Abstract
To investigate the characteristics of newly diagnosed early-onset diabetes in the Chinese population, 2801 newly diagnosed diabetes participants without known diabetes or pre-diabetes in a national cross-sectional survey were analysed. Participants were divided into quartiles (22–43, 44–52, 53–61 and >61 years) according to age of diabetes onset and the first group were defined as early-onset diabetes group. Early-onset diabetes group had lower systolic blood pressure (SBP), total cholesterol, low density lipoprotein cholesterol, 2-hour post prandial blood glucose and urine albumin creatinine ratio. There was no difference in body mass index, Homeostasis model assessment (HOMA) of beta cell function and diabetes family history between early-onset diabetes participants and any other age groups. HOMA of insulin resistance (IR) scores and disposition index 30 minutes after glucose load (DI30) were increased in early-onset diabetes participants. The beta cell function declination was more deteriorated in early-onset diabetes participants. Male gender, triglycerides, HOMA-IR and DI30 were positively associated with an earlier age at diagnosis. In conclusion, patients diagnosed with diabetes at a younger age are characterized by a similar cardiovascular risk profile with increased insulin resistance and more severe beta cell failure than patients diagnosed at a later age.
Similar content being viewed by others
Introduction
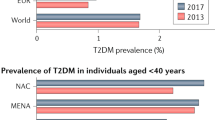
Early-onset diabetes was defined as diabetes with an age of diagnosis at a young age, and different cut-offs for age at diagnosis were used to define early-onset diabetes (30–45 years of age). Although type 2 diabetes is a disease related to aging, the prevalence of adult early-onset type has increased globally1,2,3. A higher proportion of early-onset diabetes was observed more frequently in Asian countries than in Western countries4,5. The number of early-onset diabetes cases increased 4-fold from 1997 to 2010 in China, and the number of cases will increase by at least 20% over the next 20 years2,5. Therefore, early-onset diabetes is becoming one of the major health burdens in China.
Recent studies demonstrated that adult early-onset type 2 diabetes is a more progressive disease from a cardiovascular standpoint than late-onset type 2 diabetes6,7,8. These patients lose up to 15 years of life expectancy, which is two-fold greater than the number of years lost by patients with late-onset diabetes9. In contrast to late-onset diabetes, early-onset diabetes is associated with a higher risk of developing cardiovascular and microvascular complications, which are largely due to prolonged disease exposure in both Westerners and Asians3,8,10,11. A large number of early-onset diabetes patients receive inadequate anti-glycaemic treatment and suboptimal cardio-protective treatment, which may be partially attributed to the lack of knowledge regarding the harm of early-onset diabetes in daily clinical practice3,12.
The detection of the characteristics of and risk factors for early-onset diabetes is fundamental to the development of better strategies for the prevention and management of this disease. Studies in hospital settings indicate that early-onset diabetes patients have more extensive family history of diabetes, and higher body mass index (BMI), Haemoglobin A1c (HbA1c), and low-density lipoprotein cholesterol (LDL-C) level in Western countries and Asia13,14, although there are disputes regarding the significance of these differences15. Large hospital based studies in China suggested early-onset diabetes participants had lower SBP, lower LDL-C, higher HbA1c and similar BMI and triglyceride levels compared with late-onset diabetes participants3. Selection bias in hospital-based studies is usually inevitable, particularly when using healthy participants who are recruited from hospitals as controls. Applying the study results from a hospital-based study to the general population, and also to diabetes at an elementary stage is also difficult16. Understanding the pathophysiology of newly diagnosed early-onset diabetes is useful for clinical decision making. It was reported that insulin resistance assessed by HOMA-IR was independently positively associated with age in newly diagnosed diabetes17. Beta cells function declines by 50–60% prior to T2DM diagnosis and the reduction happens before hyperglycaemia is present according to The UK Prospective Diabetes Study (UKPDS)18. However, whether the beta cell function in adult newly diagnosed early-onset diabetes participants is more impaired than late-onset diabetes is unknown. There are no population-based studies that address the clinical and pathophysiological characteristics of newly diagnosed early-onset diabetes patients. The current study aimed to explore the characteristics of and potential risk factors for newly diagnosed early-onset diabetes using the data from the China National Diabetes and Metabolic Disorders Study.
Methods
The China National Diabetes and Metabolic Disorders Study was a national cross-sectional survey of Chinese participants aged 20–75 years conducted from June 2007 to May 2008. This study recruited 47,325 subjects (18,976 men and 28,349 women) using a complex multistage stratified sampling method according to geographical region, economic development status, and degree of urbanization. Complete oral glucose tolerance test (OGTT) data and demographic information were collected in 46,239 adults. 43,864 participants without previously diagnosed diabetes or pre-diabetes, as defined by self-reporting anti-diabetes treatment or a diabetes or pre-diabetes history, were included in the final analysis. The design, protocol, and major epidemiological findings of this study have been previously published19.
The institutional review board or independent ethics committee of each participating institution approved this study protocol. The institutes included Peking University People’s Hospital, Beijing, China-Japan Friendship Hospital, Beijing, Chinese People’s Liberation Army General Hospital, Beijing, Sun Yat-sen University Third Hospital, Guangzhou, Shanghai Jiaotong University Affiliated Sixth People’s Hospital, Shanghai, First Affiliated Hospital, Chinese Medical University, Liaoning, Shanxi Province People’s Hospital, Taiyuan, Shanxi, West China Hospital, Sichuan University, Chengdu, Sichuan, Xijing Hospital, Fourth Military Medical University, Xi’an, Shaanxi, Affiliated Drum Tower Hospital of Nanjing University Medical School, Nanjing, Jiangsu, Xinjiang Uygur Autonomous Region’s Hospital, Urumqi, Xinjiang, Fujian Provincial Hospital, Fuzhou, Fujiang, Qilu Hospital of Shandong University, Jinan, Shandong, Peking University First Hospital, Beijing, Henan Province People’s Hospital, Zhengzhou, Henan, Second Affiliated Hospital of Harbin Medical University, Harbin, Heilongjiang and Xiangya Second Hospital, Changsha, Hunan. All methods were performed in accordance with the relevant guidelines, and informed consent was obtained from each subject prior to data collection.
Trained and qualified physicians completed questionnaire surveys and physical examinations in person during on-site surveys. Each subject completed a standard questionnaire on demographic characteristics, lifestyle, and medical history. Annual family income was categorized as less than 10,000 RMB or 10,000 RMB and greater. Education was divided into two groups according to the highest degree achieved by participants, namely, college education or higher and high school and lower. Smoking status was divided into current smokers who smoked every day and non-current smokers who never smoked or smoked previously or occasionally. Information on family history of diabetes, cardiovascular disease, and hypertension was collected based on the medical history of first-degree relatives (e.g., parents, siblings, and children). Height and weight were measured using a height-weight scale with subjects standing in bare feet in light clothing. Body mass index (BMI) was calculated as weight divided by height squared. Waist circumference was measured as the minimum circumference between the subcostal margin and the iliac crest. Blood pressure was measured twice with a 30-second interval between measurements using a mercury sphygmomanometer, and the mean pressure was recorded.
Participants were instructed to avoid excessive exercise and diet control for at least 3 days prior to the OGTT. Participants with no self-reported history of diabetes or diabetes treatments received a 75-g glucose solution (200 ml) after an overnight fast. Blood specimens were collected for insulin and glucose tests after fasting and 30 and 120 minutes after a glucose load or meal.
Plasma glucose was measured using the hexokinase method. Fasting total cholesterol (CHO), triglyceride (TG), high density lipoprotein cholesterol (HDL-C), and low density lipoprotein cholesterol (LDL-C) were measured enzymatically in each biochemical laboratory that met national or provincial quality standards. Specimens were transported on ice to the Central Laboratory of Endocrinology at the China-Japan Friendship Hospital for serum insulin level measurements using radioactive immunoassays. Random urine creatinine and microprotein were measured in the Central Laboratory using the picric acid method and enzymatic method, respectively. The urine albumin to creatinine ratio (ACR) was calculated as the urine microprotein (mg/L) divided by urinary creatinine (g/L).
Variable definition
Diabetes was defined as a FPG level ≥7.0 mmol/L or a 2 hPG ≥11.1 mmol/L according to the World Health Organization (WHO) diagnostic criteria of 199920. The following two parameters were calculated to evaluate insulin resistance: (1) the HOMA-IR, which primarily indicates hepatic insulin resistance, was calculated as FIN (mU/ml) × FPG (mmol/L)/22.57; and (2) the Matsuda insulin sensitivity index (Matsuda index), which represents whole-body insulin sensitivity, was calculated as 10,000/ ((18 × FPG (mmol/L) × FIN (mU/L) × OGTT average glucose (mmol/L) × OGTT mean insulin (μU/ml))1/2 21. Beta cell function and insulin release were assessed as follows: (1) the HOMA-B: 20 FIN (μU/ml)/(FPG (mmol/L)-3.5); (2) the insulinogenic index (ΔI30/ΔG30), which reflects early-phase insulin secretion after glucose challenge: (INS30 - FIN) (μU/ml)/(PG30 - FPG) (mmol/L), where INS30 and PG 30 refer to insulin and glucose levels 30 minutes after the glucose load, respectively; (3) glucose-corrected insulin area under the curve, which was the glucose-adjusted insulin release: InsAuc30/GluAuc 30 = [FIN (mU/L) + INS30 (mU/L)]/[FPG (mmol/L) + PG30 (mmol/L)] and InsAuc120/GluAuc120 = [FIN (mU/L) + 4 × INS30 (mU/L) + 3 × INS120 (mU/L)]/[FPG(mmol/L) + 4 × PG30 (mmol/L) + 3 × 2 hPG (mmol/L)], where 2 hPG and INS120 refer to glucose and insulin levels 2 hours after glucose loading, respectively; and 4) the disposition index (DI), which indicates the insulin secretion corrected by insulin sensitivity: DI30 = InsAuc30 × Matsuda index and DI120 = InsAuc120 × Matsuda index22. The decline in beta cell function and DI in early- and late-onset diabetes participants was compared with that in their non-diabetes peers in the same age groups. For example, the percentage of HOMA-B decline in early-onset diabetes participants (A) and young non-diabetes participants (B) was evaluated using the equation (B-A)/B*100.
Statistical analysis
Statistical analysis was performed using SPSS for Windows 19.0 software (SPSS Inc., Chicago, IL, USA). Newly diagnosed diabetes participants were divided into quartiles: diabetes onset at 20–43 years, 44–52 years, 53–61 years and more than 61 years. The first age group was defined as early-onset diabetes and the last group was defined as late-onset diabetes. Continuous variables are presented as the mean (95% confidence interval [CI]) or geometric means (95% CI). Categorical data are presented as numbers (%). Differences in mean values between groups were tested using analysis of variance (UNI-ANOVA) with Bonferroni correction. The chi-square test followed by post hot Bonferroni test was used to assess the differences between frequencies. The criteria for significance of multiple comparison was adjusted using Bonferroni correction. Binary logistic regression using 3 different models was used to assess the odds ratio for each risk factor for early-onset diabetes in reference to late-onset diabetes. The criteria for significance for regression was adjusted using Bonferroni correction.
Results
A total of 2,801 participants were diagnosed with diabetes based on the results of the oral glucose tolerance test (OGTT) in 43,864 adults aged 20 years and older. Among all the newly diagnosed diabetes participants, 654 (23.3%) participants were classified as having early-onset diabetes (age < = 43 years).
Characteristics of newly diagnosed early-onset diabetes participants
Newly diagnosed early-onset diabetes participants included a higher proportion of males and high income participants than participants who had diabetes onset at 53 years or later. They had more well educated participants than any other age group. The prevalence of cardiovascular disease (CVD) was lower in the early-onset diabetes group compared with participants who had diabetes onset at 53 years or later. There was no difference in family history of hypertension, diabetes and CVD between early-onset diabetes participants and any of the other three age groups. The BMI was similar across all 4 age groups after adjusting for sex, but early-onset diabetes participants had smaller waist circumstances than participants who had diabetes onset at 44 years or later. Early onset diabetes participants had the lowest SBP and DBP among all age groups and lower total cholesterol and LDL-C levels compared with participants had diabetes onset at 53 years or later. There was no difference in TG levels between early diabetes participants and any other age groups. The urine ACR were decreased in early-onset diabetes referring to late-onset diabetes participants. Early-onset diabetes participants had a lower 2-hour postprandial plasma glucose (2 hPG) and higher FPG. Early onset diabetes participants had higher fasting insulin than participants with diabetes onset between 44–61 years and lower 2-hour postprandial insulin (IN2h) values than late-onset diabetes participants. A higher percentage of diabetes diagnoses were made based on a FPG value ≥7.1 mmol/L alone and a lower percentage of diagnoses were made based on a 2 hPG value ≥11.1 mmol/L alone in early-onset diabetes participants. Higher HOMA-IR and DI30, and unaltered DI120 levels, Matsuda index and HOMA-B values were observed in the early-onset diabetes participants (Table 1).
The change in insulin secretion and beta cell function in early- onset diabetes participants
The declination of insulin secretion and beta cell function was enhanced in early-onset diabetes compared with participants had diabetes onset later than 44 years. DI30 decreased by 67.4% (65.5%, 65.3%), 65.3% (63.5%, 67.1%), 65.3% (63.5%, 67.1%) and 63.5% (61.6%, 65.4%) in the early-onset diabetes participants, participants with diabetes onset between 44–52 years, participants with diabetes onset between 53–61 years and late-onset diabetes participants, respectively (p = 0.04). DI120 decreased by 65.7% (63.8%, 67.6%), 61.7% (59.8%, 63.6%), 62.8 (60.9, 64.6%) and 60.9 (59.0%, 62.8%) in the four consecutive age groups (p = 0.003). Beta cell function as assessed by HOMA-B decreased by 59.6% (50.5%, 68.8%), 40.9% (31.9%, 49.8%), 40.5% (31.6%, 49.5%) and 44.3% (35.3%, 53.3%) (p = 0.01).
Risk factors for participants with early-onset diabetes compared with participants with diabetes onset after 44 years
A logistic regression analysis using different models was performed to calculate the odds ratio for developing early-onset diabetes compared with participants with diabetes onset at 44 years or later. After adjusting for cardiovascular risk factors and metabolic parameters, male gender resulted in an increased odds ratio (OR) for diabetes diagnosis at an earlier age. Per standard deviation (SD) elevation of triglyceride level, HOMA-IR and DI30 values increased the odds ratio for early-onset diabetes by 15%, 17% and 24%, respectively. Per SD increase of SBP led to an approximate 50% decrease in the OR for early-onset diabetes. BMI, current smoking, diabetes family history were not independent early-onset diabetes risk factors. (Table 2).
Discussion
This large, multi-centre, cross-sectional, population-based study in China revealed that the occurrence of early-onset diabetes was 23.3% among newly diagnosed diabetes patients. Early-onset diabetes participants were characterized by lower blood pressure and LDL-C levels, similar BMI, triglycerides and HOMA-B values, increased HOMA-IR and DI30 values and a more profound loss of beta cell function than late-onset diabetes and/or middle-age-onset participants. Male gender, higher triglycerides, higher HOMA-IR, higher DI30, and lower SBP were independently associated with a diabetes diagnosis at an earlier age.
This study suggested there was a high prevalence of newly-diagnosed diabetes participants in China. This is consistent with another large population based study, the China Non-communicable Disease Surveillance 2010 survey5, which revealed that newly diabetes participants aged 18–40 years accounted for 15.7% of all newly diagnosed diabetes cases as determined by the OGTT. This proportion is much higher than the IDF-predicted values in Australia, the UK, and Japan2. These alarming findings from the two large-scale population-based epidemiological studies in China indicated that diabetes in the young population had reached pandemic proportions. An imminent and effective action for the prevention of diabetes in young people should be implemented in this country.
Our results that early-onset diabetes participants had a similar ‘cardio-risk’ phenotype to middle-age and late-onset diabetes participants. This was partly inconsistent with other studies, which were all hospital based studies, demonstrating that early-onset diabetes had a similar or adverse cardiovascular profile. Although the genetics associated with type 2 diabetes was different between Westerners and Asians2, this discrepancy may not be completely due to ethnicity difference among these studies. Unchanged BMI, decreased LDL-C, increased blood glucose levels and reduced SBP was found not only in our study, but also in American newly diagnosed early-onset diabetes participants from Kaiser Permanente Northwest Division (KPNW) and Chinese early-onset diabetes participants from the China National HbA1C Surveillance System3,7. However, Joint Asia Diabetes Evaluation (JADE) study, which recruited 41,029 Asian participants and 10% of them were from China, suggested the BMI, LDL-C and TG levels were higher in early-onset diabetes participants13.
Sample selection could be one explanation for the discrepancy between our study and other studies which was the difference between hospital- and population-based studies. Hospital-based recruitment may be limited to people who can afford healthcare and those with severe symptoms. In contrast, population-based screening is advantageous for identifying individuals with less severe cases of diabetes and covering areas with a shortage of medical resources. By this means, our study has the increased external validity related to reduced recruitment bias.
Another reason for the discrepancy could be the length of risk factor exposure in these participants. Early-onset diabetes participants had a 100% increase in macrovascular complications23 and a 69% increase in microvascular complications11 at any given age, and this risk was greatly associated with disease duration11,24. It is possible that even the cardiovascular risk factors were similar between early-onset and late-onset diabetes, the exposure of these risk factors were much longer in early-onset diabetes due to longer life expectancy in these people. In fact, the atherosclerosis progression was determined by the same factors including smoking, hypertension, obesity and dyslipidaemia in both young and old individuals25. As a cross-sectional study, we were unable to measure the exposure period of these risk factors and how they contribute the the disease progression.
Young age is a remarkable protective factor for cardiovascular disease and cardiovascular risk factors such as high blood pressure, dyslipidaemia, obesity and high blood glucose26. Our study suggested these protective effects of youth were at least partly lost in early-onset diabetes participants. The absence of the ‘cardio-protective’ phenotype in newly diagnosed early-onset diabetes patients puts these patients at the same risk of developing cardiovascular disease as the middle-age-onset or late-onset diabetes participants. More social and clinical attention is necessary to develop policies and prevention and management strategies for participants with early-onset diabetes who have had the disease for a prolonged period of time.
Although age per se is an independent factor negatively associated with beta cell function in non-diabetes participants27, beta cell function, as indicated by HOMA-B, was unaltered among different age groups in this study. The early-onset diabetes had increased first phase insulin release but similar late phase insulin release with late-onset diabetes. Similarly, clamp studies with small sample size suggested there was no difference in either early phase nor late phase insulin release between middle-aged and old diabetes participants28. Our study also demonstrated that the magnitude of the decline in beta cell function was greater in early-onset diabetes than in middle age onset and late-onset diabetes when age-matched non-diabetes peers were used as a reference. Our study also has the advantage of being able to compare the characteristics of early-onset diabetes participants with their non-diabetes peers in the appropriate context because of complete data collection. This is consistent with previous findings that beta cell function declined more rapidly in early-onset diabetes (15% per year)29 later onset subjects (6% per year)30. A more severe decline in beta cell function may cause a quicker switch from oral anti-diabetes drugs to insulin injections in early-onset diabetes participants. This explains why early-onset type 2 diabetes was associated with a higher proportion of participants receiving insulin injections, even after adjustment was made for disease duration13.
A higher proportion of early-onset diabetes participants elevated fasting glucose levels alone than diabetes participants with disease onset at 44 years or later. This result supported the finding that hepatic insulin resistance, as indicated by HOMA-IR, was elevated in early-onset diabetes patients in this study because fasting hyperglycaemia is highly associated with hepatic insulin resistance31. However, the Matsuda index, which reflects both hepatic and muscle insulin sensitivity32, was unaltered among all age groups possibly because the muscle insulin sensitivity was similar between the two patient groups. This result was in contrast to previous findings that a mild positive association between age and HOMA-IR was detected in newly diagnosed diabetes participants in UKPDS17. Again, this could be owing to the different recruitment strategy between our study and UKPDS. Another possible reason for this result may involve an increase in inflammation, fatty liver, which are other determinants of insulin resistance in addition to age, BMI, and lipid levels33, in early-onset diabetes Chinese individuals.
Previous studies suggested that a family history of diabetes greatly increased the odds ratio for developing diabetes at an earlier age34. Our study suggested that diabetes family history was not significantly different between early- and other participants. A study using the same data set demonstrated that the risk of development of diabetes increased as the number of first-degree relatives with diabetes increased for any given participant. However, this risk increased evenly in both young and old participants35.
There are some limitations of this study. First, because of the cross-sectional design of this study, the clinical implication of the observed characteristics in early-onset diabetes participants is not known. Prospective cohort studies are necessary to observe the natural history of newly diagnosed early-onset diabetes patients. Second, the impact of aetiological heterogeneity on the clinical characteristics of early-onset diabetes in our study could not be addressed because of the lack of investigation using factors such as autoimmune markers. However, the prevalence of latent autoimmune diabetes in adults (LADA) was relatively low (5.9%) and consistent across different age groups36. Additionally, the impact of classic type 1 diabetes on our study could be ignored because classic type 1 diabetes is a relatively rare condition in the Chinese population37, and this condition is more likely to present in a clinical practice setting with classic symptoms, such as polydipsia, polyuria, weight loss, and ketonuria or ketone acidosis. Third, patients with known diabetes were excluded from this study because of incomplete data, leading to a shortage of participants with severe disease conditions and a long disease duration. Also, as a cross-sectional study, we were unable to include the length of exposure of all the cardiovascular risk factors. Further cohort studies involving these patients should be initiated to fill this knowledge gap.
Conclusion
Although newly diagnosed early-onset diabetes participants are more progressive to cardiovascular disease, our study suggested newly diagnosed early-onset diabetes had a similar cardiovascular risk profile with newly diagnosed middle-age and late- onset diabetes. Younger age at diabetes diagnosis was associated with increased insulin resistance and accelerated beta cell failure. The difference in the cardiovascular profiles of early-onset diabetes participants between our study and other hospital based studies may be owning to different sample recruitment strategies. Our study shed new light on the clinical characteristics of early-onset diabetes as a population based study.
Additional Information
How to cite this article: Zou, X. et al. The characteristics of newly diagnosed adult early-onset diabetes: a population-based cross-sectional study. Sci. Rep. 7, 46534; doi: 10.1038/srep46534 (2017).
Publisher's note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
Chan, J. N., Malik, V. & Jia, W. Diabetes in asia: Epidemiology, risk factors, and pathophysiology. Jama 301, 2129–2140, doi: 10.1001/jama.2009.726 (2009).
Ma, R. C. & Chan, J. C. Type 2 diabetes in East Asians: similarities and differences with populations in Europe and the United States. Annals of the New York Academy of Sciences 1281, 64–91, doi: 10.1111/nyas.12098 (2013).
Huo, X. et al. Risk of non-fatal cardiovascular diseases in early-onset versus late-onset type 2 diabetes in China: a cross-sectional study. The Lancet Diabetes & Endocrinology 4, 115–124, doi: 10.1016/S2213-8587(15)00508-2 (2016).
Cowie, C. C. et al. Full Accounting of Diabetes and Pre-Diabetes in the U.S. Population in 1988–1994 and 2005–2006. Diabetes Care 32, 287–294, doi: 10.2337/dc08-1296 (2009).
Xu, Y., Wang, L. & He, J. et al. PRevalence and control of diabetes in chinese adults. Jama 310, 948–959, doi: 10.1001/jama.2013.168118 (2013).
Constantino, M. I. et al. Long-term complications and mortality in young-onset diabetes: type 2 diabetes is more hazardous and lethal than type 1 diabetes. Diabetes Care 36, 3863–3869, doi: 10.2337/dc12-2455 (2013).
Hillier, T. A. & Pedula, K. L. Characteristics of an adult population with newly diagnosed type 2 diabetes: the relation of obesity and age of onset. Diabetes Care 24, 1522–1527 (2001).
Chan, J. C. N. et al. Premature Mortality and Comorbidities in Young-onset Diabetes: A 7-Year Prospective Analysis. The American Journal of Medicine 127, 616–624, doi: 10.1016/j.amjmed.2014.03.018 (2014).
Rhodes, E. T. et al. Estimated morbidity and mortality in adolescents and young adults diagnosed with Type 2 diabetes mellitus. Diabetic Medicine 29, 453–463, doi: 10.1111/j.1464-5491.2011.03542.x (2012).
Chuang, L.-M. et al. Comparisons of the outcomes on control, type of management and complications status in early-onset and late-onset type 2 diabetes in Asia. Diabetes Research and Clinical Practice 71, 146–155, doi: 10.1016/j.diabres.2005.05.007 (2006).
Li, L. et al. Prevalence of microvascular diseases among tertiary care Chinese with early versus late-onset of type 2 diabetes. Journal of Diabetes and its Complications 29, 32–37, doi: 10.1016/j.jdiacomp.2014.08.010 (2015).
Song, S. H. & Hardisty, C. A. Early-onset Type 2 diabetes mellitus: an increasing phenomenon of elevated cardiovascular risk. Expert Review of Cardiovascular Therapy 6, 315–322, doi: 10.1586/14779072.6.3.315 (2008).
Yeung, R. O. et al. Metabolic profiles and treatment gaps in young-onset type 2 diabetes in Asia (the JADE programme): a cross-sectional study of a prospective cohort. The Lancet Diabetes & Endocrinology 2, 935–943, doi: 10.1016/S2213-8587(14)70137-8 (2014).
Hatunic, M., Burns, N., Finucane, F., Mannion, C. & Nolan, J. J. Contrasting clinical and cardiovascular risk status between early and later onset type 2 diabetes. Diabetes & vascular disease research 2, 73–75, doi: 10.3132/dvdr.2005.012 (2005).
Gunathilake, W., Song, S., Sridharan, S., Fernando, D. J. & Idris, I. Cardiovascular and metabolic risk profiles in young and old patients with type 2 diabetes. Qjm 103, 881–884, doi: 10.1093/qjmed/hcq135 (2010).
Grimes, D. A. & Schulz, K. F. Bias and causal associations in observational research. The Lancet 359, 248–252, doi: 10.1016/S0140-6736(02)07451-2 (2002).
Adler, A. I. et al. Insulin sensitivity at diagnosis of Type 2 diabetes is not associated with subsequent cardiovascular disease (UKPDS 67). Diabetic medicine: a journal of the British Diabetic Association 22, 306–311, doi: 10.1111/j.1464-5491.2004.01418.x (2005).
UKPDS. U. K. prospective diabetes study 16. Overview of 6 years' therapy of type II diabetes: a progressive disease. U.K. Prospective Diabetes Study Group. Diabetes 44, 1249–1258 (1995).
Yang, W. et al. Prevalence of diabetes among men and women in China. The New England journal of medicine 362, 1090–1101, doi: 10.1056/NEJMoa0908292 (2010).
WHO. Definition, Diagnosis and Classification of Diabetes Mellitus and its Complications Report of a WHO Consultation Part 1: Diagnosis and Classification of Diabetes Mellitus, Geneva, World Health Organization Department of Noncommunicable Disease Surveillance. WHO/NCD/NCS/99.2 (1999).
Hu, H. et al. Increased circulating levels of betatrophin in newly diagnosed type 2 diabetic patients. Diabetes Care 37, 2718–2722, doi: 10.2337/dc14-0602 (2014).
Retnakaran, R., Qi, Y., Goran, M. I. & Hamilton, J. K. Evaluation of proposed oral disposition index measures in relation to the actual disposition index. Diabetic medicine: a journal of the British Diabetic Association 26, 1198–1203, doi: 10.1111/j.1464-5491.2009.02841.x (2009).
Hillier, T. A. & Pedula, K. L. Complications in Young Adults With Early-Onset Type 2 Diabetes: Losing the relative protection of youth. Diabetes Care 26, 2999–3005, doi: 10.2337/diacare.26.11.2999 (2003).
Burns, N. et al. Early-onset type 2 diabetes in obese white subjects is characterised by a marked defect in beta cell insulin secretion, severe insulin resistance and a lack of response to aerobic exercise training. Diabetologia 50, 1500–1508, doi: 10.1007/s00125-007-0655-7 (2007).
Strong, J. P. et al. Prevalence and extent of atherosclerosis in adolescents and young adults: implications for prevention from the Pathobiological Determinants of Atherosclerosis in Youth Study. Jama 281, 727–735 (1999).
Nowbar, A. N., Howard, J. P., Finegold, J. A., Asaria, P. & Francis, D. P. 2014 global geographic analysis of mortality from ischaemic heart disease by country, age and income: statistics from World Health Organisation and United Nations. International journal of cardiology 174, 293–298, doi: 10.1016/j.ijcard.2014.04.096 (2014).
Basu, R. et al. Mechanisms of the age-associated deterioration in glucose tolerance: contribution of alterations in insulin secretion, action, and clearance. Diabetes 52, 1738–1748 (2003).
Meneilly, G. S. & Elahi, D. Metabolic Alterations in Middle-Aged and Elderly Lean Patients With Type 2 Diabetes. Diabetes Care 28, 1498–1499, doi: 10.2337/diacare.28.6.1498 (2005).
Gungor, N., Bacha, F., Saad, R., Janosky, J. & Arslanian, S. Youth type 2 diabetes: insulin resistance, beta-cell failure, or both? Diabetes Care 28, 638–644 (2005).
Matthews, D. R., Cull, C. A., Stratton, I. M., Holman, R. R. & Turner, R. C. UKPDS 26: Sulphonylurea failure in non-insulin-dependent diabetic patients over six years. UK Prospective Diabetes Study (UKPDS) Group. Diabetic medicine: a journal of the British Diabetic Association 15, 297–303, doi: 10.1002/(sici)1096-9136(199804)15:4<297::aid-dia572>3.0.co;2-w (1998).
Bi, Y. et al. Association of beta-cell function and insulin sensitivity with fasting and 2-h plasma glucose in a large Chinese population. Diabetes, obesity & metabolism 14, 174–180, doi: 10.1111/j.1463-1326.2011.01504.x (2012).
Kim, M. K. Clinical characteristics of OGTT-derived hepatic- and muscle insulin resistance in healthy young men. Journal of exercise nutrition & biochemistry 18, 385–392, doi: 10.5717/jenb.2014.18.4.385 (2014).
Ye, J. Mechanisms of insulin resistance in obesity. Frontiers of medicine 7, 14–24, doi: 10.1007/s11684-013-0262-6 (2013).
Consortium, T. I. The link between family history and risk of type 2 diabetes is not explained by anthropometric, lifestyle or genetic risk factors: the EPIC-InterAct study. Diabetologia 56, 60–69, doi: 10.1007/s00125-012-2715-x (2012).
Zhang, J. et al. Association between Family History Risk Categories and Prevalence of Diabetes in Chinese Population. PLoS One 10, e0117044, doi: 10.1371/journal.pone.0117044 (2015).
Zhou, Z. et al. Frequency, Immunogenetics, and Clinical Characteristics of Latent Autoimmune Diabetes in China (LADA China Study): A Nationwide, Multicenter, Clinic-Based Cross-Sectional Study. Diabetes 62, 543–550, doi: 10.2337/db12-0207 (2013).
Lin, W. H. et al. Incidence of and mortality from Type I diabetes in Taiwan from 1999 through 2010: a nationwide cohort study. PLoS One 9, e86172, doi: 10.1371/journal.pone.0086172 (2014).
Acknowledgements
We give our greatest gratitude to the China National Diabetes and Metabolic Disorders Study Group who design and performed this study and the clinicians who performed the field studies. This study was supported by grants from the Chinese Medical Association Foundation and Chinese Diabetes Society, the National Key Technologies R&D Program of China (2009BAI80B02), and the National High-Tech R&D Program of China (863 Program 2012AA02A509). No potential conflicts of interest relevant to this article are reported. Grant 2016YFC1305600, 2016YFC1305603 from the Major Chronic Non-communicable Disease Prevention and Control Research Key Project of the Ministry of Science and Technology of the People’s Republic of China. This was the funding for Xiantong Zou and Xianghai Zhou from 2016 when they did part of this study.
Author information
Authors and Affiliations
Contributions
Xiantong Zou analysed the data and wrote the majority of the manuscript. Xianghai Zhou participated in the study design, data analysis, and manuscript review. Linong Ji designed the study and edited the manuscript. Linong Ji, Wenying Yang, Juming Lu, Jianping Weng, Weiping Jia, Zhongyan Shan, Jie Liu, Haoming Tian, Qiuhe Ji, Dalong Zhu, Jiapu Ge, Lixiang Li, Li Chen, Xiaohui Guo, Zhigang Zhao, Qiang Li, and Zhiguang Zhou contributed to the data collection. All authors read the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing financial interests.
Rights and permissions
This work is licensed under a Creative Commons Attribution 4.0 International License. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in the credit line; if the material is not included under the Creative Commons license, users will need to obtain permission from the license holder to reproduce the material. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/
About this article
Cite this article
Zou, X., Zhou, X., Ji, L. et al. The characteristics of newly diagnosed adult early-onset diabetes: a population-based cross-sectional study. Sci Rep 7, 46534 (2017). https://doi.org/10.1038/srep46534
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/srep46534
This article is cited by
-
Clinical characteristics of patients with early-onset diabetes mellitus: a single-center retrospective study
BMC Endocrine Disorders (2023)
-
Pathophysiology, phenotypes and management of type 2 diabetes mellitus in Indian and Chinese populations
Nature Reviews Endocrinology (2022)
-
Maximum likelihood estimation for length-biased and interval-censored data with a nonsusceptible fraction
Lifetime Data Analysis (2022)
-
Population segmentation of type 2 diabetes mellitus patients and its clinical applications - a scoping review
BMC Medical Research Methodology (2021)
-
Vitamin D concentrations from neonatal dried blood spots and the risk of early-onset type 2 diabetes in the Danish D-tect case-cohort study
Diabetologia (2021)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.