Abstract
Aim of this retrospective analysis was to evaluate the survival times after percutaneous irreversible electroporation (IRE) in inoperable liver tumors not amenable to thermal ablation. 71 patients (14 females, 57 males, median age 63.5 ± 10.8 years) with 103 liver tumors were treated in 83 interventions using IRE (NanoKnife® system). The median tumor short-axis diameter was 1.9 cm (minimum 0.4 cm, maximum 4.5 cm). 35 patients had primary liver tumors and 36 patients had liver metastases. The Kaplan-Meier method was employed to calculate the survival rates, and the different groups were compared using multivariate log-rank and Wilcoxon tests. The overall median survival time was 26.3 months; the median survival of patients with primary land secondary liver cancer did not significantly differ (26.8 vs. 19.9 months; p = 0.41). Patients with a tumor diameter >3 cm (p < 0.001) or more than 2 lesions (p < 0.005) died significantly earlier than patients with smaller or fewer tumors. Patients with hepatocellular carcinoma and Child-Pugh class B or C cirrhosis died significantly earlier than patients with Child-Pugh class A (p < 0.05). Patients with very early stage HCC survived significantly longer than patients with early stage HCC with a median survival of 22.3 vs. 13.7 months (p < 0.05).
Similar content being viewed by others
Introduction
Although hepatocellular carcinoma (HCC) is comparatively rare in Western countries, it is the most frequently occurring solid tumor worldwide, with an annual incidence in excess of one million new patients1,2,3,4,5,6. Apart from primary surgical resection and liver transplantation, there are few curative treatment options for HCC. The survival rates are low for surgical intervention (36–70%) and transplantation (60–70%)7,8,9,10. At the time of initial diagnosis, only 10–20% of patients are candidates for surgery and consequently potentially curable. Contraindications for resection generally include multifocal disease, the inability to achieve complete tumor removal and an impaired functional reserve of the liver due to underlying cirrhosis11,12,13. HCC is one of the deadliest human malignancies because there are few curative treatment options for primary, non-resectable hepatic lesions. Of all patients with HCC, 94% will die from the disease14.
In Europe and the USA, colorectal liver metastases (CRLMs) are the most frequent cause of malignant liver tumors15. Frequently, and particularly in the case of patients with colorectal carcinoma, the liver is the sole site of metastasis16. As in HCC, approximately 70–80% of patients with liver metastases are inoperable at the time of diagnosis17,18,19.
Because only a small proportion of patients with liver tumors suffer from an operable tumor disease, new treatment approaches are being investigated to control or even remove liver tumors. In the past two decades, image-guided ablation techniques for focal tumor treatment have attracted substantial attention. Most of these techniques rely on the application of thermal energy for tumor ablation. Irreversible electroporation (IRE) is a non-thermal ablation technique that is currently under early clinical investigation20. The aim of this retrospective assessment was to analyze the survival of 71 patients with primary or secondary liver tumors after percutaneous IRE.
Materials and Methods
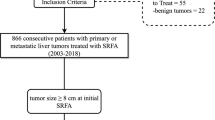
For this retrospective study with anonymized patients, approval from the institutional ethical committee was waived. Between October 2011 and July 2015, 71 patients (14 females, 57 males, median age 63.5 ± 10.8 years) with 103 liver tumors were treated via 83 interventions using IRE (NanoKnife® system; Latham, NY, United States) (Table 1). These patients included 35 (49.3%) with primary liver tumors (hepatocellular and cholangiocellular carcinoma) and 36 (50.7%) with liver metastases. The median tumor diameter was 1.9 cm (range 0.4–4.5 cm).The median time period between resection of the primary tumor and the occurrence of liver metastasis was 22.3 ± 14.5 months. Table 2 shows the baseline tumor characteristics.
Each patient was individually discussed within an interdisciplinary tumor board to ensure that all treating physicians agreed with the suggested therapeutic plan. All patients signed a written consent form in accordance with the institutional guidelines. All patients with a primary or secondary liver tumor had no clinical or radiological indications of extrahepatic tumor spread. Patients with cirrhosis of the liver and a related volume of ascites received ascites drainage prior to the start of intervention. Table 3 illustrates the study inclusion/exclusion criteria.
Staging was performed pre-interventionally using computed tomography (CT) of the thorax, abdomen and pelvis (Fig. 1). In addition, MRI of the liver was performed using a liver-specific contrast agent (GD-EOB-DTPA) (Fig. 2).
Same patient as in Fig. 1: pre-interventional MRI with liver-specific contrast agent (Gd-EOB-DTPA): (a) Hyperintense visualization of the HCC (arrow) in native fat-saturated T2-weighted sequence posterior to the main stem of the portal vein at the transition to liver segment I. (b) Dynamic T1-weighted fat-saturated sequence after contrast in arterial phase shows sluggish arterial hypervascularization of the HCC (arrow).(c) Dynamic T1-weighted fat-saturated sequence after contrast in portal venous phase shows the directly adjacent main stem of the portal vein (tip of arrow). (d) T1-weighted fat-saturated sequence in hepatobiliary phase with wash-out (arrow).
All interventions were performed under general anesthesia and mechanical ventilation with complete muscle relaxation. The electrodes of the NanoKnife® system (Angiodynamics; Latham, NY, US) were percutaneously inserted into all patients using CT fluoroscopy (CareVision, Somatom 16, Siemens, Erlangen, Germany) (Fig. 3).
Depending on the size of the target volume, 2–6 monopolar 18 G ablation electrodes were inserted to completely destroy the tumor and healthy liver tissue within a 1 cm safety margin around the tumor. Accordingly, the length of the tip had to be adapted to the size of the ablation volume (0.5–2.0 cm in 0.5 cm increments). The optimum distance between 2 parallel electrodes enclosing the tumor is between 0.7 and 2.0 cm. Once the correct needle position was verified, a 270 volt test pulse was emitted to ensure adequate conductivity of the tissue prior to initiating the actual ablation algorithm. If conductivity was inadequate, the position of the electrodes must be correspondingly corrected, and the self-test was repeated. The parameters of IRE ablation were 1,650–3,000 V, the pulse length was 90 μs, and 70 pulses were applied per cycle under constant EKG monitoring to avoid life-threatening arrhythmias.
To rule out complications, CT and MRI of the liver were performed post-interventionally before the patients were discharged (Fig. 4).
To evaluate the technical success of the intervention, an MRI of the liver was performed 6 weeks post ablation. The actual tumor response was first observed using MRI after 3 months and at 3-month intervals for 2 years after the intervention. Two years post-intervention, MRI scans of the liver were performed two times per year (Fig. 5).
Same patient as in Figs 1, 2, 3 and 4: Follow-up 2 years post-intervention: (a) Native, fat-saturated T2 sequence: cicatricial changes after IRE ablation with distinct shrinkage of the ablation defect. (b) Dynamic, fat-saturated T2 sequence after contrast: in arterial phase no indication of arterial hypervascularization (arrow), no indication of recurrence. (c) Dynamic fat-saturated T1 sequence after contrast: in portal venous phase continued full contrast of portal vein (tip of arrow). (d) Follow-up CT in the portal venous phase with full contrast of portal vein (tip of arrow) and distinct shrinkage of the hypodense ablation defect 2 years post-IRE (arrow).
Kaplan-Meier curves were plotted using SPSS (SPSS for Mac, Version 22, Chicago, IL, USA). The Cox proportional hazards model was used for multivariate analysis to evaluate prognostic factors. Factors determining local overall survival were compared using log rank analysis (p < 0.05 was considered significant). The investigated variables were the number of treated lesions, tumor diameter, underlying tumor disease, BCLC and Child-Pugh classification.
Results
At the end of the study, 36 patients were still alive. Complete ablation, as documented during the 6-week follow-up, was achieved in 95 of 103 lesions (92.2%); 8 lesions required re-treatment due to incomplete ablation (7.8%). The median total survival time was 26.3 months. Local tumor response was not the object of the study. However, after a median follow-up of 35.7 months, 33 of 103 treated lesions (31.7%) demonstrated local recurrence. Therapy-associated side effects were also not the primary aim of this study. However, during 83 interventions, we observed 5 major complications (liver abscess, n = 4; myocardial infarction, n = 1) and 7 minor complications (pneumothorax, n = 2; cardiac arrhythmia, n = 2; hematoma, n = 3). No minor complications required any further treatment.
The median survival of patients with secondary liver tumors was 19.9 months, which was shorter than that of patients with primary liver carcinoma (26.8 months). However, the survival rate did not significantly differ between these two groups (p(LogRank) = 0.41; p(Wilcoxon) = 0.73).
Patients whose tumor was greater than 3 cm (p(Log-Rank and Wilcoxon) < 0.001) exhibited a considerably shorter lifespan. The average survival time of patients with a tumor diameter ≤3 cm was 24.5 months (median survival time was not achieved). The survival time of patients with a tumor diameter >3 cm was 12.9 months (median survival time 9.5 months).
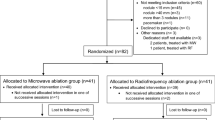
Furthermore, patients with 3 or more lesions demonstrated significantly shorter survival rates (p(Log-Rank) < 0.005; p(Wilcoxon) < 0.005). The median lifespan of patients with no more than 2 lesions was 32.8 months. Those with 3 or more lesions survived for 12.4 months (Fig. 6).
Kaplan-Meier curves: (A) The solid line shows the survival time for patients with primary liver tumors (hepatocellular and cholangiocellular carcinoma); the dashed line illustrates the survival time of patients with liver metastases. The survival time of both groups did not exhibit a significant difference. (B) The Kaplan-Meier survival curves show significantly better survival for patients with fewer than 3 tumors (solid line) when compared with patients with 3 or more tumors (dotted line). (C) Compared to patients with a tumor diameter greater than 3 cm (dashed line), the Kaplan-Meier survival curves show significantly better survival for patients with a short axis diameter less than 3 cm (solid line).
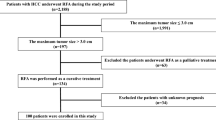
In a sub-group analysis of patients with HCC (Fig. 7), the survival times of patients with Child-Pugh B or C cirrhosis of the liver were significantly shorter that those in the Child-Pugh A cirrhosis group (p(Log-Rank) < 0.05). Average survival for Child-Pugh A cirrhosis was 19.3 months (median survival time was not reached). In Child-Pugh class B, mean survival was 14.5 months (median: 9.7 months), and in Child-Pugh class C, survival was 12.7 months (median: 10.4 months).
The Kaplan-Meier survival curves for patients with hepatocellular carcinoma: (A) significantly better survival of patients with Child-Pugh class A cirrhosis of the liver (solid line) compared to those with Child-Pugh class B (dashed line) and C (dotted line). (B) Significantly longer survival of patients with very early stage HCC (dashed line) according to the BCLC classification compared to patients with early stage HCC (solid line).
Also, patients with early stage HCC (stage 1) according to the Barcelona Clinic Liver Cancer Classification21 (single or max. 3 nodules smaller 3 cm, Child Pugh A, performance status 0) showed significant shorter survival rates in comparison to patients with very early stage (stage 0) HCC (single tumor with a diameter smaller then 2 cm, Child Pugh A, performance status 0): median survival was 22.3 vs. 13.7 months (p < 0.05).
Discussion
During the past two decades, image-guided percutaneous ablation techniques, such as radio frequency ablation or microwave ablation, have achieved a high level of acceptance, particularly – but not exclusively – with respect to inoperable liver tumors. Various studies have proven that radiofrequency ablation (RFA) is a safe therapeutic option with both low mortality and morbidity22,23. RFA has shown satisfactory results, with a local post-RFA tumor response rate of over 80% complete tumor ablation in most studies24. Likewise, when compared to percutaneous ethanol injection or chemotherapy alone, RFA has demonstrated a significantly higher probability of survival11. However, thermal ablation techniques are limited by the so-called heat sink effect. Tumors adjoining larger blood vessels cannot be ablated due to the temperature reduction caused by perfusion. Another limitation of thermal ablation is the risk of thermal damage to the tissue of adjacent structures25 or the blood vessels themselves. Typical examples of thermal damage after RFA on the liver are damage to the gallbladder, bile ducts and intestine26. Numerous strategies to protect adjoining structures against accidental thermal damage have been described27,28,29. Nevertheless, complete ablation of larger tumors (greater than 3 cm) or ablation of lesions in high-risk locations (such as adjacent to other organs or direct subcapsular position) remains problematic30. Several studies of thermal ablation have demonstrated that tumor size and/or an unfavorable (high-risk) site are considered negative prognosis factors for tumor recurrence31. The high local recurrence rate in these sites has a negative influence on the long-term outcome and is one of the main reasons thermal ablation is inferior to surgical resection with respect to outcome32. For example, Lam et al. prospectively treated 298 HCC patients using RFA and demonstrated a significantly shorter survival time for 25 patients whose tumors had been incompletely ablated33.
Electroporation is a dynamic phenomenon in which an external electrical field is used to exceed the capacity of the cell membrane, allowing nano-sized pores to be generated in the cell membrane. Depending on the amplitude and duration of the pulse application, electroporation is either reversible or irreversible. IRE results in the loss of cell homeostasis; however, the exact mechanism resulting in cell death remains unexplained. The hypothesis posed by Davalos et al. that IRE could be an independent method to ablate soft tissue has been confirmed by subsequent studies of liver cells and in animal models20,34,35. Moreover, the animal model demonstrated that blood vessels and bile ducts within or directly adjacent to the ablation zone remain undamaged34. Because thermal ablation techniques are frequently unsuitable for patients with inoperable tumors, chemotherapy frequently remains the sole palliative treatment, thus giving rise to significant interest in a new curative treatment option36. For most patients, IRE is currently considered the “last resort” from a therapeutic viewpoint. Likewise, the tumors investigated in this study were inoperable and not treatable using conventional thermal ablation. Nevertheless, an average survival time of 24.3 months was demonstrated for CRLM. This result is promising because chemotherapy would otherwise remain as the only palliative therapeutic alternative for these tumors. After chemotherapy, similar survival times of approximately 18 months have been reported for CLRM in palliative care (fluorouracil with oxaliplatin)37,38 and 21.7 months for capecitabine, irinotecan and oxaliplatin39, but without the burden of therapy associated systemic side effects.
Preclinical studies have demonstrated that IRE creates a well-defined boundary between ablated and non-ablated tissue; thus, the cells are either destroyed or remain intact. Compared with thermal ablation, perivascular tumor ablation with IRE appears to result in less frequent recurrence, indicating that the effectiveness of IRE is not influenced by the heat sink effect40. The current state of information does not permit a final statement on IRE. Larger prospective randomized studies will have to confirm these observations. The initial results with smaller hepatic tumors abutting vascular structures and the portal vein are very promising. The success rate is up to 90% but decreases rapidly in relation to tumor size41. Our previous study analyzing the risk factors for an early local recurrence demonstrated that similar to conventional (thermal) ablation techniques, a larger tumor diameter represents an independent risk factor for local recurrence40. Based on a study of 44 patients, Cannon et al. postulated that the best indication for IRE is in the case of tumors with a diameter ≤3 cm that are not accessible using a thermal ablation technique42. The results of our study point in the same direction because patients with a tumor diameter >3 cm die significantly earlier than those with smaller tumors (p < 0.001). However, this difference arises primarily because larger tumors are generally associated with greater biological activity and aggressiveness. Thus, larger tumors (diameter greater than 3 cm) may remain the domain of transarterial rather than percutaneous therapy.
In a prospective study, Thomson et al. investigated 63 tumors that had been treated using IRE. They found that HCC had distinctly better therapeutic results compared with liver metastases43. Likewise, an earlier study by our working group investigated early recurrence after percutaneous therapy using IRE and found that HCC tumors exhibited fewer earlier recurrences compared with other diagnoses40. In our current study, patients with HCC demonstrated a longer survival time (26.8 months) compared with those with liver metastases, yet this difference was not comparatively significant. One possible explanation for this phenomenon is that there is different tumor biology between primary and secondary liver cancer leading to different IRE effectiveness.
Overall, it is difficult to draw broad conclusions regarding the impact that percutaneous therapeutic procedures, specifically IRE in our case, have on the total survival time or which additional factors affect treatment using IRE. In addition to this general problem, our analysis has several further limitations, the most important of which is the retrospective nature of the study. Moreover, the patients investigated in the study represent a selected population with distinctly heterogeneous tumor characteristics. In addition, the number of included patients is small, and the follow-up was limited to only 3 years.
Nonetheless, we consider these initial results to be highly promising for the treatment of malignant liver tumors compared with other therapeutic concepts, at least with respect to comparable survival times. Prospective randomized controlled studies with a larger number of patients and longer-term follow-up are required to demonstrate whether IRE, compared with other therapeutic regimes, is superior with respect to survival, local therapeutic outcome and side effects.
Additional Information
How to cite this article: Niessen, C. et al. Percutaneous Irreversible Electroporation: Long-term survival analysis of 71 patients with inoperable malignant hepatic tumors. Sci. Rep. 7, 43687; doi: 10.1038/srep43687 (2017).
Publisher's note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
Parkin, D. M., Bray, F. I. & Devesa, S. S. Cancer burden in the year 2000. The global picture. European journal of cancer 37 Suppl 8, S4–66 (2001).
Arya, S. C., Ashraf, S. J., Parande, C. M., Tobeiqi, M. S. & Ageel, A. R. Hepatitis B and delta markers in primary hepatocellular carcinoma patients in the Gizan area of Saudi Arabia. APMIS. Supplementum 3, 30–34 (1988).
Beasley, R. P. Hepatitis B virus. The major etiology of hepatocellular carcinoma. Cancer 61, 1942–1956 (1988).
Bridbord, K. Pathogenesis and prevention of hepatocellular carcinoma. Cancer detection and prevention 14, 191–192 (1989).
Di Bisceglie, A. M., Rustgi, V. K., Hoofnagle, J. H., Dusheiko, G. M. & Lotze, M. T. NIH conference. Hepatocellular carcinoma. Annals of internal medicine 108, 390–401 (1988).
Di Bisceglie, A. M. Hepatocellular carcinoma: molecular biology of its growth and relationship to hepatitis B virus infection. The Medical clinics of North America 73, 985–997 (1989).
Figueras, J. et al. Resection or transplantation for hepatocellular carcinoma in cirrhotic patients: outcomes based on indicated treatment strategy. Journal of the American College of Surgeons 190, 580–587 (2000).
Margarit, C. et al. Resection for hepatocellular carcinoma is a good option in Child-Turcotte-Pugh class A patients with cirrhosis who are eligible for liver transplantation. Liver transplantation: official publication of the American Association for the Study of Liver Diseases and the International Liver Transplantation Society 11, 1242–1251, doi: 10.1002/lt.20398 (2005).
Bigourdan, J. M. et al. Small hepatocellular carcinoma in Child A cirrhotic patients: hepatic resection versus transplantation. Liver transplantation: official publication of the American Association for the Study of Liver Diseases and the International Liver Transplantation Society 9, 513–520, doi: 10.1053/jlts.2003.50070 (2003).
Llovet, J. M., Fuster, J. & Bruix, J. Intention-to-treat analysis of surgical treatment for early hepatocellular carcinoma: resection versus transplantation. Hepatology 30, 1434–1440, doi: 10.1002/hep.510300629 (1999).
Bruix, J., Sherman, M. & Practice Guidelines Committee, A. A. f. t. S. o. L. D. Management of hepatocellular carcinoma. Hepatology (Baltimore, Md.) 42, 1208–1236, doi: 10.1002/hep.20933 (2005).
Ryder, S. D. & British Society of, G. Guidelines for the diagnosis and treatment of hepatocellular carcinoma (HCC) in adults. Gut 52 Suppl 3, iii1–8 (2003).
Ikai, I. et al. Report of the 18th follow-up survey of primary liver cancer in Japan. Hepatology Research 40, 1043–1059, doi: 10.1111/j.1872-034X.2010.00731.x (2010).
Leong, T. Y. M. & Leong, A. S. Y. Epidemiology and carcinogenesis of hepatocellular carcinoma. HPB: The Official Journal of the International Hepato Pancreato Biliary Association 7, 5–15, doi: 10.1080/13651820410024021 (2005).
Scheele, J. Hepatectomy for liver metastases. The British journal of surgery 80, 274–276 (1993).
Adam, R. et al. Five-year survival following hepatic resection after neoadjuvant therapy for nonresectable colorectal. Annals of surgical oncology 8, 347–353 (2001).
Curley, S. A. et al. Radiofrequency ablation of unresectable primary and metastatic hepatic malignancies: results in 123 patients. Annals of surgery 230, 1–8 (1999).
Scaife, C. L. & Curley, S. A. Complication, local recurrence, and survival rates after radiofrequency ablation for hepatic malignancies. Surgical oncology clinics of North America 12, 243–255 (2003).
Shaw, I. M., Rees, M., Welsh, F. K., Bygrave, S. & John, T. G. Repeat hepatic resection for recurrent colorectal liver metastases is associated with favourable long-term survival. The British journal of surgery 93, 457–464, doi: 10.1002/bjs.5323 (2006).
Davalos, R. V., Mir, I. L. & Rubinsky, B. Tissue ablation with irreversible electroporation. Annals of biomedical engineering 33, 223–231 (2005).
Llovet, J. M., Bru, C. & Bruix, J. Prognosis of hepatocellular carcinoma: the BCLC staging classification. Seminars in liver disease 19, 329–338, doi: 10.1055/s-2007-1007122 (1999).
van Amerongen, M. J. et al. Short term and long term results of patients with colorectal liver metastases undergoing surgery with or without radiofrequency ablation. European journal of surgical oncology: the journal of the European Society of Surgical Oncology and the British Association of Surgical Oncology, doi: 10.1016/j.ejso.2016.01.013 (2016).
Fonseca, A. Z., Saad, W. A. & Ribeiro, M. A. Jr. Complications after Radiofrequency Ablation of 233 Hepatic Tumors. Oncology 89, 332–336, doi: 10.1159/000439089 (2015).
Scudamore, C. H. et al. Radiofrequency ablation followed by resection of malignant liver tumors. American journal of surgery 177, 411–417 (1999).
Zheng, R. N. et al. Efficacy of percutaneous radiofrequency ablation for the treatment of hepatocellular carcinoma. Genetics and molecular research: GMR 14, 17982–17994, doi: 10.4238/2015.December.22.24 (2015).
Dupuy, D. E. & Goldberg, S. N. Image-guided radiofrequency tumor ablation: challenges and opportunities–part II. Journal of vascular and interventional radiology: JVIR 12, 1135–1148 (2001).
Farrell, M. A. et al. Paranephric water instillation: a technique to prevent bowel injury during percutaneous renal radiofrequency ablation. AJR. American journal of roentgenology 181, 1315–1317, doi: 10.2214/ajr.181.5.1811315 (2003).
Yamakado, K., Nakatsuka, A., Akeboshi, M. & Takeda, K. Percutaneous radiofrequency ablation of liver neoplasms adjacent to the gastrointestinal tract after balloon catheter interposition. Journal of vascular and interventional radiology: JVIR 14, 1183–1186 (2003).
Akahane, M. et al. Complications of percutaneous radiofrequency ablation for hepato-cellular carcinoma: imaging spectrum and management. Radiographics: a review publication of the Radiological Society of North America, Inc 25 Suppl 1, S57–68, doi: 10.1148/rg.25si055505 (2005).
Kang, T. W. et al. Percutaneous radiofrequency ablation for the hepatocellular carcinoma abutting the diaphragm: assessment of safety and therapeutic efficacy. Korean journal of radiology 10, 34–42, doi: 10.3348/kjr.2009.10.1.34 (2009).
Ng, K. K. et al. Analysis of recurrence pattern and its influence on survival outcome after radiofrequency ablation of hepatocellular carcinoma. Journal of gastrointestinal surgery: official journal of the Society for Surgery of the Alimentary Tract 12, 183–191, doi: 10.1007/s11605-007-0276-y (2008).
Bai, H., Huangz, X., Jing, L., Zeng, Q. & Han, L. The effect of radiofrequency ablation vs. liver resection on survival outcome of colorectal liver metastases (CRLM): a meta-analysis. Hepato-gastroenterology 62, 373–377 (2015).
Lam, V. W. et al. Incomplete ablation after radiofrequency ablation of hepatocellular carcinoma: analysis of risk factors and prognostic factors. Annals of surgical oncology 15, 782–790, doi: 10.1245/s10434-007-9733-9 (2008).
Edd, J. F. & Davalos, R. V. Mathematical modeling of irreversible electroporation for treatment planning. Technology in cancer research & treatment 6, 275–286 (2007).
Sale, A. J. & Hamilton, W. A. Effects of high electric fields on micro-organisms. 3. Lysis of erythrocytes and protoplasts. Biochimica et biophysica acta 163, 37–43 (1968).
Lam, V. W. et al. A systematic review of clinical response and survival outcomes of downsizing systemic chemotherapy and rescue liver surgery in patients with initially unresectable colorectal liver metastases. Annals of surgical oncology 19, 1292–1301, doi: 10.1245/s10434-011-2061-0 (2012).
de Gramont, A. et al. Leucovorin and fluorouracil with or without oxaliplatin as first-line treatment in advanced colorectal cancer. Journal of clinical oncology: official journal of the American Society of Clinical Oncology 18, 2938–2947 (2000).
Giacchetti, S. et al. Phase III multicenter randomized trial of oxaliplatin added to chronomodulated fluorouracil-leucovorin as first-line treatment of metastatic colorectal cancer. Journal of clinical oncology: official journal of the American Society of Clinical Oncology 18, 136–147 (2000).
van Iersel, L. B. et al. Management of isolated nonresectable liver metastases in colorectal cancer patients: a case-control study of isolated hepatic perfusion with melphalan versus systemic chemotherapy. Annals of oncology: official journal of the European Society for Medical Oncology/ESMO 21, 1662–1667, doi: 10.1093/annonc/mdp589 (2010).
Niessen, C. et al. Factors associated with short-term local recurrence of liver cancer after percutaneous ablation using irreversible electroporation: a prospective single-center study. Journal of vascular and interventional radiology: JVIR 26, 694–702, doi: 10.1016/j.jvir.2015.02.001 (2015).
Scheffer, H. J. et al. Irreversible electroporation for nonthermal tumor ablation in the clinical setting: a systematic review of safety and efficacy. Journal of vascular and interventional radiology: JVIR 25, 997–1011; quiz 1011, doi: 10.1016/j.jvir.2014.01.028 (2014).
Cannon, R., Ellis, S., Hayes, D., Narayanan, G. & Martin, R. C. 2nd. Safety and early efficacy of irreversible electroporation for hepatic tumors in proximity to vital structures. Journal of surgical oncology 107, 544–549, doi: 10.1002/jso.23280 (2013).
Thomson, K. R. et al. Investigation of the safety of irreversible electroporation in humans. Journal of vascular and interventional radiology: JVIR 22, 611–621, doi: 10.1016/j.jvir.2010.12.014 (2011).
Author information
Authors and Affiliations
Contributions
C.N. and P.W. wrote the main manuscript text, L.B. and B.P. prepared figures. S.T., L.B. and C.N. collected data. L.B., P.W., E.M.J., C.N. and J.K. performed IRE. S.L. and A.T. performed literature review. All authors reviewed the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing financial interests.
Rights and permissions
This work is licensed under a Creative Commons Attribution 4.0 International License. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in the credit line; if the material is not included under the Creative Commons license, users will need to obtain permission from the license holder to reproduce the material. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/
About this article
Cite this article
Niessen, C., Thumann, S., Beyer, L. et al. Percutaneous Irreversible Electroporation: Long-term survival analysis of 71 patients with inoperable malignant hepatic tumors. Sci Rep 7, 43687 (2017). https://doi.org/10.1038/srep43687
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/srep43687
This article is cited by
-
Emerging nanobiotechnology for precise theranostics of hepatocellular carcinoma
Journal of Nanobiotechnology (2022)
-
Combination of irreversible electroporation with sustained release of a synthetic membranolytic polymer for enhanced cancer cell killing
Scientific Reports (2021)
-
Efficacy and safety of irreversible electroporation for malignant liver tumors: a systematic review and meta-analysis
European Radiology (2021)
-
Electro-Thermal Therapy Algorithms and Active Internal Electrode Cooling Reduce Thermal Injury in High Frequency Pulsed Electric Field Cancer Therapies
Annals of Biomedical Engineering (2021)
-
Multidisciplinary management of liver metastases in patients with colorectal cancer: a consensus of SEOM, AEC, SEOR, SERVEI, and SEMNIM
Clinical and Translational Oncology (2020)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.