especially for designs incorporating repeated recordings over time.
Other signals
The obvious ancillary recording for the measurement of HRV is respiration, due to its direct influence on HF HRV.124, 125, 126 However, the importance of monitoring respiration under resting conditions is not settled. Proponents for respiratory monitoring maintain that respiration should be controlled, as respiratory parameters may modify the relationship between HF HRV and cardiac vagal modulation.127 Others argue that this is not necessary,128 as these respiratory and HR oscillations have the same origin.129 Regardless, respiration is almost exclusively the source HF HRV (with some modest contributions from other sources, such chest compression130), and respiratory data provide information that directly affects the cardiac cycle, such as respiratory frequency and depth. Erratic sinus arrhythmia (see more information below) may also contribute to the HF band despite its non-respiratory origin.15 Indirect measures of respiration can also be calculated from ECG131, 132, 133 and photoplethysmographic134 signals. The potential to compute respiration directly from a record of cardiac intervals without the need for monitoring via impedance, belt or mask is appealing, considering its simplicity. In specific situations, respiration may be of interest to researchers investigating populations that happen to breathe slowly, such as athletes74 or meditators.135 On the other end of the spectrum, some patient populations,136, 137 and children138 breathe at a faster rate. There is evidence to suggest that periodic and sudden fluctuations in the respiratory rate are both a source of altered HRV variability over time and are directly mediated by experimental task demands.112 The presence and frequency of sighs, which are reported to be increased in psychiatric illnesses,139, 140 should also be monitored as these produce large deviations from typical respiratory length and depth.141 HRV is also dependent on HR in an inverse nonlinear manner.142, 143 A mathematical correction for this dependency has been proposed to improve HRV reproducibility.144 Finally, using exercise as a stress task will also increase the respiratory rate.145
Data cleaning and analysis
IBI calculation
Identifying IBIs is computationally straightforward; the Pan-Tompkins algorithm,146 where the raw ECG signal is bandpassed, differentiated, squared, integrated and smoothed to isolate R-waves, was developed over 30 years ago and remains a common and effective processing method. After peak detection is achieved, most frequency domain analysis methods resample the RR series into an evenly sampled time series (typically between 1 and 10 Hz). Different resampling rates may affect equivalent frequency transforms; however, this usually is not profound as long as researchers satisfy the Nyquist criterion.147
Several sources of artifact that may affect the frequency bands of interest are common.148 The main sources of contamination include powerline interference (at 50 or 60Hz depending on the nature of local AC power), muscle contraction or movement artifacts, and baseline drift. The occurrence of one or more of these in any given data set is almost certain, but may be highly variable; therefore, filtering of data for artifacts should be clearly noted in manuscripts along with whether beat detection was visually inspected as some systems (predominately clinically oriented suites) do not provide this facility. To aid future analysis, the raw signal should be recorded without online filtering during data acquisition, if possible.
Non-sinus beat/arrhythmia identification
A central premise of HRV is that IBIs approximate SA node-firing patterns, otherwise known as normal sinus rhythm. Accordingly, a fiducial point that does not originate from the SA node (that is, a non-sinus beat) does not represent the autonomic nervous system input to the SA node. Two common sources of non-sinus beats are the atria and ventricles, which can prompt an atrial premature contraction and ventricular premature contraction (VPC), respectively. As these beats are premature, they lead to a short R–R interval followed by a long compensatory R–R interval (Figure 3). Pathological causes of ectopy include electrolyte abnormalities, ischemia and cardiomyopathy. Ventricular arrhythmias can also be generated from an unmasked ectopic focus in populations with very low HR, such as athletes.149 More benign causes of ectopy in healthy populations include caffeine or nicotine,150, 151 which is one reason most researchers ask participants to refrain from such intake before IBI collection. To our knowledge, research is yet to examine the impact of caffeine withdrawal on HRV, which requires future investigation. However, double-blind experiments suggest that abstinence in those that regularly consume caffeine has no effect on heart rate.152
Although even one misidentified beat can have a considerable influence on HRV calculation,153 there is no consensus or absolute criteria for defining atrial premature contraction or VPCs via algorithm. Accordingly, manual inspection of the ECG trace is needed for non-sinus beat identification. Many software packages attempt to make their own corrections from R–R intervals, not from identifying incorrect ECG signals. Atrial premature contractions and VPCs are relatively common; a few percent in a healthy population,82, 83 a higher percentage in an athletic population154, 155 and higher still in some cardiac conditions.156 However, many papers do not seem to have any corrections or removals at all or omit these details entirely.
Correcting these artifacts assumes only that the directly affected beats are problematic. However, a further concern exists if VPCs are the source of heart rate turbulence, in which a non-sinus beat causes subsequent short-term R–R changes.157 In healthy people, the compensatory pause after a VPC is followed by brief R–R interval acceleration, and then R–R interval deceleration. This pattern is not observed in high-risk patients, with decreased deceleration speed (that is, turbulence slope) shown to be a powerful predictor of mortality.157, 158 It is thought that heart rate turbulence has a baroreflex origin,159 whereby a VPC causes a brief drop in blood pressure, leading to baroreceptor inhibition of vagal input, which leads to a brief increase in heart rate. Careful inspection of the ECG signal can help both identify ectopy, as this can occur without artifact, and any subsequent heart rate turbulence. Visual inspection can also help identify artifacts that can be missed with commonly used filter thresholds. For example, people with extremely high or low HRV can have normal sinus beats misidentified as ectopic beats. Thresholds can also be adapted depending on the population.
Erratic sinus arrhythmia is a less well-recognized form of persistent arrhythmia that differs from ectopy in that heart beats appear to have normal electrocardiographic morphology (that is, they have sinus origin) but display short-term variation that is non-respiratory in origin.15, 160 Although erratic sinus arrhythmia has been strongly associated with serious cardiovascular illness, predicting post-infarction survival,161 this does not preclude it from occurring in other healthy or patient populations. An inspection of the Poincaré plot (a scatterplot where each point represents two consecutive heart periods) for regularity may be sufficient to reveal the presence of erratic sinus arrhythmia,160, 162 and should be performed on IBI series with inexplicably high HRV. Consequently, how beat inspection was performed, the percentage of beats identified per participant and any exclusions because of abnormal sinus rhythm should be explicitly stated.
IBI data loss
There are many reasons for discarding data apart from persistent arrhythmia. These include hardware/software errors, wire loss, poor electrode contact, extraneous magnetic or line noise, excessive movement artifacts, EMG artifacts, experimenter error, file corruption, physical loss and accidental duplication. ECG signal characteristics, such as wide QRS complexes or tall t-waves, can also contribute to peak detection difficulties. These errors also influence how the viability of the experimental model is confirmed. For instance, movement-based tasks may destroy inappropriately filtered signals or experiments may use incorrect electrode sites or fail to manage data collection properly.
Data loss as a difference between groups is also concerning. For instance, a stress induction would conceivably cause more errors in a psychiatric sample compared with a control group. This leaves the investigator with a task by outcome interaction, which needs to be accounted for before normal task effects. The percentage of beats removed from the sample has a direct impact on accuracy, thus reporting that this percentage can be instructive. Ideally, the percentage of removed beats should be equivalent between groups to ensure that differences are because of the autonomic nervous system rather than artifact. Some methods preserve accuracy with data loss well; however, all methods perform badly when long sections are lost.163 This frequently happens with photopletysmography recordings because movement artifacts destroy adaptive filters, which often require 5–6 s to ‘re-adapt’. Five percent is the commonly stated threshold for R-peak data loss to render a series unusable (for example, Heathers et al.164), which to our knowledge has no empirical basis. However this, again, is a convention instead of an analytic barrier; therefore, the threshold used should be noted.
IBI cleaning
When adjusting for errors, as above, the beat replacement method can directly affect measurement outcome. Just removing the beat is problematic, especially for shorter recordings and frequency domain calculations.153 Linear correction and cubic spline interpolation are acceptable solutions, but both potentially introduce errors (for a review of beat replacement techniques, see Peltola165). Time-domain methods, which are less sophisticated, also have the benefit that errors can simply be removed proportionally. Multiple consecutive errors cannot be handled the same way as single errors. If the researcher expects frequencies of up to 0.4 Hz in signals, then the loss of several beats in a row requires a different approach, such as discarding the sample entirely. However, work frequently combines and compares time and frequency domain methods of HRV. Consequently, a single correction method for replacement should be used before smoothing or decimation.
HRV calculation
Method of analysis used
There are more than 70 published metrics for calculating HRV.166, 167 Methods may be time domain (such as the s.d. of the NN interval), frequency domain (such as the Fast Fourier Transform), time–frequency domain (such as the continuous wavelet transform) or ‘nonlinear’ methods, many of which are not strictly nonlinear (for example, correlation dimension, detrended fluctuation analysis, approximate entropy and sample entropy). Several direct equivalencies exist between these methods.168, 169 Frequency domain analysis is typically computed by fast Fourier transform or autoregressive techniques, which are almost equivalent for the HF band (r=0.96 Hayano et al.170). Other techniques include the Lomb–Scargle periodogram171, 172 and smoothed pseudo Wigner–Ville distribution.173
Although these methods may be similar, they should not be assumed directly equivalent under all circumstances.174 The resolution of a peak frequency in particular may be different between methods because of the smoothness of the power spectral density.175 All analytical results are subjected to a series of methodological assumptions (for example, windowing method, window length, overlap and frequency bands in frequency domain analysis). Therefore, the explanation of the analytic method chosen should be stated in enough detail such that a competent external researcher could reproduce the analysis with sole access to the manuscript. However, the exact details that this includes will differ with each method. As s.d. of the NN interval and power spectral density analysis (HF and LF powers) are the best characterized HRV metrics in terms of clinical use41 and historically the most commonly used metrics,176 continued reporting of these measures will aid replication and meta-analysis. If novel HRV methods are used, researchers should follow recent recommendations from the European Society of Cardiology, who suggest that novel methods should be reported in tandem with traditional HRV measures.41
Selection and interpretation of frequency bands
Frequency domain analysis of IBI data is computationally straightforward. Whereas there are recommendations for bands to use in adults (LF, 0.04–0.15 Hz; HF, 0.15–0.4 Hz), children and infants (LF, 0.04–0.24 Hz; HF, 0.24–1.04 Hz) at rest because of spontaneous breathing rates, these are not necessarily important in other circumstances. For instance, some athletes have respiratory rates sufficiently slow as to interfere with the traditional interpretation of the measured HF band.74 Population characteristics should be considered when bands are chosen, either by looking at past research or by calculating respiratory rates of the data in question.
Disagreements over the teleology and mechanics of HF are minimal at present (but see Billman176), especially compared with disagreements over the nature of LF and the ratio between the bands LF/HF.105, 177, 178 For instance, LF is variously reported as a measure of ‘sympathetic activation’, a component of activity in ‘sympathovagal balance’ or a measure of sympathetic nervous system activity instead of activity of the baroreflex in response to vasomotor tone.105, 179 Subsequently, the Task Force paper7 requests reporting and analysis of raw LF and HF powers in addition to additional interpretation of those bands. Likewise, the parameters of those bands and their putative interpretation should be declared. These bands should also always be reported in standard format (that is, as LF and HF power in ms2/Hz) before further calculation. Finally, it is important to not overextrapolate short-term experimental recordings against established 24-h HRV findings.
Additional considerations for reporting HRV studies
Data and analysis script archiving
Development of new signal analytic techniques, confirmation of existing findings and meta-analyses rely on access not just to both existing results and the raw data from those results. Instead of relying on effect size comparison between studies with different methodologies for meta-analysis, pooling individual data points using mega-analysis would help adjust for within-subject differences in methodology.180 Mega-analyses have already been applied to other areas of biobehavioral research.181, 182, 183 The largest HRV meta-analysis in psychiatry to date, which included 170 studies, suggested that only 20–25% of observed heterogeneity was because of sampling error.14 This indicates that other factors, such as HRV calculation methodology, are contributing to heterogeneity in effect sizes. Moreover, mega-analyses can determine the degree to which differences in methodology contribute to heterogeneity compared with other heterogeneity sources.184 However, given the complexities surrounding data sharing,185 such as the precarious balance between openness and privacy, we feel that this cannot be included as a strict recommendation to publication. Nevertheless, the increasing movement from many publishers toward open-access sharing of data as an essential publishing requirement may mean that many of these heterogeneity issues could be addressed in future analyses of pooled individual data. Finally, the availability of the precise details of statistical analysis (that is, analysis scripts) may also improve reproducibility of research, as it offers the reader and reviewers the opportunity to closely examine how results were generated.
Conclusion
The discipline of ‘meta-research’ is a relatively recent proposal to accelerate the translation of scientific research by improving research methods, reporting, reproducibility and evaluation.42 HRV research in psychiatry tends to under-report important methodological details required for critical evaluation. For this reason, we have designed guidelines that consider important details related to this research to streamline reporting. These are not additional requirements for analysis, rather are criteria by which decisions that are made in every paper by necessity. The requested information already exists, in every paper, regardless of whether or not it represents a conscious decision by the author or has been omitted for the sake of brevity in the publishing process. We have summarized these guidelines in a 13-item checklist (Table 1 and Supplementary Table 1) and expect that adherence to these guidelines will improve reproducibility, expand the ability to perform meta-analyses, improve critical evaluation and expedite the peer-review process. Moreover, these guidelines will enhance the clarity of HRV research in psychiatry. Consideration of these guidelines at early stages of project planning will also aid study design. We make no attempt to recommend how HRV studies in psychiatry ought to be conducted because of sheer impracticality. The central question when assessing a methods section is to determine how the study reached its conclusions; therefore, the singular purpose of these guidelines is to facilitate the clear communication of research findings to accelerate the translation of psychiatric research.
References
Hon EH, Lee S . Electronic evaluation of the fetal heart rate patterns preceding death, further observations. Am J Obstet Gynecol 1963; 87: 814–826.
Kleiger RE, Miller JP, Bigger JT, Moss AJ . Decreased heart rate variability and its association with increased mortality after acute myocardial infarction. Am J Cardiol 1987; 59: 256–262.
Bigger JT, Fleiss JL, Steinman RC, Rolnitzky LM, Kleiger RE, Rottman JN . Frequency domain measures of heart period variability and mortality after myocardial infarction. Circulation 1992; 85: 164–171.
Cripps T, Malik M, Farrell T, Camm A . Prognostic value of reduced heart rate variability after myocardial infarction: clinical evaluation of a new analysis method. Br Heart J 1991; 65: 14–19.
Bigger JT, Fleiss JL, Rolnitzky LM, Steinman RC . Frequency domain measures of heart period variability to assess risk late after myocardial infarction. J Am Coll Cardiol 1993; 21: 729–736.
Akselrod S, Gordon D, Ubel FA, Shannon DC, Berger A, Cohen RJ . Power spectrum analysis of heart rate fluctuation: a quantitative probe of beat-to-beat cardiovascular control. Science 1981; 213: 220–222.
Camm A, Malik M, Bigger J, Breithardt G, Cerutti S, Cohen R et al. Heart rate variability: standards of measurement, physiological interpretation and clinical use. Task Force of the European Society of Cardiology and the North American Society of Pacing and Electrophysiology. Circulation 1996; 93: 1043–1065.
Pagani M, Lombardi F, Guzzetti S, Sandrone G, Rimoldi O, Malfatto G et al. Power spectral density of heart rate variability as an index of sympatho-vagal interaction in normal and hypertensive subjects. J Hypertens Suppl 1984; 2: S383–S385.
Beauchaine TP, Thayer JF . Heart rate variability as a transdiagnostic biomarker of psychopathology. Int J Psychophysiol 2015; 98: 338–350.
Cuthbert BN, Insel TR . Toward the future of psychiatric diagnosis: the seven pillars of RDoC. BMC Med 2013; 11: 126.
Quintana DS, McGregor IS, Guastella AJ, Malhi GS, Kemp AH . A meta‐analysis on the impact of alcohol dependence on short‐term resting‐state heart rate variability: implications for cardiovascular risk. Alcoholism: Clinical and Experimental Research 2013; 37: E23–E29.
Chalmers J, Quintana DS, Abbott MJ, Kemp AH . Anxiety disorders are associated with reduced heart rate variability: a meta-analysis. Front Psychiatry 2014; 5: 80.
Kemp AH, Quintana DS, Gray MA, Felmingham KL, Brown K, Gatt JM . Impact of depression and antidepressant treatment on heart rate variability: a review and meta-analysis. Biol Psychiatry 2010; 67: 1067–1074.
Alvares GA, Quintana DS, Hickie IB, Guastella AJ . Autonomic nervous system dysfunction in psychiatric disorders and the impact of psychotropic medications: a systematic review and meta-analysis. J Psychiatry Neurosci 2016; 41: 89–104.
Stein PK, Domitrovich PP, Hui N, Rautaharju P, Gottdiener J . Sometimes higher heart rate variability is not better heart rate variability: results of graphical and nonlinear analyses. J Cardiovasc Electrophysiol 2005; 16: 954–959.
Thayer JF, Yamamoto SS, Brosschot JF . The relationship of autonomic imbalance, heart rate variability and cardiovascular disease risk factors. Int J Cardiol 2010; 141: 122–131.
Hennekens CH, Hennekens AR, Hollar D, Casey DE . Schizophrenia and increased risks of cardiovascular disease. Am Heart J 2005; 150: 1115–1121.
Newcomer JW, Hennekens CH . Severe mental illness and risk of cardiovascular disease. JAMA 2007; 298: 1794–1796.
Quintana DS, Guastella AJ, Outhred T, Hickie IB, Kemp AH . Heart rate variability is associated with emotion recognition: direct evidence for a relationship between the autonomic nervous system and social cognition. Int J Psychophysiol 2012; 86: 168–172.
Bal E, Harden E, Lamb D, Van Hecke AV, Denver JW, Porges SW . Emotion recognition in children with autism spectrum disorders: relations to eye gaze and autonomic state. J Autism Dev Disord 2010; 40: 358–370.
Hansen AL, Johnsen BH, Sollers JJ III, Stenvik K, Thayer JF . Heart rate variability and its relation to prefrontal cognitive function: the effects of training and detraining. Eur J Appl Physiol 2004; 93: 263–272.
Mulder G, Mulder LJ . Information processing and cardiovascular control. Psychophysiology 1981; 18: 392–402.
Thayer JF, Lane RD . A model of neurovisceral integration in emotion regulation and dysregulation. J Affect Disord 2000; 61: 201–216.
Porges SW . Orienting in a defensive world: mammalian modifications of our evolutionary heritage. A polyvagal theory. Psychophysiology 1995; 32: 301–318.
Vaschillo E, Lehrer P, Rishe N, Konstantinov M . Heart rate variability biofeedback as a method for assessing baroreflex function: a preliminary study of resonance in the cardiovascular system. Appl Psychophysiol Biofeedback 2002; 27: 1–27.
Vaschillo EG, Vaschillo B, Lehrer PM . Characteristics of resonance in heart rate variability stimulated by biofeedback. Appl Psychophysiol Biofeedback 2006; 31: 129–142.
Karavidas MK, Lehrer PM, Vaschillo E, Vaschillo B, Marin H, Buyske S et al. Preliminary results of an open label study of heart rate variability biofeedback for the treatment of major depression. Appl Psychophysiol Biofeedback 2007; 32: 19–30.
Wells R, Outhred T, Heathers JA, Quintana DS, Kemp AH . Matter over mind: a randomised-controlled trial of single-session biofeedback training on performance anxiety and heart rate variability in musicians. PLoS One 2012; 7: e46597.
Tan G, Dao TK, Farmer L, Sutherland RJ, Gevirtz R . Heart rate variability (HRV) and posttraumatic stress disorder (PTSD): a pilot study. Appl Psychophysiol Biofeedback 2011; 36: 27–35.
Eddie D, Kim C, Lehrer P, Deneke E, Bates ME . A pilot study of brief heart rate variability biofeedback to reduce craving in young adult men receiving inpatient treatment for substance use disorders. Appl Psychophysiol Biofeedback 2014; 39: 181–192.
Beckham AJ, Greene TB, Meltzer-Brody S . A pilot study of heart rate variability biofeedback therapy in the treatment of perinatal depression on a specialized perinatal psychiatry inpatient unit. Arch Womens Ment Health 2013; 16: 59–65.
Kamath M, Upton A, Talalla A, Fallen E . Effect of vagal nerve electrostimulation on the power spectrum of heart rate variability in man. Pacing Clin Electrophysiol 1992; 15: 235–243.
Zhang Y, Popović ZB, Bibevski S, Fakhry I, Sica DA, Van Wagoner DR et al. Chronic vagus nerve stimulation improves autonomic control and attenuates systemic inflammation and heart failure progression in a canine high-rate pacing model. Circulation 2009; 2: 692–699.
George MS, Rush AJ, Marangell LB, Sackeim HA, Brannan SK, Davis SM et al. A one-year comparison of vagus nerve stimulation with treatment as usual for treatment-resistant depression. Biol Psychiatry 2005; 58: 364–373.
Daban C, Martinez-Aran A, Cruz N, Vieta E . Safety and efficacy of Vagus Nerve Stimulation in treatment-resistant depression. A systematic review. J Affect Disord 2008; 110: 1–15.
Nemeroff CB, Mayberg HS, Krahl SE, McNamara J, Frazer A, Henry TR et al. VNS therapy in treatment-resistant depression: clinical evidence and putative neurobiological mechanisms. Neuropsychopharmacology 2006; 31: 1345–1355.
Rush AJ, Sackeim HA, Marangell LB, George MS, Brannan SK, Davis SM et al. Effects of 12 months of vagus nerve stimulation in treatment-resistant depression: a naturalistic study. Biol Psychiatry 2005; 58: 355–363.
Peuker ET, Filler TJ . The nerve supply for human auricle. Clin Anat 2002; 15: 35–37.
Fang J, Rong P, Hong Y, Fan Y, Liu J, Wang H et al. Transcutaneous vagus nerve stimulation modulates default mode network in major depressive disorder. Biol Psychiatry 2015; 79: 266–273.
Hein E, Nowak M, Kiess O, Biermann T, Bayerlein K, Kornhuber J et al. Auricular transcutaneous electrical nerve stimulation in depressed patients: a randomized controlled pilot study. J Neural Transm 2013; 120: 821–827.
Sassi R, Cerutti S, Lombardi F, Malik M, Huikuri HV, Peng C-K et al. Advances in heart rate variability signal analysis: joint position statement by the e-Cardiology ESC Working Group and the European Heart Rhythm Association co-endorsed by the Asia Pacific Heart Rhythm Society. Europace 2015; 17: 1341–1353.
Ioannidis JP, Fanelli D, Dunne DD, Goodman SN . Meta-research: evaluation and improvement of research methods and practices. PLoS Biol 2015; 13: e1002264.
Open Science Collaboration. An open, large-scale, collaborative effort to estimate the reproducibility of psychological science. Perspect Psychol Sci 2012; 7: 657–660.
Tak LM, Riese H, de Bock GH, Manoharan A, Kok IC, Rosmalen JG . As good as it gets? A meta-analysis and systematic review of methodological quality of heart rate variability studies in functional somatic disorders. Biol Psychol 2009; 82: 101–110.
Mulligan A, Hall L, Raphael E . Peer review in a changing world: an international study measuring the attitudes of researchers. J Am Soc Inform Sci Technol 2013; 64: 132–161.
Ritchie SJ, Wiseman R, French CC . Failing the future: three unsuccessful attempts to replicate Bem’s ‘retroactive facilitation of recall’ effect. PLoS ONE 2012; 7: e33423.
Klein RA, Ratliff KA, Vianello M, Adams RB Jr, Bahník Š, Bernstein MJ et al. Investigating variation in replicability. Soc Psychol 2015.
Open Science Collaboration. Estimating the reproducibility of psychological science. Science 2015; 349: aac4716.
Fletcher PC, Grafton ST . Repeat after me: replication in clinical neuroimaging is critical. NeuroImage 2013; 2: 247-248..
Button KS, Ioannidis JP, Mokrysz C, Nosek BA, Flint J, Robinson ES et al. Power failure: why small sample size undermines the reliability of neuroscience. Nat Rev Neurosci 2013; 14: 365–376.
Prinz F, Schlange T, Asadullah K . Believe it or not: how much can we rely on published data on potential drug targets? Nat Rev Drug Discov 2011; 10: 712–712.
Cumming G Understanding the New Statistics: Effect Sizes, Confidence Intervals, and Meta-Analysis. Routledge: New York, USA, 2013.
Sweeney L . k-nonymity: a model for protecting privacy. Int J Uncertain Fuzz 2002; 10: 557–570.
Li N, Li T, Venkatasubramanian S t-closeness: Privacy beyond k-anonymity and l-diversity. IEEE 23rd International Conference on Data Engineering, ICDE 2007. 15 April 2007; Istanbul, Turkey; IEEE, 2007.
Machanavajjhala A, Kifer D, Gehrke J, Venkitasubramaniam M . l-diversity: privacy beyond k-anonymity. ACM Trans Knowledge Discov Data 2007; 1: 3.
Mennes M, Biswal BB, Castellanos FX, Milham MP . Making data sharing work: the FCP/INDI experience. Neuroimage 2013; 82: 683–691.
Sarwate AD, Plis SM, Turner JA, Arbabshirani MR, Calhoun VD . Sharing privacy-sensitive access to neuroimaging and genetics data: a review and preliminary validation. Front Neuroinformatics 2014; 8: 35.
Antman EM, Benjamin EJ, Harrington RA, Houser SR, Peterson ED, Bauman MA et al. Acquisition, analysis, and sharing of data in 2015 and beyond: a survey of the landscape a conference report from the American Heart Association Data Summit 2015. J Am Heart Assoc 2015; 4: e002810.
Bohannon J . Replication effort provokes praise—and ‘bullying’ charges. Science 2014; 344: 788–789.
Mitchell AJ, Kakkadasam V . Ability of nurses to identify depression in primary care, secondary care and nursing homes—a meta-analysis of routine clinical accuracy. Int J Nurs Stud 2011; 48: 359–368.
Mitchell AJ, Rao S, Vaze A . Can general practitioners identify people with distress and mild depression? A meta-analysis of clinical accuracy. J Affect Disord 2011; 130: 26–36.
Ventura J, Liberman RP, Green MF, Shaner A, Mintz J . Training and quality assurance with the Structured Clinical Interview for DSM-IV (SCID-I/P). Psychiatry Res 1998; 79: 163–173.
Basco MR, Bostic JQ, Davies D, Rush AJ, Witte B, Hendrickse W et al. Methods to improve diagnostic accuracy in a community mental health setting. Am J Psychiatry 2014; 157: 1599–1605.
Foa EB, Cashman L, Jaycox L, Perry K . The validation of a self-report measure of posttraumatic stress disorder: The Posttraumatic Diagnostic Scale. Psychol Assess 1997; 9: 445.
Mulrow CD, Williams JW, Gerety MB, Ramirez G, Montiel OM, Kerber C . Case-finding instruments for depression in primary care settings. Ann Intern Med 1995; 122: 913–921.
Di Nardo PA, Moras K, Barlow DH, Rapee RM, Brown TA . Reliability of DSM-III-R anxiety disorder categories: using the Anxiety Disorders Interview Schedule—Revised (ADIS-R). Arch Gen Psychiatry 1993; 50: 251–256.
Alvares GA, Quintana DS, Kemp AH, Van Zwieten A, Balleine BW, Hickie IB et al. Reduced heart rate variability in social anxiety disorder: associations with gender and symptom severity. PLoS ONE 2013; 8: 7.
Kessler RC, Chiu WT, Demler O, Walters EE . Prevalence, severity, and comorbidity of 12-month DSM-IV disorders in the National Comorbidity Survey Replication. Arch Gen Psychiatry 2005; 62: 617–627.
Kemp AH, Quintana DS, Felmingham KL, Matthews S, Jelinek HF . Depression, comorbid anxiety disorders, and heart rate variability in physically healthy, unmedicated patients: Implications for cardiovascular risk. PLoS ONE 2012; 7: e30777.
Schwartz S, Susser E . The use of well controls: an unhealthy practice in psychiatric research. Psychol Med 2011; 41: 1127–1131.
Henrich J, Heine SJ, Norenzayan A . Most people are not WEIRD. Nature 2010; 466: 29–29.
Schechter D, Lebovitch R . Normal controls are expensive to find: methods to improve cost-effectiveness of the screening evaluation. Psychiatry Res 2005; 136: 69–78.
Koskinen T, Kähönen M, Jula A, Laitinen T, Keltikangas-Järvinen L, Viikari J et al. Short-term heart rate variability in healthy young adults: the Cardiovascular Risk in Young Finns Study. Auton Neurosci 2009; 145: 81–88.
Saboul D, Pialoux V, Hautier C . The breathing effect of the LF/HF ratio in the heart rate variability measurements of athletes. Eur J Sport Sci 2014; 14: S282–S288.
Rennie KL, Hemingway H, Kumari M, Brunner E, Malik M, Marmot M . Effects of moderate and vigorous physical activity on heart rate variability in a British study of civil servants. Am J Epidemiol 2003; 158: 135–143.
Quintana DS, Guastella AJ, McGregor IS, Hickie IB, Kemp AH . Moderate alcohol intake is related to increased heart rate variability in young adults: Implications for health and well‐being. Psychophysiology 2013; 50: 1202–1208.
Hayano J, Yamada M, Sakakibara Y, Fujinami T, Yokoyama K, Watanabe Y et al. Short-and long-term effects of cigarette smoking on heart rate variability. Am J Cardiol 1990; 65: 84–88.
O'Brien I, O'Hare P, Corrall R . Heart rate variability in healthy subjects: effect of age and the derivation of normal ranges for tests of autonomic function. Br Heart J 1986; 55: 348–354.
Voss A, Heitmann A, Schroeder R, Peters A, Perz S . Short-term heart rate variability—age dependence in healthy subjects. Physiol Meas 2012; 33: 1289.
Kawas C, Gray S, Brookmeyer R, Fozard J, Zonderman A . Age-specific incidence rates of Alzheimer’s disease The Baltimore Longitudinal Study of Aging. Neurology 2000; 54: 2072–2077.
Jousilahti P, Vartiainen E, Tuomilehto J, Puska P . Sex, age, cardiovascular risk factors, and coronary heart disease a prospective follow-up study of 14 786 middle-aged men and women in Finland. Circulation 1999; 99: 1165–1172.
Kostis JB, McCrone K, Moreyra A, Gotzoyannis S, Aglitz M, Natarajan N et al. Premature ventricular complexes in the absence of identifiable heart disease. Circulation 1981; 63: 1351–1356.
Haruta D, Akahoshi M, Hida A, Sera N, Imaizumi M, Ichimaru S et al. Prognostic significance of premature ventricular contractions without obvious heart diseases determined by standard 12‐lead electrocardiography considering their morphology. Ann Noninvasive Electrocardiol 2015; 21: 142–151.
Liao D, Cai J, Barnes RW, Tyroler HA, Rautaharju P, Holme I et al. Association of cardiac automatic function and the development of hypertension the ARIC Study. Am J Hypertens 1996; 9: 1147–1156.
Tsuji H, Larson MG, Venditti FJ, Manders ES, Evans JC, Feldman CL et al. Impact of reduced heart rate variability on risk for cardiac events the Framingham Heart Study. Circulation 1996; 94: 2850–2855.
Huikuri HV, Mäkikallio TH, Peng C-K, Goldberger AL, Hintze U, Møller M . Fractal correlation properties of RR interval dynamics and mortality in patients with depressed left ventricular function after an acute myocardial infarction. Circulation 2000; 101: 47–53.
Koskinen T, Kähönen M, Jula A, Mattsson N, Laitinen T, Keltikangas‐Järvinen L et al. Metabolic syndrome and short‐term heart rate variability in young adults. Diabet Med 2009; 26: 354–361.
Fukuta H, Hayano J, Ishihara S, Sakata S, Mukai S, Ohte N et al. Prognostic value of heart rate variability in patients with end‐stage renal disease on chronic haemodialysis. Nephrol Dial Transplant 2003; 18: 318–325.
Ewing D, Winney R . Autonomic function in patients with chronic renal failure on intermittent haemodialysis. Nephron 1975; 15: 424–429.
Axelrod S, Lishner M, Oz O, Bernheim J, Ravid M . Spectral analysis of fluctuations in heart rate: an objective evaluation of autonomic nervous control in chronic renal failure. Nephron 1987; 45: 202–206.
Niemelä MJ, Airaksinen KJ, Huikuri HV . Effect of beta-blockade on heart rate variability in patients with coronary artery disease. J Am Coll Cardiol 1994; 23: 1370–1377.
Heathers JA . Smartphone-enabled pulse rate variability: an alternative methodology for the collection of heart rate variability in psychophysiological research. Int J Psychophysiol 2013; 89: 297–304.
Poh M-Z, McDuff DJ, Picard RW . Non-contact automated cardiac pulse measurements using video imaging and blind source separation. Opt Express 2010; 18: 10762–10774.
Jezewski J, Roj D, Wrobel J, Horoba K . A novel technique for fetal heart rate estimation from Doppler ultrasound signal. Biomed Eng Online 2011; 10: 92.
Suzuki S, Matsui T, Sugawara K, Asao T, Kotani K . An approach to remote monitoring of heart rate variability (HRV) using microwave radar during a calculation task. J Physiol Anthropol 2011; 30: 241–249.
A smart cushion for real-time heart rate monitoring. Proceedings of the Biomedical Circuits and Systems Conference (BioCAS), IEEE 2012, 28-30 November 2012; Hsinchu, Taiwan; IEEE, 2012.
The electrically noncontacting ECG measurement on the toilet seat using the capacitively-coupled insulated electrodes. Proceedings of the Engineering in Medicine and Biology Society, 2004. IEMBS '04. 26th Annual International Conference of the IEEE 2004, 1-5 September 2004; San Francisco, USA; IEEE, 2004.
Quintana DS, Heathers JAJ, Kemp AH . On the validity of using the Polar RS800 heart rate monitor for heart rate variability research. Eur J Appl Physiol 2012; 112: 4179–4180.
Swan M . The quantified self: Fundamental disruption in big data science and biological discovery. Big Data 2013; 1: 85–99.
Method to filter ECGs and evaluate clinical parameter distortion using realistic ECG model parameter fitting. Proceedings of the Computers in Cardiology, 2005, 25-28 September 2005; Lyon, France; IEEE, 2005.
Riniolo T, Porges SW . Inferential and descriptive influences on measures of respiratory sinus arrhythmia: sampling rate, R‐wave trigger accuracy, and variance estimates. Psychophysiology 1997; 34: 613–621.
Merri M, Farden DC, Mottley JG, Titlebaum EL . Sampling frequency of the electrocardiogram for spectral analysis of the heart rate variability. IEEE Trans Biomed Eng 1990; 37: 99–106.
Fei L, Copie X, Malik M, Camm AJ . Short-and long-term assessment of heart rate variability for risk stratification after acute myocardial infarction. Am J Cardiol 1996; 77: 681–684.
Esco MR, Flatt AA . Ultra-short-term heart rate variability indexes at rest and post-exercise in athletes: evaluating the agreement with accepted recommendations. J Sports Sci Med 2014; 13: 535.
Heathers JA . Everything Hertz: methodological issues in short-term frequency-domain HRV. Front Physiol 2014; 5: 177.
Sijtsema J, Roon VA, Groot F, Riese H . Early life adversities and adolescent antisocial behavior: the role of cardiac autonomic nervous system reactivity in the TRAILS Study. Biol Psychol 2015; 110: 24–33.
Keen L, Turner AD, Mwendwa D, Callender C, Campbell A . Depressive symptomatology and respiratory sinus arrhythmia in a non-clinical sample of middle-aged African Americans. Biol Psychol 2015; 108: 56–61.
Gaebler M, Daniels JK, Lamke J-P, Fydrich T, Walter H . Heart rate variability and its neural correlates during emotional face processing in social anxiety disorder. Biol Psychol 2013; 94: 319–330.
Mukai S, Hayano J . Heart rate and blood pressure variabilities during graded head-up tilt. J Appl Physiol 1995; 78: 212–216.
Stolarz K, Staessen JA, Kuznetsova T, Tikhonoff V, Babeanu S, Casiglia E et al. Host and environmental determinants of heart rate and heart rate variability in four European populations. J Hypertens 2003; 21: 525–535.
Chan H-L, Lin M-A, Chao P-K, Lin C-H . Correlates of the shift in heart rate variability with postures and walking by time–frequency analysis. Comput Methods Programs Biomed 2007; 86: 124–130.
Vlemincx E, Van Diest I, Van den Bergh O . A sigh following sustained attention and mental stress: effects on respiratory variability. Physiol Behav 2012; 107: 1–6.
Quintana DS, Heathers JA . Considerations in the assessment of heart rate variability in biobehavioral research. Front Psychol 2014; 5: 805.
Grant CC, van Rensburg DC, Strydom N, Viljoen M . Importance of tachogram length and period of recording during noninvasive investigation of the autonomic nervous system. Ann Noninvasive Electrocardiol 2011; 16: 131–139.
Montano N, Ruscone TG, Porta A, Lombardi F, Pagani M, Malliani A . Power spectrum analysis of heart rate variability to assess the changes in sympathovagal balance during graded orthostatic tilt. Circulation 1994; 90: 1826–1831.
Vaschillo EG, Vaschillo B, Buckman JF, Nguyen-Louie T, Heiss S, Pandina RJ et al. The effects of sighing on the cardiovascular system. Biol Psychol 2015; 106: 86–95.
Werner GG, Ford BQ, Mauss IB, Schabus M, Blechert J, Wilhelm FH . High cardiac vagal control is related to better subjective and objective sleep quality. Biol Psychol 2015; 106: 79–85.
McGinley JJ, Friedman BH . Autonomic responses to lateralized cold pressor and facial cooling tasks. Psychophysiology 2015; 52: 416–424.
Jennings JR, Kamarck T, Stewart C, Eddy M, Johnson P . Alternate cardiovascular baseline assessment techniques: vanilla or resting baseline. Psychophysiology 1992; 29: 742–750.
Massin MM, Maeyns K, Withofs N, Ravet F, Gérard P . Circadian rhythm of heart rate and heart rate variability. Arch Dis Child 2000; 83: 179–182.
Guo Y-F, Stein PK . Circadian rhythm in the cardiovascular system: considerations in non-invasive electrophysiology. Card Electrophysiol Rev 2002; 6: 267–272.
Yamasaki Y, Kodama M, Matsuhisa M, Kishimoto M, Ozaki H, Tani A et al. Diurnal heart rate variability in healthy subjects: effects of aging and sex difference. Am J Physiol Heart Circ Physiol 1996; 271: H303–H310.
Lu C-L, Zou X, Orr WC, Chen J . Postprandial changes of sympathovagal balance measured by heart rate variability. Dig Dis Sci 1999; 44: 857–861.
Angelone A, Coulter NA . Respiratory sinus arrhythmia: a frequency dependent phenomenon. J Appl Physiol 1964; 19: 479–482.
Hirsch JA, Bishop B . Respiratory sinus arrhythmia in humans: how breathing pattern modulates heart rate. Am J Physiol Heart Circ Physiol 1981; 241: H620–H629.
Brown TE, Beightol LA, Koh J, Eckberg DL . Important influence of respiration on human RR interval power spectra is largely ignored. J Appl Physiol 1993; 75: 2310–2317.
Grossman P, Taylor EW . Toward understanding respiratory sinus arrhythmia: relations to cardiac vagal tone, evolution and biobehavioral functions. Biol Psychol 2007; 74: 263–285.
Denver JW, Reed SF, Porges SW . Methodological issues in the quantification of respiratory sinus arrhythmia. Biol Psychol 2007; 74: 286–294.
Eckberg DL . Point: counterpoint: respiratory sinus arrhythmia is due to a central mechanism vs. respiratory sinus arrhythmia is due to the baroreflex mechanism. J Appl Physiol 2009; 106: 1740–1742.
Saul JP, Berger R, Albrecht P, Stein S, Chen MH, Cohen R . Transfer function analysis of the circulation: unique insights into cardiovascular regulation. Am J Physiol Heart Circ Physiol 1991; 261: H1231–H1245.
Lázaro J, Alcaine A, Romero D, Gil E, Laguna P, Pueyo E et al. Electrocardiogram derived respiratory rate from QRS slopes and R-wave angle. Ann Biomed Eng 2014; 42: 2072–2083.
Sinnecker D, Dommasch M, Barthel P, Müller A, Dirschinger RJ, Hapfelmeier A et al. Assessment of mean respiratory rate from ECG recordings for risk stratification after myocardial infarction. J Electrocardiol 2014; 47: 700–704.
Bailón R, Sörnmo L, Laguna P . A robust method for ECG-based estimation of the respiratory frequency during stress testing. IEEE Trans Biomed Eng 2006; 53: 1273–1285.
Lázaro J, Gil E, Bailón R, Mincholé A, Laguna P . Deriving respiration from photoplethysmographic pulse width. Med Biol Eng Comput 2013; 51: 233–242.
Krygier JR, Heathers JA, Shahrestani S, Abbott M, Gross JJ, Kemp AH . Mindfulness meditation, well-being, and heart rate variability: a preliminary investigation into the impact of intensive Vipassana meditation. Int J Psychophysiol 2013; 89: 305–313.
Oldenburg O, Lamp B, Faber L, Teschler H, Horstkotte D, Töpfer V . Sleep‐disordered breathing in patients with symptomatic heart failure A contemporary study of prevalence in and characteristics of 700 patients. Eur J Heart Fail 2007; 9: 251–257.
Sharafkhaneh A, Giray N, Richardson P, Young T, Hirshkowitz M . Association of psychiatric disorders and sleep apnea in a large cohort. Sleep 2005; 28: 1405.
Wallis L, Healy M, Undy MB, Maconochie I . Age related reference ranges for respiration rate and heart rate from 4 to 16 years. Arch Dis Child 2005; 90: 1117–1121.
Nardi AE, Freire RC, Zin WA . Panic disorder and control of breathing. Respir Physiol Neurobiol 2009; 167: 133–143.
Abelson JL, Weg JG, Nesse RM, Curtis GC . Persistent respiratory irregularity in patients with panic disorder. Biol Psychiatry 2001; 49: 588–595.
Vlemincx E, Abelson JL, Lehrer PM, Davenport PW, Van Diest I, Van den Bergh O . Respiratory variability and sighing: a psychophysiological reset model. Biol Psychol 2013; 93: 24–32.
Monfredi O, Lyashkov AE, Johnsen A-B, Inada S, Schneider H, Wang R et al. Biophysical characterization of the underappreciated and important relationship between heart rate variability and heart rate. Hypertension 2014; 64: 1334–1343.
Sacha J, Pluta W . Alterations of an average heart rate change heart rate variability due to mathematical reasons. Int J Cardiol 2008; 128: 444–447.
Sacha J . Why should one normalize heart rate variability with respect to average heart rate. Front Physiol 2013; 4: 306.
Houtveen JH, Rietveld S, Geus EJ . Contribution of tonic vagal modulation of heart rate, central respiratory drive, respiratory depth, and respiratory frequency to respiratory sinus arrhythmia during mental stress and physical exercise. Psychophysiology 2002; 39: 427–436.
Pan J, Tompkins WJ . A real-time QRS detection algorithm. IEEE Trans Biomed Eng 1985; 3: 230–236.
Clifford GD, Tarassenko L . Quantifying errors in spectral estimates of HRV due to beat replacement and resampling. IEEE Trans Biomed Eng 2005; 52: 630–638.
Clifford GD, Azuaje F, McSharry P . Advanced Methods and Tools for ECG Data Analysis. Artech House Inc: Boston, MA,, 2006.
Maron BJ, Pelliccia A . The heart of trained athletes cardiac remodeling and the risks of sports, including sudden death. Circulation 2006; 114: 1633–1644.
D'Alessandro A, Boeckelmann I, Hammwhöner M, Goette A . Nicotine, cigarette smoking and cardiac arrhythmia: an overview. Eur J Prev Cardiol 2012; 19: 297–305.
Mehta A, Jain A, Mehta M, Billie M . Caffeine and cardiac arrhythmias. An experimental study in dogs with review of literature. Acta Cardiol 1996; 52: 273–283.
Juliano LM, Griffiths RR . A critical review of caffeine withdrawal: empirical validation of symptoms and signs, incidence, severity, and associated features. Psychopharmacology 2004; 176: 1–29.
Berntson GG, Stowell JR . ECG artifacts and heart period variability: don't miss a beat!. Psychophysiology 1998; 35: 127–132.
Pelliccia A, Maron BJ, Culasso F, Di Paolo FM, Spataro A, Biffi A et al. Clinical significance of abnormal electrocardiographic patterns in trained athletes. Circulation 2000; 102: 278–284.
Viitasalo M, Kala R, Eisalo A . Ambulatory electrocardiographic recording in endurance athletes. Br Heart J 1982; 47: 213–220.
Calvert A, Lown B, Gorlin R . Ventricular premature beats and anatomically defined coronary heart disease. Am J Cardiol 1977; 39: 627–634.
Schmidt G, Malik M, Barthel P, Schneider R, Ulm K, Rolnitzky L et al. Heart-rate turbulence after ventricular premature beats as a predictor of mortality after acute myocardial infarction. Lancet 1999; 353: 1390–1396.
Sade E, Aytemir K, Oto A, Nazli N, Özmen F, Özkutlu H et al. Assessment of Heart Rate Turbulence in the Acute Phase of Myocardial Infarction for Long‐Term Prognosis. Pacing Clin Electrophysiol 2003; 26: 544–550.
La Rovere MT, Maestri R, Pinna GD, Sleight P, Febo O . Clinical and haemodynamic correlates of heart rate turbulence as a non-invasive index of baroreflex sensitivity in chronic heart failure. Clin Sci 2011; 121: 279–284.
Stein PK, Le Q, Domitrovich PP . Development of more erratic heart rate patterns is associated with mortality post–myocardial infarction. J Electrocardiol 2008; 41: 110–115.
Stein PK, Le Q, Domitrovich PP, Investigators C. Development of more erratic heart rate patterns is associated with mortality post–myocardial infarction. J Electrocardiol 2008; 41: 110–115.
Wiklund U, Hörnsten R, Karlsson M, Suhr OB, Jensen SM . Abnormal heart rate variability and subtle atrial arrhythmia in patients with familial amyloidotic polyneuropathy. Ann Noninvasive Electrocardiol 2008; 13: 249–256.
Salo MA, Huikuri HV, Seppanen T . Ectopic beats in heart rate variability analysis: effects of editing on time and frequency domain measures. Ann Noninvasive Electrocardiol 2001; 6: 5–17.
Heathers JA, Fink E, Kuhnert RL, de Rosnay M . Blood volume pulse (BVP) derived vagal tone (VT) between 5 and 7 years of age: A methodological investigation of measurement and longitudinal stability. Dev Psychobiol 2014; 56: 23–35.
Peltola MA . Role of editing of R–R interval in the analysis of heart rate variability. Front Physiol 2012; 3: 148.
Bravi A, Longtin A, Seely A . Review and classification of variability analysis techniques with clinical applications. Biomed Eng Online 2011; 10: 90.
Smith A-L, Owen H, Reynolds KJ . Heart rate variability indices for very short-term (30 beat) analysis. Part 1: survey and toolbox. J Clin Monit Comput 2013; 27: 569–576.
Burr RL . Interpretation of normalized spectral heart rate variability indices in sleep research: a critical review. Sleep 2007; 30: 913-919.
Willson K, Francis DP . A direct analytical demonstration of the essential equivalence of detrended fluctuation analysis and spectral analysis of RR interval variability. Physiol Meas 2003; 24: N1-N7.
Hayano J, Sakakibara Y, Yamada A, Yamada M, Mukai S, Fujinami T et al. Accuracy of assessment of cardiac vagal tone by heart rate variability in normal subjects. Am J Cardiol 1991; 67: 199–204.
Lomb NR . Least-squares frequency analysis of unequally spaced data. Astrophys Space Sci 1976; 39: 447–462.
Scargle JD . Studies in astronomical time series analysis. II-Statistical aspects of spectral analysis of unevenly spaced data. Astrophys J 1982; 263: 835–853.
Martin W, Flandrin P . Wigner-Ville spectral analysis of nonstationary processes. IEEE Trans Acoustics Speech Signal Proc 1985; 33: 1461–1470.
Chemla D, Young J, Badilini F, Maison-Blanche P, Affres H, Lecarpentier Y et al. Comparison of fast Fourier transform and autoregressive spectral analysis for the study of heart rate variability in diabetic patients. Int J Cardiol 2005; 104: 307–313.
Cowan MJ, Pike K, Burr RL, Cain KC, Narayanan SB . Description of time-and frequency-domain-based measures of heart rate variability in individuals taking antiarrhythmics, beta blockers, calcium channel blockers, and/or antihypertensive drugs after sudden cardiac arrest. J Electrocardiol 1992; 26: 1–13.
Billman GE . Heart rate variability–a historical perspective. Front Physiol 2011; 2: 86.
Goldstein DS, Bentho O, Park MY, Sharabi Y . Low‐frequency power of heart rate variability is not a measure of cardiac sympathetic tone but may be a measure of modulation of cardiac autonomic outflows by baroreflexes. Exp Physiol 2011; 96: 1255–1261.
Billman GE . The LF/HF ratio does not accurately measure cardiac sympatho-vagal balance. Front Physiology 2013; 4: 26.
Berntson GG, Bigger JT, Eckberg DL, Grossman P, Kaufmann PG, Malik M et al. Heart rate variability: origins, methods, and interpretive caveats. Psychophysiology 1997; 34: 623–648.
Tak LM, Meijer A, Manoharan A, de Jonge P, Rosmalen JG . More than the sum of its parts: meta-analysis and its potential to discover sources of heterogeneity in psychosomatic medicine. Psychosom Med 2010; 72: 253–265.
Ripke S, Wray NR, Lewis CM, Hamilton SP, Weissman MM, Breen G et al. A mega-analysis of genome-wide association studies for major depressive disorder. Mol Psychiatry 2013; 18: 497–511.
Gupta CN, Calhoun VD, Rachakonda S, Chen J, Patel V, Liu J et al. Patterns of gray matter abnormalities in schizophrenia based on an international mega-analysis. Schizophr Bull 2014; 41: 1133–1142, sbu177.
de Wit SJ, Alonso P, Schweren L, Mataix-Cols D, Lochner C, Menchón JM et al. Multicenter voxel-based morphometry mega-analysis of structural brain scans in obsessive-compulsive disorder. Am J Psychiatry 2014.
Hallahan B, Newell J, Soares JC, Brambilla P, Strakowski SM, Fleck DE et al. Structural magnetic resonance imaging in bipolar disorder: an international collaborative mega-analysis of individual adult patient data. Biol Psychiatry 2011; 69: 326–335.
Lewandowsky S, Bishop D . Research integrity: don't let transparency damage science. Nature 2016; 529: 459–461.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Additional information
Supplementary Information accompanies the paper on the Translational Psychiatry website
Supplementary information
Rights and permissions
This work is licensed under a Creative Commons Attribution 4.0 International License. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in the credit line; if the material is not included under the Creative Commons license, users will need to obtain permission from the license holder to reproduce the material. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/
About this article
Cite this article
Quintana, D., Alvares, G. & Heathers, J. Guidelines for Reporting Articles on Psychiatry and Heart rate variability (GRAPH): recommendations to advance research communication. Transl Psychiatry 6, e803 (2016). https://doi.org/10.1038/tp.2016.73
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/tp.2016.73
This article is cited by
-
Short-Term Effects of Heart Rate Variability Biofeedback on Working Memory
Applied Psychophysiology and Biofeedback (2024)
-
Evidence of deviant parasympathetic response to social exclusion in women with borderline personality disorder
European Archives of Psychiatry and Clinical Neuroscience (2024)
-
Effects of stress management interventions on heart rate variability in adults with cardiovascular disease: a systematic review and meta-analysis
Journal of Behavioral Medicine (2024)
-
The impact of traumatic childhood experiences on interoception: disregarding one’s own body
Borderline Personality Disorder and Emotion Dysregulation (2023)
-
Anterior cingulate and medial prefrontal cortex oscillations underlie learning alterations in trait anxiety in humans
Communications Biology (2023)