Abstract
ABT-384 is a potent, selective inhibitor of 11-beta-hydroxysteroid dehydrogenase type 1 (HSD-1). One milligram of ABT-384 daily fully inhibited hepatic HSD-1. Establishing the dose that fully inhibits central nervous system (CNS) HSD-1 would enable definitive clinical studies in potential CNS indications. [9,11,12,12-2H4] cortisol (D4 cortisol), a stable labeled tracer, was used to characterize HSD-1 inhibition by ABT-384. D4 cortisol and its products were measured in the plasma and cerebrospinal fluid (CSF) of healthy male volunteers during D4 cortisol infusions, for up to 40 h after five daily doses of 1–50 mg ABT-384. Similar procedures were conducted in control subjects who received no ABT-384. Peripheral HSD-1 inhibition was calculated from plasma levels of D4 cortisol and its products. CNS HSD-1 inhibition was characterized from plasma and CSF levels of D4 cortisol and its products. ABT-384 regimens ⩾2 mg daily maintained peripheral HSD-1 inhibition ⩾88%. ABT-384 1 mg daily maintained peripheral HSD-1 inhibition ⩾81%. No CNS formation of D3 cortisol (the mass-labeled product of HSD-1) was detected following ABT-384 ⩾2 mg daily, indicating full CNS HSD-1 inhibition by these regimens. Partial CNS HSD-1 inhibition was associated with 1 mg ABT-384 daily. CNS HSD-1 inhibition was characterized by strong hysteresis and increased with maximum post-dose plasma concentration of ABT-384 and its active metabolites. ABT-384 has a wide potential therapeutic window for potential indications including Alzheimer’s disease and major depressive disorder. Stable labeled substrates may be viable tools for measuring CNS effect during new drug development for other enzyme targets.
Similar content being viewed by others
Introduction
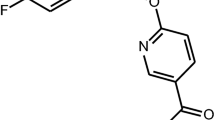
ABT-384 is a potent and selective inhibitor of 11-beta-hydroxysteroid dehydrogenase type 1 (HSD-1).1 HSD-1 converts inactive cortisone to active cortisol in glucocorticoid-dependent tissues including the liver, fat, brain (including multiple regions implicated in cognition and mood regulation), bone and eye.2 Major pathways of ABT-384 catabolism are hydrolysis of the adamantane-1-carboxylic acid amide to form a carboxylic acid metabolite and oxidative metabolism of the piperazine ring. The major acid and oxidative metabolites are also potent and selective HSD-1 inhibitors (Supplementary Figure 1).
A range of medical conditions including Cushing’s syndrome, obesity, insulin resistance, hypertension, dyslipidemia, major depressive disorder, Alzheimer’s disease, osteoporosis and glaucoma have been associated with excess levels of the stress hormone cortisol. An HSD-1 inhibitor, by blocking local tissue regeneration of cortisol, may have therapeutic potential for any of these diseases.2 We have demonstrated ABT-384 safety for regimens up to 100 mg daily in healthy volunteers and elderly subjects, and full hepatic HSD-1 inhibition with ABT-384 regimens from 1 mg daily.1 As potential indications include major depressive disorder and Alzheimer’s disease, we developed a method to measure HSD-1 inhibition in the central nervous system (CNS) in man following the administration of an HSD-1 inhibitor.
[9,11,12,12-2H4] cortisol (D4 cortisol)3 has been used as a stable labeled tracer to measure peripheral HSD-1 activity and characterize the contribution of HSD-1 to circulating cortisol levels (Figure 1).4, 5, 6, 7, 8, 9 HSD-2 inactivates cortisol to cortisone in mineralocorticoid-sensitive tissues such as the kidney and intestine.10 When it acts on D4 cortisol, HSD-2 removes a deuteron leading to the formation of [9,12,12-2H3] cortisone (D3 cortisone). As deuterated water is rare in vivo, the product of HSD-1 acting on D3 cortisone is [9,12,12-2H3] cortisol (D3 cortisol). D3 cortisol is uniquely formed by the action of HSD-1 on D3 cortisone, and thus has been used as a biomarker of HSD-1 activity. D3 cortisol formed by HSD-1 can be converted to D3 cortisone by the action of HSD-2.
Continuous cerebrospinal fluid (CSF) sample collection techniques have enabled the measurement of drug levels and biomarkers that reflect CNS drug action over extended time intervals, similarly as intravenous catheterization has long enabled measurements that reflect peripheral drug action over time. This procedure has been demonstrated to be safe and tolerable.11 Following multiple daily ABT-384 doses and during D4 cortisol infusions, D4 cortisol, D3 cortisone and D3 cortisol levels were measured in the plasma and CSF during intervals of up to 48 h. The goals of this clinical study were to demonstrate ABT-384 target engagement (HSD-1 inhibition) simultaneously in the CNS and the periphery, and to characterize the relationship between plasma drug levels and CNS target engagement for ABT-384.
Materials/subjects and methods
Clinical study
Institutional review board approval for the protocol, informed consent and subject information and advertising was obtained. Any amendments to the protocol were approved by the institutional review board before implementation of any changes to the study design. Written informed consent was obtained from all participating subjects. The clinicaltrials.gov identifier is NCT01009216.
Adult male subjects between 18 and 55 years of age, in general good health (on the basis of medical history, physical examination, brief neurological examination, 12-lead electrocardiogram, vital signs, clinical chemistry tests, hematology tests, urinalysis, hepatitis/HIV tests and drug/alcohol screens) and not using any medication (including over-the-counter, vitamins and herbal supplements) were eligible for the study. Patients with a history of seizures or convulsions, including febrile, alcohol or drug withdrawal seizures, complicated migraines, head injury other than mild (mild defined as unconsciousness or amnesia alone or in combination lasting less than 1 h and occurring at least 1 year before study screening with no residual dysfunction or complication) or CNS infection, including meningitis and encephalitis, were excluded. Patients with a history of cancer (except basal cell carcinoma of the skin) or any clinically significant cardiovascular, respiratory (except mild asthma), renal, hepatic, gastrointestinal, hematologic, neurologic or psychiatric disease or disorder, as well as with a history of gastric surgery, cholecystectomy, vagotomy, bowel resection or any surgical procedure that might interfere with gastrointestinal motility, pH or absorption, were also excluded. Safety and tolerability of the ABT-384 doses were assessed throughout the study by adverse event collection, physical examination, brief neurological examination, 12-lead electrocardiogram, vital signs including orthostatic blood pressure and pulse, and clinical chemistry tests, hematology tests, urinalysis and drug/alcohol screens. Adverse events were recorded until 30 days after the last dose of the study drug.
This was an open-label study of multiple doses of ABT-384 conducted at a single site (PAREXEL International, Glendale, CA, USA). Subjects were confined to the study site starting on Day-1 (one day before the first ABT-384 dose) until at least 48 h after removal of the CSF catheter. Methods used for CSF collection have been described.12
Two subjects were administered 50 mg ABT-384 quaque die (QD) for 5 days (Supplementary Figure 2, Part I). On Day 5, catheters for blood and CSF collection were inserted until 24 h after the last ABT-384 dose. Blood and CSF samples for the measurement of ABT-384 and metabolites were obtained before dosing, at 30-min intervals for 8 h, and at 9, 12, 16 and 24 h post dose. Additional blood samples were obtained at 36, 40 and 48 h post dose. The purpose of this portion of the study was to provide an estimate of ABT-384 CSF exposures to guide dosing for the remaining subjects.
Eight subjects were administered ABT-384 doses daily for 5 days, and also received two primed continuous infusions of D4 cortisol (manufactured by Isotech, Miamisburg, OH, USA; prepared for use by McGuff Compounding Pharmacy Services, Santa Ana, CA, USA). Each D4 cortisol infusion included a 1.76 mg bolus, followed by 0.88 mg h−1 for 8 h (Supplementary Figure 2, Parts II and III). Two subjects each received 1, 2 or 50 mg ABT-384 QD. One subject received 10 mg ABT-384 QD. One subject received 50 mg ABT-384 on Days 1 and 2 and 10 mg ABT-384 on Days 3 through to 5. For analyses by dose, this subject was analyzed together with the subject who received 10 mg ABT-384 QD. On Day 5, catheters for blood and CSF collection were inserted until 48 h after the last ABT-384 dose. Venous catheters for blood sampling were placed upstream of, or contralateral to, a catheter used for D4 cortisol infusion. The first D4 cortisol infusion started at the same time as the last ABT-384 dose and the other ∼22 (for those subjects who received 10 or 50 mg ABT-384 QD) or 32 h (for those subjects who received 1 or 2 mg ABT-384 QD) post dose. Blood and CSF samples for the measurement of ABT-384 and metabolites, D4 cortisol, D3 cortisone, D3 cortisol, cortisol and cortisone were obtained before dosing, at 60-min intervals during each D4 cortisol infusion, and at 9, 12, 16, 36, 40 and 48 h post dose (for those subjects who received 10 or 50 mg ABT-384 QD) or at 10, 14, 24, 42, 44 and 48 h post dose (for those subjects who received 1 or 2 mg ABT-384 QD). Adrenocorticotropic hormone and cortisol-binding globulin were also measured in some blood samples. Additional blood samples for the measurement of ABT-384 and metabolites were obtained at 72 and 96 h post dose. Urine samples for the measurement of cortisol metabolites were collected on Day 1 before dosing and on Days 5 and 6 twice during each D4 cortisol infusion.
Two subjects were not administered ABT-384 (Supplementary Figure 2, Part IV), but received a primed continuous infusion of D4 cortisol (1.76 mg bolus and 0.88 mg h−1 for 4 h). On the day of infusion, catheters for blood and CSF collection were inserted until 8 h after the start of the infusion. Venous catheters for blood sampling were placed upstream of, or contralateral to, a catheter used for D4 cortisol infusion. Blood and CSF samples for the measurement of D4 cortisol, D3 cortisone, D3 cortisol, cortisol and cortisone were obtained before dosing and at 60-minute intervals for 8 h. No placebo for ABT-384 was administered as it was not considered that placebo could alter D4 cortisol metabolism.
Bioanalysis
D4 cortisol was purchased from Isotech and formulated for human use by McGuff Compounding Pharmacy Services. The chemical purity was 97.9% and the isotopic purity was 98.3%. The infusion solution had a D4 cortisol concentration of ∼0.044 mg ml−1 in sterile isotonic saline and ∼3% ethyl alcohol United States Pharmacopeia.
Mass spectrometric assays for D4 cortisol, D3 cortisone, D3 cortisol, cortisol and cortisone were developed and conducted by Prevalere Life Sciences (Whitesboro, NY, USA). D7 cortisone (Sigma-Aldrich, St Louis, MO, USA) was used as an internal standard. D3 cortisone was quantified by interpolation against cortisone standard curves, because a D3 cortisone standard was not available. Reference standards for cortisol and cortisone were obtained from Toronto Research Chemicals (Toronto, ON, Canada), and for D3 cortisol and D4 cortisol from Cambridge Isotope Laboratories (Andover, MA, USA).
Samples (100 μl plasma or 250 μl CSF) were extracted with methyl tert-butyl ether and reconstituted in 200 μl (plasma) or 150 μl (CSF) 1:1 (v:v) methanol:water. A volume of 5 μl (plasma) or 10 μl (CSF) of each sample was applied to the liquid chromatography-mass spectrometry system using a Shimadzu SIL-20AC autosampler (Columbia, MD, USA). Sample matrix cleanup was done with a Phenomenex KrudKatcher Ultra in-line filter (Torrance, CA, USA). HPLC separation was performed on a Phenomenex Kinetix C18, 2.6 μm, 3.00 mm × 100 mm analytical column, with a mobile phase of 5 mM ammonium acetate with methanol. The flow rate was 0.250 ml min−1. Detection was achieved on a PE Sciex API 5000 mass spectrometer (Framingham, MA, USA). Ionization was by positive ion turboionspray with a spray voltage of 5500, declustering potential of 60 eV, entrance potential of 10 eV, collision energy of 35 eV and collision cell exit potential of 30 eV. The tandem mass spectrometry analysis was operated in the MRM mode with high resolution in the first quadrupole and unit resolution in the third quadrupole. Transitions were m/z 363→121, 366→121, 367→121, 361→163, 364→164 and 368→169 for cortisol, D3 cortisol, D4 cortisol, cortisone, D3 cortisone and D4 cortisone, respectively.
During method development, the impact of isotopic contribution from one analyte to others was assessed using solutions of each at 250 ng/ml in 1:1 (v:v) methanol:water. The cortisol mass+3 signal was 0.164%. The D3 cortisol mass+1 signal was 15.6%. The cortisone mass+3 signal was 0.173%. Observed impurities in each of the standards as well as naturally occurring isotopic contribution made it impossible to discern the exact isotopic contribution of any one standard to another. In addition, based on the relative abundances in the clinical trial samples, the potential differences between corrected and uncorrected values were small. In particular, D4 cortisol levels during infusions were generally at least 10-fold higher than D3 cortisol levels, such that the interference from D3 cortisol could not meaningfully alter study results. Therefore, a correction for the isotopic contribution of one analyte to another was not needed.
ABT-384 and its acid metabolite were measured in plasma using validated methods.1
The following changes from the plasma method1 were validated for analysis of M1 in plasma. ABT-510 was used as the internal standard (IS) for M1. Sample matrix cleanup was performed using online solid-phase extraction with a Waters Xbridge C18, 3.5 μm, 2.1 × 10 mm column (Milford MA). The analytical column was the same as described previously, with a mobile phase of 30:70 (v:v) acetonitrile:water with 0.5% acetic acid and 2 mM ammonium acetate. Detection of the analytes was achieved with the Thermo Fisher Scientific TSQ Quantum Ultra mass spectrometer (San Jose CA). Ionization was by positive ion electrospray with a spray voltage of 4000 and source collisionally induced dissociation of 18 eV. The tandem mass spectrometry analysis was operated in the selected reaction monitoring mode with a peak width of 0.2 amu in the first quadrupole and 0.7 amu in the third quadrupole. The collision energy for fragmentation was set at 38 eV. The nominal selected reaction monitoring transitions were m/z 468→189 and 994→270 for the M1 metabolite and the IS. Reference standard for the M1 metabolite was synthesized by Anthem Biosciences Pvt. Ltd. (Bangalore, India), and the IS by AbbVie, North Chicago, IL, USA.
The following changes from the plasma method1 were validated for the analysis of ABT-384 and its acid metabolite in CSF. Sample preparation involved the addition of stable label D6 IS for both ABT-384 and the metabolite to the CSF samples. The samples were injected for HPLC separation directly without using online solid-phase extraction. The HPLC separation used the same analytical column as described for the plasma method. The mobile phase for the CSF method was 2 mM ammonium acetate, 0.5% (v/v) acetic acid in 60/40 (v/v) acetonitrile/water. The isocratic flow rate was 0.4 ml min−1. Detection of the analytes was achieved with the AB Sciex API 5000 mass spectrometer (Framingham, MA, USA), with positive ion Turbo Ion Spray The tandem mass spectrometry analysis was operated in the multiple reaction monitoring mode with the same nominal m/z transitions outlined for the plasma method.
Pharmacokinetic parameters
Pharmacokinetic parameters were calculated on the basis of noncompartmental methods using WinNonlin-Professional, Version 5.2 (Pharsight Corporation, Mountain View, CA, USA), and summarized by descriptive statistics. Plasma concentration data from all subjects who received ABT-384 were included in the pharmacokinetic analyses. Plasma concentrations below the lower limit of quantitation were assigned as zero during the analyses.
Calculation of intrinsic CSF D3 cortisol formation
D3 cortisol may be present in the lumbar CSF because of either intrinsic (converted from D3 cortisone by HSD-1 in the CNS) or extrinsic (formed in the periphery and equilibrated across the blood–brain barrier) mechanisms. Extrinsic CSF D3 cortisol was calculated on the basis of the assumption that, as chemically identical species, the equilibria of D4 cortisol and D3 cortisol between plasma and CSF are identical. Thus, extrinsic CSF D3 cortisol (D3CSF,t,ext) for each time point was calculated as the following ratio:

where D4CSF,t is CSF D4 cortisol at time t, D3plasma,t-1 is plasma D3 cortisol 60 min before time t and D4plasma,t-1 is plasma D4 cortisol 60 min before time t.
Intrinsic CSF D3 cortisol (D3CSF,t,int), the parameter relevant to CNS HSD-1 inhibition, was then calculated as the following difference:

where D3CSF,t is CSF D3 cortisol at time t.
Results
Subject demographics and safety
Twelve men in general good health, between 30 and 47 years of age with a mean body mass index of 26.6±2.3, participated in the study.
No deaths, other serious adverse events or discontinuations due to adverse events occurred during the study. Treatment-emergent adverse events were post-lumbar puncture syndrome (N=6), procedural pain (N=4) and headache (N=2). All of the treatment-emergent adverse events were assessed by the investigator as not related or probably not related to ABT-384 and as mild or moderate in severity. No clinically significant changes of clinical laboratory tests, vital signs or electrocardiography parameters were observed. No subject showed adrenocorticotropic hormone or cortisol values above normal during the study. Two subjects, one of whom had above normal baseline cortisol-binding globulin, showed sporadic cortisol-binding globulin values above normal (all less than two times the upper limit of normal).
Pharmacokinetics of ABT-384 and its active metabolites
The median total plasma and CSF concentration-time profiles for ABT-384 after the last dose of ABT-384 on Day 5 are presented in Supplementary Figure 2. Pharmacokinetic parameters are presented in Supplementary Table 1. ABT-384 concentrations reached peak levels within 1.5–3 h in the plasma. The mean terminal-phase plasma elimination half-life of ABT-384 ranged from 4 to 14 h across the 1–50 mg QD dose regimens. The much shorter half-life at the 1 mg dose was due to a single subject who had low systemic exposure and whose ABT-384 concentrations quickly went below the lower limit of quantitation during the elimination phase. The exposure of the M1 metabolite in the plasma is higher than that of the acid metabolite, with the mean metabolite/parent area under the concentration-time curve (AUC) ratio ranging from 32 to 84% for the M1 metabolite and from 11 to 20% for the acid metabolite. The mean metabolite/parent maximum post-dose concentration (Cmax) ratio was 29–53% for the M1 metabolite and 6–9% for the acid metabolite.
The overall mean CSF concentration versus time profiles for ABT-384 and its acid metabolite were consistent with the profiles observed in plasma. ABT-384 concentrations reached peak levels within 2.5–5 h in the CSF. ABT-384 CSF levels were ∼10–50% of the free plasma levels and 0.3–1% of the total plasma levels. The acid metabolite CSF levels were ∼110–150% of the free plasma levels and 3–4% of the total plasma levels. The mean acid metabolite/parent Cmax and AUC0-24 ratios in CSF (Cmax ∼40% and AUC0–24 ∼70–90%) were higher than those observed in plasma (Cmax<10% and AUC0-24<20%).
Peripheral HSD-1 inhibition
In the liver, cortisol and cortisone are converted to their tetrahydro metabolites, which are rapidly excreted in the urine. Thus, the ratio of cortisol metabolites (5-α-tetrahydrocortisol+5-β-tetrahydrocortisol) to cortisone metabolite (tetrahydrocortisone) in urine is a proxy for the ratio of hepatic levels of HSD-1 product (cortisol) to substrate (cortisone).13 We had previously observed that regimens of 1–100 mg ABT-384 QD for 7 days decreased this ratio by 87–97% when calculated from a 24-h urine collection to eliminate potential confounding of results by interindividual variation of urination patterns or diurnal cortisol rhythms.1 Reasoning that it might not be particularly affected by those factors, we calculated the ratio of cortisol metabolites to cortisone metabolites in spot urine samples before dosing (Day 1) and at four time points between 2 and 40 h after five daily doses of ABT-384 (Days 5 and 6). The median decrease of hepatic HSD-1 inhibition from baseline was between 83 and 91% at each of four time points for each of four ABT-384 regimens (Figure 2). No differences of maximum inhibition or time to maximum inhibition between ABT-384 regimens were apparent. Consistent with results obtained from 24-h urine collection,1 those from spot urine samples in this study indicated full hepatic HSD-1 inhibition by regimens of 1–50 mg ABT-384 QD for 5 days. There were no values of urine cortisol metabolites below the limit of quantitation (BLQ).
ABT-384 inhibits its target 11-beta-hydroxysteroid dehydrogenase type 1 (HSD-1) in the liver. Spot urine samples were collected before dosing and four times between 2 and 40 h after five daily doses of ABT-384. The HSD-1 ratio is urine cortisol metabolites (5-α-tetrahydrocortisol+5-β-tetrahydrocortisol) divided by urine cortisone metabolite (tetrahydrocortisone). The median of two individuals is represented for each regimen.
D3 cortisol is uniquely formed by the action of HSD-1 on D3 cortisone. Thus, the ratio (plasma D3 cortisol/plasma D3 cortisone) can be used to assess peripheral HSD-1 inhibition by a highly selective inhibitor such as ABT-384. Low values of this ratio represent low (that is, inhibited) HSD-1 activity.4 The observed ratio of ∼4 in subjects to whom ABT-384 was not administered is consistent with prior results.8 On the basis of labeled plasma cortisol levels, peripheral HSD-1 inhibition was generally between 88 and 93% at each of eight time points during the first D4 cortisol infusion for 2, 10 and 50 mg QD ABT-384 regimens during the first D4 cortisol infusion (Figure 3, upper left panel). ABT-384 regimens of 2, 10 and 50 mg QD maintained this degree of HSD-1 inhibition at each of eight time points during the second D4 cortisol infusion, that is, up to 40 h after the last dose of ABT-384 (Figure 3, upper right panel). Peripheral HSD-1 inhibition of ∼81–87% was observed at each hour from 33 to 40 h after the last dose of 1 mg ABT-384 QD regimen (Figure 3, upper right panel). At each hour from 2 to 8 h after the last dose (near and after Tmax), similar inhibition was associated with the 1 mg ABT-384 QD regimen as with higher dose regimens (Figure 3, upper left panel). Somewhat lower peripheral HSD-1 inhibition was associated with the 1 mg ABT-384 QD regimen 1 h after the last dose (before Tmax).
ABT-384 inhibits its target 11-beta-hydroxysteroid dehydrogenase type 1 (HSD-1) in the periphery. Plasma samples were collected hourly during D4 cortisol infusions. D4 cortisol was infused on Day 5 from just after the last dose of ABT-384 for 8 h and again for 8 h starting either 22 (10, 50 mg) or 32 h (1, 2 mg) after the last dose of ABT-384. Subjects who did not receive ABT-384 received only one D4 cortisol infusion. The median of two individuals is represented for each regimen. Upper panels show the ratio (D3 cortisol/D3 cortisone) that is a direct measure of HSD-1 activity. Lower panels show the ratio (D3 cortisol/D4 cortisol) that is a measure of flux through the HSD-2+HSD-1 pathway.
The ratio (plasma D3 cortisol/plasma D4 cortisol) measures peripheral cortisol regeneration through HSD-2 and HSD-1, normalized for variations in kinetics of the injected tracer.4, 5, 6, 7, 8 It can serve as a measure of HSD-1 inhibition, although it could be confounded by concomitant HSD-2 inhibition or induction. Further, the ratio (plasma D3 cortisol/plasma D4 cortisol) is a useful measure only during D4 cortisol infusion, as D4 cortisol is not regenerated in vivo after it is converted to D3 cortisone by HSD-2. Therefore, the results for this ratio were censored at hour 4 for subjects to whom no ABT-384 was administered and did not clearly establish a steady-state value. However, the observed ratio of ∼1 at hour 4 is consistent with the steady-state value reported previously.4, 5, 6, 7, 8 Peripheral HSD-1 inhibition was therefore estimated as the difference between the ratio for subjects to whom no ABT-384 was administered and to whom each dose of ABT-384 was administered: 1—(plasma D3 cortisol/plasma D4 cortisol), where 1 is an approximation of the steady-state ratio in the absence of inhibitor. By this estimate, ABT-384 regimens of 2, 10 and 50 mg QD maintained ∼91–93% peripheral HSD-1 inhibition at each of 16 time points up to 40 h after the last dose of ABT-384 (Figure 3, lower panels). The 1 mg ABT-384 regimen maintained ∼90% peripheral HSD-1 inhibition at each of eight time points up to 8 h after the last dose (Figure 3, lower left panel). The inhibition decreased to ∼86% at 40 h after the last dose (Figure 3, lower right panel).
D4 cortisol, D3 cortisone and D3 cortisol plasma concentrations for each subject are presented in Supplementary Figures 4,5 and 8. There were no BLQ values at the time points during the D4 cortisol infusions.
CNS HSD-1 inhibition
Cortisol and cortisone equilibrate between plasma and the CSF mainly at the choroid plexus and reach the lumbar CSF by slow pulsatile flow, either directly or secondary to distribution in the brain. Thus, it was not expected that levels measured in the lumbar CSF would correspond to those measured at the same time in the plasma. Plasma- and CSF-labeled cortisol and cortisone data from the two subjects to whom D4 cortisol, but not ABT-384, were used to estimate a lag time for the calculation of CNS HSD-1 inhibition. The linear correlation between plasma D4 cortisol and CSF D4 cortisol at the same time point was poor (r2=0.14). Linear correlation was then assessed on the basis of lag times of 30, 45, 60 or 75 min from the plasma to lumbar CSF. Plasma values at intermediate time points were imputed by linear interpolation. The best correlation was between CSF D4 cortisol and plasma D4 cortisol measured 60 min earlier (r2=0.76). Similar results were obtained for D3 cortisone (r2=0.91) and D3 cortisol (r2=0.63). Quadratic fits were not superior to linear fits incorporating a 60-min lag time. Accordingly, the calculation of CNS HSD-1 inhibition assumed a 60-min interval for the distribution of cortisol and cortisone from the plasma to lumbar CSF.
Extrinsic and intrinsic CSF D3 cortisol levels were calculated using equations 1 and 2. As many D3CSF.t values were BLQ and the corresponding D3CSF.t,ext values were nonzero, D3CSF.t,int was frequently a negative number. Because of the small number of subjects and high proportion of BLQ values, we did not attempt to establish whether the negative D3CSF.t,int values are distinct from zero. In the results presented here, no attempt was made to impute a nonzero value to BLQ observations of D3CSF.t (Figure 4). A sensitivity analysis was performed in which all BLQ values were assumed to be half the lower limit of quantitation. The results of that analysis were not meaningfully different. The data from subjects to whom ABT-384 was not administered did not clearly establish a steady-state value for intrinsic CSF D3 cortisol. Therefore, any quantitative estimate of CNS HSD-1 inhibition would be speculative. Intrinsic CSF D3 cortisol was positive for the 2, 10 and 50 mg ABT-384 QD regimens at only one time point (for the 10 mg ABT-384 regimen). These data suggest essentially complete CNS HSD-1 inhibition by these regimens. Intrinsic CSF D3 cortisol was positive, yet approximately two- to three-fold lower during hours 4–8 of each infusion, compared with the level attained in the absence of study drug for the 1 mg ABT-384 regimen. These data suggest partial but substantial CNS HSD-1 inhibition, with some diminishment of such inhibition near the end of the second infusion (39–40 h after the last ABT-384 dose).
ABT-384 inhibits its target 11-beta-hydroxysteroid dehydrogenase type 1 (HSD-1) in the central nervous system (CNS). Cerebrospinal fluid (CSF) samples were collected hourly during D4 cortisol infusions. D4 cortisol was infused on Day 5 from just after the last dose of ABT-384 for 8 h and again for 8 h starting either 22 (10, 50 mg) or 32 h (1, 2 mg) after the last dose of ABT-384. Subjects who did not receive ABT-384 received only one D4 cortisol infusion. Results are not presented for hour 2 owing to a sample collection problem in one of these two subjects. The median of two individuals is represented for each regimen. See Discussion for potential explanations of negative intrinsic CSF D3 cortisol values.
The intrinsic CSF D3 cortisol values for the 1 mg ABT-384 regimen at 4–8 h after the last dose were similar to those at 36–38 h post dose. These time points were at least 4 h after initiation of the first and second D4 cortisol infusions, hence likely representing equilibrium values. This observation was somewhat surprising as the plasma and CSF levels of ABT-384 and its major metabolites were substantially lower at 36–38 h after the last dose. A potential explanation for the strong observed hysteresis is that ABT-384 and its major metabolites are characterized by rapid binding to, and very slow dissociation from, HSD-1 in vitro (data on file). On the basis of the enzyme kinetic data, it was expected that relatively constant HSD-1 inhibition would be observed for at least several hours after Tmax and that individual intrinsic CSF D3 cortisol would have a negative relationship with plasma Cmax. We further explored this possibility by plotting intrinsic D3 cortisol versus plasma Cmax (Figure 5). Intrinsic CSF D3 cortisol was averaged from hour 4 to hour 8 during the first D4 cortisol infusion. Earlier time points were not included as it appeared that approximate equilibrium was not attained before hour 4. Plasma Cmax was calculated as the sum of ABT-384 and its major metabolites, adjusted for relative in vitro Ki values (see Supplementary Figure 1):
Intrinsic cerebrospinal fluid (CSF) D3 cortisol decreases with increasing plasma Cmax. Intrinsic CSF D3 cortisol was averaged from hour 4 to hour 8 during the first D4 cortisol infusion. Plasma Cmax was calculated as the sum of ABT-384 and its major metabolites, adjusted for relative in vitro Ki values. See Discussion for potential explanations of negative intrinsic CSF D3 cortisol values.

As expected, among those who received 1 mg ABT-384 daily, the higher plasma Cmax (10.4 ng ml−1, ABT-384 equivalents) was in the subject who showed the lower intrinsic CSF D3 cortisol. No subject with plasma Cmax of at least 20.5 ng ml−1 (ABT-384 equivalents) showed any intrinsic CSF D3 cortisol.
D4 cortisol, D3 cortisone and D3 cortisol CSF concentrations for each subject are presented in Supplementary Figures 6 to 8. Calculated intrinsic and extrinsic CSF D3 cortisol concentrations for each subject are presented in Supplementary Table 2.
Discussion
Regimens of 1–50 mg ABT-384 QD for 5 days were well tolerated in this study. ABT-384 showed limited distribution across the blood–brain barrier with CSF/free plasma exposure ratios less than 0.5 across the dose range tested. The acid metabolite appeared to penetrate better across the blood–brain barrier with CSF/free plasma exposure ratios greater than 1 for each dose. The M1 metabolite of ABT-384 was not previously measured. In this study, the M1 metabolite plasma exposures were 70–80% of those of ABT-384. The M1 metabolite was detected in some CSF samples; however, the assay results were inconsistent and the assay is not considered validated (data on file).
D4 cortisol, which is converted to D3 cortisone by HSD-2 and D3 cortisol by HSD-1, was utilized as a tool to measure HSD-1 inhibition following ABT-384 administration to healthy volunteers.
Regimens of 2–50 mg ABT-384 QD for 5 days were associated with at least 87% inhibition of peripheral HSD-1 through up to 40 h after the last dose. The 1 mg ABT-384 QD regimen was associated with slightly lower peripheral HSD-1 inhibition compared with the other regimens at later time points, but was equivalent up to 8 h after the last dose. Steady-state plasma levels are not achieved after only five 1 mg ABT-384 doses but are achieved after seven 1 mg ABT-384 doses.1 In a prior study, full hepatic HSD-1 inhibition for 24 h, equivalent to that associated with higher doses, was observed for a regimen of 1 mg ABT-384 QD for 7 days.1 The combined results suggest that daily doses of 1 mg ABT-384 are sufficient for achieving full peripheral (not just hepatic) HSD-1 inhibition.
Complete blockade of D3 cortisol formation in the CNS through 40 h after the last dose was observed with administration of 2–50 mg ABT-384 QD for 5 days. Reduced CNS D3 cortisol formation, relative to that observed in subjects who received no ABT-384, was observed with the administration of 1 mg ABT-384 QD for 5 days. In a prior study, mean plasma Cmax values of 9.41 ng ml−1 ABT-384 and 0.31 ng ml−1 acid metabolite were observed for a regimen of 1 mg ABT-384 QD for 7 days (M1 was not measured).1 These higher drug levels might be sufficient to achieve full CNS HSD-1 inhibition for a 24-h dosing interval in many or most subjects. The minimum daily dose to achieve full CNS HSD-1 inhibition is no higher than 2 mg ABT-384. At steady state, it could be 1 mg ABT-384 (based on higher exposures achieved after 7 days compared with those achieved in this study after 5 days) or possibly lower. Additional study of lower dose ABT-384 regimens at steady state would be informative in this regard. As daily doses up to 100 mg were generally well tolerated in healthy volunteers and elderly subjects,1 ABT-384 has a wide potential therapeutic window for diseases such as Alzheimer’s disease and major depressive disorder in which CNS HSD-1 inhibition may have therapeutic benefit.
The observed HSD-1 inhibition may not be fully explained by plasma or CSF levels. Preclinical data indicate that ABT-384 preferentially distributes to the liver, the organ that expresses the highest HSD-1 levels, relative to the plasma in rats and monkeys (data on file). Similar preferential distribution in man can explain the observed full peripheral HSD-1 inhibition with plasma Cmax ∼2 ng ml−1, which would predict ∼60% HSD-1 inhibition (assuming reversible inhibition) in the absence of preferential tissue distribution. The relationships between brain and CSF levels of ABT-384 and its metabolites have not been well characterized. The observed full central HSD-1 inhibition in this study could be explained by preferential distribution of ABT-384 to the brain, relative to CSF. Further study of these relationships in preclinical species could be of value. The rapid binding, slow dissociation kinetics of ABT-384 (data on file) could possibly contribute to increased local concentrations where HSD-1 is expressed.
Peripheral HSD-1 inhibition by ABT-384 has been estimated using four different parameters, without substantial differences between the results. In a prior study, hepatic HSD-1 inhibition was measured as the ratio of cortisol metabolites to cortisone metabolite in urine collected during 24-h intervals.1 We have now demonstrated that hepatic HSD-1 inhibition is readily measured in spot urine samples. The ratio of D3 cortisol/D3 cortisone provides a measure of total body HSD-1 activity, and D3 cortisol/D4 cortisol provides a measure of total body flux through the HSD pathway. As results for these parameters were not meaningfully different from those obtained using urine metabolites, the additional complexity of D4 cortisol infusion is not justified to characterize the in vivo potency of an HSD-1 inhibitor in the periphery. The ratio of cortisol metabolites to cortisone metabolite in spot urine samples is a preferred method.
Calculation of intrinsic CSF D3 cortisol during a D4 cortisol infusion, utilizing data obtained via timed interval CSF collection, provided an estimate of CNS potency of an HSD-1 inhibitor. In the present experiment, extrinsic CSF D3 cortisol was low, as all tested ABT-384 regimens fully inhibited peripheral HSD-1. This condition was ensured by dosing ABT-384 for several days before the initiation of D4 cortisol infusion. We expect that results might be more difficult to interpret following a single dose of an HSD-1 inhibitor or with an inhibitor that achieves only partial peripheral HSD-1 blockade.
A limitation of the present results is that we could not precisely quantify submaximal CNS HSD-1 inhibition. The D4 cortisol infusion in subjects who did not receive ABT-384 was not of sufficient duration to establish an equilibrium value for intrinsic CSF D3 cortisol in the absence of an HSD-1 inhibitor. Longer (for example, 8 h) D4 cortisol infusions to a larger number of inhibitor-naïve subjects can establish this reference value for future experiments. Alternately, it may be feasible in future experiments to establish individual baselines in study subjects during a D4 cortisol infusion with timed interval CSF collection just before initial administration of an HSD-1 inhibitor. Another limitation of this study is that intrinsic CSF D3 cortisol formation was observed in only two subjects. In future experiments, it will be desirable to increase the number of subjects in whom full enzyme inhibition is not achieved to better understand the concentration–effect relationship and variability thereof. Additional limitations of this study are apparent in the mostly negative intrinsic CSF D3 cortisol values for subjects who received ⩾2 mg ABT-384 QD. These negative values might reflect conversion within the CNS of extrinsic D3 cortisol to D3 cortisone by HSD-2, which is expressed in circumventricular brain regions distinct from those that express HSD-1.10 Another likely reason for these values is that we did not impute a nonzero value for BLQ measurements of CSF D3 cortisol in the presented analyses. Further validation work to reduce the lower limit of quantitation for CSF D3 cortisol could help in this regard. Imperfect estimation of the lag time between the plasma and CSF used for the calculation of extrinsic CSF D3 cortisol, by leading to overestimation of that parameter, might also have contributed to the preponderance of negative intrinsic CSF D3 cortisol values.
The administration of a labeled enzyme substrate coupled with continuous or timed interval CSF collection may be an attractive method for measuring CNS target engagement by other enzyme inhibitors. Most commonly, CNS target engagement has been demonstrated using positron emission tomography (PET). PET has been used to show CNS target engagement by inhibitors of monoamine oxidases A and B, catechol-O-methyltransferase and acetylcholinesterase.14, 15, 16, 17, 18, 19 PET provides regional activity information, which detection of a mass-labeled tracer in CSF cannot. However, there are several limitations to PET. Developing a PET ligand for a new target can be as complex as developing a new drug, often requiring exploitation of a structure–activity relationship distinct from optimal physical characteristics of medications. Some targets are not amenable to PET neuroimaging, particularly if not abundant. Separate regulatory documentation is required for PET ligands. In contrast, the chemistry to mass label a natural enzyme substrate, and mass spectrometric assay development for the labeled substrate and product, will often be straightforward. A labeled substrate approach can be useful for low-abundance enzymes, as mass spectrometric assays are highly sensitive and the catalytic activity of the enzyme is a natural signal amplifier. Labeled tracers can be formulated for clinical administration without the specialized facilities, equipment and procedures necessary for radioactive tracers. Clinical use of D4 cortisol did not require any additional animal safety testing or filing of a separate Investigational New Drug application with the Food and Drug Administration. Labeled enzyme substrates, exemplified by D4 cortisol as a precursor of the HSD-1 substrate D3 cortisone, represent a viable additional tool, besides PET, for measuring CNS effect during new drug development.
References
Liu W, Katz DA, Locke C, Daszkowski D, Wang Y, Rieser MJ et al. Clinical safety, pharmacokinetics and pharmacodynamics of the 11β-hydroxysteroid dehydrogenase type 1 inhibitor ABT-384 in healthy volunteers and elderly adults. Clin Pharmacol Drug Dev 2013; 2: 133–151.
Tomlinson JW, Walker EA, Bujalska IJ, Draper N, Lavery GG, Cooper MS et al. 11ß-Hydroxysteroid dehydrogenase type 1: a tissue-specific regulator of glucocorticoid response. Endocr Rev 2004; 25: 831–866.
Linberg L, Wang JZ, Arison BH, Ulick S . Synthesis of a deuterium-labeled cortisol for the study of its rate of 11-beta-hydroxy dehydrogenation in man. J Steroid Biochem Mol Biol 1991; 38: 351–357.
Andrew R, Smith K, Jones GC, Walker BR . Distinguishing the activities of 11ß-hydroxysteroid dehydrogenases in vivo using isotopically labeled cortisol. J Clin Endocrinol Metab 2002; 87: 277–285.
Basu R, Singh RJ, Basu A, Chittilapilly EG, Johnson CM, Toffolo G et al. Splanchnic cortisol production occurs in humans: evidence for conversion of cortisone to cortisol via the 11-ß hydroxysteroid dehydrogenase (11ß-HSD) type 1 pathway. Diabetes 2004; 53: 2051–2059.
Andrew R, Westerbacka J, Wahren J, Yki-Järvinen H, Walker BR . The contributions of visceral adipose tissue to splanchnic cortisol production in healthy humans. Diabetes 2005; 54: 1364–1370.
Basu R, Singh RJ, Basu A, Chittilapilly EG, Johnson MC, Toffolo G et al. Obesity and type 2 diabetes do not alter splanchnic cortisol production in humans. J Clin Endocrinol Metab 2005; 90: 3919–3926.
Basu R, Singh R, Basu A, Johnson CM, Rizza RA . Effect of nutrient ingestion on total-body and splanchnic cortisol production in humans. Diabetes 2006; 55: 667–674.
Basu R, Basu A, Grudzien M, Jung P, Jacobsen P, Johnson M et al. Liver is the site of splanchnic cortisol production in obese nondiabetic humans. Diabetes 2009; 58: 39–45.
White PC, Mune T, Agarwal AK . 11ß-Hydroxysteroid dehydrogenase and the syndrome of apparent mineralocorticoid excess. Endocr Revi 1997; 18: 135–156.
Jhee SS, Zarotsky V . Safety and tolerability of serial cerebrospinal fluid collections during pharmacokinetic/pharmacodynamic studies: 5 years of experience. Clin Res Regul Aff 2003; 20: 357–363.
Li J, Llano DA, Ellis T, LeBlond D, Bhathena A, Jhee SS et al. Effect of human cerebrospinal fluid sampling frequency on amyloid-β levels. Alzheimer’s Dement 2012; 8: 295–303.
Palermo M, Shackleton CHL, Mantero F, Stewart PM . Urinary free cortisone and the assessment of 11ß-hydroxysteroid dehydrogenase activity in man. Clin Endocrinol 1996; 45: 605–611.
Bergström M, Westerberg G, Németh G, Traut M, Gross G, Greger G et al. MAO-A inhibition in brain after dosing with esuprone, moclobemide and placebo in healthy volunteers: in vivo studies with positron emission tomography. Eur J Clin Pharmacol 1997; 52: 121–128.
Fowler JS, Logan J, Azzaro AJ, Fielding RM, Zhu W, Poshusta AK et al. Reversible inhibitors of monoamine oxidase-A (RIMAs): robust, reversible inhibition of human brain MAO-A by CX157. Neuropsychopharmacology 2010; 35: 623–631.
Freedman NMT, Mishani E, Krausz Y, Weininger J, Lester H, Blaugrund E et al. In vivo measurement of brain monoamine oxidase B occupancy by rasagiline, using 11C-L-deprenyl and PET. J Nuclear Med 2005; 46: 1618–1624.
Hirvonen J, Kailajärvi M, Haltia T, Koskimies S, Någren K, Virsu P et al. Assessment of MAO-B occupancy in the brain with PET and [11C]-L-deprenyl-D2: A dose-finding study with a novel MAO-B inhibitor, EVT 301. ClinPharmacol Therap 2009; 85: 506–512.
Ruottinen HM, Niinivirta M, Bergman J, Oikonen V, Solin O, Eskola O et al. Detection of response to COMT inhibition in FDOPA PET in advanced Parkinson’s disease requires prolonged imaging. Synapse 2001; 40: 19–26.
Shinotoh H, Aotsuka A, Fukushi K, Nagatsuka S, Tanaka N, Ota T et al. Effect of donepezil on brain acetylcholinesterase activity in patients with AD measured by PET. Neurology 2001; 56: 408–410.
Acknowledgements
This research was funded by AbbVie. ABT-384 is a proprietary compound owned by AbbVie.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors designed, conducted and analyzed the study as employees or contractors of AbbVie. The decision to publish was approved with research management and legal review at AbbVie. Rita Basu was paid as an independent consultant during the design of the study. Hakop Gevorkian, Stanford S Jhee and Larry Ereshefsky are employees of California Clinical Trials Medical Group or PAREXEL International, organizations that were contracted by AbbVie to conduct the study. David A Katz, Wei Liu, Charles Locke, Peer Jacobson, Diane M Barnes, Guohua An, Matthew J Rieser, Dan Daszkowski, Frances Groves, Gerard Heneghan, Ajay Shah and Gerard J. Marek are (or were at the time of the study) employees of AbbVie and may own AbbVie stock or options.
Additional information
Supplementary Information accompanies the paper on the Translational Psychiatry website
Supplementary information
Rights and permissions
This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivs 3.0 Unported License. To view a copy of this license, visit http://creativecommons.org/licenses/by-nc-nd/3.0/
About this article
Cite this article
Katz, D., Liu, W., Locke, C. et al. Peripheral and central nervous system inhibition of 11β-hydroxysteroid dehydrogenase type 1 in man by the novel inhibitor ABT-384. Transl Psychiatry 3, e295 (2013). https://doi.org/10.1038/tp.2013.67
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/tp.2013.67