Abstract
Comparisons of home-based versus hospital-based approach in managing patients with suspected obstructive sleep apnoea syndrome(OSAS). A prospective, controlled CPAP parallel study of new referrals with suspected OSAS randomized into group A) home-based or B) hospital-based approach. Following detection of AHI ≥ 15/hr by Embletta sleep study (group A) or polysomnography (group B), patients received CPAP for 3 months after an overnight autoCPAP titration at home or in hospital respectively. Modified intention-to-treat analysis of those with AHI ≥ 15/hr on CPAP (n = 86 vs 86) showed no difference in Epworth sleepiness score, the primary endpoint, but greater improvement in Sleep-Apnoea-Quality-of-Life-Index[difference 0.3,(95%CI 0.02, 0.6), p = 0.033] at 3 months in group A. The mean costs for the patients in group A and group B were HK$8479(989) and HK$22,248(2407) respectively. The mean difference between groups was HK$-13,769(USD 1770 equivalent) per patient with 95% CI. (−14324, −13213), p < 0.001. The waiting time of patients with AHI ≥ 15/hr who were started on CPAP treatment from the first clinic consultation to the diagnostic sleep test, autoCPAP titration, and CPAP treatment was 189.6, 148.8 and 145.0 days shorter in group A than group B respectively. Home-based approach is non-inferior to hospital-based approach in managing patients with suspected OSAS, with shorter waiting time, and substantial cost savings.
Similar content being viewed by others
Introduction
Untreated obstructive sleep apnoea syndrome (OSAS) causes daytime sleepiness, cognitive function impairment and is associated with hypertension, atrial fibrillation, heart failure, sudden death, and stroke1. Attended polysomnography (PSG) is the standard investigation for patients with suspected OSAS, but the waiting time is often lengthy2. In recent years, several portable monitoring devices have been validated as useful alternatives of PSG, with the potential advantages of reducing the waiting time and healthcare cost3,4. The algorithms of managing patients with suspected OSAS were discussed by the American Academy of Sleep Medicine (AASM), and other professional societies5,6. The AASM task force has recommended that at a minimum, portable monitoring device must record airflow, respiratory effort, and blood oxygenation7.
Several research groups have examined different models of care involving initial home-based sleep test in diagnosing OSAS, identifying patients who may benefit from continuous positive airway pressure (CPAP), and reducing the need for hospital-based PSG and CPAP titration with encouraging results8,9,10,11,12,13,14. However very few studies have addressed healthcare costs, with conflicting results13,14, and there are unresolved issues as to what disease management models based on economic outcome and what patient population would be appropriate for ambulatory management15,16.
This comprehensive study aimed to assess the role of an ambulatory approach with home diagnostic sleep test followed by home autoCPAP titration versus the hospital-based approach in managing patients with suspected OSAS with reference to 1) Improvement of subjective sleepiness; 2) Quality of life; 3) Cognitive function; 4)CPAP usage; and 5) Healthcare costs.
We hypothesized that the ambulatory approach would be non-inferior to the conventional approach in managing patients with OSAS in terms of clinical outcome but the former approach would lead to substantial cost savings.
Methods
Subjects and Methods
We conducted a prospective, randomized, controlled CPAP parallel study on new referrals to the Respiratory Clinic, Prince of Wales Hospital, Shatin, with suspected OSAS from 25 September 2013 to 31 August 2014. OSAS was defined by apnea-hypopnea index (AHI) ≥ 5/hr of sleep plus excessive daytime sleepiness or two of the following symptoms: choking or gasping during sleep, recurrent awakenings from sleep, unrefreshed sleep, daytime fatigue, and impaired concentration17.
Inclusion criteria
All patients, age 18–80 years, with suspected OSAS underwent assessment at the clinic with the Epworth sleepiness score (ESS)18 and symptoms evaluation. Patients who had ESS score >9 or at least two OSAS symptoms as described above were invited to join the study.
Exclusion criteria included patients with (a) unstable cardiovascular diseases (e.g. recent unstable angina, myocardial infarction, stroke within the previous 6 months or severe left ventricular failure), (b) neuromuscular disease affecting respiratory muscles, (c) moderate to severe respiratory disease or documented hypoxemia or awake SaO2 <92% or (d) psychiatric disease that limited the ability to give informed consent.
They were randomized by a random table into either group (A) home-based management approach or group (B) hospital-based management approach by a third party not involved in the trial. In both groups, the patients first went through the evaluation phase and if they had symptoms of OSAS with AHI ≥ 15/hr on home Embletta sleep test (Group A) or hospital-based PSG (Group B), they would then be enrolled to the CPAP outcome study (i.e. the second phase).
Group A
Patients in group A underwent a level 3 home sleep study with the Embletta device (Medcare, Iceland), which had been validated against hospital-based PSG in the Chinese population in Hong Kong4. The EmblettaTM PDS is a pocket-sized, digital, multi-channel recording device that measures airflow through a nasal cannula connected to a pressure transducer, providing an AHI based on recording time. It detects respiratory and abdominal efforts through the effort sensor and can differentiate between obstructive and central events. Built-in position sensors can differentiate supine from non-supine events. Patients were instructed by nurses how to operate the Embletta device for the sleep recording and estimate their time of sleep4.
Respiratory events are scored when desaturations of ≥4% occurs in the absence of moving artefacts and irrespective of co-existing changes in snoring or heart rate. The EmblettaTM PDS default settings for apneas and hypopneas were used in this study. An apnea was defined as a decrease in airflow by 80% of baseline for ≥10 seconds. A hypopnea was defined as a decrease in airflow by 50% of baseline for ≥10 seconds. The EmblettaTM PDS AHI used for analysis was automatically analyzed by the EmblettaTM PDS software4.
Following detection of OSAS with AHI ≥ 15/hr on home Embletta sleep study, each patient was interviewed by the physician on duty and invited to participate in the overnight home autoCPAP titration study. We offered symptomatic patients with AHI ≥ 15/hr early CPAP treatment as this group of patients were most likely to be adherent to CPAP19, and had the greatest risk of adverse health outcomes related to OSAS20,21. Those who had failed the Embletta sleep study were arranged to have a second home Embletta sleep study. Patients who were symptomatic of OSAS with a negative home Embletta sleep study were arranged to have a hospital-based PSG. Patients with AHI ≥ 15/hr were offered a basic CPAP education package by nurses and a 30-minute CPAP acclimatization trial with the AutoSet device (ResMed, NSW, Australia) in the afternoon at the clinic before an unattended overnight autoCPAP titration study at home (22).
Group B
Overnight PSG(Alice LE, Respironics, USA) was performed as at the hospital for every subject in group B recording electroencephalogram, electro-oculogram, submental electromyogram, bilateral anterior tibial electromyogram, electrocardiogram, chest and abdominal wall movement by inductance plethysmography, airflow measured by a nasal pressure transducer [PTAF2, Pro-Tech, Woodinville, WA, USA] and supplemented by oronasal airflow thermistor, plus finger pulse oximetry. (22) Apnea was defined as cessation of airflow for >10 seconds with drop in the peak thermal sensor excursion by ≥90% of baseline whereas hypopnea as a reduction of nasal pressure airflow of ≥30% of baseline for >10 seconds plus an oxygen desaturation of ≥4% (23).
Patients with AHI ≥ 15/hr on PSG underwent attended autoCPAP titration in the hospital setting after receiving a basic CPAP education package by nurses and a 30-minute CPAP acclimatization trial with the AutoSet device in the afternoon at the clinic (22).
The CPAP level for both groups A and B was set at the median 95th centile pressure needed during autoCPAP titration at home (group A) and hospital setting (group B) to abolish snoring, obstructive respiratory events and airflow limitation. The patients in both groups were followed up at the CPAP clinic at 1 month and at 3 months by nurses to manage any problem with the CPAP device or mask fit and monitor the CPAP compliance. Subjects in both groups were prescribed nasal CPAP units with time clocks to assess objective CPAP usage (run time). In both arms of care, extra nursing consultations and phone advice were possible and were recorded.
Those with mild OSAS (AHI 5–15/hr) in both group A and group B were advised by physicians on treatment alternatives such as dental device, lifestyle modifications22 if appropriate or a trial of CPAP if agreeable but they were not included in the CPAP outcome study.
Outcome assessment
Prior to commencement of home or conventional CPAP treatment, all patients underwent baseline assessment including ESS18, sleep-apnoea-specific-quality-of-life index(SAQLI)23, and cognitive function tests24, and these were reassessed at 3 months after CPAP treatment.
The ESS is a questionnaire specific to symptoms of daytime sleepiness and the patients are asked to score the likelihood of falling asleep in eight different situations with different levels of stimulation, adding up to a total score of 0 to 24 (18).
The SAQLI has 35 questions organized into four domains: daily functioning, social interactions, emotional functioning and symptoms with a fifth domain, treatment-related symptoms, to record the possible negative impacts of treatment (25).
Cognitive function tests including trail-making, digit-symbol, digit-span and Stroop colour testing were performed to provide objective evidence for improvement in daytime function on CPAP treatment, as in our previous study. (22) The trail-making test estimates the minimum time required to connect a structured number sequence and the lower the score, the better the performance. The digit symbol and span tests involve the immediate memory and recall of number sequences while the stroop colour test evaluates the correct matching of colour and their corresponding characters. For the Stroop color, digit-symbol, and digit-span tests, a higher score indicated superior performance (22).
The primary endpoints included the difference in changes in ESS, SAQLI, cognitive function tests, objective CPAP usage after 3 months of CPAP treatment between the 2 groups. Secondary endpoints included difference in healthcare costs.
Sample size estimation
The study was powered to demonstrate non-inferiority of the ambulatory approach versus the conventional approach with respect to change in ESS, the primary outcome measure. A sample size of 86 patients in each group achieved 90% power to detect non-inferiority using a one-sided, independent samples t-test. The margin of equivalence was set at 2, i.e. a difference of this size or less on the ESS scale was not considered to be clinically important. The one-sided significance level (alpha) of the test was set at 0.025. It was assumed that the common standard deviation for change in ESS in moderate-severe OSAS was 425. As our respiratory clinic generally attracted 75% of patients with at least moderate OSAS, in order to allow for 10% drop-out over the course of the study, we proceeded to recruit at least 130 patients in each group.
Statistical analysis
Data were analysed on an intention-to-treat (ITT) basis comparing the two groups in terms of demographics, and waiting time for diagnostic tests, CPAP titration and treatment by including all patients randomized. Data were analysed on a modified ITT basis by including patients with AHI ≥ 15/hr starting CPAP therapy in both groups. For comparisons of baseline characteristics, health economics, CPAP compliance and magnitude on change in outcomes (treatment minus baseline) between the 2 groups, independent samples t-test was used for continuous variables and chi-squared test for categorical variables. To compare the measurements before and after CPAP treatment, paired samples t-test was used. Data analysis was performed with IBM SPSS (IBM SPSS Statistics for Windows, Version 22.0. Armonk, NY: IBM Corp). As a sensitivity analysis, treatment per-protocol (TPP) analysis was conducted for those with AHI ≥ 15/hr and had completed the 3-month CPAP outcome study.
Cost-effectiveness analysis
Costs were divided into 2 parts, namely within-study costs and implementation costs in practice11,15. Cost consequences analysis, i.e. a comparison of costs with different outcomes, was conducted26. Within study costs included the resource use and cost over the study period from randomization (eg, staff cost, CPAP device and its education package, attended training for the patients at clinic or hospital, overnight testing with PSG versus home monitoring, any Embletta recording failure and need for repeating the test, productivity loss due to sick leave of patients, and etc). The implementation cost in practice not only included the within-study cost but also other factors comparable to the reality (eg, the prevalence of patients with different severity, the waiting time for having PSG or unattended home CPAP titration, etc) (15). All costs associated with the continuum of care (CPAP equipment and disposables, dental appliance or surgical intervention, physician visits, etc) were taken into account (15). More details of the cost-effectiveness analyses are available in the Supplementary Information.
This study protocol was approved by the Ethics Committees of the Chinese University of Hong Kong (CREC-2011.215-T) and registered at ClinicalTrials.gov(Identifier: NCT01828216) on 8 April 2013. The methods were carried out in accordance with the relevant guidelines and regulations. Written informed consent was obtained from all subjects enrolled in this study.
Results [mean(SD) unless stated otherwise]
Baseline Characteristics
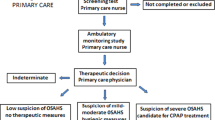
In the first phase, altogether 316 subjects were recruited and randomized into group A (n = 157) and group B (n = 159) as shown in Fig. 1. Eighty six subjects were found to have AHI ≥ 15/hr in both Group A and B. Sixty two subjects in Group A and 69 subjects in Group B completed the 3-month follow-up. Table 1 showed the demographic data between Group A and B. The two groups were similar for most of the variables including the oxygen desaturation index (ODI) except for lower AHI and ESS in Group A (Table 1).
Data were analysed on an intention-to-treat (ITT) basis comparing the two groups in terms of demographics, and waiting time for diagnostic tests, CPAP titration and treatment by including all patients randomized. Data were analysed on a modified ITT basis by including patients with AHI ≥ 15/hr starting fixed CPAP therapy in both groups whereas treatment per-protocol (TPP) analysis was conducted for those with AHI ≥ 15/hr who had completed the 3-month CPAP outcome study. * In group A with AHI ≥ 15/hr, 17 out of 86 patients failed the first home sleep test and had to undergo the second home sleep test which was successful. In group B with AHI ≥ 15/hr, 2 out of 86 patients had to undergo PSG twice. Seven out of 157 and 4 out of 159 in group A and group B “failed” sleep tests twice respectively due to either technical problems or poor sleep (total sleep time <0034 hrs) and the 7 patients in group A proceeded to PSG. # In group B, 25 patients refused to continue the study after randomization as the waiting time for polysomnography was too long.
The waiting time of patients with AHI ≥ 15/hr who were started on CPAP treatment from the first clinic consultation to the diagnostic sleep test, autoCPAP titration, and CPAP treatment was 59.3 (35.2), 117.3 (41.0) and 154.7 (69.5) days for group A versus 248.9 (186.0), 266.1 (192.5) and 299.7 (198.7) days for group B respectively. All the waiting time for sleep tests and treatment in group A was significantly shorter than group B (p < 0.001) (Table 2).
Using a modified ITT analysis of those with AHI ≥ 15/hr (n = 86 vs 86), group A had greater improvement in SAQLI at 3 months [difference 0.3, (95% CI 0.02, 0.6), p = 0.033]. There were no significant differences in ESS and most of the cognitive function tests except for greater improvement in stroop colour testing with words in group A [difference 2.6, (95% CI 0.1, 5.1), p = 0.038] (Table 3). The results using TPP approach were similar to those analyzed by the modified ITT approach (Tables 4 and 5).
Since home sleep test could underestimate the AHI, additional analysis was performed by comparing moderate OSA (AHI 15–30/hr by home Embletta) in group A with severe OSA (AHI > 30/hr by PSG) in group B by modified ITT (n = 43 vs n = 48) and TPP (n = 33 vs n = 39) respectively. Apart from some differences in trail making with words and stroop colour, differences in other endpoints were not significant (supplemental file Table S2a–d).
Healthcare costs
For those who had dropped out after commencement of CPAP, a last observation carried forward approach was used to impute their wage loss and transportation expense. The approach should be acceptable in this scenario as it is expected their salary and the route to go to hospital would be the same. Following modified ITT analysis, the mean (SD) costs for the patients in group A (n = 86) and group B (n = 86) were HK$8479 (989) and HK$22,248 (2407) respectively. The mean difference between groups was HK$-13,769 per patient with 95% CI. (−14324, −13213), p < 0.001.
Status of those with AHI < 15/hr (n = 98) who were excluded from the 3-month CPAP outcome study is shown in the Supplementary Table S1.
Patients who were symptomatic of OSAS with a negative home Embletta sleep study (n = 10) were arranged to have a hospital-based PSG, which revealed that 2 patients had AHI ≥ 15/hr. Those who had failed the first Embletta sleep study (n = 7) were arranged to have a second home Embletta sleep study. A “failed” home study means that a case could not complete the home sleep test successfully due to either technical problems (poor signals) or poor sleep (TST < 4 hrs), despite having repeated the test. Of these 7 patients who had undergone PSG, 3 were found to have AHI ≥ 15/hr. Thus altogether 10 + 7 = 17 patients in group A finally required PSG, with a waiting time of 384.4 (312.4) days for PSG.
Discussion
This randomized controlled trial (RCT) compared a home-based approach using a validated level 3 sleep diagnostic device4 for diagnosis followed by one night of autoCPAP titration against the hospital-based sleep laboratory approach in managing clinic patients with suspected OSAS. The waiting time of patients with AHI ≥ 15/hr who were started on CPAP treatment from the first clinic consultation to the diagnostic sleep test, autoCPAP titration, and CPAP treatment was 189.6, 148.8 and 145.0 days shorter in group A than in group B respectively. The much longer waiting time for PSG and autoCPAP titration in the hospital setting was due to the limited number of hospital beds designated for sleep medicine service whereas the home-based approach offered much more flexibility.
Using a modified ITT analysis of those with AHI ≥ 15/hr who had commenced home CPAP treatment, Group A had slightly greater improvement in SAQLI and stroop colour testing with words at 3 months whereas there was no difference in other cognitive function tests between the 2 groups. As importantly, there was significant cost saving of HK$13,769 (USD1770 equivalent) per patient in favour of group A. However, whether there is significant cost saving using home management approach would depend on the local healthcare system and costs. A RCT in Spain has shown that patients with a high probability of OSAS could be diagnosed and treated in a home setting, with a high level of CPAP compliance and lower cost (€590 vs €894 vs €644) than using either a hospital-based approach or home respiratory polygraphy/hospital follow-up.(13) In contrast, another RCT in the USA has shown cost saving of US$264(95% CI $39, $496, P = 0.02) in favor of home-based management from the patient’s perspective but US$40 (95% CI -$213, $142, P = 0.66) in favor of the laboratory-based arm under the base case from the provider perspective14.
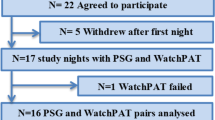
Our study findings add more strength to the growing literature that the ambulatory approach is an alternative strategy in managing clinic patients with suspected OSAS. In a RCT conducted by Skomro et al.8 comparing an ambulatory approach (home-based level 3 testing followed by one week of autoCPAP titration and then fixed-pressure CPAP based on 95th centile pressure) vs in-laboratory PSG and CPAP titration, the laboratory approach did not lead to superior four-week outcomes in sleepiness scores, sleep quality, quality of life, blood pressure, and CPAP adherence. Another RCT by Berry et al.9, comparing a level 3 portable monitoring(Watch PAT-100) and autoCPAP titration(2–3 nights) vs PSG for the diagnosis and treatment of OSAS, has shown that the former approach resulted in CPAP adherence and clinical outcomes similar to the one using PSG. In a RCT that compared standard PSG against ambulatory CPAP titration (autoCPAP titration for 1 week followed by CPAP set at 95th centile pressure) in high-risk patients identified by a diagnostic algorithm involving symptom score and a level 3 portable sleep diagnostic device, Mulgrew et al.10 have shown no advantage of PSG over the ambulatory approach in terms of diagnosis, CPAP titration(AHI on CPAP), ESS, and SAQLI over 3 months whereas adherence to CPAP therapy was better in the ambulatory group. A nurse-led model of care by Antic et al.11 using 4 nights of home auto-adjusting device after overnight home oximetry to set therapeutic CPAP has demonstrated non-inferior results(change in ESS, CPAP adherence at 3 months) to physician-directed care, which involved two laboratory PSG to diagnose and treat patients with moderate to severe OSAS. Kuna et al.12, who randomized patients with suspected OSAS to either home testing with the Embletta device followed by at least 3 nights of autoCPAP titration or laboratory-based management, found that functional outcome and treatment adherence in patients evaluated through the home testing approach was not clinically inferior to that in patients receiving standard in-laboratory PSG.
Pressure for alternative approaches to the in-laboratory/hospital management of patients with OSAS will continue to increase given the cost of PSG, the limited number of hospital or laboratory-based facilities and the growing demand for more rapid access to testing16. Since 2007, the AASM has approved the use of home portable monitoring and recommended that unobserved registers with type 2–3 monitors be used as an alternative to PSG diagnosis7, and unattended autoCPAP titration to determine a fixed CPAP treatment pressure in patients with a high probability of moderate-to-severe OSAS without significant medical comorbidities27.
It is important to shorten the waiting time for sleep investigation and treatment especially for those with a high clinical probability of OSAS, as many studies have shown that untreated OSA is associated with increased risks of hypertension28, platelet activation29, diastolic dysfunction30, mortality20,31,32,33, sudden death21,34, and stroke21,35,36. CPAP has been shown to reduce systemic blood pressure37,38, daytime sleepiness39, risk of driving accidents40, and platelet activation29 although it remains to be seen by proper RCTs whether it may reduce mortality in patients with OSAS41.
One limitation of this study was that the Embletta diagnostic device had underestimated the AHI because it only recorded the number of obstructive events/hour of recording instead of actual sleep time although the ODI in both groups was comparable. Moreover, only 62 and 69 out of 86 patients completed 3 months of CPAP treatment in group A and group B respectively. Without adequate contact with health professionals, more patients in group A were likely not inclined to follow-up care.
In conclusion, the ambulatory approach for diagnosis and treatment was non-inferior to the conventional hospital-based approach in managing clinic patients in Hong Kong with suspected OSAS in terms of CPAP usage and improvement of some clinical endpoints, with the advantages of much shorter waiting time, and substantial cost savings.
Additional Information
How to cite this article: Hui, D. S. et al. A randomized controlled trial of an ambulatory approach versus the hospital-based approach in managing suspected obstructive sleep apnea syndrome. Sci. Rep. 7, 45901; doi: 10.1038/srep45901 (2017).
Publisher's note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
Bradley, T. D. & Floras, J. S. Obstructive sleep apnoea and its cardiovascular consequences. Lancet 373, 82–93 (2009).
Flemons, W. W., Douglas, N. J., Kuna, S. T., Rodenstein, D. O. & Wheatley, J. Access to diagnosis and treatment of patients with suspected sleep apnea. Am. J. Respir. Crit. Care Med. 169, 668–672 (2004).
Ng, S. S. et al. Validation of a portable recording device (ApneaLink) for identifying patients with suspected obstructive sleep apnoea syndrome. Intern Med J 39, 757–762 (2009).
Ng, S. S. et al. Validation of Embletta portable diagnostic system for identifying patients with suspected obstructive sleep apnoea syndrome (OSAS). Respirology 15, 336–342 (2010).
Kushida, C. A. et al. Practice parameters for the indications for polysomnography and related procedures: an update for 2005. Sleep 28, 499–521 (2005).
Flemons, W. W. et al. Home diagnosis of sleep apnea: a systematic review of the literature. An evidence review cosponsored by the American Academy of Sleep Medicine, the American College of Chest Physicians, and the American Thoracic Society. Chest 124, 1543–1579 (2003).
Collop, N. A. et al. Clinical guidelines for the use of unattended portable monitors in the diagnosis of obstructive sleep apnea in adult patients. Portable Monitoring Task Force of the American Academy of Sleep Medicine. J Clin Sleep Med 3, 737–747 (2007).
Skomro, R. P. et al. Outcomes of home-based diagnosis and treatment of obstructive sleep apnea. Chest 138, 257–263 (2010).
Berry, R. B., Hill, G., Thompson, L. & McLaurin, V. Portable monitoring and autotitration versus polysomnography for the diagnosis and treatment of sleep apnea. Sleep 31, 1423–1431 (2008).
Mulgrew, A. T., Fox, N., Ayas, N. T. & Ryan, C. F. Diagnosis and initial management of obstructive sleep apnea without polysomnography: a randomized validation study. Ann. Intern. Med. 146, 157–166 (2007).
Antic, N. A. et al. A randomized controlled trial of nurse-led care for symptomatic moderate-severe obstructive sleep apnea. Am. J. Respir. Crit. Care Med. 179, 501–508 (2009).
Kuna, S. T. et al. Noninferiority of functional outcome in ambulatory management of obstructive sleep apnea. Am. J. Respir. Crit. Care Med. 183, 1238–1244 (2011).
Andreu, A. L. et al. Effect of an ambulatory diagnostic and treatment programme in patients with sleep apnoea. Eur. Respir. J. 39, 305–312 (2012).
Kim, R. D. et al. An Economic Evaluation of Home Versus Laboratory-Based Diagnosis of Obstructive Sleep Apnea. Sleep 38, 1027–1037 (2015).
Kuna, S. T. et al. An official ATS/AASM/ACCP/ERS workshop report: Research priorities in ambulatory management of adults with obstructive sleep apnea. Proc Am Thorac Soc 8, 1–16 (2011).
McNicholas, W. T. & Levy, P. Portable monitoring in sleep apnoea: the way forward? Eur. Respir. J. 37, 749–751 (2011).
Sleep-related breathing disorders in adults: recommendations for syndrome definition and measurement techniques in clinical research. The Report of an American Academy of Sleep Medicine Task Force. Sleep 22, 667–689 (1999).
Johns, M. W. A new method for measuring daytime sleepiness: the Epworth sleepiness scale. Sleep 14, 540–545 (1991).
McArdle, N. et al. Long-term use of CPAP therapy for sleep apnea/hypopnea syndrome. Am. J. Respir. Crit. Care Med. 159, 1108–1114 (1999).
Marin, J. M., Carrizo, S. J., Vicente, E. & Agusti, A. G. Long-term cardiovascular outcomes in men with obstructive sleep apnoea-hypopnoea with or without treatment with continuous positive airway pressure: an observational study. Lancet 365, 1046–1053 (2005).
Yaggi, H. K. et al. Obstructive sleep apnea as a risk factor for stroke and death. N. Engl. J. Med. 353, 2034–2041 (2005).
Ng, S. S. et al. A Randomized Controlled Study to Examine the Effect of a Lifestyle Modification Program in OSA. Chest 148, 1193–1203 (2015).
Flemons, W. W. & Reimer, M. A. Development of a disease-specific health-related quality of life questionnaire for sleep apnea. Am. J. Respir. Crit. Care Med. 158, 494–503 (1998).
Hui, D. S. et al. Effects of augmented continuous positive airway pressure education and support on compliance and outcome in a Chinese population. Chest 117, 1410–1416 (2000).
Engleman, H. M. et al. Randomised placebo controlled trial of daytime function after continuous positive airway pressure (CPAP) therapy for the sleep apnoea/hypopnoea syndrome. Thorax 53, 341–345 (1998).
Rainer, T. H. et al. Cost effectiveness analysis of intravenous ketorolac and morphine for treating pain after limb injury: double blind randomised controlled trial. BMJ 321, 1247–1251 (2000).
Morgenthaler, T. I. et al. Practice parameters for the use of autotitrating continuous positive airway pressure devices for titrating pressures and treating adult patients with obstructive sleep apnea syndrome: an update for 2007. An American Academy of Sleep Medicine report. Sleep 31, 141–147 (2008).
Peppard, P. E., Young, T., Palta, M. & Skatrud, J. Prospective study of the association between sleep-disordered breathing and hypertension. N. Engl. J. Med. 342, 1378–1384 (2000).
Hui, D. S. et al. The effects of nasal continuous positive airway pressure on platelet activation in obstructive sleep apnea syndrome. Chest 125, 1768–1775 (2004).
Fung, J. W. et al. Severe obstructive sleep apnea is associated with left ventricular diastolic dysfunction. Chest 121, 422–429 (2002).
Young, T. et al. Sleep disordered breathing and mortality: eighteen-year follow-up of the Wisconsin sleep cohort. Sleep 31, 1071–1078 (2008).
Marshall, N. S. et al. Sleep apnea as an independent risk factor for all-cause mortality: the Busselton Health Study. Sleep 31, 1079–1085 (2008).
Punjabi, N. M. et al. Sleep-disordered breathing and mortality: a prospective cohort study. PLoS Med 6, e1000132 (2009).
Gami, A. S., Howard, D. E., Olson, E. J. & Somers, V. K. Day-night pattern of sudden death in obstructive sleep apnea. N. Engl. J. Med. 352, 1206–1214 (2005).
Redline, S. et al. Obstructive sleep apnea-hypopnea and incident stroke: the sleep heart health study. Am. J. Respir. Crit. Care Med. 182, 269–277 (2010).
Hui, D. S. et al. Prevalence of sleep-disordered breathing and continuous positive airway pressure compliance: results in chinese patients with first-ever ischemic stroke. Chest 122, 852–860 (2002).
Bratton, D. J., Gaisl, T., Wons, A. M. & Kohler, M. CPAP vs Mandibular Advancement Devices and Blood Pressure in Patients With Obstructive Sleep Apnea: A Systematic Review and Meta-analysis. JAMA 314, 2280–2293 (2015).
Hui, D. S. et al. Nasal CPAP reduces systemic blood pressure in patients with obstructive sleep apnoea and mild sleepiness. Thorax 61, 1083–1090 (2006).
McDaid, C. et al. A systematic review of continuous positive airway pressure for obstructive sleep apnoea-hypopnoea syndrome. Sleep Med Rev 13, 427–436 (2009).
Tregear, S., Reston, J., Schoelles, K. & Phillips, B. Continuous positive airway pressure reduces risk of motor vehicle crash among drivers with obstructive sleep apnea: systematic review and meta-analysis. Sleep 33, 1373–1380 (2010).
McEvoy, R. D. et al. CPAP for Prevention of Cardiovascular Events in Obstructive Sleep Apnea. N. Engl. J. Med. 375, 919–931 (2016).
Acknowledgements
We thank the Health & Medical Research Fund (Ref: 10110811), Food and Health Bureau, Hong Kong, for supporting this study. The study sponsor, Health & Medical Research Fund, Food & Health Bureau, Hong Kong, played no role in study design, data collection, analysis, data interpretation in the writing of the report and in the decision to submit the paper for publication. Health & Medical Research Fund (#10110811), Food and Health Bureau, HK.
Author information
Authors and Affiliations
Contributions
D.S.H. is the overall guarantor of this report and takes responsibility for the content, including the data and analysis. Concept and design: D.S.H., W.T., S.N. Drafting the manuscript for important intellectual content: D.S.H., S.N., W.T. Analysis and interpretation of data: T.O.C., W.T., D.S.H. Patient recruitment, manuscript drafting: S.N., K.W.T., F.K., J.N., K.C., W.H.Y., K.Y. All authors have read and approved the submission of the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing financial interests.
Supplementary information
Rights and permissions
This work is licensed under a Creative Commons Attribution 4.0 International License. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in the credit line; if the material is not included under the Creative Commons license, users will need to obtain permission from the license holder to reproduce the material. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/
About this article
Cite this article
Hui, D., Ng, S., To, KW. et al. A randomized controlled trial of an ambulatory approach versus the hospital-based approach in managing suspected obstructive sleep apnea syndrome. Sci Rep 7, 45901 (2017). https://doi.org/10.1038/srep45901
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/srep45901
This article is cited by
-
Content Comparison of Quality-of-Life Instruments Used in Economic Evaluations of Sleep Disorder Interventions: A Systematic Review
PharmacoEconomics (2024)
-
Initiation of therapy for obstructive sleep apnea syndrome: a randomized comparison of outcomes of telemetry-supported home-based vs. sleep lab-based therapy initiation
Sleep and Breathing (2022)
-
Economic evaluation of diagnostic sleep studies for obstructive sleep apnoea: a systematic review protocol
Systematic Reviews (2021)
-
A machine learning-based test for adult sleep apnoea screening at home using oximetry and airflow
Scientific Reports (2020)
-
Patient characteristics affecting accurate detection of sleep apnea using a bed sheet-type portable monitor
Sleep and Breathing (2020)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.