Abstract
Diabetes impairs the microcirculation and function of various vital tissues throughout the body. The conjunctival microcirculation can be non-invasively imaged and thus enables assessment of microvascular hemodynamics. In this study, alterations in conjunctival microvascular hemodynamics were quantitatively assessed at stages of increasing diabetic microvasculopathy based on diabetic retinopathy (DR). Subjects were categorized into non-diabetic control (C, N = 34), no clinically visible DR (NDR, N = 47), non-proliferative DR (NPDR, N = 45), and proliferative DR (PDR, N = 35). Conjunctival hemodynamic descriptors, namely vessel diameter (D), blood velocity (V), blood flow (Q), wall shear rate (WSR), and wall shear stress (WSS) were measured in arterioles and venules, and compared between DR and C subjects using generalized linear mixed models. In arterioles, V, WSR, and WSS were lower in NDR (P ≤ 0.01). V was lower in NDR than NPDR and PDR subjects (P ≤ 0.02). In venules, D was higher in NDR and NPDR (P ≤ 0.03), while V was lower in PDR (P = 0.04). Venular V and Q were higher in NPDR than PDR subjects (P ≤ 0.04). WSR and WSS were lower in all stages of DR (P ≤ 0.05), suggestive of the potential of WSS as a marker of diabetic microvasculopathy. Quantitative assessment of conjunctival hemodynamics can potentially be useful for evaluation of diabetic microvasculopathy.
Similar content being viewed by others
Introduction
Diabetes was the seventh leading cause of death in the US in 20101. The prevalence of diabetes among US adults is projected to increase from 14% in 2010 to 21% by 20502, representing a significant burden on the population. Previous studies have reported a high prevalence of microvascular disease in diabetic subjects3,4, and indeed the most common cause of morbidity and mortality among diabetics is related to vasculopathy5,6. Alterations in circulation due to diabetes adversely affect various organ systems, causing complications such as, diabetic retinopathy (DR), nephropathy, neuropathy, cardiovascular disease, genitourinary problems, amputations and foot ulcers7. Therefore, assessment of microvascular hemodynamics can be useful for evaluation and monitoring of complications due to diabetes.
Microvascular hemodynamic alterations due to diabetes have been reported in various tissues, including the brain, heart, foot, sublingual tissues, nail fold, retina, and conjunctiva8,9,10,11,12,13,14,15,16,17,18,19,20,21,22,23,24,25,26. Due to the accessibility of the conjunctiva for direct visualization of microcirculation, alterations in the conjunctival microvasculature due to diabetes have been reported based on determination of a severity index (SI)21,23,24,25. The SI incorporated several factors, including the number of blood vessels with abnormal morphometry, blood vessel diameter, arteriole to venule ratio, blood velocity and viscosity. However, these studies did not provide assessment of conjunctival hemodynamic alterations at progressive stages of diabetic microvasculopathy.
Since DR stage is thought to parallel progressive levels of diabetic microvasculopathy in other tissues27,28, assessment of the conjunctival hemodynamics at stages of DR may become useful for gaining a better understanding of diabetes pathophysiology, and potentially allow diagnostic evaluation of diabetic microvasculopathy. Additionally, conjunctival and retinal hemodynamics may be comparable as suggested by a previous report of similarities in diabetic-related microvasculopathies between the conjunctiva and the retina20. The purpose of the current study was to provide a comprehensive and quantitative assessment of alterations in conjunctival hemodynamic descriptors at progressive stages of diabetic microvasculopathy by application of our previously established conjunctival microcirculation imaging technique29.
Methods
Subjects
The study was approved by an institutional review board of the University of Illinois at Chicago. The study was explained to subjects and written informed consents were obtained from participants according to the tenets of the Declaration of Helsinki. The cohort consisted of 161 subjects (58 males and 103 females) with ages ranging from 21 to 87 years. Based on a complete clinical history and ocular examination, including a dilated fundus examination, the subjects were categorized into one of four groups: non-diabetic control (C, N = 34) and 3 diabetic groups of increasing microvasculopathy severity: no diabetic microvasculopathy corresponding to no clinically visible diabetic retinopathy (NDR, N = 47), mild/moderate diabetic microvasculopathy corresponding to non-proliferative diabetic retinopathy (NPDR, N = 45), and advanced diabetic microvasculopathy corresponding to proliferative diabetic retinopathy (PDR, N = 35). Twelve (5 NDR, 2 NPDR, 5 PDR) and 115 (42 NDR, 43 NPDR, 30 PDR) subjects had type 1 and 2 diabetes, respectively. Exclusion criteria were inability to give informed consent or participate in the study, stroke or myocardial infarction within 3 months of imaging, active angina, dry eye syndrome, conditions that can affect the ocular surface, clinical diagnosis of glaucoma, age-related macular degeneration, retinal vascular occlusions or any other retinal, choroidal or optic nerve disease that could interfere with the staging of DR, history of intraocular surgery within 4 months of imaging, or cataract surgery within 4 months of imaging. Glycated hemoglobin (HbA1c), hematocrit (HCT), systolic blood pressure (SBP), diastolic blood pressure (DBP), and heart rate (HR) were measured at the time of imaging. Mean arterial pressure (MAP) was computed as (SBP + 2DBP)/3. Data from one eye per subject was included in the study based on the exclusion criteria, ability to maintain fixation during imaging, and image quality. If both eyes qualified, the eye with the larger number of acquired images was selected. During imaging, a headrest and forehead support were used to stabilize subject’s head, and a fixation target was presented to the fellow eye to minimize eye motion. Subjects were asked to suspend blinking during the one-second duration of image acquisition, and then allowed to blink normally.
Image Acquisition
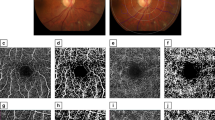
Imaging of the conjunctival microcirculation was performed using our previously described non-invasive optical imaging system (EyeFlow)29. Briefly, the imaging system comprised a slit lamp biomicroscope and a digital charged coupled device (CCD) camera (Prosilica GT, AVT, Exton, PA) for acquisition of image sequences of red blood cell motion through the conjunctival microvasculature. The slit lamp light source, fitted with a narrow band optical filter with a transmission wavelength of 540 ± 5 nm, was used to illuminate the conjunctival microvasculature. One-second image sequences were captured from the superficial conjunctival microvasculature at a rate of 50 frames per second with 5.1X magnification. Each image consisted of 1360 × 550 pixels with a pixel resolution of 1.25 μm on the object plane. This process was repeated to acquire image sequences from multiple non-overlapping conjunctival microvascular regions temporal to the limbus that encompassed up to 10 mm × 13 mm areas.
Image Processing and Analysis
Conjunctival image sequences were automatically analyzed with our previously validated method29 using customized software written in MATLAB (Release 2015b, MathWorks, Inc. Natick, MA, USA). The automated method for measuring conjunctival hemodynamics consisted of several steps including image registration, vessel segmentation, centerline and bifurcation extraction, diameter measurement, blood flow detection, and axial blood velocity measurement. Briefly, an intensity-based image registration algorithm was employed to correct for eye movement in image sequences. Frames with blinks, large eye motion, or illumination artifacts were eliminated from each image sequence, then the longest consecutive number of frames were registered. A time-averaged image was then generated from the registered image set, and Frangi filtering was performed for segmentation of conjunctival vessels. Vessel centerlines were extracted by thinning the segmented vessels, then bifurcation points were identified to define centerlines of all individual vessel segments. To ensure adequate sampling and reliability of measurements, only vessel segments with centerline lengths above 50 microns were included for hemodynamic analysis. Variance filtering was performed on the remaining vessel segments to distinguish vessels with detectable blood flow. Vessel diameter (D) and vessel boundaries were measured by computing the full width at half maximum of intensity profiles, established perpendicular to the centerline direction at every five pixels along the microvessel. Axial blood velocity (V) was determined by tracking the movement of red blood cells along the vessel centerline in the registered image sequences using a spatial-temporal image (STI) technique29. The STI showed variation of intensity values along a vessel centerline over time due to red blood cell motion. V was calculated by determining the slope of the prominent bands in the STI. Average cross sectional velocity (Vs) from D and V, blood flow (Q = VsπD2/4), wall shear rate (WSR = 8Vs/D), dynamic blood viscosity (η) from HCT and D, and wall shear stress (WSS = ηWSR) were determined using previously described formulas30,31.
Blood vessels were categorized as arterioles or venules by visualization of the direction of blood flow within the vessels and distinguished if the flow diverged into smaller vessel branches (arteriole) or collected into a larger vessel (venule). If multiple measurements were obtained along the same vessel, data from the vessel segment with the longest centerline were included for analysis. Image acquisition was not synchronized with the heart rate, and hence arteriolar and venular hemodynamic measurements were obtained at different time points during the cardiac cycle, though hemodynamics in venules are less dependent on the cardiac cycle32.
Statistical Analysis
Compiled data consisting of one value per hemodynamic descriptor (D, V, Q, WSR, WSS) per vessel per subject were analyzed using Stata version 12 (College Station, TX: StataCorp LP). Demographic and systemic physiologic data were compared among groups using the Chi-Square test or ANOVA. Mean conjunctival hemodynamic descriptors were computed and compared among C and stages of DR (NDR, NPDR and PDR) using ANOVA. A generalized linear mixed model (GLMM) with random intercepts was used to estimate beta (β) and 95% confidence intervals (CI) and examine associations between DR stage and each hemodynamic descriptor outcome. Fixed effects were analogous to standard regression analysis and estimated directly. The model assumed a Gaussian error distribution. Unadjusted models regressed the DR stage group (categorical) on the hemodynamic descriptors with no additional fixed effects. The random intercepts were established by identification of the individual study participants using their study id number. The adjusted models regressed the DR stage group (categorical), and the following fixed effects: age (continuous), race (categorical), sex (categorical), MAP (continuous), HR (continuous), HCT (continuous) and HbA1C (continuous) on the hemodynamic descriptors. Again, the random intercepts were established by identification of the individual study participants using their study id number. Since race was not matched between groups of subjects, race differences were adjusted in the models according to well-established statistical data analysis methodologies. Eye examined was not considered as a covariate in the model because it was not associated with hemodynamic descriptors. The association between V (dependent variable) and D (independent variable) was determined in each group and compared to C subjects while accounting for multiple measurements per subject in both adjusted and unadjusted models. The estimated β value (denoted by slope) derived by the model represented the increase in V per one unit increase in D. Statistical tests were two-sided and significance was accepted at P ≤ 0.05.
Results
Demographic and Physiologic Data
Subjects’ demographics and physiologic data are reported in Table 1. Sex, MAP, and eyes examined were not different among DR stages (P ≥ 0.3). However, age, race, HR, HCT, and HbA1C were different (P ≤ 0.03).
Conjunctival Hemodynamic Descriptors in Arterioles
Conjunctival hemodynamic measurements were obtained in a total of 1861 arterioles. The mean (±standard deviation (SD)) number of arteriole measurements was 13 ± 8, 12 ± 6, 12 ± 5, and 10 ± 7 in C, NDR, NPDR, and PDR subjects, respectively. There was no difference in the number of arteriole measurements among the groups of subjects (P = 0.3).
Mean and SD of unadjusted conjunctival arteriolar D, V, Q, WSR, and WSS stratified by DR stage are provided in Table 2. D and Q were similar (P ≥ 0.8), while V, WSR, and WSS were different among DR groups (P ≤ 0.03).
Estimates of DR stage differences from the statistical model with and without adjusting for age, race, sex, MAP, HR, HCT, and HbA1C are shown in Table 3. D and Q were not different between C and stages of DR with and without adjusting for covariates (P ≥ 0.3). V, WSR, and WSS were lower in NDR than C subjects with and without adjusting for covariates (P ≤ 0.01). Additionally, unadjusted WSR and WSS were lower in NPDR than C subjects (P ≤ 0.04), but the adjusted differences were not significant (P ≥ 0.2). Similarly, unadjusted WSS was lower in PDR than C subjects (P = 0.05), but not after adjusting for covariates (P = 0.3). After adjusting for covariates, V and WSR were lower in NDR as compared to NPDR subjects (P ≤ 0.02; results not shown in Table 3) and V was lower in NDR as compared to PDR subjects (P = 0.02; results not shown in Table 3).
The associations between conjunctival arteriolar V and D stratified by DR stage with and without adjusting for age, race, sex, MAP, HR, HCT, and HbA1C are provided in Table 4. After adjusting for covariates, the associations between V and D were significant in C, NDR, and PDR. The associations between V and D were weaker in NPDR and PDR as compared to C subjects (P ≤ 0.006).
Conjunctival Hemodynamic Descriptors in Venules
Conjunctival hemodynamic measurements were obtained in a total of 9027 venules. The mean (±SD) number of venule measurements was 52 ± 21, 59 ± 18, 59 ± 23, and 52 ± 16 in C, NDR, NPDR, and PDR subjects, respectively. There was no difference in the number of venules measurements among the groups of subjects (P = 0.1).
Mean and SD of unadjusted conjunctival venular D, V, Q, WSR, and WSS stratified by DR stage are provided in Table 5. D, V and Q were similar among groups (P ≥ 0.08), whereas WSR and WSS were different (P ≤ 0.05).
Estimates of DR stage differences from the statistical model with and without adjusting for age, race, sex, MAP, HR, HCT, and HbA1C are shown in Table 6. Q was not different between C and stages of DR with and without adjusting for covariates (P ≥ 0.1). D was higher in NDR than C subjects with and without adjusting for covariates (P = 0.03). WSR and WSS were lower in NDR than C subjects with and without adjusting for covariates (P ≤ 0.01). D was higher in NPDR than C subjects, regardless of the effects of age, race, sex, MAP, HR, HCT, and HbA1C (P ≤ 0.02). WSR was lower in NPDR than C subjects after adjusting for covariates (P = 0.05). WSS was lower in NPDR than C subjects with and without adjusting for covariates (P ≤ 0.02). V was lower in PDR than C subjects after adjusting for covariates (P = 0.04). WSR and WSS were lower in PDR than C subjects with and without adjusting for covariates (P ≤ 0.03). After adjusting for covariates, V and Q were higher in NPDR as compared to PDR subjects (P ≤ 0.04; results not shown in Table 6).
The associations between conjunctival venular V and D stratified by DR stage with and without adjusting for age, race, sex, MAP, HR, HCT, and HbA1C are provided in Table 7. After adjusting for covariates, the associations between V and D were significant in all groups. The association between V and D was stronger in NPDR as compared to C subjects (P = 0.01).
Discussion
In the current study, a comprehensive and quantitative assessment of alterations in hemodynamic descriptors (D, V, Q, WSR, and WSS) within the conjunctival microcirculation network was reported differentially in arterioles and venules at progressive stages of DR. In arterioles, V was reduced in NDR subjects, consistent with a previous finding22, though arterioles and venules were not differentiated in this study. Arteriolar WSR were reduced only in NDR subjects, suggestive of a potential early marker of diabetic microvasculopathy. Conjunctival microvascular hemodynamic abnormalities were more frequent in venules than arterioles, similar to a previous report that used a non-quantitative method26. In venules, vasodilation was observed in NDR and NPDR subjects, consistent with previously studies22,33, though these studies did not differentiate dilation in arterioles and venules and reported vasodilation in the entire conjunctival microvascular network. Increased vascular endothelial growth factor (VEGF) expression is known to cause vasodilation34,35 and VEGF expression has been previously reported to be elevated in conjunctival macrophages, epithelial, endothelial, and fibroblast cells in NPDR and PDR subjects36. Therefore, the finding of venular vasodilation in NPDR may be attributed, at least in part, to the elevation of VEGF expression. Further combined studies of vascular caliber and VEGF levels are needed to investigate the potential effect of VEGF expression on conjunctival vasodilation. In venules, WSR was reduced at all stages of DR, which is likely attributed to the observed vasodilation in NDR and NPDR subjects, and decreased V in PDR subjects. Reduction in V is supported by previously reported increased blood viscosity in diabetic subjects37.
There is no previous study, to the best of our knowledge, that reported alterations in conjunctival Q in a quantitative manner due to diabetes. In the current study, no alteration in conjunctival Q in arterioles or venules of DR subjects was detected as compared to C subjects. This finding is in agreement with a previous study that compared the nail fold microcirculation between diabetic and non-diabetic subjects38. However, previous studies of the retinal circulation have reported conflicting results of increased Q in early DR8, unaltered Q in NDR or early DR9, decreased Q in NPDR10, decreased Q in PDR11, and unaltered Q in PDR12. Future studies are needed to evaluate Q in both retina and conjunctiva of the same subjects to determine whether conjunctival and retinal Q are related.
WSS is an important hemodynamic parameter in cardiovascular pathophysiology39 and affects endothelial functions, such as migration of leukocytes, adhesion, control of vessel diameter, cytoskeletal structure, and energy metabolism39,40,41,42. WSS is generally lower in subjects at risk of vascular diseases43, and causes vessel wall remodeling and pathophysiology44,45. Reduced WSS in the retinal arterioles of subjects with early DR46 and in the carotid and branchial arteries of diabetic subjects47,48 was previously reported. No previous study, to our knowledge, has reported WSS in conjunctival microcirculation of diabetic subjects. In the current study, WSS was lower in conjunctival arterioles of NDR subjects and in venules at all stages of DR, as compared to non-diabetic subjects.
Reduced WSS may promote endothelial dysfunction46 and contribute to the development of microvasculopathy and DR49,50. Furthermore, previous studies have found an association of reduced WSS with increased vascular cellular adhesion molecules-1 (VCAM-1)51,52 and upregulation in the expression of VCAM-1 and intercellular adhesion molecules-1 (ICAM-1) in DR which leads to leukocytes accumulation in the retinal microcirculation53,54,55. Therefore, assessment of WSS in the conjunctival microcirculation may be potentially useful for evaluating microcirculatory abnormalities due to diabetes with and without clinical DR.
Murray’s law56 predicts a linear relationship between V and D under a normal physiological condition. The large sample size in the current study allowed us to test the linearity of this relationship in the conjunctival microcirculation. A positive linear association was found between V and D in both arterioles and venules in C subjects. This finding is in agreement with a previous study that showed a trend of increased V with larger D57. Furthermore, alterations in the dependence of V on D were present in NPDR and PDR subjects that suggest physiological abnormalities in conjunctival arterioles and venules at clinical stages of DR.
In the current study, the number of venules was greater than arterioles which is primarily due to the conjunctiva anatomy in which arterioles are less numerous than venules, as previously reported23,24. The lower sampling of arterioles could also be attributed by the fact that arterioles tend to have lower image contrast compared to venules. Despite the difference in vessel sampling, the findings of the current study are based on a very large sample size of approximately ten thousand arterioles and venules.
There were limitations in the current study. First, the imaging system was not synchronized with the cardiac cycle to account for velocity changes in arterioles due to pulsatility which was reported previously32. However, variability of V measurements due to pulsatility was reduced by averaging multiple arteriole measurements per subject. In the future, synchronization of imaging system with the cardiac cycle will enable assessment of conjunctival hemodynamics at peak systolic and diastolic blood pressure and should improve reliability of arteriole measurements. Second, identification of arterioles and venules was performed manually. Although human error in the identification of vessel type cannot be completely eliminated, the error was likely minimal since the direction of blood flow was clearly visualized in the image sequences. Third, motion of red blood cells was detectable in superficial vessels that were in the focal plane of the instrument and between 6 and 75 microns in diameter.
In summary, in non-clinical DR, arteriolar V was decreased and venular D was increased, while venular V was decreased in advanced DR and D was increased in clinical DR. At all stages of DR, venular WSS was decreased. Future studies are needed to determine the association between retinal and conjunctival hemodynamic alterations and substantiate the value of conjunctival microcirculation imaging as a surrogate for screening and monitoring of DR. Additionally, further investigation is warranted to relate alterations in conjunctival microvascular hemodynamic descriptors with incidence of complications due to diabetic microvasculopathy. Overall, assessment of conjunctival hemodynamic alterations has the potential for diagnostic evaluation and longitudinal monitoring of diabetic microvasculopathy complications.
Additional Information
How to cite this article: Khansari, M. M. et al. Assessment of Conjunctival Microvascular Hemodynamics in Stages of Diabetic Microvasculopathy. Sci. Rep. 7, 45916; doi: 10.1038/srep45916 (2017).
Publisher's note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
Centers for Disease Control and, P. National diabetes statistics report: estimates of diabetes and its burden in the United States, 2014. Atlanta (GA): US Department of Health and Human Services (2014).
Boyle, J. P., Thompson, T. J., Gregg, E. W., Barker, L. E. & Williamson, D. F. Projection of the year 2050 burden of diabetes in the US adult population: dynamic modeling of incidence, mortality, and prediabetes prevalence. Population health metrics 8, 1, doi: 10.1186/1478-7954-8-29 (2010).
Haffner, S. M., Lehto, S., Rönnemaa, T., Pyörälä, K. & Laakso, M. Mortality from coronary heart disease in subjects with type 2 diabetes and in nondiabetic subjects with and without prior myocardial infarction. New England journal of medicine 339, 229–234, doi: 10.1056/NEJM199807233390404 (1998).
Stehouwer, C. D., Fischer, H. A., Van Kuijk, A. W., Polak, B. C. & Donker, A. J. Endothelial dysfunction precedes development of microalbuminuria in IDDM. Diabetes 44, 561–564 (1995).
Algenstaedt, P. et al. Microvascular alterations in diabetic mice correlate with level of hyperglycemia. Diabetes 52, 542–549, doi: 10.2337/diabetes.52.2.542 [pii] (2003).
Squadrito, G. & Cucinotta, D. The late complications of diabetes mellitus. Annali italiani di medicina interna: organo ufficiale della Societa italiana di medicina interna 6, 126–136 (1990).
Association, A. D. Diagnosis and classification of diabetes mellitus. Diabetes care 33, S62–S69, doi: 10.2337/dc10-S062 (2010).
Feke, G. T. et al. Retinal circulatory changes related to retinopathy progression in insulin-dependent diabetes mellitus. Ophthalmology 92, 1517–1522 (1985).
Lorenzi, M. et al. Retinal haemodynamics in individuals with well-controlled type 1 diabetes. Diabetologia 51, 361–364, doi: 10.1007/s00125-007-0872-0 (2008).
Bursell, S.-E. et al. Retinal blood flow changes in patients with insulin-dependent diabetes mellitus and no diabetic retinopathy. Investigative ophthalmology & visual science 37, 886–897 (1996).
Cuypers, M. H. M., Kasanardjo, J. S. & Polak, B. C. P. Retinal blood flow changes in diabetic retinopathy measured with the Heidelberg scanning laser Doppler flowmeter. Graefe’s archive for clinical and experimental ophthalmology 238, 935–941, doi: 10.1007/s004170000207 (2000).
Grunwald, J. E., Riva, C. E., Sinclair, S. H., Brucker, A. J. & Petrig, B. L. Laser Doppler velocimetry study of retinal circulation in diabetes mellitus. Archives of Ophthalmology 104, 991–996, doi: 10.1001/archopht.1986.01050190049038 (1986).
Rayman, G., Hassan, A. & Tooke, J. E. Blood flow in the skin of the foot related to posture in diabetes mellitus. British medical journal 292, 87–90 (1986).
Terry, E. N., Messina, E. J., Schwartz, M. S., Redisch, W. & Steele, J. M. Manifestation of diabetic microangiopathy in nailfold capillaries. Diabetes 16, 595–597 (1967).
Tooke, J. E., Sandeman, D. D. & Shore, A. C. Microvascular hemodynamics in hypertension and diabetes. Journal of cardiovascular pharmacology 18 Suppl 2, S51–53 (1991).
SI, X.-m. et al. Clinical significance of sublingual vein in patients with diabetes mellitus. Liaoning Journal of Traditional Chinese Medicine 7, 006 (2008).
Mooradian, A. D. Central nervous system complications of diabetes mellitus—a perspective from the blood–brain barrier. Brain Research Reviews 23, 210–218, doi: http://dx.doi.org/10.1016/S0165-0173(97)00003-9 [pii] (1997).
Mcdonagh, P. & Hokama, J. Y. Microvascular perfusion and transport in the diabetic heart. Microcirculation 7, 163–181, doi: 10.1111/j.1549-8719.2000.tb00118.x (2000).
Wahlqvist, M., Relf, I., Myers, K. & Lo, C. Diabetes and macrovascular disease: risk factors for. Human Nutrition. Clinical Nutrition 38, 175–I184 (1984).
Stuebiger, N., Smiddy, W., Wang, J., Jiang, H. & DeBuc, D. C. Assesment of Conjunctival Microangiopathy in a Patient with Diabetes Mellitus Using the Retinal Function Imager. Journal of clinical & experimental ophthalmology 6, doi: 10.4172/2155-9570.1000400 (2015).
To, W. J., Telander, D. G., Lloyd, M. E., Chen, P. C. Y. & Cheung, A. T. W. Correlation of conjunctival microangiopathy with retinopathy in type-2 diabetes mellitus (T2DM) patients. Clinical hemorheology and microcirculation 47, 131–141, doi: 10.3233/CH-2010-1374 (2011).
Cheung, A. T. W., Ramanujam, S., Greer, D. A., Kumagai, L. F. & Aoki, T. T. Microvascular abnormalities in the bulbar conjunctiva of patients with type 2 diabetes mellitus. Endocrine Practice 7, 358–363, doi: 10.4158/EP.7.5.358 [pii] (2001).
Cheung, A. T. W. et al. Microvascular abnormalities in pediatric diabetic patients. Microvascular research 63, 252–258, doi: 10.1006/mvre.2001.2386 [pii] (2002).
Cheung, A. T. W., Chen, P. C. Y., Miguelino, E., Li, C.-S. & Devaraj, S. Correlation of microvascular abnormalities and endothelial dysfunction in Type-1 Diabetes Mellitus (T1DM): a real-time intravital microscopy study. Clinical hemorheology and microcirculation 42, 285–295, doi: 10.3233/CH-2009-1199 (2009).
Devaraj, S. et al. Evidence of increased inflammation and microcirculatory abnormalities in patients with type 1 diabetes and their role in microvascular complications. Diabetes 56, 2790–2796, doi: db07-0784 [pii] (2007).
Ditzel, J. & Sagild, U. Morphologic and Hemodynamic Changes in the Smaller Blood Vessels in Diabetes Mellitus: The Degenerative and Hemodynamic Changes in the Bulbar Conjunctiva of Normotensive Diabetic Patients. New England Journal of Medicine 250, 587–594, doi: 10.1056/NEJM195404082501401 (1954).
Margetis, P. I., Antonelou, M. H., Petropoulos, I. K., Margaritis, L. H. & Papassideri, I. S. Increased protein carbonylation of red blood cell membrane in diabetic retinopathy. Experimental and molecular pathology 87, 76–82, doi: http://dx.doi.org/10.1016/j.yexmp.2009.04.001 [pii] (2009).
Khansari, M. M. et al. Automated fine structure image analysis method for discrimination of diabetic retinopathy stage using conjunctival microvasculature images. Biomedical Optics Express 7, 2597–2606, doi: https://doi.org/10.1364/BOE.7.002597 [pii] (2016).
Khansari, M. M., Wanek, J., Felder, A. E., Camardo, N. & Shahidi, M. Automated assessment of hemodynamics in the conjunctival microvasculature network. IEEE Transactions on Medical Imaging 35, 605–611, doi: 10.1109/TMI.2015.2486619 (2016).
Koutsiaris, A. G. et al. Volume flow and wall shear stress quantification in the human conjunctival capillaries and post-capillary venules in vivo . Biorheology 44, 375–386 (2007).
Pries, A. R. et al. Resistance to blood flow in microvessels in vivo . Circulation research 75, 904–915, doi: https://doi.org/10.1161/01.RES.75.5.904 [pii] (1994).
Koutsiaris, A. G. et al. Blood velocity pulse quantification in the human conjunctival pre-capillary arterioles. Microvascular research 80, 202–208, doi: 10.1016/j.mvr.2010.05.001 [pii] (2010).
Owen, C. G., Newsom, R. S. B., Rudnicka, A. R., Ellis, T. J. & Woodward, E. G. Vascular response of the bulbar conjunctiva to diabetes and elevated blood pressure. Ophthalmology 112, 1801–1808, doi: 10.1016/j.ophtha.2005.04.030 [pii] (2005).
Facemire, C. S., Nixon, A. B., Griffiths, R., Hurwitz, H. & Coffman, T. M. Hypertension (Dallas, Tex.: 1979) 54, 652–658, doi: 10.1161/HYPERTENSIONAHA.109.129973 (2009).
Henry, T. D. et al. The VIVA trial: Vascular endothelial growth factor in Ischemia for Vascular Angiogenesis. Circulation 107, 1359–1365 (2003).
Citirik, M., Berker, N., Haksever, H., Elgin, U. & Ustun, H. Conjunctival impression cytology in non-proliferative and proliferative diabetic retinopathy. International journal of ophthalmology 7, 321–325, doi: 10.3980/j.issn.2222-3959.2014.02.23 (2014).
Schmid-Schönbein, H. & Volger, E. Red-cell aggregation and red-cell deformability in diabetes. Diabetes 25, 897–902 (1975).
Chao, C. Y. L., Zheng, Y.-P. & Cheing, G. L. Y. The association between skin blood flow and edema on epidermal thickness in the diabetic foot. Diabetes technology & therapeutics 14, 602–609, doi: 10.1089/dia.2011.0301 (2012).
Koutsiaris, A. G. Wall shear stress in the human eye microcirculation in vivo, segmental heterogeneity and performance of in vitro cerebrovascular models. Clinical hemorheology and microcirculation 63, 15–33, doi: 10.3233/CH-151976 (2016).
Ando, J. & Yamamoto, K. Vascular mechanobiology endothelial cell responses to fluid shear stress. Circulation Journal 73, 1983–1992 (2009).
Cucullo, L., Hossain, M., Puvenna, V., Marchi, N. & Janigro, D. The role of shear stress in Blood-Brain Barrier endothelial physiology. BMC neuroscience 12, 1, doi: 10.1186/1471-2202-12-40 (2011).
Palmiotti, C. A. et al. In vitro cerebrovascular modeling in the 21st century: current and prospective technologies. Pharmaceutical research 31, 3229–3250, doi: 10.1007/s11095-014-1464-6 (2014).
Jiang, Y., Kohara, K. & Hiwada, K. Low wall shear stress in carotid arteries in subjects with left ventricular hypertrophy. American journal of hypertension 13, 892–898, https://doi.org/10.1016/S0895-7061(00)00275-2 [pii] (2000).
Zarins, C. K., Zatina, M. A., Giddens, D. P., Ku, D. N. & Glagov, S. Shear stress regulation of artery lumen diameter in experimental atherogenesis. Journal of Vascular Surgery 5, 413–420, doi: 10.1016/0741-5214(87)90048-6 (1987).
Gibbons, G. H. & Dzau, V. J. The emerging concept of vascular remodeling. New England Journal of Medicine 330, 1431–1438, doi: 10.1056/NEJM199405193302008 (1994).
Nagaoka, T. et al. Impaired retinal circulation in patients with type 2 diabetes mellitus: retinal laser Doppler velocimetry study. Investigative ophthalmology & visual science 51, 6729–6734, doi: 10.1167/iovs.10-5364 (2010).
Nagaoka, T. & Yoshida, A. Noninvasive evaluation of wall shear stress on retinal microcirculation in humans. Investigative ophthalmology & visual science 47, 1113–1119, doi: 10.1167/iovs.05-0218 (2006).
Irace, C. et al. NIDDM is associated with lower wall shear stress of the common carotid artery. Diabetes 48, 193–197, doi: 10.2337/diabetes.48.1.193 (1999).
Sheetz, M. J. & King, G. L. Molecular understanding of hyperglycemia’s adverse effects for diabetic complications. Jama 288, 2579–2588, doi: 10.1001/jama.288.20.2579 (2002).
Horio, N. et al. Angiotensin AT1 receptor antagonism normalizes retinal blood flow and acetylcholine-induced vasodiliation in normotensive diabetic rats. Diabetologia 47, 113–123, doi: 10.1007/s00125-003-1262 (2004).
Ando, J. et al. Shear stress inhibits adhesion of cultured mouse endothelial cells to lymphocytes by downregulating VCAM-1 expression. American Journal of Physiology-Cell Physiology 267, C679–C687 (1994).
Miyahara, S. et al. Simvastatin inhibits leukocyte accumulation and vascular permeability in the retinas of rats with streptozotocin-induced diabetes. The American journal of pathology 164, 1697–1706, doi: 10.1016/S0002-9440(10)63728-5 (2004).
Miyamoto, K. et al. Prevention of leukostasis and vascular leakage in streptozotocin-induced diabetic retinopathy via intercellular adhesion molecule-1 inhibition. Proceedings of the National Academy of Sciences 96, 10836–10841 (1999).
McLeod, D. S., Lefer, D. J., Merges, C. & Lutty, G. A. Enhanced expression of intracellular adhesion molecule-1 and P-selectin in the diabetic human retina and choroid. The American journal of pathology 147, 642 (1995).
Joussen, A. M. et al. Nonsteroidal anti-inflammatory drugs prevent early diabetic retinopathy via TNF-α suppression. The FASEB journal 16, 438–440, doi: 10.1096/fj.01-0707fje (2002).
Murray, C. D. The Physiological Principle of Minimum Work: I. The Vascular System and the Cost of Blood Volume. Proceedings of the National Academy of Sciences of the United States of America 12, 207–214 (1926).
Koutsiaris, A. G. Correlation of axial blood velocity to venular and arteriolar diameter in the human eye in vivo . Clinical hemorheology and microcirculation 61, 429–438, doi: 10.3233/CH-141888 (2016).
Acknowledgements
Supported by NIH research grants DK104393, EY001792, Senior Scientific Investigator Award (MS) and departmental award from Research to Prevent Blindness.
Author information
Authors and Affiliations
Contributions
The specific contributions made by authors were as following. Concept and design of the work: M.S., J.W.; data collection: J.W., M.T.; data analysis and interpretation: M.M.K., C.E.J., J.K.K., N.C., N.P.B., M.S.; drafting the article: M.M.K., J.W., M.S.; critical revision of the article: M.M.K., J.W., N.P.B., M.S.; final approval for publication: M.M.K., J.W., M.T., C.E.J., J.K.K., N.P.B., M.S. M.S. is the guarantor of this study and takes responsibility for the contents of the manuscript.
Corresponding author
Ethics declarations
Competing interests
M.S. and J.W. hold a patent for the EyeFlow imaging system. The remaining authors declare no conflict of interest.
Rights and permissions
This work is licensed under a Creative Commons Attribution 4.0 International License. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in the credit line; if the material is not included under the Creative Commons license, users will need to obtain permission from the license holder to reproduce the material. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/
About this article
Cite this article
Khansari, M., Wanek, J., Tan, M. et al. Assessment of Conjunctival Microvascular Hemodynamics in Stages of Diabetic Microvasculopathy. Sci Rep 7, 45916 (2017). https://doi.org/10.1038/srep45916
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/srep45916
This article is cited by
-
Identifying diabetes from conjunctival images using a novel hierarchical multi-task network
Scientific Reports (2022)
-
Assessment of the conjunctival microcirculation for patients presenting with acute myocardial infarction compared to healthy controls
Scientific Reports (2021)
-
Inter-visit measurement variability of conjunctival vasculature and circulation in habitual contact lens wearers and non-lens wearers
Eye and Vision (2019)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.