Abstract
Chronic intermittent hypoxia (IH) associated with obstructive sleep apnea (OSA) is a major risk factor for cardiovascular and metabolic diseases (insulin resistance: IR). Autophagy is involved in the pathophysiology of IR and high intensity training (HIT) has recently emerged as a potential therapy. We aimed to confirm IH-induced IR in a tissue-dependent way and to explore the preventive effect of HIT on IR-induced by IH. Thirty Swiss 129 male mice were randomly assigned to Normoxia (N), Intermittent Hypoxia (IH: 21–5% FiO2, 30 s cycle, 8 h/day) or IH associated with high intensity training (IH HIT). After 8 days of HIT (2*24 min, 50 to 90% of Maximal Aerobic Speed or MAS on a treadmill) mice underwent 14 days IH or N. We found that IH induced IR, characterized by a greater glycemia, an impaired insulin sensitivity and lower AKT phosphorylation in adipose tissue and liver. Nevertheless, MAS and AKT phosphorylation were greater in muscle after IH. IH associated with HIT induced better systemic insulin sensitivity and AKT phosphorylation in liver. Autophagy markers were not altered in both conditions. These findings suggest that HIT could represent a preventive strategy to limit IH-induced IR without change of basal autophagy.
Similar content being viewed by others
Introduction
Obstructive sleep apnea (OSA) syndrome is characterized by recurrent episodes of pharyngeal collapses occurring during sleep, leading to chronic intermittent hypoxia (IH). OSA is well established as a cardiovascular risk factor1. Insulin resistance (IR) and diabetes are two cardiovascular risk factors promoted by OSA1. Indeed, OSA is associated with an increased prevalence of type 2 diabetes and has been shown to be a risk factor for insulin resistance and incident diabetes2,3,4.
Clinical and experimental studies have shown the major role of chronic IH in the insulin resistance induced by OSA. Furthermore, IR induced by IH can occur independently of obesity1. Several factors in OSA/IH patients may lead to IR among which: sympathetic nervous system hyper-activity, decrease in insulin growth factor I (IGF-1), hyperlipidemia induced proinflammatory and oxidative stress pathways (NF-ĸB pathway, reactive oxygen species), ectopic fat and release of inflammatory cytokines1. Muscle is particularly important in the regulation of glucose metabolism since it can account for 80% of glucose disposal5. Intermittent hypoxia induced IR has been shown in the soleus muscle of mice independently of autonomic activity6. Mechanisms involved in this IR are not fully understood and deserve attention.
The first-line therapy for OSA is the application of continuous positive airway pressure (CPAP), which substantially decreases the number and severity of respiratory events in patients7. Its efficiency on IR is not clear8 however slight improvement of insulin resistance has been observed after 2 weeks of 8 h of nightly treatment, a compliance scarcely reached by patients9. Thus, a better understanding of the pathophysiological mechanisms involved in the deleterious effects of IH could help to provide new alternative or complementary treatment to CPAP in the management of OSA-associated metabolic impairment.
The role of autophagy in metabolic alterations and, in particular IR, has been well documented10. Autophagy consists of a cellular recycling program that controls the quality of cellular elements by turning over cytoplasmic components within lysosomes. It protects against cellular toxicity and death by recycling oxidized proteins and aged organelles. It is finely regulated by more than 30 autophagy related genes and involves several steps after induction: generation of the nucleation complex, autophagosome formation, and cargo recognition11. Nucleation complex requires the dissociation of Beclin1 from Bcl-2, which leads to the functional class III phosphatidylinositol 3-kinase (PI3K) complex facilitating the targeting of other autophagic molecules to the nucleation complex. Thereafter, recruitment of membranes to the nucleation complex promotes formation of the limiting membrane12 Finally, membrane elongation and autophagosome formation occurs following activation of Atg5-Atg12 and the microtubule-associated protein light chain 3 (LC3), which may be lipidated to membrane-associated phosphatidylethanolamine10. Sealing upon itself, the limiting membrane can sequester cargo within double-membraned autophagosomes. Then cargo can be hydrolyzed after fusion of autophagosomes with lysosomes.
Numerous signaling factors converge to the metabolic sensor mammalian target of rapamycin mTOR to fine-tune autophagy. Briefly when nutrients and growth factors are available, mTOR inhibits autophagy. By contrast, energy depletion reduces the inhibitory effects of mTOR on autophagy through an increase of AMPK activity. Moreover, autophagy can be inhibited by the insulin pathway PI3K-AKT-mTOR and mTOR activation is regulated by AKT13. On a cellular model, hypoxia itself, via the transcription factor HIF-1, directly activates autophagy through BNIP3 regulation (allowing dissociation of Beclin from Bcl-2)14.
Moreover, autophagy has been shown to be activated in situations of energy imbalance such as stress, starvation and exercise15. However, its regulation seems more complex and tissue dependent. Exercise training activates autophagy in muscle to overcome insulin resistance developed in the case of overnutrition16. Others factors can negatively influence autophagy among which insulin17, high fat feeding, lipid toxicity and the resulting IR, hepatic steatosis and inflammation10. Previous studies have shown that livers from dietary and genetic mouse models of obesity decreased autophagy, resulting in insulin resistance18. Conversely, obesity might be associated with increased autophagy in adipose tissue, leading to an increase in circulating lipids19.
The question whether the insulin resistance associated to OSA or IH is related to modulation of autophagy in a tissue dependent manner remains unanswered. To our knowledge, apart from a study showing the importance of autophagy to maintain cardiac contractility20, the effects of chronic IH on autophagy and its relationship with insulin resistance has never been studied. We hypothesized that chronic IH exposure would fail to activate autophagy, in a tissue dependent manner, due to the alteration of insulin sensitivity in OSA.
Beneficial effects of aerobic exercise on metabolic health and particularly insulin resistance are well established21. Intense exercise intensity (high intensity training: HIT) seems suitable and more efficient to get rapid benefits on metabolic health on whole body insulin sensitivity and some of its contributors such muscle microvascular density and eNOS protein22,23. In previous studies performed on rat24 and in mice (unpublished results), we assessed metabolic and functional variables to determine which protocol (moderate intensity aerobic endurance training or high-intensity aerobic endurance training (HIT)) of equal volume (i.e. total energy expenditure although different intensity) promoted more beneficial outcomes after short-term training. We selected the HIT used in the present study since only 10 sessions elicited the greater effects regarding training performance (i.e. maximal aerobic speed and endurance) and muscle adaptations (i.e. citrate synthase activity).
Thus, our second hypothesis was that HIT would reduce insulin resistance and improve autophagy status in a context of intermittent hypoxia.
If our hypotheses are verified, targeting IH induced IR by HIT could represent a new promising preventive strategy in OSA patients.
Results
Effect of intermittent hypoxia associated or not with high intensity exercise training on weight, food intake, hematocrit and exercise performance
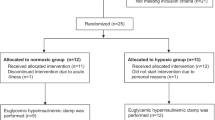
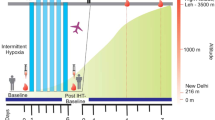
The experimental design is described in Fig. 1A. Intermittent hypoxia, independently of exercise training, decreased weight after 7 days of exposure (N: 43.4 ± 0.6 g; IH: 38.1 ± 0.7 g; IH HIT: 38.7 ± 0.6 g; p < 0.001). Thereafter the weight plateaued until the last day of exposure (Fig. 1B). This weight loss was paralleled by a decrease in food intake in both groups exposed to intermittent hypoxia (N: 5.2 ± 5.2; IH: 3.0 ± 0.1; IH HIT: 3.8 ± 0.1 g.day−1; p < 0.001; Fig. 1C). However, exercise training induced a greater food intake compared to the non-trained group, which prevented further weight loss in this group (Fig. 1C). Hematocrit did not differ between the 3 groups (Fig. 1D). Post IH exposition, maximal aerobic speed (MAS) was greater after hypoxia compared to normoxia whether associated or not to exercise training (Fig. 1E). Endurance at 75% of MAS followed the same tendency but did not reach statistical significance (p = 0,095; Fig. 1F).
(A) Experimental design of the study. After 7 days of habituation to the treadmill, animals started 18 days of High Intensity Training on a 0% incline. Intermittent Hypoxia began at day 8 of HIT for 14 days. 3 days before euthanasia, insulin tolerance test, maximal aerobic speed and endurance tests have been performed. Mice weight evolution (B) and food intake (C) over the exposure to IH and HIT. Running performance: (D) Maximal Aerobic Speed (MAS) and (E) endurance were measured. (F) Hematocrit levels were measured on mice capillaries collected at D17 during the Insulin Tolerance Test. Data are presented as mean ± SEM. *P < 0.05, ***P < 0.001 vs N, $$$P < 0.001 IH HIT vs IH. (n = 9–10 per group).
Impact of intermittent hypoxia on insulin sensitivity
Fasting glycemia was significantly higher after intermittent hypoxia compared to normoxia (N: 133.3 ± 6.5 mg.dL−1; IH: 164.7 ± 6.7 mg.dL−1; p < 0.01; Fig. 2A) whereas fasting insulinemia did not significantly differ (Fig. 2B). Glycemia measured during 90 minutes after insulin injection was less decreased after intermittent hypoxia compared to normoxia, indicating insulin resistance (F = 4.183; P = 0.044; Fig. 2C).
Impact of intermittent hypoxia on insulin and autophagy activation signaling pathways
In gastrocnemius, AKT phosphorylations on serine 308 (Fig. 3A; 1.6 ± 0.3 fold increase; p < 0.05) and on threonine 473 (Fig. 3A; 1.4 ± 0.1 fold control value; p < 0.05) were greater after intermittent hypoxia compared to normoxia whereas neither AMPK (Fig. 3A) nor mTOR phosphorylations differed between the 2 groups (Fig. 3A). Conversely in adipose tissue, AKT phosphorylations on serine 308 (Fig. 3B; p < 0.05) and on threonine 473 (Fig. 3B; p < 0.15) were lower after intermittent hypoxia although for the latter it did not reach statistical significance. In the liver, only AKT phosphorylation on serine 308 (Fig. 3C; 0.7 ± 0.1 fold control value; p < 0.05) was significantly lower compared to normoxia; AKT phosphorylation on threonine 473, AMPK and mTOR did not differ (Fig. 3C).
Quantification of phosphorylation of AKT (Thr308 and Ser473), mTOR (Ser2448) and AMPK (Th172) protein expression and representative immunoblot images in (A) gastrocnemius muscle, (B) adipose tissue and (C) liver. AMPK and mTOR were undetectable in adipose tissue. Comparisons were performed after normalization to the total form of the protein. Data are presented as mean ± SEM. *P < 0.05 vs N (n = 9–10 per group).
Impact of intermittent hypoxia on autophagy markers
In gastrocnemius, autophagy protein expressions such Bnip3, Beclin1, p62 and LC3B-II/LC3B-I did not differ between IH and N (Fig. 4A). Bnip3 (0.8 ± 0.1 fold control value; p < 0.01) and Bnip3L (0.8 ± 0.1 fold control value; p < 0.05) mRNA relative expressions were lower after IH compared to N whereas those of ATG5 or LC3B were similar (Fig. 4B). In adipose tissue, none of measured protein expression among which Bnip3, Beclin1, p62, LC3B differed between IH and N (Fig. 4C). The same applied in liver (Fig. 4D).
mRNA (A) and protein (B–D) analyses were performed on mice that underwent normoxia (N) or fourteen days of intermittent hypoxia (IH). Quantification of phosphorylation of Bnip3, Beclin1, p62, the ratio LC3-II/LC3-I protein expression and representative immunoblot images in (B) gastrocnemius muscle, (C) adipose tissue and (D) liver. Comparisons were performed after normalization to α-Tubulin or GAPDH. Data are presented as mean ± SEM. *P < 0.05 vs N(n = 9–10 per group).
Effects of high intensity training on intermittent hypoxia induced insulin resistance
High intensity training did not alter fasting glycemia or fasting insulinemia compared to intermittent hypoxia alone (Fig. 5A,B).
Glycemia measured for 90 minutes after the insulin injection decreased more after IH HIT compared to IH exposition alone, suggesting a decrease in insulin resistance (Fig. 5C; F = 3.94; P = 0.05).
Effects of high training intensity during intermittent hypoxia exposure on insulin and autophagy activation signaling pathways
In gastrocnemius, AKT phosphorylations on serine 308 and on Threonine 473, and on AMPK, were not altered after high intensity training compared to intermittent hypoxia alone (Fig. 6A). Conversely, mTOR phosphorylation was lower in IH HIT compared to HIT (Fig. 6A; 0.6 ± 0.1 fold control value, p < 0.05). In adipose tissue, AKT phosphorylations on serine 308 and on Threonine 473 did not differ between IH HIT and IH (Fig. 6B). In liver, AKT phosphorylations on serine 308 (p < 0.07) and on threonine 473 were greater in IH HIT but differences did not reach statistical significance (Fig. 6C). In addition, phosphorylations of AMPK and mTOR were similar between IH HIT and IH.
Quantification of phosphorylation of AKT (Thr308 and Ser473), mTOR (Ser2448) and AMPK (Th172) protein expression and representative immunoblot images in (A) gastrocnemius muscle, (B) adipose tissue and (C) liver. AMPK and mTOR were undetectable in adipose tissue. Comparisons were performed after normalization to total protein. Data are presented as mean ± SEM. *P < 0.05 vs IH (n = 9–10 per group).
Effects of high intensity training during intermittent hypoxia on autophagy markers
In gastrocnemius, Bnip3 and ATG5 mRNA relative expressions were lower after IH HIT compared to IH whereas those of Bnip3L, LC3B, HIF-1 were similar (Fig. 7A). Autophagy protein expressions such Beclin 1, p62 and LC3B-II/LC3B-I did not differ between IH and IH HIT (Fig. 7B). Bnip3 protein expression tended to be greater in IH HIT compared to IH but the difference did not reach statistical significance (1.5 ± 0.3 fold control value; p = 0.098; Fig. 7B). In adipose tissue, Beclin 1, p62, LC3B-II protein expressions did not differ between IH and IH HIT (Fig. 7C). However, there was a tendency for a lower expression of Bnip3 in IH HIT compared to IH (0.6 ± 0.1 fold control value; p = 0.09; Fig. 7C).
ARNm (A) and protein (B–D) analyses were performed on mice that underwent fourteen days of intermittent hypoxia (IH) alone or in association with 3 weeks of high intensity training (IH HIT). Quantification of Bnip3, Beclin1, p62, the ratio LC3-II/LC3-I protein expression and representative immunoblot images in (B) gastrocnemius muscle, (C) adipose tissue and (D) liver. Comparisons were performed after normalization to α-Tubulin or GAPDH. Data are presented as mean ± SEM. *P < 0.05 vs IH (n = 9–10 per group).
In liver, Beclin 1, p62, LC3B-II protein expressions did not differ between IH and IH HIT. However, Bnip3 was significantly lower in IH HIT compared to IH (0.7 ± 0.1 fold control value; p = 0.05; Fig. 7D).
Discussion
In the present study, we confirmed that intermittent hypoxia induces insulin resistance, characterized by greater fast glycemia, an impaired systemic insulin sensitivity and lower AKT phosphorylation in adipose tissue and liver in our model. When added to IH, HIT induced better systemic insulin sensitivity and a tendency to greater AKT phosphorylation in liver. Thus, our findings suggest that HIT might represent a potential preventive strategy to limit IH-induced IR in OSA patients.
Observational studies have demonstrated that OSA is an independent risk factor for prediabetes and incident diabetes8. Both animal and human models of intermittent hypoxia and sleep fragmentation acutely mimicking OSA show evidence of insulin resistance and glucose intolerance9. In our study, IH altered the glycemic status and induced insulin resistance. Indeed, fasting glycemia was greater in IH and was not compensated by a hyperinsulinemia. This hyperglycemia might be due to an IR or pancreatic dysfunction associated with insulin secretion perturbation25. Also, Shin et al. demonstrated that fasting hyperglycemia after four weeks of IH is due to an increase of the sympathetic nervous system, which triggers an increase of baseline hepatic glucose output and hepatic enzymes of the gluconeogenesis (PEPCK)26. The insulin tolerance test revealed impaired insulin sensitivity in IH compared to control mice, which confirmed a systemic insulin resistance. Thomas et al. have recently shown that hypoxia-inducible factor prolyl hydroxylase 1 (PHD1) deficiency promotes hepatic steatosis and liver-specific insulin resistance in mice27. In our study, IR seems also to be tissue dependent. The phosphorylation of protein kinase B (PKB, AKT) is the major signaling pathway modulating glucose metabolism in different tissues28. Our results showed that IH induced less phosphorylation of AKT in liver and adipose tissue than in normoxia, which confirms previous results29. As opposed to liver and adipose tissue, phosphorylation of AKT (Serine 473 and threonine 308) was greater in muscle after intermittent hypoxia but this could not counteract the systemic insulin resistance. These results contrast with Liyori et al.’s observations. These authors attributed the reduced insulin sensitivity to a decrease of glucose disposal and oxidation in the soleus muscle, without modification in the gastrocnemius6. In our study, we did not measure AKT phosphorylation in soleus, but gastrocnemius might have partly compensated the insulin resistance in adipose tissue and liver. Nevertheless, this was not sufficient to maintain an adequate glycemic control. Thus, IR induced by IH is systemic and tissue dependent. Of note, this IR occurred despite the greater weight loss largely described in continuous hypoxia conditions30, recurrently observed in our lab because of a decrease of food intake. In addition, maximal exercise performance was slightly increased after IH exposition as reported in human beings31. The latter could not be explained by a greater hematocrit because this variable was not altered in the present study. However, greater muscle vascularization is a possible explanation because of the well-known effects of IH on HIF1-α and VEGF, one of its targets genes32. Furthermore, we cannot exclude a greater maximal cardiac output. However this hypothesis is not consistent with the rather deleterious cardiac effects of IH24.
Recent findings highlight the involvement of autophagy in mobilization of diverse cellular energy stores. Thus, autophagy may play an important role in metabolic diseases development. Given the metabolic perturbations associated with OSA or IH, it was reasonable to expect an autophagy perturbation in IR development induced by IH. Few studies have explored autophagy involvement in intermittent hypoxia. Giordano et al. showed an activation of autophagy in the diaphragm muscle after 4 days of IH exposure33. These authors showed that the diaphragm underwent structural and metabolic changes after short-term IH (4 days exposure), with autophagy-associated atrophy whereas limb muscles were not altered. Moreover, Maeda et al. showed the necessity of autophagy integrity to avoid a decrement in myocardium contractile function20. In our study, we did not find any alteration in basal autophagy status in muscle, adipose tissue or liver. Autophagy is a dynamic process. A key point that needs to be specified is the difference between measurements that monitor the number or volume of autophagic elements at any stage of the autophagic process versus those that measure flux through the autophagy pathway (the complete process including the amount and rate of cargo sequestered and degraded)34. In our study, we did not observe any change in basal autophagy whereas we found a modification of AKT-PI3K signaling pathway involved in autophagy activation. He et al. generated mutant mice showing normal levels of basal autophagy but the latter could not be modulated by a stimulus (e.g. exercise)16. Other studies should investigate those autophagy dynamic aspects (the autophagy flux) in IH context.
In metabolic syndrome, the beneficial effects of high intensity training on insulin signaling have been shown in muscles and adipose tissue35. The second part of our study showed that exercise could improve IH-induced insulin resistance, which is consistent with previously published studies. Indeed, when added to IH, exercise improved systemic insulin sensitivity without changing fasting glycemia or insulinemia. Moreover, HIT tended to improve hepatic phosphorylation of AKT, thus increasing insulin signaling in liver without modification in others tissues. In young obese, exercise improved hepatic insulin sensitivity36. Heled et al. reported that aerobic exercise training (treadmill) increased hepatic insulin sensitivity due to a greater insulin signaling response and an inhibition of PEPCK activity, a key enzyme of gluconeogenesis, in the hepatocytes of diabetes prone rats37. Whether in rodents or humans, exercise improves liver insulin resistance. Moreover, since IH can disturb glucose homeostasis via sympathetic hyperactivity29,38, we cannot exclude the well-known decrease in sympathetic activity induced by exercise training in the improvement of IR24.
In order to find other mechanisms concerning the improvement of insulin sensitivity, we measured the impact of High Intensity Training on autophagy modulation. Indeed, it has been shown that autophagy can mediate chronic exercise-induced metabolic benefits. Furthermore, animal models in which autophagy is perturbed do not adapt to exercise to the same extent. He et al. reported that autophagy induction may contribute to the beneficial metabolic effects of exercise16. They generated mutant mice (BCL2 phosphorylation mutation) presenting decrease of endurance to exercise and altered glucose metabolism during acute exercise, as well as impaired chronic exercise-mediated protection against high-fat-diet-induced glucose intolerance. These mice showed normal levels of basal autophagy but were deficient in exercise-induced autophagy. In this study, we did not observe a modulation of basal autophagy-related protein as known as the ratio LC3-II/LC3-I and p62 as well as autophagy induction markers. After HIT added to IH, we measured basal autophagy, and more investigation is needed to confirm that stimulus-induced autophagy is not attenuated.
Nevertheless, we observed a decrease of Bnip3 (Bcl-2/adenovirus E1B 19-kDa-interacting protein 3) protein expression in liver and Bnip3 mRNA in muscle after HIT in intermittent hypoxia.
Although Bnip3 is known to be activated through HIF1 and to contribute to mitochondrial autophagy in hypoxia14, Bnip3 is also a mitochondrial BH3-only protein that contributes to cell death through activation of the mitochondrial pathway of apoptosis39. The decrease of bnip3 could contribute to a decrease of apoptosis in liver, leading to an improvement of the mitochondrial function. Also, Rikka et al.40 have shown that Bnip3-mediated impairment of mitochondrial respiration induces mitochondrial turnover by activating mitochondrial autophagy40. Thus, given the dual role of Bnip3, the decrease of Bnip3 protein expression could be an adaptive response40 to reduce apoptosis in liver without modification of autophagy. In diabetes, hepatic insulin resistance is associated with mitochondria alterations and ER stress activation41. These two parameters could be interesting to explore to identify mechanisms involved in intermittent hypoxia induced insulin resistance.
In conclusion, our study confirmed the deleterious effects of IH on metabolism and notably insulin resistance without basal autophagy modulation. Moreover, high intensity training improves IH-induced insulin resistance without involvement of basal autophagy. These findings suggest that HIT could represent a preventive strategy to limit IH-induced IR in OSA.
Methods
Animals
This investigation conforms to the Guide for the Care and Use of Laboratory Animals published by the US National Institutes of Health (NIH Publication no. 85-23, revised 1996).
We used 30 adult males Swiss 129 mice, of 8 weeks old (20–25 g) obtained from Janvier labs (Le Genest-Saint-Isle, France). The study was approved by the University Grenoble Alpes Animal Research Ethic Committee (ComEth) (authorization number: 184_UHTA_U1042_CA_03). The mice were housed (n = 6 or 9 per cage) at the animal care facility of the HP2 laboratory (approval: A38 516 10006), under a 12-hour light-dark cycle with 20–22 °C and allowed free access to standard food and water.
Experimental design
Mice were first randomly divided into three conditions (n = 10 mice per group): normoxia (N), hypoxia (IH) and hypoxia with high intensity training (IH HIT).
All mice were first accustomed to the treadmill running and aerobic performance tests were evaluated before starting 18 days of high intensity training for the IH HIT group. After 8 days of HIT protocol, all mice were exposed to either normoxia (N) or intermittent hypoxia (IH) for 13 additional days. In each group (N, IH, IH HIT), insulin tolerance test and aerobic performance tests were evaluated before the sacrifice (Fig. 1A).
Aerobic performance tests and training protocol
Tests and training were achieved on a motorized treadmill (0% grade; Bioseb, Vitrolles, France). Mice were first accustomed to the treadmill running for 4 days before the training and hypoxic protocol (30 min per session). Then, aerobic performance tests were performed before and after hypoxia and training protocol.
Aerobic performance tests
MAS (Maximal Aerobic Speed) consisted of a maximal progressive continuous exercise on the motorized treadmill (0% grade). After a 6 min warm-up at 10 cm/s the intensity was increased by 2 cm/s every 3 min until the mice could no longer keep the pace. MAS is the speed corresponding to the last entire stage completed by the animal.
Endurance at 75% MAS
Aerobic endurance is defined in this experiment as the running time to exhaustion at 75% of MAS. After a 6 minutes warm-up at 10 cm/min, the speed was increased to reach an intensity of 75% MAS. Exercise was stopped when mice were unable to run.
High-intensity aerobic training protocol
HIT consists in 2 bouts of 24 min exercise, interspaced by 30 min recovery. The treadmill speed was set at 10 cm/s for the first step and corresponds to 6 min warm-up (50% of MAS), followed by six steps of 3 min progressive intensity to reach respectively 65, 70, 75, 80, 85 and 90% of MAS.
Intermittent hypoxia protocol
Animals were exposed daily to 8 hours of intermittent hypoxia (IH) or normoxia (N) during their daytime sleep period, for 16 days. The IH stimulus was performed using a specifically designed device, as previously described (2). It consisted in 1-min cycles alternating 30 s of hypoxia (5% inspired oxygen fraction (FiO2) and 30 s of normoxia (21% FiO2). FiO2 was monitored throughout the experiment with a gas analyzer (ML206, ADInstruments, Oxford, United Kingdom). Normoxic mice were exposed to air streams to reproduce equivalent levels of noise and turbulences related to gas circulation than IH, without hypoxia.
Insulin tolerance test (ITT)
At the 17th day of the protocol (9 days oh IH), we used the ITT to assess global insulin sensitivity. Mice were fasted for 5 h then weighed before blood was collected from the tail tip for glycemia, insulin rate and hematocrit measurement (T0). Intraperitoneal injection of insulin (0.5 UI.kg−1 body weight; Novorapid, Novo Nordisk A/S, Bagsvaerd, Danemark) was made and followed by further blood glucose measurement at 15, 30, 45, 60 and 90 min after the injection.
Glycemia
Blood glucose was measured before insulin injection (T0) by blood sampling (≈5 μL) using the glucometer OneTouch® Ultra® (LifeScan France, Issy-Les-Moulineaux, France).
Plasma Insulin
Blood samples were collected before the ITT (T0) in heparinized capillaries (≈50 μL). Capillaries (Brand, Finland) were then centrifuged (13000 rpm, 7 min, 21 °C) in order to separate the plasma and the formed elements of blood allowing to measure hematocrit. Plasmas were then collected for blood insulin rate measures. Blood insulin level of each mouse was subsequently measured using a Mouse Insulin ELISA Kit 96-well plate (EMD Millipore, St Charles, Missouri, USA).
Hematocrit measurement
Hematocrit was assessed as a ratio of blood cells on the total blood volume.
Tissue sampling
At the end of the exposure, intraperitoneal injection of insulin (0.5 UI.kg−1 body weight; Novorapid, Novo Nordisk A/S, Bagsvaerd, Danemark) was made 10 min before mice were euthanized by cervical dislocation. Liver, epididymal adipose tissue, gastrocnemius, soleus and plantaris muscles were immediately removed and frozen in liquid nitrogen for further analysis (western blot and qPCR analysis).
Western-blot analysis
Frozen livers, adipose tissues and gastrocnemius muscles were homogenized (Precellys 24, 6500 rpm, 3 × 20 s–5 s; Bertin Technology, Montigny le Bretonneux, France) in order to extract total proteins (Sample lysis buffer: 5 mM EDTA, 1 mM Na3VO4, 20 mM NaF, 1 mM DTT, proteases inhibitor cocktail). Protein concentration was calculated using a BCA assay (Pierce® BCA Protein, Thermo Scientific, Rockford, USA). Depending on proteins analyzed, 30 to 40 μg of protein were separated by SDS polyacrylamide gels (8–15%) and transferred to polyvinylidene difluoride (PVDF) membranes. Next, membranes were blocked with 5% non-fat milk or bovine serum albumin (BSA) in Tris-buffered saline (TBS) with Tween 20 (0.1%). Then, membranes were incubated overnight at 4 °C with primary antibodies in TBS-Tween 20–5% BSA or non-fat milk (Supplementary Table S1). The following day, membranes were incubated for 1 h at room temperature with horseradish peroxidase-conjugated appropriate anti-IgG (1/5000, Santa Cruz Biotechnology, Heidelberg, Germany). Enhanced chemiluminescence was performed with the Western-Blot ECL substrate (Clarity, Bio-Rad, Marnes-la Coquette, France) according to the manufacturer’s instructions and video acquisition (chemidoc-xrs-system, Bio-Rad, Marnes-la Coquette, France). The relative amount of protein was quantified by densitometry (Image Lab, Bio-Rad, Marnes-la Coquette, France) and expressed as the ratio of loading control. Phospho-proteins were expressed relative to total proteins and not phospho-proteins were expressed relative to GAPDH or tubulin. Finally, protein expressions of different groups were expressed relative to the control groups (N for the evaluation of IH effects or IH when evaluating the effects of IH HIT) normalized at 1.
Quantitative real-time RT-PCR analysis
Total RNA was collected from gastrocnemius muscle using the Total RNA isolation kit (Tri-reagent, Ambion, Austin, TX) followed by purification using the RNeasy Fibrous Tissue Mini Kit (Qiagen). Complementary DNA was generated from 200 ng of RNA using the Eurogentec Core Kit and the C-1000 Thermal Cycler (Bio-Rad). The selected forward and reverse primer sequences are listed in Supplementary Table S2. Real-time quantitative polymerase chain reaction (qPCR) was performed in a 20-μL final volume and optimized concentrations for each primer using the SYBR Master Mix dTTP Blue (Eurogentec). Fluorescence intensity was recorded using a CFX96 Real-Time PCR Detection System (Bio-Rad). Data were analyzed using the ΔΔCt method of analysis42. Reference genes (GAPDH, B-Actin and α-tubulin) were used to normalize the expression levels of genes of interest.
Statistical analysis
Statistics were performed using GraphPad Prism 6 Software (San Diego, California, USA). Data are expressed as mean ± SEM. T-test or unparametric test (Mann & Whitney) were used for two-groups comparisons. For ITT, differences between groups over time were determined by two-way ANOVA, with repetition on the last factor. A p value < 0.05 was considered statistically significant.
Additional Information
How to cite this article: Pauly, M. et al. High intensity aerobic exercise training improves chronic intermittent hypoxia-induced insulin resistance without basal autophagy modulation. Sci. Rep. 7, 43663; doi: 10.1038/srep43663 (2017).
Publisher's note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
Dempsey, J. A., Veasey, S. C., Morgan, B. J. & O’Donnell, C. P. Pathophysiology of sleep apnea. Physiol. Rev. 90, 47–112 (2010).
Kendzerska, T., Gershon, A. S., Hawker, G., Tomlinson, G. & Leung, R. S. Obstructive sleep apnea and incident diabetes. A historical cohort study. Am. J. Respir. Crit. Care Med. 190, 218–225 (2014).
Seicean, S. et al. Sleep-disordered breathing and impaired glucose metabolism in normal-weight and overweight/obese individuals: the Sleep Heart Health Study. Diabetes Care 31, 1001–1006 (2008).
Marshall, N. S. et al. Is sleep apnea an independent risk factor for prevalent and incident diabetes in the Busselton Health Study? J. Clin. Sleep Med. JCSM Off. Publ. Am. Acad. Sleep Med. 5, 15–20 (2009).
Baron, A. D., Brechtel, G., Wallace, P. & Edelman, S. V. Rates and tissue sites of non-insulin- and insulin-mediated glucose uptake in humans. Am. J. Physiol. 255, E769–774 (1988).
Iiyori, N. et al. Intermittent hypoxia causes insulin resistance in lean mice independent of autonomic activity. Am. J. Respir. Crit. Care Med. 175, 851–857 (2007).
Baguet, J.-P., Barone-Rochette, G., Tamisier, R., Levy, P. & Pépin, J.-L. Mechanisms of cardiac dysfunction in obstructive sleep apnea. Nat. Rev. Cardiol. 9, 679–688 (2012).
Pamidi, S. & Tasali, E. Obstructive sleep apnea and type 2 diabetes: is there a link? Front. Neurol. 3, 126 (2012).
Pamidi, S. et al. Eight Hours of Nightly Continuous Positive Airway Pressure Treatment of Obstructive Sleep Apnea Improves Glucose Metabolism in Patients with Prediabetes. A Randomized Controlled Trial. Am. J. Respir. Crit. Care Med. 192, 96–105 (2015).
Yamada, E. & Singh, R. Mapping autophagy on to your metabolic radar. Diabetes 61, 272–280 (2012).
He, C. & Klionsky, D. J. Regulation Mechanisms and Signaling Pathways of Autophagy. Annu. Rev. Genet. 43, 67–93 (2009).
Chang, C.-Y. & Huang, W.-P. Atg19 Mediates a Dual Interaction Cargo Sorting Mechanism in Selective Autophagy. Mol. Biol. Cell 18, 919–929 (2007).
Alessi, D. R. et al. Mechanism of activation of protein kinase B by insulin and IGF-1. EMBO J. 15, 6541–6551 (1996).
Zhang, H. et al. Mitochondrial autophagy is an HIF-1-dependent adaptive metabolic response to hypoxia. J. Biol. Chem. 283, 10892–10903 (2008).
Vainshtein, A. & Hood, D. A. The regulation of autophagy during exercise in skeletal muscle. J. Appl. Physiol. 664–673 (2016).
He, C. et al. Exercise-induced BCL2-regulated autophagy is required for muscle glucose homeostasis. Nature 481, 511–515 (2012).
Fritzen, A. M. et al. Regulation of autophagy in human skeletal muscle: effects of exercise, exercise training and insulin stimulation. J. Physiol. 594, 745–761 (2016).
Yang, L., Li, P., Fu, S., Calay, E. S. & Hotamisligil, G. S. Defective hepatic autophagy in obesity promotes ER stress and causes insulin resistance. Cell Metab. 11, 467–478 (2010).
Singh, R. et al. Autophagy regulates adipose mass and differentiation in mice. J. Clin. Invest. 119, 3329–3339 (2009).
Maeda, H. et al. Intermittent-hypoxia induced autophagy attenuates contractile dysfunction and myocardial injury in rat heart. Biochim. Biophys. Acta 1832, 1159–1166 (2013).
O’Hagan, C., De Vito, G. & Boreham, C. A. G. Exercise prescription in the treatment of type 2 diabetes mellitus: current practices, existing guidelines and future directions. Sports Med. Auckl. NZ 43, 39–49 (2013).
Cocks, M. & Wagenmakers, A. J. M. The effect of different training modes on skeletal muscle microvascular density and endothelial enzymes controlling NO availability. J. Physiol. 594, 2245–2257 (2016).
Jelleyman, C. et al. The effects of high-intensity interval training on glucose regulation and insulin resistance: a meta-analysis. Obes. Rev. Off. J. Int. Assoc. Study Obes. 16, 942–961 (2015).
Bourdier, G. et al. High-intensity training reduces intermittent hypoxia-induced ER stress and myocardial infarct size. Am. J. Physiol. Heart Circ. Physiol. 310, H279–289 (2016).
Drager, L. F., Jun, J. C. & Polotsky, V. Y. Metabolic consequences of intermittent hypoxia: relevance to obstructive sleep apnea. Best Pract. Res. Clin. Endocrinol. Metab. 24, 843–851 (2010).
Shin, M.-K. et al. Carotid body denervation prevents fasting hyperglycemia during chronic intermittent hypoxia. J. Appl. Physiol. 117, 765–776 (2014).
Thomas, A. et al. Hypoxia-inducible factor prolyl hydroxylase 1 (PHD1) deficiency promotes hepatic steatosis and liver-specific insulin resistance in mice. Sci. Rep. 6, 24618 (2016).
Garofalo, R. S. et al. Severe diabetes, age-dependent loss of adipose tissue, and mild growth deficiency in mice lacking Akt2/PKB beta. J. Clin. Invest. 112, 197–208 (2003).
Gileles-Hillel, A., Kheirandish-Gozal, L. & Gozal, D. Biological plausibility linking sleep apnoea and metabolic dysfunction. Nat. Rev. Endocrinol. 12, 290–298 (2016).
de Theije, C. C., Langen, R. C. J., Lamers, W. H., Schols, A. M. W. J. & Köhler, S. E. Distinct responses of protein turnover regulatory pathways in hypoxia- and semistarvation-induced muscle atrophy. Am. J. Physiol. Lung Cell. Mol. Physiol. 305, L82–91 (2013).
Burtscher, M. et al. Intermittent hypoxia increases exercise tolerance in elderly men with and without coronary artery disease. Int. J. Cardiol. 96, 247–254 (2004).
Semenza, G. L. Regulation of oxygen homeostasis by hypoxia-inducible factor 1. 97–106 (2009).
Giordano, C., Lemaire, C., Li, T., Kimoff, R. J. & Petrof, B. J. Autophagy-associated atrophy and metabolic remodeling of the mouse diaphragm after short-term intermittent hypoxia. PloS One 10, e0131068 (2015).
Klionsky, D. J. et al. Guidelines for the use and interpretation of assays for monitoring autophagy (3rd edition). Autophagy 12, 1–222 (2016).
Tjønna, A. E. et al. Aerobic interval training versus continuous moderate exercise as a treatment for the metabolic syndrome: a pilot study. Circulation 118, 346–354 (2008).
Van Der Heijden, G.-J. et al. Strength exercise improves muscle mass and hepatic insulin sensitivity in obese youth. Med. Sci. Sports Exerc. 42, 1973–1980 (2010).
Heled, Y. et al. Physical exercise enhances hepatic insulin signaling and inhibits phosphoenolpyruvate carboxykinase activity in diabetes-prone Psammomys obesus. Metabolism. 53, 836–841 (2004).
Fletcher, E. C. Invited Review: Physiological consequences of intermittent hypoxia: systemic blood pressure. J. Appl. Physiol. 90, 1600–1605 (2001).
Gustafsson, Å. B. Bnip3 as a Dual Regulator of Mitochondrial Turnover and Cell Death in the Myocardium. Pediatr. Cardiol. 32, 267–274 (2011).
Rikka, S. et al. Bnip3 impairs mitochondrial bioenergetics and stimulates mitochondrial turnover. Cell Death Differ. 18, 721–731 (2011).
Rieusset, J. Contribution of mitochondria and endoplasmic reticulum dysfunction in insulin resistance: Distinct or interrelated roles? Diabetes Metab. 41, 358–368 (2015).
Pfaffl, M. W. A new mathematical model for relative quantification in real-time RT-PCR. Nucleic Acids Res. 29, e45 (2001).
Acknowledgements
This work was supported by Structure Fédérative de Recherche Sport Exercice Motricité, UFRAPS, Université Grenoble Alpes. We thank Monique Mendelson for critical reading and helpful comments on the manuscript.
Author information
Authors and Affiliations
Contributions
A.A., A.R., J.C., P.F. and M.P. performed experiments. A.A., M.P. and P.F. analyzed data and drafted the manuscript; A.T., H.D., D.F., H.B. contributed to discussion and critically reviewed the manuscript; M.P. and P.F. contributed to discussion, supervised the project, conceptualized the project, performed experiments, analyzed data, wrote and edited the manuscript. P.F. is the guarantor of this work and, as such, has full access to all the data generated in the framework of the study and takes responsibility for their integrity and the accuracy of their analysis.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing financial interests.
Rights and permissions
This work is licensed under a Creative Commons Attribution 4.0 International License. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in the credit line; if the material is not included under the Creative Commons license, users will need to obtain permission from the license holder to reproduce the material. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/
About this article
Cite this article
Pauly, M., Assense, A., Rondon, A. et al. High intensity aerobic exercise training improves chronic intermittent hypoxia-induced insulin resistance without basal autophagy modulation. Sci Rep 7, 43663 (2017). https://doi.org/10.1038/srep43663
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/srep43663
This article is cited by
-
The importance of autophagy regulation in obstructive sleep apnea
Sleep and Breathing (2021)
-
Intermittent hypoxia-induced insulin resistance is associated with alterations in white fat distribution
Scientific Reports (2017)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.