Abstract
Clinical studies have shown that assessing circulating concentrations of high-density lipoprotein (HDL) particles by nuclear magnetic resonance (NMR) spectroscopy is superior to HDL-cholesterol in predicting cardiovascular risk. We tested the hypothesis that circulating concentrations of HDL particles predict 3-month mortality of patients with acute heart failure (AHF). Out of 152 included patients, 52% were female, additionally the mean patient age was 75.2 ± 10.3 years, and three-month mortality was 27%. Serum lipoprotein profile at admission was determined by NMR spectroscopy. Univariate logistic regression analyses revealed a significant inverse association of total (odds ratio (OR) 0.38 per 1-SD increase, 95% confidence interval (CI) 0.23–0.60, p < 0.001) and small HDL particle concentrations (OR 0.35 per 1-SD increase, 95% CI 0.19–0.60, p < 0.001) with 3-month mortality, whereas concentrations of large HDL particles (p = 0.353) or HDL-cholesterol (p = 0.107) showed no significant association. After adjustment for age, sex, mean arterial pressure, low-density lipoprotein cholesterol, glomerular filtration rate, urea, and N-terminal pro-brain natriuretic peptide, both the total and small HDL particle concentrations remained significantly associated with 3-month mortality. Based on our results, we conclude that total and small HDL particle concentrations strongly and independently predict 3-month mortality in AHF patients.
Similar content being viewed by others
Introduction
Heart failure (HF) remains an important cause of morbidity and mortality worldwide1. Accurate prognostic biomarkers are crucial for risk assessment, timely and appropriate therapeutic intervention, and overall management of HF. Therefore, identification of new markers reflecting different aspects of the underlying pathophysiology may improve risk assessment in HF.
High-density lipoprotein (HDL) exerts numerous beneficial effects on the cardiovascular system. These include attenuation of the inflammatory response in the vascular endothelium and macrophages, low-density lipoprotein (LDL) protection from oxidation, endothelial nitric oxide (NO) production stimulation and the associated vasodilatation promotion, as well as insulin-independent glucose uptake stimulation in cardiomyocytes2,3,4,5,6.
The promotion of reverse cholesterol transport is the best-studied protective activity of HDL. It is a dynamic process by which cholesterol is transported by HDL from the periphery to the liver for excretion7. Recent studies delivered solid evidence that cholesterol efflux capacity is inversely related to incident coronary heart events in the general population, independent of well-known cardiovascular risk factors8,9. However, it has to be pointed out that this association is not present in patients with chronic kidney disease10.
Even though clinical and epidemiological studies revealed an inverse relationship between HDL-cholesterol and cardiovascular disease11, a number of studies argue against HDL-cholesterol as therapeutic target. This thesis was exemplified by a failure of the Mendelian randomization approach to show a relationship between genetic variants that increase plasma concentrations of HDL cholesterol and a decreased risk of cardiovascular events12 as well as by a failure of pharmacological HDL-cholesterol raising therapy to reduce cardiovascular events13,14. HDL-cholesterol concentrations, therefore, appear to provide limited information regarding the cardioprotective activities of HDL, despite increasing evidence supporting the clinical significance of these pleiotropic HDL functions.
Decreased HDL cholesterol plasma levels and impaired HDL function have previously been reported in HF patients15, and several studies examined the association of outcome and prognosis in HF with HDL-cholesterol16,17,18.
Clinical studies have shown that assessing circulating concentrations of HDL particles by nuclear magnetic resonance (NMR) spectroscopy is superior to HDL-cholesterol in predicting cardiovascular risk19. HDL particle concentrations attribute equal weight to all HDL subclasses and therefore better represent the biological relationship between HDL and clinical risk19. While assessing the functional properties of HDL may not be readily applicable in the everyday clinical practice, NMR-based measurements of HDL particle concentrations bear a great potential for improved assessment of cardiovascular risk.
We hypothesized that HDL particle concentration might predict mortality in subjects presenting with acute heart failure (AHF). Therefore, we explored the association of HDL particle concentrations with 3-month mortality in patients with AHF.
Results
Patients
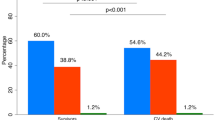
The patients’ baseline characteristics were reported elsewhere20. In brief, out of 152 included patients 52% were female, 7.2% belonged to New York Heart Association Functional Classification (NYHA) class 2, 54.6% belonged to NYHA class 3, and 38.2% belonged to NYHA class 4. The mean patient age was 75.2 ± 10.3 years. Frequent comorbidities were hypertension (89.5%), followed by type 2 diabetes mellitus (51.7%), hyperlipidemia/hypertriglyceridemia (39.5%), and hypercholesterolemia (38.8%). Worsening of chronic HF emerged in 69.1% of patients, and 42.4% had a preserved ejection fraction. Three-month mortality was 27.4%. The patients’ laboratory parameters are shown in Table 1.
Correlation of HDL particle- and HDL cholesterol- concentrations with laboratory and clinical variables
As presented in Table 2, the concentrations of total and small HDL particles were positively correlated with albumin and glomerular filtration rate (GFR) and negatively correlated with urea, N-terminal pro-Brain Natriuretic Peptide (NT-proBNP), and C-reactive protein (CRP). Concentrations of large HDL particles were not significantly correlated with any laboratory parameters, whereas levels of HDL-cholesterol were positively correlated with GFR and negatively correlated with urea and CRP. The concentrations of large HDL particles were negatively correlated with body weight and body mass index (BMI), a correlation that was observed neither for the concentrations of total and small HDL particles nor for HDL- cholesterol (Table 2).
Logistic regression analyses
Univariate analyses revealed a highly significant inverse association of 3-month mortality with total and small HDL particle concentrations as well as with total cholesterol, LDL-cholesterol, mean arterial pressure (MAP), and GFR (Table 3). A significant positive association with 3-month mortality was observed for creatinine, urea, and NT-proBNP (Table 3). Concentrations of large HDL particles were not significantly associated with 3-month mortality (Table 3). Importantly, the concentrations of both total and small HDL particles remained significantly associated with 3-month mortality after adjusting for age and sex, as well as for clinical and laboratory parameters that showed a significant association with 3-month mortality in the univariate analyses, taking multicollinearity into account (Table 4).
Discussion
Accurate prognostic biomarkers are critical for risk assessment, appropriate therapeutic intervention, and overall management of HF. The present study shows for the first time that a low concentration of circulating small HDL particles is associated with 3-month mortality of AHF patients. Interestingly, only the concentrations of small HDL particles were associated with mortality, whereas the concentrations of large HDL particles and HDL-cholesterol were not.
Our results appear to be in line with recent studies showing that elevated concentrations of HDL particles were associated with a reduced risk of coronary heart disease (CHD) as well as with reduced CHD mortality [reviewed in21]. However, as mentioned above, no single study so far has examined the role of HDL particle concentrations on mortality in AHF. Previous studies have clearly shown that cardioprotective activities of HDL, including cholesterol efflux capacity, anti-inflammatory, anti-apoptotic, as well as endothelial protective capabilities, depend on specific HDL particle characteristics that are not well represented by the HDL-cholesterol content (a measure of larger, more cholesterol-rich HDL subclasses)21,22. The results of the present study appear to be in agreement with the concept of a strong structure-function relationship of HDL particles.
Our results clearly demonstrate that circulating HDL particle concentrations, but not the levels of HDL-cholesterol, predict 3-month mortality of AHF patients. Interestingly, serum concentrations of total and small HDL particles, but not of HDL-cholesterol, were positively correlated with the albumin level, a marker of nutritional status and liver biosynthetic capacity, and negatively correlated with NT-proBNP, a marker of HF severity (Table 2). This difference between small HDL particles and HDL-cholesterol regarding their sensitivity to the AHF pathophysiology could be explained by the fact that circulating HDL-cholesterol levels mainly reflect the concentrations of large (cholesterol-rich) HDL particles. Our observation that neither HDL-cholesterol nor the concentrations of large HDL particles were correlated with albumin or NT-proBNP levels (Table 2) is in full agreement with that notion.
In line with previous studies21, small HDL particles constituted the majority of total HDL particles (Table 1). In the present study, the concentration of small HDL particles differed markedly from that of the less abundant large HDL particles, regarding their associations with serum albumin, the markers of renal function, urea, and GFR, as well as with the inflammatory marker CRP or with NT-proBNP (Table 2). A previous study showed that adiposity affects lipoprotein size and subclass concentrations in the general population23. We also observed that the concentrations of large, but not small, HDL particles were negatively correlated with the body mass index (Table 2). Strikingly, we found no correlation between the serum levels of small and large HDL particles (ρ = −0.16; p = 0.132). This observation suggests that in AHF patients the metabolism of small and large HDL particles is not linked. Our results are in agreement with a recent metabolic study showing that the liver directly secrets HDL particles of different sizes into the circulation, whereas the interconversion of circulating HDL particles appears to be of minor importance24.
Circulating HDL particles may exert direct positive effect on the failing heart. HDL has been shown to attenuate apoptosis, improve cell survival, preserve mitochondrial function, attenuate oxidative stress25,26, as well as to promote glucose uptake by cardiomyocytes27. Furthermore, by inducing the expression and activity of endothelial nitric oxide synthase, HDL increases vascular NO bioavailability5, thereby promoting vasorelaxation of the coronary arteries and, in turn, perfusion of the failing heart. By attenuation of the endothelial inflammatory response3, as well as by endotoxin-binding and neutralization, HDL may ameliorate the chronic inflammatory status in HF28. In line with this, we found a negative correlation of HDL particle concentrations and CRP in our AHF cohort (Table 2).
Based on our results, we conclude that serum concentrations of total and small HDL particles are strong and independent predictors of 3-month mortality in AHF patients.
Because the limited number of participants in this monocentric study may have affected the statistical power of our analyses, further large studies are needed to confirm our results.
Methods
Study design and patients
The study was designed as a prospective, single-center study. It included hospitalized adult Caucasian consecutive patients with AHF. The Ethics Committee of the University Hospital Centre Sisters of Charity, Zagreb, Croatia as well as the Ethics Committee of the Medical University of Graz approved the study. Written informed consent was obtained in compliance with Good Clinical Practice, and the Declaration of Helsinki29. In total, 152 patients were enrolled from November 2013 to February 2015. The patients were classified according to the European Society of Cardiology (ESC) and the American College of Cardiology Foundation/American Heart Association (ACCF/AHA) Guidelines for HF30,31,32. All patients were treated according to the ESC Guidelines for AHF31,32. Hypertension was diagnosed according to the ESC criteria33. Diabetes was diagnosed in patients with dietary treatment, antidiabetic medication or current fasting plasma glucose levels higher than 7.0 mmol/L34. Hypercholesterolemia was defined as LDL-cholesterol levels higher than 3.5 mmol/L, or taking a lipid-lowering drug and hypertriglyceridemia was defined as triglyceride levels higher than 1.7 mmol/L. Patients with severe renal failure (serum creatinine ≥400 mmol/L) were not included in the study.
Laboratory assays
Blood samples were obtained at admission to the hospital. The blood was collected in 6 mL tubes, VACUETTE® Z Serum Clot Activator (Greiner Bio-one GmbH, Kremsmuenster, Austria). Beckman Coulter instrument AU 2700, 2007 (Brea, CA, SAD) and Architect c8000, Abbott 2013 (Chicago, IL, SAD) were used for analysis of serum albumin, creatinine, urea, CRP, total plasma cholesterol, LDL-cholesterol, HDL-cholesterol, and triglycerides. GFR was calculated as previously described35. Electrochemiluminescence immunoassay with Elecsys e411 (Roche Diagnostics GmbH, Mannheim, Germany) was used for NT-proBNP quantification.
Lipoprotein profiling by NMR spectroscopy
The lipoprotein profiles of 138 serum samples were available for analysis using the AXINON® lipoFIT®-S100 test system (Numares Health, Regensburg, Germany) as described previously36. In brief, serum (630 μl) was gently mixed with 70 μl of an internal standard (with reference substances, NaN3 and D2O). From this solution 600 μl were transferred into 5-mm NMR tubes, followed by the recording of NMR spectra at a temperature of 310 K on a shielded 600 MHz Bruker Avance III HD spectrometer with a 5-mm triple resonance TXI probe head including a deuterium lock channel and a z-grade coil. Only samples and their spectra which met a defined set of quality criteria were analyzed, in order to ensure the data quality. Lipoprotein particle concentrations and mean sizes reported are calibrated to an NMR-based lipoprotein profiling method37. HDL particles with a diameter smaller than 8.8 nm were designated small, and those with a diameter of 8.8 nm or more were considered large38. The number (n) of samples, which were analyzed for a particular lipoprotein parameter, is indicated in Table 2.
Statistical analysis
Categorical data are shown as absolute and relative frequencies; continuous data are shown as median and range from minimum to maximum. Correlations between various laboratory/clinical parameters and certain lipid parameters, including concentrations of HDL particles and HDL-cholesterol, were determined by Spearman correlation. Univariate logistic regression analyses was used to examine the impact of various clinical and laboratory parameters on 3-month mortality. To further assess the predictive ability of the total and small HDL particle concentrations, we adjusted for age, gender, mean arterial pressure (MAP), LDL-cholesterol, GFR, urea, and NT-proBNP in a multivariate model. Results were expressed as odds ratio (OR) and the respective 95% confidence interval (CI) per standard deviation (SD) increase. Variance inflation factor was used to assess multicollinearity among covariates in the multivariate model. R version 3.2.2. was used to analyse data.
Additional Information
How to cite this article: Potočnjak, I. et al. Serum Concentration of HDL Particles Predicts Mortality in Acute Heart Failure Patients. Sci. Rep. 7, 46642; doi: 10.1038/srep46642 (2017).
Publisher's note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
Roger, V. L. et al. Trends in heart failure incidence and survival in a community-based population. Jama 292, 344–350 (2004).
Besler, C. et al. Mechanisms underlying adverse effects of HDL on eNOS-activating pathways in patients with coronary artery disease. The Journal of clinical investigation 121, 2693–2708 (2011).
Cockerill, G. W., Rye, K. A., Gamble, J. R., Vadas, M. A. & Barter, P. J. High-density lipoproteins inhibit cytokine-induced expression of endothelial cell adhesion molecules. Arteriosclerosis, thrombosis, and vascular biology 15, 1987–1994 (1995).
Parthasarathy, S., Barnett, J. & Fong, L. G. High-density lipoprotein inhibits the oxidative modification of low-density lipoprotein. Biochimica et biophysica acta 1044, 275–283 (1990).
Yuhanna, I. S. et al. High-density lipoprotein binding to scavenger receptor-BI activates endothelial nitric oxide synthase. Nature medicine 7, 853–857 (2001).
Bursill, C. A. et al. High-density lipoproteins suppress chemokines and chemokine receptors in vitro and in vivo . Arteriosclerosis, thrombosis, and vascular biology 30, 1773–1778 (2010).
Rothblat, G. H. & Phillips, M. C. High-density lipoprotein heterogeneity and function in reverse cholesterol transport. Current opinion in lipidology 21, 229–238 (2010).
Rohatgi, A. et al. HDL cholesterol efflux capacity and incident cardiovascular events. The New England journal of medicine 371, 2383–2393 (2014).
Saleheen, D. et al. Association of HDL cholesterol efflux capacity with incident coronary heart disease events: a prospective case-control study. The lancet. Diabetes & endocrinology 3, 507–513 (2015).
Bauer, L. et al. HDL Cholesterol Efflux Capacity and Cardiovascular Events in Patients With Chronic Kidney Disease. Journal of the American College of Cardiology 69, 246–247 (2017).
Gordon, T., Castelli, W. P., Hjortland, M. C., Kannel, W. B. & Dawber, T. R. High density lipoprotein as a protective factor against coronary heart disease. The Framingham Study. The American journal of medicine 62, 707–714 (1977).
Voight, B. F. et al. Plasma HDL cholesterol and risk of myocardial infarction: a mendelian randomisation study. Lancet 380, 572–580 (2012).
Investigators, A.-H. et al. Niacin in patients with low HDL cholesterol levels receiving intensive statin therapy. The New England journal of medicine 365, 2255–2267 (2011).
Group, H. T. C. et al. Effects of extended-release niacin with laropiprant in high-risk patients. The New England journal of medicine 371, 203–212 (2014).
Patel, P. J., Khera, A. V., Wilensky, R. L. & Rader, D. J. Anti-oxidative and cholesterol efflux capacities of high-density lipoprotein are reduced in ischaemic cardiomyopathy. European journal of heart failure 15, 1215–1219 (2013).
Freitas, H. F., Barbosa, E. A., Rosa, F. H., Lima, A. C. & Mansur, A. J. Association of HDL cholesterol and triglycerides with mortality in patients with heart failure. Brazilian journal of medical and biological research = Revista brasileira de pesquisas medicas e biologicas/Sociedade Brasileira de Biofisica … [et al.] 42, 420–425 (2009).
Mehra, M. R. et al. High-density lipoprotein cholesterol levels and prognosis in advanced heart failure. The Journal of heart and lung transplantation: the official publication of the International Society for Heart Transplantation 28, 876–880 (2009).
Cai, A. et al. Associations of high HDL cholesterol level with all-cause mortality in patients with heart failure complicating coronary heart disease. Medicine 95, e3974 (2016).
Santos-Gallego, C. G. HDL: Quality or quantity? Atherosclerosis 243, 121–123 (2015).
Potocnjak, I. et al. Metrics of High-Density Lipoprotein Function and Hospital Mortality in Acute Heart Failure Patients. PloS one 11, e0157507 (2016).
Kontush, A. HDL particle number and size as predictors of cardiovascular disease. Frontiers in pharmacology 6, 218 (2015).
Birner-Gruenberger, R., Schittmayer, M., Holzer, M. & Marsche, G. Understanding high-density lipoprotein function in disease: recent advances in proteomics unravel the complexity of its composition and biology. Progress in lipid research 56, 36–46 (2014).
Goff, D. C., Jr., D’Agostino, R. B., Jr., Haffner, S. M. & Otvos, J. D. Insulin resistance and adiposity influence lipoprotein size and subclass concentrations. Results from the Insulin Resistance Atherosclerosis Study. Metabolism: clinical and experimental 54, 264–270 (2005).
Mendivil, C. O., Furtado, J., Morton, A. M., Wang, L. & Sacks, F. M. Novel Pathways of Apolipoprotein A-I Metabolism in High-Density Lipoprotein of Different Sizes in Humans. Arteriosclerosis, thrombosis, and vascular biology 36, 156–165 (2016).
Gomaraschi, M., Calabresi, L. & Franceschini, G. Protective Effects of HDL Against Ischemia/Reperfusion Injury. Frontiers in pharmacology 7, 2 (2016).
Van Linthout, S., Frias, M., Singh, N. & De Geest, B. Therapeutic potential of HDL in cardioprotection and tissue repair. Handbook of experimental pharmacology 224, 527–565 (2015).
Siebel, A. L., Heywood, S. E. & Kingwell, B. A. HDL and glucose metabolism: current evidence and therapeutic potential. Frontiers in pharmacology 6, 258 (2015).
Rauchhaus, M., Coats, A. J. & Anker, S. D. The endotoxin-lipoprotein hypothesis. Lancet 356, 930–933 (2000).
World Medical, A. World Medical Association Declaration of Helsinki: ethical principles for medical research involving human subjects. Jama 310, 2191–2194 (2013).
Dickstein, K. et al. ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure 2008: the Task Force for the Diagnosis and Treatment of Acute and Chronic Heart Failure 2008 of the European Society of Cardiology. Developed in collaboration with the Heart Failure Association of the ESC (HFA) and endorsed by the European Society of Intensive Care Medicine (ESICM). European heart journal 29, 2388–2442 (2008).
McMurray, J. J. et al. ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure 2012: The Task Force for the Diagnosis and Treatment of Acute and Chronic Heart Failure 2012 of the European Society of Cardiology. Developed in collaboration with the Heart Failure Association (HFA) of the ESC. European heart journal 33, 1787–1847 (2012).
Yancy, C. W. et al. 2013 ACCF/AHA guideline for the management of heart failure: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. Journal of the American College of Cardiology 62, e147–239 (2013).
Mancia, G. et al. 2007 Guidelines for the Management of Arterial Hypertension: The Task Force for the Management of Arterial Hypertension of the European Society of Hypertension (ESH) and of the European Society of Cardiology (ESC). Journal of hypertension 25, 1105–1187 (2007).
American Diabetes, A. Diagnosis and classification of diabetes mellitus. Diabetes care 34 Suppl 1, S62–69 (2011).
Levey, A. S. et al. A new equation to estimate glomerular filtration rate. Annals of internal medicine 150, 604–612 (2009).
Kaess, B. M. et al. Large-scale candidate gene analysis of HDL particle features. PloS one 6, e14529 (2011).
Hopkins, P. N., Pottala, J. V. & Nanjee, M. N. A comparative study of four independent methods to measure LDL particle concentration. Atherosclerosis 243, 99–106 (2015).
Otvos, J. D. Measurement of lipoprotein subclass profiles by nuclear magnetic resonance spectroscopy. Clinical laboratory 48, 171–180 (2002).
Acknowledgements
Authors would like to thank Aleksandra Žmegač Horvat, University of Zagreb School of Medicine, for language editing the text. This research was supported by the Austrian Science Foundation [P27166-B23 to SF; P22976-B18 to GM] and the Jubilee Foundation of the Austrian National Bank [15858 to S.F.]. They had no roles in the design of the study, data collection, analysis, and interpretation, report writing or article submission.
Author information
Authors and Affiliations
Contributions
Experiments conceived and designed by: I.P., V.D., S.F., G.M. Experiments carried out by: I.P., V.D., M.T. Contribution of reagents/materials/analysis tools: S.F. G.M. Contributed significantly to the execution, the analysis or both and interpretation of data: I.P., M.T., G.P., A.B., G.M., V.D., S.F. Paper was written by: I.P., V.D., A.B., G.P., G.M., S.F. Participated in reviewing, and/or revising the manuscript for intellectual content: I.P., M.T., G.P., A.B., G.M., V.D., S.F. The manuscript was approved for submission by: I.P., M.T., G.P., A.B., G.M., V.D., S.F.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing financial interests.
Rights and permissions
This work is licensed under a Creative Commons Attribution 4.0 International License. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in the credit line; if the material is not included under the Creative Commons license, users will need to obtain permission from the license holder to reproduce the material. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/
About this article
Cite this article
Potočnjak, I., Degoricija, V., Trbušić, M. et al. Serum Concentration of HDL Particles Predicts Mortality in Acute Heart Failure Patients. Sci Rep 7, 46642 (2017). https://doi.org/10.1038/srep46642
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/srep46642
This article is cited by
-
High-density lipoprotein-mediated cardioprotection in heart failure
Heart Failure Reviews (2021)
-
Particle size and cholesterol content of circulating HDL correlate with cardiovascular death in chronic heart failure
Scientific Reports (2021)
-
Serum level of HDL particles are independently associated with long-term prognosis in patients with coronary artery disease: The GENES study
Scientific Reports (2020)
-
Serum Concentrations of Citrate, Tyrosine, 2- and 3- Hydroxybutyrate are Associated with Increased 3-Month Mortality in Acute Heart Failure Patients
Scientific Reports (2019)
-
Atrial fibrillation is associated with alterations in HDL function, metabolism, and particle number
Basic Research in Cardiology (2019)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.