Abstract
We here present data on immune gene expression of chemokines, chemokine receptors, cytokines and regulatory T-cell (T-reg) markers in chronic patients suffering from either schizophrenia (SCZ, N=20) or bipolar disorder (BD=20) compared with healthy controls (HCs, N=20). We extracted RNA from peripheral blood mononuclear cells and performed real-time (RT)-PCR to measure mRNA levels of chemokines, chemokine receptors, cytokines and T-reg markers. All the analyses were Bonferroni-corrected. The classical monocyte activation (M1) markers il6, ccl3 were significantly increased in BD as compared with both HC and SCZ patients (P=0.03 and P=0.002; P=0.024 and P=0.021, respectively), whereas markers of alternative (M2) monocyte activation ccl1, ccl22 and il10 were coherently decreased (controls: P=0.01, P=0.001 and P=0.09; SCZ subjects: P=0.02, P=0.05 and P=0.011, respectively). Concerning T-cell markers, BD patients had compared with HC downregulated ccr5 (P=0.02) and upregulated il4 (P=0.04) and compared with both healthy and SCZ individuals downregulated ccl2 (P=0.006 and P=0.003) and tgfβ (P=0.004 and P=0.007, respectively). No significant associations were found between any immune gene expression and clinical variables (prior hospitalizations, Brief Psychiatric Rating Scale, medications’ dosages and lifetime administration). Although some markers are expressed by different immune cell types, these findings suggest a coherent increased M1/decrease M2 signature in the peripheral blood of BD patients with potential Th1/Th2 shift. In contrast, all the explored immune marker levels were preserved in SCZ. Further larger studies are needed to investigate the relevance of inflammatory response in BD, trying to correlate it to psychopathology, treatment and outcome measures and, possibly, to brain connectivity.
Similar content being viewed by others
Introduction
The immune system is considered a key factor in brain homeostasis and plasticity.1 Immune response can be achieved by the innate or the adaptive immune response, both of which include the activation of leukocytes. Cytokines represent the signal for communication between leukocytes. Briefly, the innate immune system induces a fast and general immune response and includes cells (that is, monocytes and macrophages) and soluble mediators, whereas the adaptive system is slower but more specific and the main component of it are B and T lymphocytes (the complement system and cytokines; for a detailed description see Sperner-Unterweger2). Cytokines are therefore the key signaling molecules of the immune system and regulators of inflammation.
Inflammation and immunity have been recently proposed as potential components of the etiology of schizophrenia (SCZ) and bipolar disorder (BD).3, 4, 5 Hope et al.6 found no major differences in BD and SCZ patients compared with healthy controls (HCs) except for an increase in the plasma level of soluble TNF-receptor 1 and von Willebrand factor in both types of patients. In contrast, other authors7,8 found only interleukin 1β (IL1β) to be increased in BD, as compared with HC, whereas IL1β, IL-6, tumor necrosis factor α (TNFα) and CCL2 were all increased, as compared with HC, in SCZ patients. Some recent lines of evidence demonstrated the presence of both pro-inflammatory activation of the innate immune system and of the T cells of the adaptive immune system in SCZ and BD,9,10 showing that levels of soluble TNF-receptor 1, IL-1Ra, osteoprogesterin and IL-6 are state-related for BD but not in patients with SCZ. This finding would suggest a different immunological pattern in the two diseases.
Concerning SCZ, a putative role in its etiopathogenesis was already proposed 40 years ago11 and led to the hypothesis of a possible cytokine imbalance. Indeed, some investigations demonstrated alterations in circulating inflammatory cytokine levels in patients with SCZ12,13 and their relatives,14, 15, 16 but other studies had controversial results.17, 18, 19, 20, 21 Recently, a population-based study found IL-1 receptor antagonist to be marker of metabolic comorbidity, rather than of an inflammatory etiology in SCZ.22
Few studies have been conducted in BD that found a lack of T-regulatory (T-reg) cells and an overall inflammatory gene expression 'signature' in the circulating monocytes8,9,23 including PDE4B, IL1B, IL6, TNF, TNFAIP3, PTGS2, PTX3, CCL2, CCL7, CCL20, CXCL2, CCR2 and CDC42. Moreover, acute symptomatology has been associated with higher levels of pro-inflammatory cytokines (IL-1Ra, IL-8, IL-4, C reactive protein, TNF-α and IL-6)13,24, 25, 26, 27 but not in all studies.28,29 There is however a lack of studies exploring BD, and, due to methodology variability and small sample sizes, findings are still controversial. However, recent meta-analyses have confirmed the importance of cytochine alterations in BD.30 In this regards, it should be noted that cytokines and chemokines control both the traffic of immune cells into the central nervous system and the formation of perivenular inflammatory infiltrates, which may lead to demyelination and axonal loss.31,32 Moreover, it has been shown that pro-inflammatory cytokines are associated with cognitive disturbance in humans33 and that, in rodents, T cells are needed for normal cognitive functioning.34 Therefore, an altered immune system may potentially affect brain connectivity, and cognition, having a major role in the pathophysiology of BD.
In order to test the hypothesis of an immunological activation in BD, the objective of the current study was to investigate whether the levels of inflammatory parameters in a sample of chronic BD are different compared with chronic SCZ and HC.
Materials and methods
Participants
Three groups of participants were enrolled in the study. The first group included 20 outpatients with clinical diagnosis of SCZ (14 males, 6 females; mean age=39.75±7.86). The second group was composed of 20 outpatients with BD (7 males, 13 females; mean age=42.45±6.58).
The two groups of patients were selected from the South-Verona Psychiatric Case Register,35 a community-based mental health register that refers to the four Psychiatric Services of Verona. Diagnoses of SCZ and BD were established according to the DSM-IV criteria, using the Structural Clinical Interview for DSM-IV, SCID-I, Italian version36 and subsequently confirmed with the clinical consensus of two staff psychiatrists. Clinical consensus of two staff psychiatrists was also regularly taken into account in order to double-check all the diagnoses, according to the DSM-IV criteria. Patients with other Axis I disorders, alcohol or substance abuse, history of traumatic head injury, neurological or medical diseases and mental retardation were excluded from the study.
Additional exclusion criteria for the patient group were: electroconvulsive therapy during 6 months before the recruitment and treatment with immunomodulatory drugs in the prior 6 months, pregnancy, head injury with loss of consciousness, family history of hereditary neurologic disorder or floating metallic objects in the body. Symptoms at the moment of the assessment (in the same day or within 1 week) were evaluated by administering the Brief Psychiatric Rating Scale37 for SCZ and BD patients, whereas only for the BD group manic or depressive symptoms were characterized by using the Bech–Rafaelsen Mania Rating Scale (BRMRS) and the Hamilton Depression Rating Scale (HAM-D), respectively.38
The third group included 20 HCs (9 males, 11 females; mean age=36.6±7.69) with no DSM-IV Axis I and Axis-II disorders, no history of psychiatric disorders among their first-degree relatives, no history of alcohol or substance abuse, no history of head injury and no current neurological or medical illness, including hypertension and diabetes. The absence of psychiatric disturbances was determined by a brief interview modified from the SCID-IV non-patient version.39 Sociodemographic and clinical data of the three groups are outlined in Table 1. Except for three patients on treatment with clopixol, all patients with SCZ were receiving atypical antipsychotic medications: four olanzapine, four clozapine, four risperidone, three quetiapine, two aripiprazole. Three of them were receiving also haloperidol in combination with the atypical. All BD participants but three were receiving medications at the time of assessment. Specifically, four patients were on atypical neuroleptics (olanzapine), five were on typical neuroleptics (two haloperidol and three clotiapine), four patients were on antidepressant medications (one citalopram, one fluoxetine, one imipramine and one escitalopram); 11 of BD patients were taking one mood stabilizer (one oxcarbamazepine, four lithium, four valproic acid and two lamotrigine).
As for BD, based on the HAM-D, eight had mild depression (HAM-D score between 8 and 17), four had moderate depression (HAM-D score between 18 and 24) and one had severe depression (HAM-D score ⩾25). On the basis of the BRMRS, three BD patients had a hypomania state (BRMRS score between 8 and 24). On the basis of both HAM-D and BRMRS, five patients were euthymic (HAM-D score ⩽7; BRMRS score ⩽7) and two were in a mixed state (HAM-D score >7; BRMRS score >7).
All control participants were recruited in the Hospital/University and in the community areas by word of mouth and through advertisements. Informed consent was obtained from all participants after they had understood the aims and the procedures of the study and the issues involved in study participation. The study was approved by the Ethical Committee of the Azienda Ospedaliera Universitaria Integrata of Verona.
RNA extraction and complementary DNA (cDNA) synthesis
Blood has been collected in PAXgene Blood RNA Tubes (Qiagen, Milano, Italy). RNA has been extracted using PAXgene Blood RNA Kit (Qiagen), according to the manufacturer's protocol. cDNA has been synthesized from 3–5 μg of RNA using a random hexamer-primed kit (Ready-to-go, Amersham Bioscience, Milan, Italy). Blood samples were collected in the morning, and the subjects were asked not to drink coffee or smoke cigarettes before the blood draw.
Real-time PCR
The cDNA from ~100 ng of starting RNA was used for real-time (RT) PCR using Pre-developed Taqman Assay Reagents (Applied Biosystems, Monza, Italy) on an ABI Prism 7700 thermal cycler (Applied Biosystems) according to the manufacturer's protocol. Reactions were performed in 25 μl volume and each reaction contained the FAM-labeled probe and primers for the given target. Human GAPDH was used as the housekeeping gene. Threshold parameters were maintained constant for GAPDH and for each target throughout the study. Relative quantification was obtained using the same reference sample, cDNA from peripheral blood mononuclear cells from a healthy blood donor, in which all targets were amplifiable, throughout the study, and results were expressed as arbitrary units (a.u.), according to the manufacturer's instructions (User Bulletin no. 2, Applied Biosystems). The following mRNAs have been quantified: chemokine (ccl1, ccl2, ccl3, ccl4, ccl5, ccl20, ccl22 and cxcl10), chemokine receptors (ccr3, ccr4, ccr5, ccr6, ccr7 and cxcr5), cytokines (il1α, il1β, il4, il6, il10, il17, ifnγ, tgfβ and tnfα) and T-reg cell markers (CD25/il2ra and foxp3).
Auto-antibodies
On paired serum samples obtained from patients and controls, the clinical laboratory of the San Raffaele Scientific Institute, Laboraf, measured antinuclear antibodies (using indirect immunofluorescence): anti-cardiolipin (IgG and IgM), anti-transglutaminase (IgA and IgG), anti-B2microglubulin, anti-tireoperoxidase and anti-tireoglobulin antibodies (using standard enzyme-linked immunosorbent assay).
Statistics
All statistical analyses were performed using the STATA 13 (College Station, TX, USA). Continuous variables were described as the mean and s.d. or median and range, based on the results of the Shapiro–Wilk test. Categorical variables were described as frequencies and percentages and X2 or Fisher exact test were used to compare distributions. To compare age and body mass index among the three diagnostic groups, analysis of variance was used after verifying the assumptions. To compare GAF score and to explore differences in marker levels, Kruskal–Wallis test was used, as there was no homogeneity of variances. Two group comparisons were made using the Mann–Whitney test. Spearman’s correlation analyses were used to explore possible associations between quantitative variables. Bonferroni’s correction for multiple comparisons was applied to all the analyses.
Results
We measured peripheral blood mononuclear cell mRNA levels of ccl1, ccl2, ccl3, ccl4, ccl5, ccl20, ccl22, cxcl10, ccr3, ccr4, ccr5, ccr6, ccr7, cxcr5, il1α, il1β, il4, il6, il10, il17, ifnγ, tgfβ tnfα, CD25/il2ra and foxp3 in HCs, patients affected by SCZ and in patients affected by BD, trying to group them according to their most likely cell of origin.
M1 and M2 monocyte activation markers
We considered il1α, il1β, il6, ccl3, ccl1, ccl22 and il10 as innate immune cell markers.
The M1 markers il6 and ccl3, but not il1α, and il1β, significantly differed among the three groups (P=0.009 and P=0.007, respectively, Kruskal–Wallis test, Bonferroni-corrected), being higher in BD patients compared with both HC (P=0.03 and P=0.002, respectively) and SCZ patients (P=0.024 and P=0.021, respectively; Mann–Whitney U-test, Bonferroni-corrected; Figures 1a and b).
The M1 markers il6 (a) and ccl3 (b) differed among the three groups (P=0.009 and P=0.007, respectively; Kruskal–Wallis test, Bonferroni-corrected) and were upregulated in bipolar disorder patients (BD) compared with both healthy controls (HCs; P=0.03 and P=0.002, respectively) and schizophrenia patients (SCZ; P=0.024 and P=0.021, respectively; Mann–Whitney U-test, Bonferroni-corrected). The M2 markers ccl1 (c), ccl22 (d) and il10 (e) significantly differed among the groups (P=0.005, P=0.002 and P=0.009, respectively; Kruskal–Wallis test, Bonferroni-corrected) and were downregulated in individuals with BD compared with both HC (P=0.01, P=0.001 and P=0.09, respectively) and SCZ subjects (P=0.02, P=0.05 and P=0.011, respectively; Mann–Whitney U-test, Bonferroni-corrected).
As per the M2 markers, ccl1, ccl22 and il10 significantly differed across the three groups (P=0.005, P=0.002 and P=0.009, respectively; Kruskal–Wallis test, Bonferroni-corrected), being significantly lower in individuals with BD compared with both control (P=0.01, P=0.001 and P=0.09, respectively) and SCZ subjects (P=0.02, P=0.05 and P=0.011, respectively; Mann–Whitney U-test, Bonferroni-corrected) (Figures 1c–e). In contrast, no abnormal values were found in subjects with SCZ for any M1 or M2 markers (P>0.05; Mann–Whitney U-test, Bonferroni-corrected).
In Table 2, a tentative classification of the analyzed immune genes according to the M1/M2 paradigm is reported. However, it should be kept in mind that genes that have been linked to monocyte/macrophage polarization can have important roles in other cell types such as T-helper cells.
Th1, Th2 and T-reg cell markers
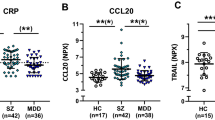
The Th1 chemokine receptor ccr5 significantly differed across the three groups (P=0.015; Kruskal–Wallis test, Bonferroni-corrected), being lower in BD patients compared with HC (P=0.02) but not with SCZ patients (P=0.26; Mann–Whitney U-test, Bonferroni-corrected; Figure 2a). No differences were found for the other putative Th1 markers ccl3 (which is also a M1 marker, as mentioned above), ccl5, ccl20, ifnγ, cxcl10, tnfα across the three groups (P>0.05; Kruskal–Wallis test, Bonferroni-corrected).
The prototypical Th1 cytokine ccr5 (a) significantly differed across the three groups (P=0.015; Kruskal–Wallis test, Bonferroni-corrected) and was downregulated in BD patients compared with HC (P=0.02) but not to SCZ patients (P=0.26; Mann–Whitney U-test, Bonferroni-corrected). The prototypical Th2 cytokine ccl2 (b) and il4 mRNA (c) and the T-regulatory cell marker tgfβ (d) were significantly different among the three groups (P=0.036, P=0.002 and P=0.001, respectively). In particular, BD patients had downregulated ccl2 and tgfβ compared with controls (P=0.006 and P=0.004, respectively) and individuals with SCZ (P=0.003 and P=0.007, respectively) and upregulated il4 compared with HC (P=0.04) but not to SCZ patients (P=0.145; Mann–Whitney U-test, Bonferroni-corrected).
Moreover, the prototypical Th2 cytokine ccl2 and il4 mRNAs were significantly different among the three groups (P=0.036 and P=0.002, respectively; Figures 2b and c), whereas no differences were found for the other Th2 marker mRNA levels including il10 (which is also a M2 marker, as mentioned above), ccl4, ccl11, ccr3, ccr4 (P>0.05; Kruskal–Wallis test, Bonferroni-corrected). In particular, BD patients had significantly lower ccl2 compared with control and SCZ subjects (P=0.006 and P=0.003, respectively) and higher il4 significantly compared with HC (P=0.04) but not to SCZ patients (P=0.145; Mann–Whitney U-test, Bonferroni-corrected).
Finally, the T-reg cell marker tgfβ significantly differed across groups (P=0.001; Kruskal–Wallis test, Bonferroni-corrected) being significantly lower in BD patients compared with both HC and SCZ individuals (P=0.004 and P=0.007, respectively; Mann–Whitney U-test, Bonferroni-corrected; Figure 2d). No significant differences of any other T-reg cells markers, including foxp3, il2ra (CD25), nor of ccr7 mRNAs, across the three groups were found (P>0.05; Kruskal–Wallis test, Bonferroni-corrected).
No significant differences were found between subjects with SCZ and HC for any T-cell markers (P>0.05; Mann–Whitney U-test, Bonferroni-corrected).
Marker correlations
Spearman correlation analyses (Bonferroni-corrected) were conducted among the immunological markers in each group. CD25/il2ra and foxp3 significantly directly correlated in each group (controls: Spearman’s rho=0.739, P<0.001; bipolar patients: Spearman’s rho=0.854, P<0.0001; SCZ patients: Spearman’s rho=0.681, P<0.0001). Moreover, il1a significantly directly associated with cxcl10 in subjects with BD (Spearman’s rho=0.651, P=0.025) and with il1b in those with SCZ (Spearman’s rho=0.611, P=0.043).
Clinical variable impact
Immunological variables did not show any significant association with GAF score and body mass index in the three groups or with number of prior hospitalizations, Brief Psychiatric Rating Scale subscores (anxiety and depression, negative symptoms, positive symptoms and mania) and medications (both dosages and lifetime administration of antipsychotics and mood stabilizers) in BD and SCZ patients (Spearman's correlation analyses, P>0.05, Bonferroni-corrected). In addition, no significant differences were found between smokers and non-smokers for the markers that had different results across the three groups (P>0.05; Mann–Whitney U-test, Bonferroni-corrected).
Anti-cardiolipin IgGs are more frequent among bipolar patients
In light to detect signs of a dis-immune status in BD and SCZ, we measured a small panel of auto-antibodies including antinuclear antibodies, IgG and IgM anti-cardiolipin antibodies, anti-β2 microglobulin antibodies, IgG and IgA anti-transglutaminase antibodies, anti-thyreoglobulin and anti-thyreoperoxidase antibodies. We found no differences among groups for all these autoreactivities but for anti-cardiolipin IgGs, where the only four positive samples were clustered in the group of BD patients (P=0.030; Fisher exact test). Further, all samples have been used to stain mouse cerebellum, a typical procedure used in diagnostic neuroimmunology to detect antineural antigen autoreactivity. No reactivity, however, was detected, neither in HCs nor in patients affected by either BD or SCZ (not shown).
Discussion
We interrogated blood samples from a relatively small but very selected and homogenous cohort of patients affected by major psychoses, either BD or SCZ, to identify an immune-signature in comparison with age and gender-matched healthy individuals. We found a number of myeloid cell markers to be modulated in patients affected by BD as compared with SCZ patients and HCs. Myeloid cells have been recently in the spotlight of innate immunity studies because of their newly discovered ability to have different functional phenotypes. In macrophages, this plasticity has been simplified in two main polarization types: M1 macrophages, regarded as pro-inflammatory, phagocytic, potentially tissue damaging; and M2 macrophages, considered immunomodulatory, tissue remodeling and pro-reparative.40, 41, 42, 43 Macrophages derive from circulating monocytes, and it is not completely clear whether circulating macrophages can be polarized. Nevertheless, we, as many authors in other diseases, found a coherent M1 signature, implying also the decrease of M2 markers, in the peripheral blood of bipolar patients. This is not new: myeloid cell alteration has been already reported in bipolar and psychotic patients. It is interesting that also the first reports on monocyte modulation in depressed patients describe the decrease in beta-2 adrenoceptors,44 and increased phagocytosis,45 phenomena associated today to M1 skewing.40,46 No doubt, however, that the field has been pioneered by Drexhage et al.23 describing a raised number of pro-inflammatory (M1) monocytes in bipolar patients, by several technical means.47, 48, 49 Thus, our study is the first independent confirmation of an M1 signature in monocytes from peripheral blood mononuclear cells of bipolar patients without medical comorbidities and strengthens the case for the identification of a subgroup of BD patients who may benefit by anti-inflammatory therapies. Altered monocyte cytokine profile can be the result of an immune or inflammatory process occurring in the central nervous system. For example, substance P release has been linked to major depression50 and is also well known to activate monocytes.51 On the other hand, a large literature has shown how peripheral pro-inflammatory cytokines induce depression behavior on both experimental conditions and human patients.52 Available data do not indicate whether the M1 shift in monocytes from bipolar patients is cause or consequence of the disease. In the latter case, anti-inflammatory therapeutic strategies would be less relevant. If, however, this monocyte modulation precedes disease onset, it is most likely connected to its etiology, and its therapeutic targeting may be extremely efficacious.
Considering the T-helper markers, the Th1 chemokine receptor ccr5 was downregulated in BD, whereas the prototypical Th2 marker il4 was upregulated in BD, suggesting a Th1/Th2 shift in BD. However, the downregulaton of ccl2, considered a Th2 marker, limits the possibility to fairly discuss this shift. Nonetheless, ccl2 is mostly released by monocytes and might very well be considered in the context of the M1 shift described above, thus leading to a more coherent picture. Future larger studies in BD should further investigate the potential Th1/Th2 shift in BD. Interestingly, as already been described, we also detected a downregulation of tgfβ in BD,53,54 which is considered a potent anti-inflammatory mediator.55 Therefore, reduced tgfβ expression may expose the brain of subjects with BD to an increased susceptibility to neurotoxicity. In contrast, we were not able to confirm alterations in the expression of the major T-regulatory markers (that is, CD25 and foxp3) previously reported.56 However, in this perspective, downregulated tgfβ may cause a functional impairment of these cells, being released by a variety of leukocytes including T-reg cells.
Finally, anti-cardiolipin auto-antibodies were detected only among BD patients. However, relatively low frequency and sample size do not allow definitive conclusions. Nonetheless, it has been reported that anti-phospholipid auto-antibodies, of which anti-cardiolipin auto-antibodies are a subset, are associated with BD.57,58 Therefore, this suggestive finding clearly needs to be confirmed in a larger series of samples.
Some limitations of our study must be taken into account in the interpretation of these results: first, the mean duration of illness, as our patient groups were chronically ill, the cross-sectional design of the study and the relatively small sample size of our population. Second, elevated cytokine levels might also reflect general medical comorbidity and lifestyle-related factors of psychiatric disorders such as smoking, alcohol use and poor physical condition. Smoking was differently present in the three groups, nevertheless all our patients had no medical comorbidities. Third, our study was naturalistic and most of patients were receiving psychotropic drugs, the majority was on atypical antipsychotics. These medications are thought not to induce but rather correct the abnormal inflammatory set-point of patient monocytes.59,60 Regarding BD, half of them were treated also with mood stabilizers, four of them were on lithium, considered in general to be anti-inflammatory.61 Thus, we cannot rule out that some of the findings may have been influenced by medications.
Future larger studies should further investigate the relevance of M1/M2 and potential Th1/Th2 signature in BD, trying to correlate it to episode type, treatment and outcome measures and, possibly, to brain connectivity.
References
Schwartz M, Kipnis J . A conceptual revolution in the relationships between the brain and immunity. Brain Behav Immun 2011; 25: 817–819.
Sperner-Unterweger B . Immunological aetiology of major psychiatric disorders: evidence and therapeutic implications. Drugs 2005; 65: 1493–1520.
Hanson DR, Gottesman II . Theories of schizophrenia: a genetic-inflammatory-vascular synthesis. BMC Med Genet 2005; 11: 6–7.
Nunes SO, Matsuo T, Kaminami MS, Watanabe MA, Reiche EM, Itano EN . An autoimmune or an inflammatory process in patients with schizophrenia, schizoaffective disorder, and in their biological relatives. Schizophr Res 2006; 84: 180–182.
Drexhage RC, Knijff EM, Padmos RC, Heul-Nieuwenhuijzen L, Beumer W, Versnel MA et al. The mononuclear phagocyte system and its cytokine inflammatory networks in schizophrenia and bipolar disorder. Expert Rev Neurother 2010; 10: 59–76.
Hope S, Melle I, Aukrust P, Steen NE, Birkenaes AB, Lorentzen S et al. Similar immune profile in bipolar disorder and schizophrenia: selective increase in soluble tumor necrosis factor receptor I and von Willebrand factor. Bipolar Disord 2009; 11: 726–734.
Drexhage RC, Padmos RC, de Wit H, Versnel MA, Hooijkaas H, van der Lely AJ et al. Patients with schizophrenia show raised serum levels of the pro-inflammatory chemokine CCL2: association with the metabolic syndrome in patients? Schizophr Res 2008; 102: 352–355.
Padmos RC, Hillegers MHJ, Knijff EM, Vonk R, Bouvy A, Staal FJT et al. A discriminating messenger RNA signature for bipolar disorder formed by an aberrant expression of inflammatory genes in monocytes. Arch Gen Psychiatry 2008; 65: 395–407.
Drexhage RC, van der Heul-Nieuwenhuijsen L, Padmos RC, van Beveren N, Cohen D, Versnel MA et al. Inflammatory gene expression in monocytes of patients with schizophrenia: overlap and difference with bipolar disorder. A study in naturalistically treated patients. Int J Neuropsychopharmacol 2010; 13: 1369–1381.
Hope S, Dieset I, Agartz I, Steen NE, Ueland T, Melle I et al. Affective symptoms are associated with markers of inflammation and immune activation in bipolar disorders but not in schizophrenia. J Psychiatr Res 2011; 45: 1608–1616.
Heath RG, Krupp IM . Schizophrenia as an immunologic disorder. I. Demonstration of antibrain globulins by fluorescent antibody techniques. Arch Gen Psychiatry 1967; 16: 1–9.
Potvin S, Stip E, Sepehry AA, Gendron A, Bah R, Kouassi E .2008 Inflammatory cytokine alterations in schizophrenia: a systematic quantitative review. Biol Psychiatry 63: 801–808.
Brietzke E, Kauer-Sant'Anna M, Teixeira AL, Kapczinski F . Abnormalities in serum chemokine levels in euthymic patients with bipolar disorder. Brain Behav Immun 2009; 23: 1079–1082.
Garver DL, Tamas RL, Holcomb JA . Elevated interleukin-6 in the cerebrospinal fluid of a previously delineated schizophrenia subtype. Neuropsychopharmacology 2003; 28: 1515–1520.
Van Kammen DP, McAllister-Sistilli CG, Kelley ME, Gurklis JA, Yao JK . Elevated interleukin-6 in schizophrenia. Psychiatry Res 1999; 87: 129–136.
Miller BJ, Buckley P, Seabolt W, Mellor A, Kirkpatrick B . Meta-analysis of cytokine alterations in schizophrenia: clinical status and antipsychotic effects. Biol Psychiatry 2011; 70: 663–671.
O Brien SM, Scully P, Dinan TG . Increased tumor necrosis factor-alpha concentrations with interleukin-4 concentrations in exacerbations of schizophrenia. Psychiatry Res 2008; 160: 256–262.
Coelho FM, Reis HJ, Nicolato R, Romano-Silva MA, Teixeira MM, Bauer ME et al. Increased serum levels of inflammatory markers in chronic institutionalized patients with schizophrenia. Neuroimmunomodulation 2008; 15: 140–144.
Laske C, Zank M, Klein R, Stransky E, Batra A, Buchkremer G et al. Autoantibody reactivity in serum of patients with major depression, schizophrenia and healthy controls. Psychiatry Res 2008; 158: 83–86.
Yolken RH, Torrey EF . Are some cases of psychosis caused by microbial agents? A review of the evidence. Mol Psychiatry 2008; 13: 470–479.
Kim YK, Suh IB, Kim H, Han CS, Lim CS, Choi SH et al. The plasma levels of interleukin-12 in schizophrenia, major depression, and bipolar mania: effects of psychotropic drugs. Mol Psychiatry 2002; 7: 1107–1114.
Suvisaari J, Loo BM, Saarni SE, Haukka J, Perälä J, Saarni SI et al. Inflammation in psychotic disorders: a population-based study. Psychiatry Res 2011; 189: 305–311.
Drexhage RC, Hoogenboezem TH, Versnel MA, Berghout A, Nolen WA, Drexhage HA . The activation of monocyte and T cell networks in patients with bipolar disorder. Brain Behav Immun 2011; 25: 1206–1213.
Liu HC, Yang YY, Chou YM, Chen KP, Shen WW, Leu SJ . Immunologic variables in acute mania of bipolar disorder. J Neuroimmunol 2004; 150: 116–122.
Kim YK, Jung HG, Myint AM, Kim H, Park SH . Imbalance between pro-inflammatory and anti-inflammatory cytokines in bipolar disorder. J Affect Disord 2007; 104: 91–95.
O'Brien SM, Scully P, Scott LV, Dinan TG . Cytokine profiles in bipolar affective disorder: focus on acutely ill patients. J Affect Disord 2006; 90: 263–267.
De Berardis D, Conti CM, Campanella D, Carano A, Scali M, Valchera A et al. Evaluation of C-reactive protein and total serum cholesterol in adult patients with bipolar disorder. Int J Immunopathol Pharmacol 2008; 21: 319–324.
Dickerson F, Stallings C, Origoni A, Boronow J, Yolken R . C-reactive protein is associated with the severity of cognitive impairment but not of psychiatric symptoms in individuals with schizophrenia. Schizophr Res. 2007; 93: 261–265.
Ortiz-Domínguez A, Hernández ME, Berlanga C, Gutiérrez-Mora D, Moreno J, Heinze G et al. Immune variations in bipolar disorder: phasic differences. Bipolar Disord 2007; 9: 596–602.
Modabbernia A, Taslimi S, Brietzke E, Ashrafi M . Cytokine alterations in bipolar disorder: a meta-analysis of 30 studies. Biol Psychiatry 2013; 74: 15–25.
Ransohoff RM, Kivisakk P, Kidd G . Three or more routes for leukocyte migration into the central nervous system. Nat Rev Immunol 2003; 3: 569–581.
Bar-Or A, Nuttall RK, Duddy M, Alter A, Kim HJ, Ifergan I et al. Analyses of all matrix metalloproteinase members in leukocytes emphasize monocytes as major inflammatory mediators in multiple sclerosis. Brain 2003; 126: 2738–2749.
Reichenberg A, Yirmiya R, Schuld A, Kraus T, Haack M, Morag A et al. Cytokine-associated emotional and cognitive disturbances in humans. Arch Gen Psychiatry 2001; 58: 445–452.
Kipnis J, Cohen H, Cardon M, Ziv Y, Schwartz M . T cell deficiency leads to cognitive dysfunction: implications for therapeutic vaccination for schizophrenia and other psychiatric conditions. Proc Natl Acad Sci USA 2004; 101: 8180–8185.
Amaddeo F, Tansella M . Information systems for mental health. Epidemiol Psichiatr Soc 2009; 18: 1–4.
Mazzi F Morosini P De Girolamo G Bussetti M Guaradi G . SCID-I, Structured Clinical Interview for DSM-IV-Axis I Disorder. Firenze: Organizzazioni Speciali, 2000.
Overall JE, Gorham DR . The Brief Psychiatric Rating Scale. Psychol Rep 1962; 10: 799–812.
Bech P, Bolwig TD, Kramp P, Rafaelsen OJ . The Bech-Rafaelsen mania scale and the Hamilton depression scale. Acta Psychiatr Scand 1979; 59: 420–430.
First MB, Spitzer RL, Gibbon M, Williams JBW . Structured Clinical Interview for DSM-IV-TR Axis I Disorders, Research Version, Non-patient Edition. (SCID-I/NP). Biometrics Research, New York State Psychiatric Institute: New York, NY, USA, 2002.
Mantovani A, Sica A, Locati M . Macrophage polarization comes of age. Immunity 2005; 23: 344–346.
Mantovani A, Sica A, Sozzani S, Allavena P, Vecchi A, Locati M . The chemokine system in diverse forms of macrophage activation and polarization. Trends Immunol 2004; 25: 677–686.
Porta C, Rimoldi M, Raes G, Brys L, Ghezzi P, Di Liberto D et al. Tolerance and M2 (alternative) macrophage polarization are related processes orchestrated by p50 nuclear factor kappaB. Proc Natl Acad Sci USA 2009; 14: 978–983.
Sironi M, Martinez FO, D'Ambrosio D, Gattorno M, Polentarutti N, Locati M et al. Differential regulation of chemokine production by Fcgamma receptor engagement in human monocytes: association of CCL1 with a distinct form of M2 monocyte activation (M2b, Type 2). J Leukoc Biol 2006; 80: 342–349.
Jeanningros R, Mazzola P, Azorin JM, Samuelian-Massa C, Tissot R . Beta-adrenoceptor density of intact mononuclear leukocytes in subgroups of depressive disorders. Biol Psychiatry 1991; 29: 789–798.
McAdams C, Leonard BE . Neutrophil and monocyte phagocytosis in depressed patients. Prog Neuropsychopharmacol Biol Psychiatry 1993; 17: 971–984.
Kobayashi M, Jeschke MG, Asai A, Kogiso M, Yoshida S, Herndon DN et al. Propranolol as a modulator of M2b monocytes in severely burned patients. J Leukoc Biol 2011; 89: 797–803.
Knijff EM, Breunis MN, Kupka RW, de Wit HJ, Ruwhof C, Akkerhuis GW et al. An imbalance in the production of IL-1beta and IL-6 by monocytes of bipolar patients: restoration by lithium treatment. Bipolar Disord 2007; 9: 743–753.
Kupka RW, Breunis MN, Knijff E, Ruwhof C, Nolen WA, Drexhage HA . Immune activation, steroid resistancy and bipolar disorder. Bipolar Disord 2002: 73–74.
Weigelt K, Carvalho LA, Drexhage RC, Wijkhuijs A, Hd Wit, van Beveren NJM et al. TREM-1 and DAP12 expression in monocytes of patients with severe psychiatric disorders. EGR3, ATF3 and PU.1 as important transcription factors. Brain Behav Immun 2011; 25: 1162–1169.
Bondy B, Baghai TC, Minov C, Schüle C, Schwarz MJ, Zwanzger P et al. Substance P serum levels are increased in major depression: preliminary results. Biol Psychiatry 2003; 53: 538–542.
Khan MM, Douglas SD, Benton TD . Substance P-neurokinin-1 receptor interaction upregulates monocyte tissue factor. J Neuroimmunol 2012; 242: 1–8.
Felger JC, Lotrich FE . Inflammatory cytokines in depression: neurobiological mechanisms and therapeutic implications. Neuroscience 2013; 246C: 199–229.
Kim YK, Myint AM, Lee BH, Han CS, Lee SW, Leonard BE et al. T-helper types 1, 2, and 3 cytokine interactions in symptomatic manic patients. Psychiatry Res 2004; 129: 267–272.
Bezchlibnyk YB, Wang JF, McQueen GM, Young LT . Gene expression differences in bipolar disorder revealed by cDNA array analysis of post-mortem frontal cortex. J Neurochem 2001; 79: 826–834.
Stevens DB, Gould KE, Swanborg RH . Transforming growth factor-beta 1 inhibits tumor necrosis factor-alpha/lymphotoxin production and adoptive transfer of disease by effector cells of autoimmune encephalomyelitis. J Neuroimmunol 1994; 51: 77–83.
do Prado CH, Rizzo LB, Wieck A, Lopes RP, Teixeira AL, Grassi-Oliveira R et al. Reduced regulatory T cells are associated with higher levels of Th1/TH17 cytokines and activated MAPK in type 1 bipolar disorder. Psychoneuroendocrinology 2013; 38: 667–676.
Sokol DK, O'Brien RS, Wagenknecht DR, Rao T, McIntyre JA . Antiphospholipid antibodies in blood and cerebrospinal fluids of patients with psychosis. J Neuroimmunol 2007; 190: 151–156.
Sidhom O, Laadhar L, Zitouni M, Ben Alaya N, Rafrafi R, Kallel-Sellami M et al. Spectrum of autoantibodies in Tunisian psychiatric inpatients. Immunol Invest 2012; 41: 538–549.
Drzyzga L, Obuchowicz E, Marcinowska A, Herman ZS . Cytokines in schizophrenia and the effects of antipsychotic drugs. Brain Behav Immun 2006; 20: 532–545.
Pollmächer T, Haack M, Schuld A, Kraus T, Hinze-Selch D . Effects of antipsychotic drugs on cytokine networks. J Psychiatr Res 2000; 34: 369–382.
Rybakowski JK . Antiviral and immunomodulatory effect of lithium. Pharmacopsychiatry 2000; 33: 159–164.
Kitade H, Sawamoto K, Nagashimada M, Inoue H, Yamamoto Y, Sai Y et al. CCR5 plays a critical role in obesity-induced adipose tissue inflammation and insulin resistance by regulating both macrophage recruitment and M1/M2 status. Diabetes 2012; 61: 1680–1690.
Mantovani A, Sozzani S, Locati M, Allavena P, Sica A . Macrophage polarization: tumor-associated macrophages as a paradigm for polarized M2 mononuclear phagocytes. Trends Immunol 2002; 23: 549–555.
Sironi M, Martinez FO, D'Ambrosio D, Gattorno M, Polentarutti N, Locati M et al. Differential regulation of chemokine production by Fcgamma receptor engagement in human monocytes: association of CCL1 with a distinct form of M2 monocyte activation (M2b, Type 2). J Leukoc Biol 2006; 80: 342–349.
Sun L, Louie MC, Vannella KM, Wilke CA, LeVine AM, Moore BB et al. New concepts of IL-10-induced lung fibrosis: fibrocyte recruitment and M2 activation in a CCL2/CCR2 axis. Am J Physiol Lung Cell Mol Physiol 2011; 300: L341–L353.
Waddell A, Ahrens R, Steinbrecher K, Donovan B, Rothenberg ME, Munitz A et al. Colonic eosinophilic inflammation in experimental colitis is mediated by Ly6C(high) CCR2(+) inflammatory monocyte/macrophage-derived CCL11. J Immunol 2011; 186: 5993–6003.
Acknowledgements
This study was partially supported by grants from the Italian Ministry of Health to Dr Paolo Brambilla (GR-2010-2316745) and to Dr Marcella Bellani (GR-2010-2319022) and by a grant from Fondazione Cariverona (Sotto-obiettivo A9 ‘Disabilità cognitiva e comportamentale nelle demenze e nelle psicosi’) to Dr Brambilla. We thank, for the precious help in collecting the blood sample, Professor GC Guidi and his laboratory staff, Sezione di Chimica Clinica, Dipartimento di Scienze della Vita e della Riproduzione, University of Verona, Verona, Italy. We are grateful to Professor P Brown and L Muzio for helpful discussion.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
This work is licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 3.0 Unported License. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in the credit line; if the material is not included under the Creative Commons license, users will need to obtain permission from the license holder to reproduce the material. To view a copy of this license, visit http://creativecommons.org/licenses/by-nc-sa/3.0/
About this article
Cite this article
Brambilla, P., Bellani, M., Isola, M. et al. Increased M1/decreased M2 signature and signs of Th1/Th2 shift in chronic patients with bipolar disorder, but not in those with schizophrenia. Transl Psychiatry 4, e406 (2014). https://doi.org/10.1038/tp.2014.46
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/tp.2014.46
This article is cited by
-
Abelson Helper Integration Site 1 haplotypes and peripheral blood expression associates with lithium response and immunomodulation in bipolar patients
Psychopharmacology (2024)
-
T cells: an emerging cast of roles in bipolar disorder
Translational Psychiatry (2023)
-
Evidence of innate immune dysfunction in first-episode psychosis patients with accompanying mood disorder
Journal of Neuroinflammation (2022)
-
A unified model of the pathophysiology of bipolar disorder
Molecular Psychiatry (2022)
-
Toll-like receptor 4 methylation grade is linked to depressive symptom severity
Translational Psychiatry (2021)