Abstract
PG2 is an infusible polysaccharide extracted from Astragalus membranaceus, which is a Chinese herb traditionally used for stroke treatment. We investigated the effect of PG2 on patients with spontaneous acute intracerebral hemorrhage (ICH). A total of 61 patients with acute spontaneous ICH were randomized to either the treatment group (TG, 30 patients), which received 3 doses of PG2 (500 mg, IV) per week for 2 weeks, or the control group (CG, 31 patients), which received PG2 placebo. At 84 days after PG2 administration, the percentage of patients with a good Glasgow outcome scale (GOS 4–5) score in the TG was similar to that in the CG (69.0% vs. 48.4%; p = 0.2). The percentage of good mRS scores (0–2) in the TG was similar to that in the CG (62.1% vs. 45.2%; p = 0.3). In addition, no significant differences were seen when comparing differences in the C-reactive protein, erythrocyte sedimentation rate, interleukin-6 (IL-6), IL-1β, tumor necrosis factor-α, and S100B levels between baseline and days 4, 7, and 14 after PG2 administration (all p > 0.05). The results are preliminary, necessitating a more thorough assessment.
Similar content being viewed by others
Introduction
Hypertensive spontaneous intracerebral hemorrhage (ICH) is responsible for 10–15% of strokes, and is their most lethal cause, with a one-month mortality rate of 30–50%1. ICH is also associated with high levels of disability, with only 20% of survivors being functionally independent at 6 months and 36% of survivors remaining moderately to severely disabled at discharge2. Therefore, treatments that enhance the recovery of neurologic function are necessary. Astragalus membranaceus (AM) is a Chinese herb used extensively in China as a traditional treatment to facilitate recovery after a stroke. Our previous studies have demonstrated enhanced recovery of neurologic function in patients with acute hemorrhagic stroke who received AM. It is hypothesized that AM either reduces inflammatory response or reduces perihematomal edema3,4. AM can be administered only orally; by contrast, PG2, a polysaccharide extract from AM, has been approved for intravenous (IV) use in treating cancer-related fatigue in Taiwan5. Several preclinical studies have shown that PG2 stimulates the secretion of hematopoietic growth factors in activated human peripheral blood mononuclear cells6, enhances proliferation and maturation of peripheral blood cell progenitors in mitomycin C-treated mice7, and supports hematopoiesis in long-term bone marrow cultures8. These results indicate that PG2 can stimulate immunity and decrease inflammation.
The basal ganglion is the most common location of hypertensive spontaneous ICH, followed by the subcortical white matter, and then the cerebellum or pons9. Hematomas that extend to the ventricles, that are in a deep location, and that have a large mass and volume are associated with poor outcomes in patients with medium and large supratentorial ICH10. Hematoma size can affect the six-month survival rate after stroke. For instance, patients with hematomas with a volume of <29 mL have a survival rate of 64%, whereas patients with hematomas with a volume of >60 mL have a survival rate of 15%11. Both hematoma size and brain edema, which are caused by the breakdown of the brain–blood barrier (BBB), can cause cerebral ischemia, resulting in primary brain damage. In addition, several factors may induce secondary brain damage: (1) the presence of heme and iron, from erythrocyte lysis and free hemoglobin, which can incite reactive oxygen species production; (2) the disruption of the BBB, which can cause leucocyte infiltration; and (3) the presence of intracerebral blood, which can induce microglial activation, systemic immune cell infiltration, and the generation of proinflammatory cytokines such as tumor necrosis-α (TNF-α), interleukin-1beta (IL-1β), interleukin-6 (IL-6), and other chemokines12,13,14. Inflammatory response thus plays a critical role in the pathophysiology of ICH.
We hypothesize that the anti-inflammatory response induced by PG2 can counter the inflammatory response induced by ICH, which in turn enhances the recovery of neurologic function. Therefore, in the present preliminary double-blind, randomized, placebo-controlled study, we evaluated the effect of PG2 on patients with acute spontaneous ICH.
Materials and Methods
Subjects
Patients were recruited from the neurosurgery and emergency departments of China Medical University Hospital, Taichung City, Taiwan, from March 30, 2011, to June 14, 2013. All patients were recruited within 24 h of ICH onset. The study complied with the ethical principles of clinical trials as dictated in the Declaration of Helsinki. The protocol was approved by the Institutional Review Board of China Medical University Hospital (IRB: DMR100-IRB-005; NIH registration NCT 01325233, March 28, 2011), and informed consent was provided by patients prior to inclusion in the study. The study also abided by the International Conference on Harmonization and Good Clinical Practice guidelines. The inclusion criteria were as follows: (1) both female and male patients, (2) between the ages of 30 and 80 years, (3) admission within 24 h of ICH onset, (4) first incidence of hemorrhagic stroke with the hematoma located in the putamen, and (5) a signed informed consent by the patient or their legal representative. The exclusion criteria were as follows: (1) recent thrombolysis treatment, (2) history of previous stroke, (3) full-dose or long-term anticoagulation therapy, (4) hemorrhagic stroke but the location was not the putamen, (5) coexisting systemic diseases such as terminal cancer, renal failure, liver cirrhosis, severe dementia, or psychosis, (6) participation in another clinical trial within the last three months, (7) pregnancy or lactation, and (8) planned surgical evacuation of hematoma.
Preparation of PG2
The investigational drug PG2 (PhytoHealth Corp., Taiwan) was extracted from AM as previously described6,7,8. PG2 is an IV injectable extract of AM polysaccharide approved by the Taiwan Food and Drug Administration for cancer-related fatigue (Drug No. 054853). Prior to administration, this polysaccharide mixture was formulated as a sterile powder. The PG2 sterile powder was stored in the clinical trial pharmacy department of China Medical University Hospital. The pharmacist used a vial of PG2 (500 mg) reconstituted with 10 mL normal saline and shaken thoroughly until completely dissolved. It was then injected into a bag of normal saline (490 mL) and mixed well prior to intra-venous (IV) infusion at 150–200 mL/h. The appearance and odor of PG2 injection was not different from that of a normal saline injection based on naked sensory assessment.
Design and Sample Size
The present study was a preliminary, single-center, double-blind, placebo-controlled, randomized phase II/III study. Sample size was calculated according to the hypothesis that PG2 can increase a patient’s good outcome score (mRS score ≤2) percentage in ten dimensions. We further hypothesized that the increase in mRS scores would be evident when comparing mRS scores at the baseline (prior to PG2 administration) to those at one week (W1), four weeks (W4) and twelve weeks (W12) after PG2 administration. According to our previous results3, a sample size of 46 patients (23 per group) was necessary to achieve a statistical power of 90%. Assuming a patient follow-up rate of 0.8, at least 58 patients were required for this study.
Randomization and Grouping
Subjects were randomly assigned to either the treatment group (TG) or the control group (CG). The statistical center of China Medical University applied a block randomization with a block size of two or four by using computer generated random numbers. The random numbers were placed in a sealed envelope that was then sent to the manufacturer of PG2. The manufacturer packed and labelled the study drug package with a random number, and then forwarded it to the clinical trial pharmacy. The labelled package was managed by a specific pharmacist. After screening and meeting the inclusion and exclusion criteria, the subjects signed the informed consent form. The coordinator then called the pharmacist to enroll a new subject. The pharmacist then dispensed the drug according to the sequence number. In the TG, the subjects received an IV injection of PG2 (500 mg in 500 mL saline) once daily 3 days per week for 2 weeks after starting treatment within 24 hours of stroke onset. All patients received the standard treatment according to the Guidelines for the Management for Spontaneous Intracerebral Hemorrhage (American Stroke Association, 2010)15. The CG patients received an IV injection of PG2 placebo (500 mL, normal saline). Thus, the study team could not distinguish the placebo from true PG2. The patients, investigators, coordinator, and study nurse were blinded.
Outcome measures
The primary outcome measures were the change in the percentage of good Glasgow outcome scale (GOS) and/or Modified Rankin scale (mRS) scores after PG2 treatment. Good outcome scores were defined as GOS scores of 4–5 and mRS scores of 0–2. Bad outcome scores were defined as GOS scores of 1–3 and mRS scores of 3–5. The secondary outcome measures included changes in C-reactive protein (CRP), erythrocyte sedimentation rate (ESR), interleukin-6 (IL-6), interleukin-1β (IL-1β), tumor necrosis factor-α (TNF-α), and S100B calcium-binding protein B (S100B) after PG2 treatment.
A certified clinical trial coordinator blinded to the groups assessed the GOS, mRS scores at baseline (B), one week (7 ± 1 days; W1), four weeks (28 ± 4 days; W4) and 12 weeks (84 ± 10 days; W12) after PG2 administration. CRP, ESR, IL-6, IL-1β, TNF-α, and S100B were assessed at B and at Days 4 (D4), 7 (D7), and 14 (D14) after PG2 administration.
CRP, ESR, IL-6, IL- IL-1β, TNF-α, and S100B measurement
Four mL of blood was drawn from the cubital vein at the baseline and at days 4, 7, and 14 after PG2 administration. The blood was divided into two tubes containing 2.0 mL of blood each. One tube was sent to the laboratory department of China Medical University Hospital for CRP and ESR measurements. The other tube was sent for IL-6, IL-1β, TNF-α, and S100B measurements to the neuroscience laboratory of China Medical University. The samples were centrifuged for 10 min at 3600 rpm, and the supernatant was immediately stored at −20 °C until analysis. The IL-1β, IL-6, TNF-α, and S100B levels were measured using commercial enzyme-linked immunosorbent assay (ELISA) kits (IL-1β, IL-6 and TNF-α; eBioscience, USA; S100B, Millipore, USA) and an ELISA reader (BioTek Instruments, USA). No cross-reactivity or interference with other related interleukins was observed. The data were represented in picograms per milliliter, and all assays were performedduplicate. The ELISA kit sensitivities for IL-1B, IL-6, TNF-a, and S100B are 0.3 pg/mL, 0.92 pg/mL, 2.3 pg/mL, and 2.7 pg/mL.
Statistical Analysis
Baseline variables were compared using a two-group t-test for continuous variables (e.g., age) and a chi-squared (χ2) test for categorical variables (e.g., gender). Intention-to-treat analysis was used. The efficacy variables of the two groups were compared at B, W1, W4, and W12, respectively. The two-sample t-test was used separately for each comparison. To consider multiple testing, p-values were reported using false discovery rate method, a linear step up adjustment for false discovery rate. To allow for the possibility of nonnormal distribution, the nonparametric Mann–Whitney test was performed. All analyses were performed using SAS version 9.2 (SAS Institute Inc., Cary, NC); p ≤ 0.05 was considered statistically significant.
Results
Baseline demographic data characteristics
Sixty-one patients with acute spontaneous ICH were recruited into this study and were randomized to either the CG (31 patients) or the TG (30 patients). Six patients dropped out in the CG: three dropped out due to pruritus, two were lost to follow-up, and one died of congestive heart failure. Eight patients dropped out in the TG: three dropped out due to pruritus, two because of the presence of hematomas not located in the putamen, one owing to having a craniotomy performed, and two were lost to follow-up. The remaining 47 patients (25 in the CG and 22 in the TG) completed the trial (Fig. 1). Baseline characteristics—namely gender, age, body temperature (BT), blood pressure (including systolic blood pressure and diastolic blood pressure), atrial fibrillation, ischemic heart disease, diabetic mellitus, use of statins and antiplatelet medications, Glasgow coma scale score, intraventricular hemorrhage (IVH), hematoma size and location (i.e., right or left hemisphere)—in the CG and TG did not differ significantly (Table 1).
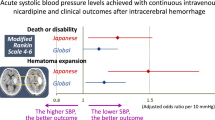
Effect of PG2 on the percentage of good and bad GOS and mRS scores in patients with acute spontaneous ICH
The percentage of good and bad GOS scores at B, W1, W4 and W12 did not differ significantly between CG and TG (all p > 0.05; Table 2).
The percentage of good and bad mRS scores at B, W1, W4, and W12 did not differ significantly between the CG and the TG (all p > 0.05; Table 2).
Effect of PG2 on CRP, ESR, IL-6, IL-1β, TNF-α, and S100B in patients with acute spontaneous ICH
The CRP, ESR, IL-6, IL-1β, TNF-α, and S100B levels at B, D4, D7, and D14 did not differ significantly between the CG and TG (all p > 0.05; Table 3). No significant differences were seen when comparing differences in the CRP, ESR, IL-6, IL-1β, TNF-α, and S100B levels between B and D4, D7, and D14 (all p > 0.05; Table 3).
Regarding the area under the curve measures, the percentage of log CRP, ESR, IL6, IL-1β, TNF-α, and S100B from baseline to D14 after PG2 treatment were not significantly different between the CG and the TG (all p > 0.05; Table 4).
Adverse events
The adverse events encountered in the present study included headache, cough, fever, constipation, skin puritis, and urinary problems. These adverse events were not significantly different for CG and TG (all p > 0.05; Table 5). One patient died of congenital heart failure because of myocardial infarction induced by factors unrelated to the study medications.
Discussion
The present study demonstrated that there was no significant difference between the CG and the TG regarding the percentages of good GOS and mRS scores at B, W1, W4, and W12. The CRP, ESR, IL-6, IL-1β, TNF-α, and S100B levels at B, D4, D7, and D14 did not differ significantly between the CG and TG. No significant differences were seen when comparing differences in the CRP, ESR, IL-6, IL-1β, TNF-α, and S100B levels between B and D4, D7, and D14. Taken together, these results suggest administration of PG2 for 2 weeks would not increase the percentage of good GOS and mRS scores, and that also not produced any anti-inflammatory properties. The Surgical Trial in Intracerebral Hemorrhage group found no significant difference in neurological function and mortality rates between patients treated with early surgery and those who received conservative treatment16,17. Physiological responses to hematomas and hematoma degradation products may contribute to the development of inflammatory reactions18,19,20. Inflammation begins immediately after hematoma formation, and increasing evidence suggests that inflammation is a crucial contributor to ICH-induced secondary brain injury19. The mechanisms of ICH-induced brain damage mediated by inflammation are complex and involve multiple signaling pathways19. Anti-inflammatory medications provide potential strategies for treating ICH. Preclinical experiments have reported that inhibition of the inflammatory response is an effective approach in the treatment of ICH21. ICH causes perihematomal edema, which increases the mass effect and intracranial pressure (ICP) and may exacerbate brain damage or even lead to cerebral herniation22,23. Increased ICP may reduce microcirculation through mechanical compression24,25, and edema may change osmotic gradients and disrupt the BBB resulting in direct toxicity to the neurons and glia26,27. Many studies have reported that increased water content, also called perihematomal edema, is involved in apoptosis and necrosis after ICH28,29,30. Studies have also shown that antioxidant therapy can decrease brain edema31. AM polysaccharides increased splenic lymphocyte proliferation and IL-2 levels in rats with gastric neoplasia, indicating that they play an anti-inflammatory and immune modulating role32. They also decrease CD40 expression32,33, which has both inflammatory and anti-inflammatory actions in renal proximal tubular epithelial cells, as well as regulating these two processes34. In addition, AM polysaccharides have antioxidant properties, scavenging superoxide anions and hydroxyl radicals33.
Serum CRP levels increase in response to inflammation and following IL-6 secretion35. CRP levels >10 mg/L are predictive factors for early hematoma growth and worsening neurologic function in patients with acute spontaneous ICH36. ESR is a nonspecific test in which an increase in ESR suggests the presence of inflammation. ESR is often used as a laboratory indicator to assess clinical disease in patients with polymyalgia rheumatic and giant cell arteritis37. Both TNF-α and IL-1β are proinflammatory cytokines that play an important role in inflammation and BBB disruption after ICH. TNF-α is secreted from neurons and activated microglia and astrocytes. IL-β is produced and secreted by activated microglia and astrocytes. In a porcine model of ICH, TNF-α and IL-1β expression measurements at 4 h after ICH revealed decreased TNF-α levels. However, the IL-1β levels did not decrease even 24 h after ICH38. TNF-α antibodies, such as CNTO 5048, reduced inflammation and improved functional outcome in a murine ICH model39. By contrast, TNF-α was found to have anti-inflammatory effects through negatively regulating inflammation40. Thus, TNF-α plays a dual role in the regulation of inflammation. In a murine model of hypertensive ICH, IL-1β levels correlated positively with brain edema41. IL-6 levels were elevated after ICH and correlated with blood volume and the mass effect42. IL-6 has both a proinflammatory and an immunomodulatory role, and may be proinflammatory after acute stroke; however, it is not involved in brain damage43. In addition, IL-6 has both anti-inflammatory and immunosuppressive properties44. S100B is a Ca2+ binding protein present in the central nervous system, mainly in glial cells. Serum levels rise after ICH, and S100B levels have a positive correlation with hematoma volume and can predict early neurologic deterioration and unfavorable outcomes 3 months after acute spontaneous ICH45. Serum S100B levels increase prior to thrombolytic treatment and may predict the risk of hemorrhagic transformation in patients with acute stroke46. Several studies have reported that Serum S100B is an early marker of BBB disruption47,48, but this may have no relevance to neuronal damage47.
Similar adverse events including headache, cough, fever. diarrhea, vomiting, constipation, skin puritis, and urinary problems was were observed in the CG and TG in the present study. One patient died because of heart failure, which was unrelated to PG2 administration and involved a history of myocardial infarction. Overall, administration of IV PG2 for two weeks is safe.
The limitations of this study are as follows: (1) a small sample size, (2) a short investigation time of only 3 months after ICH, and (3) a safety evaluation of IV PG2 based on administration only 6 times in 2 weeks. These drawbacks can be overcome by (1) performing a larger study, (2) observing patient follow-up for more than 3 months, and (3) re-evaluating post-PG2 safety more frequently and for a longer duration than in this study.
IV PG2 administration for 2 weeks did not increase the percentage of good GOS and mRS scores, and that also not produced any anti-inflammatory properties. However, these results are preliminary and conducting a more thorough assessment of them is necessary.
Additional Information
How to cite this article: Chen, C.-C. et al. PG2 for patients with acute spontaneous intracerebral hemorrhage: a double-blind, randomized placebo-controlled study. Sci. Rep. 7, 45628; doi: 10.1038/srep45628 (2017).
Publisher's note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
Kase, C. S & Caplan, L. R. Intracerebral hemorrhage (Butterworth-Heinemann Medical, 1994).
Sze, K. H., Wong, E., Or, K. H., Lum, C. M. & Woo, J. Factors predicting stroke disability at discharge: a study of 793 Chinese. Archives of physical medicine and rehabilitation 81, 876–880 (2000).
Chen, C. C. et al. Chinese Herb Astragalus membranaceus Enhances Recovery of Hemorrhagic Stroke: Double-Blind, Placebo-Controlled, Randomized Study. Evidence-based complementary and alternative medicine: eCAM 2012, 708452, doi: 10.1155/2012/708452 (2012).
Wei, G., Ji, X., Bai, H. & Ding, Y. Stroke research in China. Neurological research 28, 11–15, doi: 10.1179/016164106x91807 (2006).
Chen, H. W. et al. A novel infusible botanically-derived drug, PG2, for cancer-related fatigue: a phase II double-blind, randomized placebo-controlled study. Clinical and investigative medicine. Medecine clinique et experimentale 35, E1–11 (2012).
Lou, X., Zhang, B., Song, J., Liu, B. & Deng, X. Effect of Astragalus Polysaccharide in Stimulating the Secretion of Hematopoietic Growth Factors from Activated Human PBMC [J]. Traditional Chinese Drug Research & Clinical Pharmacology 5, 006 (2003).
Shao, B. M. et al. A study on the immune receptors for polysaccharides from the roots of Astragalus membranaceus, a Chinese medicinal herb. Biochemical and biophysical research communications 320, 1103–1111, doi: 10.1016/j.bbrc.2004.06.065 (2004).
Wang, Y. F. et al. Protective effect of Astragalus polysaccharides on ATP binding cassette transporter A1 in THP-1 derived foam cells exposed to tumor necrosis factor-alpha. Phytotherapy research: PTR 24, 393–398, doi: 10.1002/ptr.2958 (2010).
Siddique, M. S. & Mendelow, A. D. Surgical treatment of intracerebral haemorrhage. Br Med Bull 56, 444–456 (2000).
Castellanos, M. et al. Predictors of good outcome in medium to large spontaneous supratentorial intracerebral haemorrhages. Journal of neurology, neurosurgery, and psychiatry 76, 691–695, doi: 10.1136/jnnp.2004.044347 (2005).
Salihovic, D., Smajlovic, D. & Ibrahimagic, O. C. Does the volume and localization of intracerebral hematoma affect short-term prognosis of patients with intracerebral hemorrhage? ISRN neuroscience 2013, 327968, doi: 10.1155/2013/327968 (2013).
Karwacki, Z. et al. The pathophysiology of intracerebral haemorrhage. Folia morphologica 65, 295–300 (2006).
Wang, J. & Dore, S. Inflammation after intracerebral hemorrhage. Journal of cerebral blood flow and metabolism: official journal of the International Society of Cerebral Blood Flow and Metabolism 27, 894–908, doi: 10.1038/sj.jcbfm.9600403 (2007).
Mracsko, E. & Veltkamp, R. Neuroinflammation after intracerebral hemorrhage. Frontiers in cellular neuroscience 8, 388, doi: 10.3389/fncel.2014.00388 (2014).
Morgenstern, L. B. et al. Guidelines for the management of spontaneous intracerebral hemorrhage: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke; a journal of cerebral circulation 41, 2108–2129, doi: 10.1161/STR.0b013e3181ec611b (2010).
Mendelow, A. D. et al. Early surgery versus initial conservative treatment in patients with spontaneous supratentorial intracerebral haematomas in the International Surgical Trial in Intracerebral Haemorrhage (STICH): a randomised trial. Lancet (London, England) 365, 387–397, doi: 10.1016/s0140-6736(05)17826-x (2005).
Mendelow, A. D. et al. Early surgery versus initial conservative treatment in patients with spontaneous supratentorial lobar intracerebral haematomas (STICH II): a randomised trial. Lancet (London, England) 382, 397–408, doi: 10.1016/s0140-6736(13)60986-1 (2013).
Lok, J. et al. Intracranial hemorrhage: mechanisms of secondary brain injury. Acta neurochirurgica. Supplement 111, 63–69, doi: 10.1007/978-3-7091-0693-8_11 (2011).
Chen, S., Yang, Q., Chen, G. & Zhang, J. H. An update on inflammation in the acute phase of intracerebral hemorrhage. Translational stroke research 6, 4–8, doi: 10.1007/s12975-014-0384-4 (2015).
Hatakeyama, T., Okauchi, M., Hua, Y., Keep, R. F. & Xi, G. Deferoxamine reduces neuronal death and hematoma lysis after intracerebral hemorrhage in aged rats. Translational stroke research 4, 546–553, doi: 10.1007/s12975-013-0270-5 (2013).
Yang, Z., Zhao, T., Zou, Y., Zhang, J. H. & Feng, H. Curcumin inhibits microglia inflammation and confers neuroprotection in intracerebral hemorrhage. Immunology letters 160, 89–95, doi: 10.1016/j.imlet.2014.03.005 (2014).
Zazulia, A. R., Diringer, M. N., Derdeyn, C. P. & Powers, W. J. Progression of mass effect after intracerebral hemorrhage. Stroke; a journal of cerebral circulation 30, 1167–1173 (1999).
Inaji, M. et al. Chronological changes of perihematomal edema of human intracerebral hematoma. Acta neurochirurgica. Supplement 86, 445–448 (2003).
Langfitt, T. W., Weinstein, J. D., Kassell, N. F. & Gagliardi, L. J. TRANSMISSION OF INCREASED INTRACRANIAL PRESSURE. II. WITHIN THE SUPRATENTORIAL SPACE. Journal of neurosurgery 21, 998–1005, doi: 10.3171/jns.1964.21.11.0998 (1964).
Nath, F. P., Jenkins, A., Mendelow, A. D., Graham, D. I. & Teasdale, G. M. Early hemodynamic changes in experimental intracerebral hemorrhage. Journal of neurosurgery 65, 697–703, doi: 10.3171/jns.1986.65.5.0697 (1986).
Lee, K. R., Kawai, N., Kim, S., Sagher, O. & Hoff, J. T. Mechanisms of edema formation after intracerebral hemorrhage: effects of thrombin on cerebral blood flow, blood-brain barrier permeability, and cell survival in a rat model. Journal of neurosurgery 86, 272–278, doi: 10.3171/jns.1997.86.2.0272 (1997).
Freeman, W. D. et al. Computer-assisted volumetric analysis compared with ABC/2 method for assessing warfarin-related intracranial hemorrhage volumes. Neurocritical care 9, 307–312, doi: 10.1007/s12028-008-9089-4 (2008).
Holmin, S. & Mathiesen, T. Intracerebral administration of interleukin-1beta and induction of inflammation, apoptosis, and vasogenic edema. Journal of neurosurgery 92, 108–120, doi: 10.3171/jns.2000.92.1.0108 (2000).
Wang, H. & Reiser, G. Thrombin signaling in the brain: the role of protease-activated receptors. Biological chemistry 384, 193–202, doi: 10.1515/bc.2003.021 (2003).
Venkatasubramanian, C. et al. Natural history of perihematomal edema after intracerebral hemorrhage measured by serial magnetic resonance imaging. Stroke; a journal of cerebral circulation 42, 73–80, doi: 10.1161/strokeaha.110.590646 (2011).
Lyden, P. D. et al. Safety and tolerability of NXY-059 for acute intracerebral hemorrhage: the CHANT Trial. Stroke; a journal of cerebral circulation 38, 2262–2269, doi: 10.1161/strokeaha.106.472746 (2007).
Rui, L., Wei-chang, C., Wei-peng, W., Wen-yan, T. & Xue-guang, Z. Optimization of extraction technology of Astragalus polysaccharides by response surface methodology and its effect on CD40. Carbohydrate Polymers 78, 784–788, doi: 10.1016/j.carbpol.2009.06.018 (2009).
Li, R., Chen, W.-c., Wang, W.-p., Tian, W.-y. & Zhang, X.-g . Antioxidant activity of Astragalus polysaccharides and antitumour activity of the polysaccharides and siRNA. Carbohydrate Polymers 82, 240–244, doi: 10.1016/j.carbpol.2010.02.048 (2010).
Laxmanan, S., Datta, D., Geehan, C., Briscoe, D. M. & Pal, S. CD40: a mediator of pro- and anti-inflammatory signals in renal tubular epithelial cells. Journal of the American Society of Nephrology: JASN 16, 2714–2723, doi: 10.1681/asn.2005010045 (2005).
Thompson, D., Pepys, M. B. & Wood, S. P. The physiological structure of human C-reactive protein and its complex with phosphocholine. Structure (London, England: 1993) 7, 169–177, doi: 10.1016/s0969-2126(99)80023-9 (1999).
Di Napoli, M. et al. C-reactive protein predicts hematoma growth in intracerebral hemorrhage. Stroke; a journal of cerebral circulation 45, 59–65, doi: 10.1161/strokeaha.113.001721 (2014).
Kyle, V., Cawston, T. E. & Hazleman, B. L. Erythrocyte sedimentation rate and C reactive protein in the assessment of polymyalgia rheumatica/giant cell arteritis on presentation and during follow up. Annals of the rheumatic diseases 48, 667–671 (1989).
Bimpis, A. et al. Neuronal tumour necrosis factor-alpha and interleukin-1beta expression in a porcine model of intracerebral haemorrhage: Modulation by U-74389G. Brain research 1615, 98–105, doi: 10.1016/j.brainres.2015.04.034 (2015).
Lei, B. et al. Tumor necrosis factor alpha antagonism improves neurological recovery in murine intracerebral hemorrhage. Journal of neuroinflammation 10, 103, doi: 10.1186/1742-2094-10-103 (2013).
Masli, S. & Turpie, B. Anti-inflammatory effects of tumour necrosis factor (TNF)-alpha are mediated via TNF-R2 (p75) in tolerogenic transforming growth factor-beta-treated antigen-presenting cells. Immunology 127, 62–72, doi: 10.1111/j.1365-2567.2008.02933.x (2009).
Wei, P., You, C., Jin, H., Chen, H. & Lin, B. Correlation between serum IL-1beta levels and cerebral edema extent in a hypertensive intracerebral hemorrhage rat model. Neurological research 36, 170–175, doi: 10.1179/1743132813y.0000000292 (2014).
Dziedzic, T. et al. Intracerebral hemorrhage triggers interleukin-6 and interleukin-10 release in blood. Stroke; a journal of cerebral circulation 33, 2334–2335 (2002).
Kim, J. S., Yoon, S. S., Kim, Y. H. & Ryu, J. S. Serial measurement of interleukin-6, transforming growth factor-beta, and S-100 protein in patients with acute stroke. Stroke; a journal of cerebral circulation 27, 1553–1557 (1996).
Tilg, H., Dinarello, C. A. & Mier, J. W. IL-6 and APPs: anti-inflammatory and immunosuppressive mediators. Immunology today 18, 428–432 (1997).
Delgado, P. et al. Plasma S100B level after acute spontaneous intracerebral hemorrhage. Stroke; a journal of cerebral circulation 37, 2837–2839, doi: 10.1161/01.STR.0000245085.58807.ad (2006).
Foerch, C. et al. Elevated serum S100B levels indicate a higher risk of hemorrhagic transformation after thrombolytic therapy in acute stroke. Stroke; a journal of cerebral circulation 38, 2491–2495, doi: 10.1161/strokeaha.106.480111 (2007).
Kapural, M. et al. Serum S-100beta as a possible marker of blood-brain barrier disruption. Brain research 940, 102–104 (2002).
Marchi, N. et al. Peripheral markers of blood-brain barrier damage. Clinica chimica acta; international journal of clinical chemistry 342, 1–12, doi: 10.1016/j.cccn.2003.12.008 (2004).
Acknowledgements
The study drug was supplied by PhytoHealth Corporation, which also paid a partial fee. The study was supported in part by the Taiwan Ministry of Health and Welfare Clinical Trial and Research Center of Excellence (MOHW106-TDU-B-212-113004), and also was supported by a grant from the Chinese Medicine Research Center, China Medical University (Ministry of Education, The aim for the Top Universities Plan) and partially by the grant from China Medical University Hospital (DMR100-111). We thank Professor Wen-Ling Liao for providing his opinions during revision.
Author information
Authors and Affiliations
Contributions
C.-C. Chen conducted the trial, participated in protocol design, and wrote the main manuscript text. X.-X. Chen performed the assessment, collected data, and wrote the main manuscript text. T.-C. Li designed and performed the statistical analysis. H.-L. Lin, Y.-T. Chu, H.-C. Lee, Y.-K. Cheng, D.-C. Chen, S.-C. Tsai, and D.-Y. Cho participated in patient recuritment. C.-L. Hsieh participated in the protocol design and revised the main manuscript text. All authors have reviewed and approved the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing financial interests.
Rights and permissions
This work is licensed under a Creative Commons Attribution 4.0 International License. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in the credit line; if the material is not included under the Creative Commons license, users will need to obtain permission from the license holder to reproduce the material. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/
About this article
Cite this article
Chen, CC., Chen, X., Li, TC. et al. PG2 for patients with acute spontaneous intracerebral hemorrhage: a double-blind, randomized, placebo-controlled study. Sci Rep 7, 45628 (2017). https://doi.org/10.1038/srep45628
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/srep45628
This article is cited by
-
SIRT1-Mediated HMGB1 Deacetylation Suppresses Neutrophil Extracellular Traps Related to Blood–Brain Barrier Impairment After Cerebral Venous Thrombosis
Molecular Neurobiology (2024)
-
Pharmacological Properties of Preparations Based on Astragalus Extract (Review)
Pharmaceutical Chemistry Journal (2020)
-
Incorporation of Astragalus polysaccharides injection during concurrent chemoradiotherapy in advanced pharyngeal or laryngeal squamous cell carcinoma: preliminary experience of a phase II double-blind, randomized trial
Journal of Cancer Research and Clinical Oncology (2020)
-
Inflammatory Profiles of the Interleukin Family and Network in Cerebral Hemorrhage
Cellular and Molecular Neurobiology (2018)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.