Abstract
Most guidelines for the diagnosis and management of thyroid nodules have suggested fine-needle aspiration as a diagnostic tool, with some of these previously published guidelines suggesting a cutoff size of 1.5 cm. In thyroid cancers (1–2 cm), we hypothesized that tumors 1.5 cm or larger had more unfavorable clinical outcomes than ones smaller than 1.5 cm nodules. Using the Surveillance, Epidemiology, and End Results database, we identified 14,117 patients diagnosed with only primary thyroid cancer between 1988 and 2007. After multivariable adjustment, we found that having a tumor 1.5 cm or larger in size was not associated with distant metastasis [adjusted odds ratio, 1.18; 95% confidence interval (CI), 0.95 to 1.48; P = 0.14] or the two causes of death (adjusted subdistributional hazard ratio (SDHR), 1.40; 95% CI, 0.96 to 2.04; P = 0.08 for thyroid cancer mortality; adjusted SDHR, 1.06; 95% CI, 0.88 to 1.27; P = 0.55 for noncancer mortality). Using a population-based cohort, in patients with primary thyroid cancer with a tumor size of 1.5–2 cm, there was no increased association with distant metastasis or probability of death, when compared with patients with primary thyroid cancer with a tumor size of 1.0–1.5 cm.
Similar content being viewed by others
Introduction
With the increased use of imaging studies, especially high-resolution ultrasonography (US), the number of thyroid nodules detected has rapidly increased1,2. While it is crucial not to miss cancers among these detected thyroid nodules, it is also critically important to detect and diagnose cancers which may be clinically significant. Fine-needle aspiration (FNA) is the standard method used to diagnose thyroid nodules detected on US, and it is known to be both accurate and cost-effective3,4. Although there have been several guidelines that recommend FNA for thyroid nodules3,5,6,7,8,9, a worldwide consensus on indications for FNA of thyroid nodules has not yet been achieved.
Because distant metastases can occur in patients with thyroid cancers larger than 2 cm, all nodules larger than 2 cm except simple cysts are recommended for FNA even if they have very few suspicious US features3,6,8,10. Also, most guidelines do not recommend FNA for thyroid nodules smaller than 1 cm except in high risk patients because most papillary microcarcinomas without unfavorable features have no clear negative outcomes11,12. For thyroid nodules 1–2 cm in size, most guidelines suggest FNA based on the size and US features of the thyroid nodule3,5,6,8. The Society of Radiologists in Ultrasound (SRU), the National Comprehensive Cancer Network, and the American Thyroid Association use a size cutoff of 1.5 cm according to how suspicious the thyroid nodules appear on US;3,5,6,8 however, the guidelines of the American Association of Clinical Endocrinologists/Associazione Medici Endocrinologi/European Thyroid Association do not consider a size cutoff of 1.5 cm9. Using a 1.5 cm size cutoff along with US features as an indication for FNA can be burdensome in real practice. Taking into account that guidelines should be easily applicable in clinical practice, a less complicated subclassification system/algorithm is required to indicate which nodules need FNA. Recently, the diagnostic performances and abilities of six major worldwide guidelines to identify aggressive cancers were compared for patients with small thyroid nodules13. Although there were no significant associations between positive findings that indicated FNA and distant metastasis, recurrence or persistence, the study power of this previous study was too low to detect significant differences. With a population-based cohort, we sought to find an association with distant metastasis or thyroid cancer mortality using a size cutoff of 1.5 cm in patients with small thyroid cancers between 1 cm and 2 cm. We hypothesized that among thyroid nodules 1 cm or larger but smaller than 2 cm, nodules 1.5 cm or larger had more unfavorable clinical outcomes than ones smaller than 1.5 cm. We thought that our research could help provide potential evidence to support the 1.5 cm size cutoff as an indication for FNA.
Results
Patient Characteristics
Table 1 lists patient demographics and clinical characteristics according to tumor size. The significant factors between the tumor size groups (group 1: 1–1.4 cm, group 2: 1.5–1.9 cm) were as follows; histologic subtype, extrathyroidal extension, cervical lymph node metastasis, distant metastasis, and radiation therapy. The number of patients 55 years or older for group 1 and group 2 were 1653 (22.2%) and 1395 (20.9%), respectively. The rates of extrathyroidal extension, cervical lymph node metastasis and distant metastasis in group 2 were 17.1%, 64.9% and 2.7%, respectively.
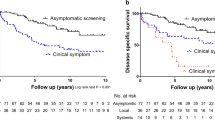
The cumulative incidence over the entire follow-up time was significantly different between the tumor size subgroups among patients who died of thyroid cancer-related causes (P = 0.02), but was not different among patients who died of noncancer causes (P = 0.85).
The most frequent causes of noncancer mortality were heart disease (31.2%), other causes (18.3%), cerebrovascular diseases (8.1%), and chronic obstructive pulmonary disease (6.3%). The median follow-up time in group 1 and group 2 was 105 months (range, 0 to 299 months) and 110 months (range, 0 to 299 months), respectively.
Distant Metastasis
At univariable analysis, group 2 was associated with increased risk of distant metastasis compared to group 1 (OR, 1.65; 95% CI, 1.08 to 1.68; P = 0.008). Other significant risk factors for distant metastasis were male sex, other thyroid carcinoma except papillary or follicular carcinomas, extrathyroidal extension, cervical lymph node metastasis, surgery type (no surgery, total thyroidectomy v lobectomy), and radiation therapy. Multivariable analysis showed that group 2 was not significantly associated with the risk of distant metastasis compared to group 1 after adjustment for patient demographics and clinical characteristics (adjusted OR, 1.19; 95% CI, 0.95 to 1.49; P = 0.13) (Table 2).
We also performed subgroup analyses according to an age cutoff of 55 years to identify groups associated with distant metastasis (Table 3). In univariable analysis, group 2 was significantly associated with distant metastasis when patients were younger than 55 years (OR, 1.39; 95% CI, 1.08 to 1.78; P = 0.01), but was not significantly associated with distant metastasis when patients were 55 years or older (OR, 1.22; 95% CI, 0.77 to 1.93; P = 0.39). Multivariable analyses showed that group 2 was not significantly associated with distant metastasis for both age groups, for both patients 55 years or older (adjusted OR, 0.88; 95% CI, 0.54 to 1.45; P = 0.62) and patients younger than 55 years (adjusted OR, 1.27; 95% CI, 0.99 to 1.63; P = 0.06), after adjustment for patient and tumor characteristics.
Competing Risk Analysis
The cumulative incidence curves are shown in Fig. 1. For thyroid cancer-specific mortality, the 5-year cumulative incidences of death for group 1 and group 2 were 0.51% and 0.57%, the 10-year cumulative incidences were 0.64% and 1.16%, the 15-year cumulative incidences were 0.69% and 1.51%, and the 20-year cumulative incidences were 1.07% and 1.61%, respectively. For noncancer deaths, the 5-year cumulative incidences of death for group 1 and group 2 were 1.34% and 1.26%, the 10-year cumulative incidences were 3.23% and 2.86%, the 15-year cumulative incidences were 5.16% and 4.53%, and the 20-year cumulative incidences were 6.87% and 8.46%, respectively.
On univariable analysis, the risk of thyroid cancer-related mortality was significantly increased in group 2 than in group 1, whereas the risk of noncancer mortality was not significantly associated with both groups (Table 4). In patients younger than 55 years, group 2 was not significantly associated with thyroid cancer-specific mortality, or noncancer mortality, but it was significantly associated with increased thyroid cancer-specific mortality for patients 55 years or older (Table 3).
On multivariable analysis, group 2 did not significantly increase thyroid cancer-related mortality or noncancer mortality (Table 5). Increased thyroid cancer-specific mortality was associated with patient age 55 years or older, male sex, cancers other than papillary carcinoma, extrathyroidal extension, cervical lymph node metastasis, distant metastasis, and no surgery. Significant risk factors for noncancer mortality were patient age 55 years or older, male sex, black race, no surgery, and radiation therapy (Table 5). Group 2 was not significantly associated with death resulting from thyroid cancer or noncancer causes on multivariable analyses in both age subgroups (Table 3).
Discussion
We found that a tumor size of 1.5 cm or larger in small thyroid nodules was not associated with death resulting from thyroid cancer or other noncancer causes and was not associated with distant metastasis on multivariable analyses using logistic regression and the subdistributional hazards models. These findings were consistent when patients were stratified according to age, with the newly updated cutoff of 55 years in the cancer staging system14. Significant differences for age disappeared between the two tumor size groups when a cutoff age of 55 years was applied rather than the traditional cutoff age of 45 years, and other results were not notably different (data not shown).
In this study, noncancer causes of death were treated as competing risk rather than censoring or all-cause mortality, because deaths due to causes unrelated to thyroid cancer interfere with the ability to observe deaths resulting from thyroid cancer. The effects of the covariates on multivariable models differ for each cause of death. Therefore, we treated deaths from noncancer causes as competing risk events. Another study using the SEER database found that patients with thyroid cancer who did not undergo surgical treatment were observed with a smaller 5-year overall survival rate, older age, advanced cancer stage, and more distant metastases; however, this study did not explain the reason for these differences because the SEER database does not offer information about comorbidities15. Our analysis incorporated competing risks using the COD variable in the SEER database instead of comorbidity information to infer the effects of noncancer causes of death. The results of our multivariable analysis suggest that patients who do not undergo surgery are at significantly high risk of noncancer mortality. The most common cause of noncancer mortality in our study was heart disease. Non-surgical patients might not be eligible for surgery because of their comorbidities, and this in turn, affected the occurrence of distant metastases and mortalities. We resolved these issues by the multivariable competing risks model which included non-surgical patients.
Thyroid cancer is the most common cancer among endocrine tumors and its incidence is increasing rapidly throughout the world16,17,18. The main cause of this increase is the rising number of incidentally detected thyroid nodules at imagings with US, computed tomography, and magnetic resonance imaging. Considering that most thyroid nodules are benign, it is important to identify and select nodules for which FNA is necessary. Most societies recommend FNA for nodules 1 cm or larger which also have the respective US features and for nodules 2 cm or larger except for those with a simple cyst3,6,7,8. Since the SRU recommended FNA for thyroid nodules, a size cutoff of 1.5 cm has been used to decide whether or not to perform FNA in accordance to each society’s US criteria3. The cutoff tumor size of 1.5 cm currently suggested by thyroid nodule management guidelines would be acceptable if cancers 1.5 cm or larger showed poorer clinical outcomes compared to tumors smaller than 1.5 cm. Some studies were cited in guidelines for FNA of thyroid nodules to support a size cutoff of 1.5 cm. A long-term study of 1,355 patients with thyroid cancers demonstrated that tumors smaller than 1.5 cm had lower 30-year recurrence and lower cancer mortality rates than tumors between 1.5 cm and 4.4 cm, and 4.5 cm or larger, respectively19. However, this study included cancers from 0.2 cm to 10 cm in size; thus, there was insufficient evidence to support using the 1.5 cm cutoff to indicate FNA for nodules 1–2 cm in size, as was suggested by previous guidelines. Although multivariable analyses with adjustment for patient and tumor characteristics were performed, tumor size was considered as continuous scale. Another study using the SEER database found that the 10-year relative survival rates for tumors sized 1.5 cm or larger and tumors less than 1.5 cm were 95.4% and 99.8%, respectively20. However, this study included thyroid cancers which were less than 5 mm to thyroid cancers 4 cm or larger; moreover, no adjustment was made for tumor and treatment characteristics.
Developing appropriate criteria to select which small thyroid nodules should undergo FNA is essential to prevent the risk of missing clinically significant cancers, to decrease the number of patients who undergo unnecessary FNAs, and to enhance user convenience. Established methodological standards and researches for developing guidelines have suggested that guideline features should be of high quality, be trustworthy, and be implementable21,22,23,24. Therefore, it is very surprising that there has been no evidence that proves that thyroid nodules 1.5 cm or larger have poorer clinical outcomes compared to nodule smaller than 1.5 cm when focusing on nodules 1 cm or larger but smaller than 2 cm. So far, a worldwide consensus on indications for FNA of thyroid nodules has not been achieved, making the need for logical evidence more crucial. Our study is the first population-based study to demonstrate that there is not enough evidence to support a cutoff tumor size of 1.5 cm for managing thyroid nodules after adjusting for patient, tumor, and treatment characteristics although this study cannot provide direct evidence for some guidelines which use a cutoff tumor size of 1.5 cm to indicate FNA for thyroid nodules.
This study has several strengths. By using the COD variable in the SEER database, we were able to classify specific causes of mortality, and were able to perform analyses with an adequate number of deaths occurring in thyroid cancer patients. Hence, the SEER database allows us to perform multivariable competing risk analyses adjusting for patient and tumor characteristics, and surgical treatments. The SEER data gave our study, a population-based long-term follow-up study, adequate statistical power that could not have been achieved by single institution studies. Also, results from a population-based SEER study have more generalizability and reliability.
Our study does have several limitations. The SEER database does not include detailed data on comorbidity, disease recurrence, and sonographic features which have been included in most FNA guidelines. External validations using well-constructed prospective multi-institutional data for thyroid nodules may provide relevant validity for various guidelines. Also, the SEER database might have some coding errors. Before constructing the study population, we first excluded patients who were classified as having thyroid cancer but recorded as having non-thyroid malignancy as the histological subtype. Information regarding COD in the SEER database is acquired from a patient’s death certificate, and there is a chance that this information might be misclassified. However, a previous study has found the COD coding in SEER to be highly accurate25.
In summary, we found that having a tumor 1.5 cm or larger in size was not associated with distant metastasis and the two causes of death (thyroid cancer mortality and noncancer mortality) after adjustment for patient, tumor, and clinical characteristics. Therefore, further studies using the 1.5 cm cutoff as an indication for FNA in thyroid nodules are needed.
Methods
SEER Database and Study Population
The Surveillance, Epidemiology, and End Results (SEER) database covers approximately 30% of the United States population26. We contacted the SEER program of the National Cancer Institute in August 2015. Our study only selected cases diagnosed after 1988 because information on extent of disease such as lymph node involvement, or detailed information on tumor size was required. 127512 patients with thyroid cancer (C73.9) as the first primary malignancy as well as histologically diagnosed tumors of the thyroid were identified according to the International Classification of Diseases for Oncology, 3rd Edition (ICD-O-3).
To include a minimum of 5 years of follow-up survival data, we only selected patients who were diagnosed up to 2007. Tumors with sizes equal to or larger than 2 cm or smaller than 1 cm were excluded. We excluded patients who were diagnosed with other cancers than thyroid cancer. Patients with no available information on race, surgical findings (extrathyroidal extension, lymph node involvement, surgery type), and radiation therapy were also excluded. Patients with a cause of death (COD) record that indicated an unavailable death certificate or patients with no records of survival time were excluded. Patients with this data but with no COD recorded (SEER code of 41000) were excluded as well. The final study cohort was comprised of 14117 patients with thyroid cancers.
Variables included age at diagnosis (55 years or older vs younger than 55 years), sex, race, extrathyroidal extension, cervical lymph node metastasis, distant metastasis, surgery type, and radiotherapy. The presence of distant metastasis was determined using the SEER historical staging system. Extent of surgery was grouped as no surgery, lobectomy, and total thyroidectomy including subtotal or near-total thyroidectomy.
Thyroid cancer-specific death was ascertained with the SEER COD record of 32010, and noncancer mortality was also defined. Survival time was determined from the SEER records on survival time, that is, from date of diagnosis to date of last contact. The date of last contact was as follows: for deaths, date of death; for survivors, the date of last contact if before December 31, 2012; or December 31, 2012, if date of last contact was after 2012.
Institutional review board approval was not required because data from the SEER program is publically available and anonymized.
Statistical Analyses
We divided the patients into two groups, group 1 (nodules 1 cm or larger and smaller than 1.5 cm) and group 2 (nodules 1.5 cm or larger and smaller than 2 cm). Patient demographics and clinical characteristics were compared between the two groups using Pearson χ2 test or Fisher’s exact test.
Univariable and multivariable logistic regression models were used to examine the effects of patient demographics and clinical characteristics for the presence of distant metastasis. Odds ratios (ORs) and 95% confidence intervals (CIs) were estimated.
Cumulative incidence curves for death in the presence of the competing risk were estimated and compared between the two groups by Gray’s method27. We used proportional subdistribution hazards regression modeling proposed by Fine and Gray to estimate the effects of the covariates on the cumulative probability of specific causes of death28. The proportional hazards assumption was assessed graphically with plots of Schoenfeld-type residuals against time for each cause of death in the model and by testing the time-dependent covariate for each variable.
The latest American Joint Committee on Cancer (AJCC) staging criteria for differentiated thyroid cancer consider patient age at diagnosis, with 55 years of age being the cutoff value for staging14. Reflecting this guideline, we performed separate analyses for both distant metastasis and mortality according to age subgroups using 55 years as the cutoff.
All tests were two-sided, and a P value of less than.05 was considered statistically significant. Statistical analyses were performed using SAS (version 9.2; SAS Institute Inc, Cary, NC) and R statistical software (version 3.1.1; R Foundation, Vienna, Austria). The R package cmprsk was used for competing risks analyses29.
Additional Information
How to cite this article: Han, K. et al. 1.5-2 cm tumor size was not associated with distant metastasis and mortality in small thyroid cancer: A population-based study. Sci. Rep. 7, 46298; doi: 10.1038/srep46298 (2017).
Publisher's note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
Guth, S. et al. Very high prevalence of thyroid nodules detected by high frequency (13 MHz) ultrasound examination. Eur J Clin Invest 39, 699–706 (2009).
Leenhardt, L. et al. Advances in diagnostic practices affect thyroid cancer incidence in France. Eur J Endocrinol 150, 133–139 (2004).
Frates, M. C. et al. Management of thyroid nodules detected at US: Society of Radiologists in Ultrasound consensus conference statement. Radiology 237, 794–800 (2005).
Gharib, H. & Goellner, J. R. Fine-needle aspiration biopsy of the thyroid: an appraisal. Ann Intern Med 118, 282–289 (1993).
Hoang, J. K. et al. Managing incidental thyroid nodules detected on imaging: white paper of the ACR Incidental Thyroid Findings Committee. J Am Coll Radiol 12, 143–150 (2015).
Haugen, B. R. et al. 2015 American Thyroid Association Management Guidelines for Adult Patients with Thyroid Nodules and Differentiated Thyroid Cancer: The American Thyroid Association Guidelines Task Force on Thyroid Nodules and Differentiated Thyroid Cancer. Thyroid 26, 1–133 (2016).
Russ, G. Risk stratification of thyroid nodules on ultrasonography with the French TI-RADS: description and reflections. Ultrasonography 35, 25–38 (2016).
NCCN, NCCN Clinical Practice Guidelines in Oncology (NCCN guidelines) Thyroid carcinoma. Version 2. https://www.nccn.org/professionals/physician_gls/pdf/thyroid.pdf (2013).
Gharib, H. et al. American Association of Clinical Endocrinologists, Associazione Medici Endocrinologi, and EuropeanThyroid Association Medical Guidelines for Clinical Practice for the Diagnosis and Management of Thyroid Nodules. Endocr Pract 16 Suppl 1, 1–43 (2010).
Machens, A., Holzhausen, H. J. & Dralle, H. The prognostic value of primary tumor size in papillary and follicular thyroid carcinoma. Cancer 103, 2269–2273 (2005).
Harach, H. R., Franssila, K. O. & Wasenius, V. M. Occult papillary carcinoma of the thyroid. A “normal” finding in Finland. A systematic autopsy study. Cancer 56, 531–538 (1985).
Ito, Y. et al. An observational trial for papillary thyroid microcarcinoma in Japanese patients. World J Surg 34, 28–35 (2010).
Yoon, J. H. et al. Diagnosis and Management of Small Thyroid Nodules: A Comparative Study with Six Guidelines for Thyroid Nodules. Radiology, doi: 10.1148/radiol.2016160641. 160641 (2016).
Amin, M. B. et al. AJCC Cancer Staging Manual8th edn (Springer 2017).
Sanabria, A., Dominguez, L. C., Vega, V. & Osorio, C. Prognosis of patients with thyroid cancer who do not undergo surgical treatment: a SEER database analysis. Clin Transl Oncol 13, 692–696 (2011).
Cho, B. Y. et al. Changes in the clinicopathological characteristics and outcomes of thyroid cancer in Korea over the past four decades. Thyroid 23, 797–804 (2013).
Davies, L. & Welch, H. G. Increasing incidence of thyroid cancer in the United States, 1973-2002. JAMA 295, 2164–2167 (2006).
Elisei, R. et al. Are the clinical and pathological features of differentiated thyroid carcinoma really changed over the last 35 years? Study on 4187 patients from a single Italian institution to answer this question. J Clin Endocrinol Metab 95, 1516–1527 (2010).
Mazzaferri, E. L. & Jhiang, S. M. Long-term impact of initial surgical and medical therapy on papillary and follicular thyroid cancer. Am J Med 97, 418–428 (1994).
Nguyen, X. V. et al. Incidental thyroid nodules on CT: evaluation of 2 risk-categorization methods for work-up of nodules. AJNR Am J Neuroradiol 34, 1812–1817 (2013).
Browman, G. P., Somerfield, M. R., Lyman, G. H. & Brouwers, M. C. When is good, good enough? Methodological pragmatism for sustainable guideline development. Implement Sci 10, 28 (2015).
Brouwers, M. C. et al. AGREE II: advancing guideline development, reporting and evaluation in health care. Cmaj 182, E839–842 (2010).
Steinberg, E. et al. Clinical practice guidelines we can trust(National Academies Press, 2011).
Gagliardi, A. R. et al. How can we improve guideline use? A conceptual framework of implementability. Implement Sci 6, 26 (2011).
Percy, C. L., Miller, B. A. & Gloeckler Ries, L. A. Effect of changes in cancer classification and the accuracy of cancer death certificates on trends in cancer mortality. Ann N Y Acad Sci 609, 87–97; discussion 97–89 (1990).
SEER Surveillance, Epidemiology, and End Results (SEER) Program Research Data (1973-2012), released April 2015, based on the November 2014 submission. (National Cancer Institute, Division of Cancer Control and Population Sciences, Surveillance Research Program, Surveillance Systems Branch, 2015).
Gray, R. J. A class of K-sample tests for comparing the cumulative incidence of a competing risk. Ann Stat 16, 1141–1154 (1988).
Fine, J. P. & Gray, R. J. A proportional hazards model for the subdistribution of a competing risk. J Am Stat Assoc 94, 496–509 (1999).
Gray, B. cmprsk: Subdistribution Analysis of Competing Risks. R package version 2.2–7. http://CRAN.R-project.org/package=cmprsk (2014).
Author information
Authors and Affiliations
Contributions
All authors were responsible for the study concept. K.H. and J.Y.K. contributed to the study design, data collection and statistical analyses, and wrote the first draft of the manuscript. All authors reviewed and approved the final draft of the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing financial interests.
Rights and permissions
This work is licensed under a Creative Commons Attribution 4.0 International License. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in the credit line; if the material is not included under the Creative Commons license, users will need to obtain permission from the license holder to reproduce the material. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/
About this article
Cite this article
Han, K., Kim, EK. & Kwak, J. 1.5–2 cm tumor size was not associated with distant metastasis and mortality in small thyroid cancer: A population-based study. Sci Rep 7, 46298 (2017). https://doi.org/10.1038/srep46298
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/srep46298
This article is cited by
-
Comparison of diagnostic performance of the ACR and Kwak TIRADS applying the ACR TIRADS’ size thresholds for FNA
European Radiology (2021)
-
Patient and tumor factors contributing to distant metastasis in well-differentiated thyroid cancer: A retrospective cohort study
Journal of Otolaryngology - Head & Neck Surgery (2020)
-
Strap muscle invasion in differentiated thyroid cancer does not impact disease-specific survival: a population-based study
Scientific Reports (2020)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.