Abstract
The objective of this study was to determine whether Lactobacillus rhamnosus GG culture supernatant (LCS) has a preventive effect against gut-derived systemic neonatal Escherichia coli (E. coli) K1 infection. The preventive effects were evaluated in human colonic carcinoma cell line Caco-2 and neonatal rat models. Our in vitro results showed that LCS could block adhesion, invasion and translocation of E. coli K1 to Caco-2 monolayer via up-regulating mucin production and maintaining intestinal integrity. In vivo experiments revealed that pre-treatment with LCS significantly decrease susceptibility of neonatal rats to oral E. coli K1 infection as reflected by reduced bacterial intestinal colonization, translocation, dissemination and systemic infections. Further, we found that LCS treated neonatal rats have higher intestinal expressions of Ki67, MUC2, ZO-1, IgA, mucin and lower barrier permeability than those in untreated rats. These results indicated that LCS could enhance neonatal resistance to systemic E. coli K1 infection via promoting maturation of neonatal intestinal defense. In conclusions, our findings suggested that LCS has a prophylactic effect against systemic E. coli K1 infection in neonates. Future studies aimed at identifying the specific active ingredients in LCS will be helpful in developing effective pharmacological strategies for preventing neonatal E. coli K1 infection.
Similar content being viewed by others
Introduction
In spite of great progress in anti-microbial therapy and supportive care, sepsis and meningitis remain a major cause of high mortality and severe neurological morbidity in neonates, especially in the preterm and very-low-birth-weight infants1,2,3. Escherichia coli (E. coli) K1 is the most predominant gram-negative bacteria that cause neonatal sepsis and meningitis4. The incidence of E. coli infections may further increase because of the recent emergence of antibiotic resistant E. coli strains. Furthermore, both clinical and experimental data suggest that the therapeutic efficacy of antimicrobial treatment alone is always limited for gram-negative bacillary meningitis5. A previous report demonstrated that prolonged neonatal administration of antibiotics is associated with increased risk of sepsis6. Therefore, it is necessary to develop alternate treatment strategies for preventing neonatal sepsis and meningitis.
Understanding and delineating the mechanism and the course of neonatal E. coli K1 sepsis and meningitis could provide a foundation for developing novel prophylactics. Although the exact mechanisms of E. coli K1–induced pathogenicity remain unclear, the natural course of E. coli K1 infection involving a series of steps as following have been established in detail: (a) gastrointestinal colonization by E. coli K1, often vertical transmission from the mother’s birth canal during delivery7,8; (b) E. coli K1 crosses the intestinal mucosal barrier and escape into the blood stream, then survive and multiply in the blood resulting in bacteraemia9; (c) finally, the bacteria transmigrate across the blood-brain barrier (BBB) and invade the central nervous system resulting in inflammatory responses and pathophysiological alterations such as pleocytosis and BBB injury that ultimately leads to neurological complications or death10. These steps indicate that the blockage of bacterial adherence to enterocyte and translocation across the intestinal barrier into the bloodstream would be a potential approach to prevent neonatal E. coli K1 sepsis and meningitis. Accumulating evidence shows that, probiotics exhibit protective effects on the intestinal mucosal barrier function, and are considered as an attractive option for preventing and/or treating E. coli K1 sepsis and meningitis. Further to this observation, our recent studies suggested that probiotics have a great potential to become a novel prophylactic for preventing neonatal bacteremia and meningitis11.
Probiotics are live bacteria which confer a beneficial effect on the host if administered in adequate amounts12. There is growing evidence that probiotics showed protective effect against a variety of disorders, such as obesity13, allergic asthma14, necrotizing enterocolitis15, diarrhea16, infection17,18 and cardiovascular diseases19. To date, many beneficiary effects of administering probiotics in gut associated diseases have been characterized, which includes maintenance of intestinal homeostasis, competitive exclusion of pathogens, promotion of mucin production, enhancement of intestinal barrier function, anti-inflammatory effects and immunomodulatory functions20,21. However, concern about the safety of live probiotics should be addressed, because of many up coming reports on increasing evidence of probiotic-associated infection in preterm infants and immunocompromised patients22,23,24. A randomised, double-blind, placebo-controlled trial demonstrated that in patients with predicted severe acute pancreatitis, probiotic prophylaxis with a multispecies probiotic preparation did not reduce the risk of infectious complications and was associated with an increased risk of mortality25. Furthermore, studies have revealed that E. coli Nissle 1917, a well known probiotic, exerts protective effect against mucosal disorders with considerable potential to induce gene mutations in vitro and cause DNA damage in vivo26,27. These adverse effects are associated with the development of colorectal carcinoma27. Additionally, a more serious problem was indicated by Million M et al., who noticed that there are publication biases in probiotics related papers, because lots of smaller or deleterious results were not published, even when authors are directly sponsored by food industry28. Thus, it is mandatory to develop a safer alternative to the live probiotics for clinical applications.
More recently, probiotic-derived soluble factors (defined as “postbiotics”29) have been suggested to have beneficial properties as same as their original “parent”-live probiotics. Some active components have been identified from postbiotics, including short chain fatty acids, polyamines, polyphosphate, proteins and peptides. These active components have been implicated to exhibit a beneficial effect against several intestinal disorders through competition with pathogens, maintenance of intestinal barrier integrity and promoting immune function30,31,32,33. Administering postbiotics not only can avoid the potential risks associated with live microorganisms but also confers the same beneficial effects on the host. Thus, developing postbiotics as innovative health-promoting agents and their successful implementation in clinical medicine could revolutionize the modern drug therapeutics.
Based on the rationale mentioned above, we speculated that Lactobacillus rhamnosus GG culture supernatant (LCS) could have a protective effect against gut-derived E. coli K1–induced neonatal bacteremia and meningitis. To verify this speculation, human colonic carcinoma cell line Caco-2 and neonatal rats were pre-incubated with and without LCS and then exposed to E. coli K1. We found that pre-treatment with LCS could inhibit adhesion, invasion and translocation of E. coli K1 to Caco-2 monolayer as well as alleviate bacterial intestinal colonization, translocation, dissemination and systemic infection in neonatal rats. Furthermore, we observed that pre-incubation with LCS could promote the maturation of neonatal intestinal defense and thereby, enhance the resistance of neonatal rats to oral E. coli K1 infection. Overall, our data indicate that LCS has a potential to become an effective prophylaxis for neonatal sepsis and meningitis.
Results
Pre-treatment with LCS inhibited the adhesion and invasion of E. coli K1 to Caco-2
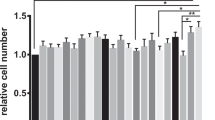
Because adherence and invasion to intestinal epithelium are the pivotal steps for intestinal bacterial translocation and to enter the circulation resulting in a systemic infection, we firstly determined whether LCS has the inhibitory effect on adhesion and invasion of E. coli K1. Caco-2 monolayers were pre-incubated with different concentrations of LCS for 3 hours (h) before the bacterial infection. Monolayers treated with cell culture medium or MRS (LGG culture medium, not used, 2% in the cell culture medium without antibiotics) alone served as controls. Numbers of cell-associated bacteria and intracellular bacteria were determined. The data reveal that pre-incubation with LCS could dose- and time-dependently inhibits adhesion and invasion of E. coli K1 (Fig. 1A–D). Interestingly, we could not find any obvious inhibitory effects on adhesion and invasion of E. coli K1 on adding LCS 1 h after E. coli K1 infection (Data not shown). To examine whether LCS has antibacterial activity, we assessed the influence of LCS on the growth of bacteria cultured in vitro with brain heart infusion (BHI) broth. As shown in Fig. 1E, the growth curves of bacteria grown in BHI with or without LCS were similar. This result demonstrates that LCS has no lethal effect on in vitro growth of E. coli K1. Furthermore, the trypan blue stain assay showed that LCS has no detectable cytotoxicity on Caco-2 (data not shown). Overall, these data suggested that LCS can effectively inhibit adhesion and invasion of E. coli K1 but has no impact on in vitro growth of E. coli K1.
Caco-2 monolayers were incubated with cell culture medium, MRS or different concentrations of LCS for 3 h, or with 1% LCS for different time duration before infection. MRS (LGG’s medium) and cell culture medium were used as controls. Then E. coli K1 (MOI = 100) was added and incubated for 3 h. The numbers of associated bacteria (A,B) and intracellular bacteria (C,D) were determined. The results were expressed as a percentage of the control. Error bars indicate standard deviations. (E) Effect of LCS on the growth of E. coli K1 in BHI broth at different concentrations of LCS. Bacterial growth was monitored by measuring the absorbance of liquid cultures at 600 nm. *P < 0.05, **P < 0.01, ***P < 0.001.
Mucin is required for LCS-mediated inhibitory effect on adhesion and invasion of E. coli K1
Direct killing and competing adhesion sites with pathogen are two major mechanisms by which viable LGG inhibit bacterial adhesion and invasion. Thus, it is puzzling that how LCS exhibit an inhibitory effect on adhesion and invasion of E. coli K1 (Fig. 1A–D), without any steric-hindrance or direct killing effect on E. coli K1 (Fig. 1E). Mucin layer is an important barrier that separates the pathogen from enterocyte. We thus speculated that, mucin layer may play a pivotal role in LCS-mediated inhibitory effect on adhesion and invasion of E. coli K1. To test this hypothesis, we firstly evaluated the influence of LCS or E. coli K1 on production of mucin in Caco-2 monolayer using Periodic Acid Schiff (PAS) assay as described in Methods. As shown in Fig. 2A, infection with E. coli K1 markedly reduced the expression of mucin from multiplicity of infection (MOI) of 50 to 200 compared with the control. In contrast, LCS could significantly elevate mucin production in a concentration-dependent manner. We next examined whether LCS has any protective role against mucin-depletion effect of E. coli K1. Result shown in Fig. 2B suggested that pre-treatment with LCS could significantly alleviate E. coli-induced loss of mucin. Similar results were also observed with morphological alterations of mucin layers. As shown in Fig. 2C, untreated Caco-2 monolayer was covered with a purple, homogeneous and continuous mucin layer. After exposure to E. coli K1, however, the mucin layer became thinner and disrupted. In contrast, pre-incubation with LCS for 3 h could prevent from E. coli K1-induced disruption of the mucin layer. Furthermore, we evaluated the expression levels of MUC2 in each group using western blot analysis. As shown in Fig. 2D, pre-incubation with LCS alleviated E. coli K1-induced depletion of MUC2.
Caco-2 cells were treated with various concentrations of E. coli K1 or LCS for 3 h, or pre-incubated with cell culture medium, MRS, or LCS for 3 h followed by E. coli K1 challenge. (A,B) The contents of mucin in cell lysates were determined by PAS assay as described in Methods. The results are expressed as relative content, taking the value for the control as 1. (C) Morphological alterations of mucin layers were determined by PAS staining. (D) Cells were treated as shown above for western blotting using an anti-MUC2 antibody. (E,F) Cells were pre-treated with various concentrations of LCS for 3 h and followed by E. coli K1 infection, cell-associated bacteria and mucus trapped bacteria were separated and counted as described in Methods. Data are expressed as the percentage of trapped E. coli K1 or adhered E. coli K1 among the added bacteria. *P < 0.05, **P < 0.01, ***P < 0.001.
N-acetylcysteine (NAC) is an agent which could remove the mucin layer from intestinal mucosa34. Hence, we used NAC to explore whether the mucin layer is required for LCS-mediated inhibitory effect. Caco-2 monolayers were infected as described in the adhesion assay and then the bacteria that were trapped in mucin and adhering to Caco-2 monolayers were separated using NAC and counted as described in Methods. As shown in Fig. 2E and F, untreated Caco-2 mucin layer (CON) only trapped about 1.5 ± 0.9% E. coli K1, led to about 5.3 ± 1.0% E. coli K1 adhered to monolayer. However, when pre-treated with 2% LCS for 3 h before the E. coli K1 challenge, the mucin layer trapped about 7.2 ± 1.4% E. coli K1 and only 1.6 ± 0.56% E. coli K1 were detected on Caco-2 cell surface. These data indicated that LCS could induce mucin production to trap E. coli K1 and block bacteria from getting access to the intestinal epithelia.
Pre-treatment with LCS abrogate the deleterious effects of E. coli K1 on intestinal integrity
Once adhere to enterocyte, pathogen such as E. coli K1 could compromise intestinal integrity and translocation across the intestinal barrier into the blood stream, leading to systemic infection. Many studies have reported the protective effects of LCS against gut barrier injury caused by chemicals, such as alcohol, dextran sodium sulfate and hydrogen peroxide35,36,37,38,39. However, little is known about the roles of LCS on pathogen-induced intestinal barrier injury. Here, we examined whether LCS could abrogate the deleterious effects of E. coli K1 on intestinal integrity. Firstly, we explored whether treatment with MRS or LCS alone could reduce the trans-epithelial electrical resistance (TEER) values of Caco-2 monolayers. As shown in Fig. 3A, stable TEER values were observed in the control, MRS, 1% LCS and 2% LCS treated Caco-2 monolayers, suggesting that these factors have no detrimental role on intestinal integrity. However, infection with E. coli K1 could reduce the TEER values of Caco-2 monolayer in a time-dependent manner. In contrast, when pre-incubated with LCS for 3 h before infection, the reduction of TEER was alleviated (Fig. 3A). In parallel, the numbers of E. coli K1 translocated from the upper chamber to the lower chamber of transwell insert were dramatically reduced in LCS treated groups (Fig. 3B). These results suggest that LCS could reduce E. coli-caused gut barrier injury and prevent from intestinal translocation of E. coli K1.
(A) TEER value of Caco-2 monolayers incubated with cell culture medium (CON), 2% MRS, 1% LCS and 2% LCS for 0–5 h without E. coli K1 infection or pre-treatment with LCS for 3 h prior to infection with E. coli K1 (MOI = 100) for 5 h. (B) The numbers of recovered E. coli K1 that were translocated to the basolateral medium after 5 h of apical infection. Results are presented as CFU/ml cell culture medium, **P < 0.01. Cells were treated as shown in Fig. 2C, (C) representative western blot for ZO-1 in Caco-2 lysates. β-actin bands were used as an indicator of protein loading. (D) Caco-2 monolayers stained for the tight junction protein ZO-1 (green, red arrows) was detected by a fluorescence microscope. Yellow arrows show the broken lining of ZO-1 expressions.
To further investigate the protective effect of LCS on intestinal barrier function, we examined the zonula occludens-1 (ZO-1) expression in Caco-2 during E. coli K1 infection using western blot and immunofluorescent staining. As shown in Fig. 3C, E. coli K1 challenge resulted in a marked reduction of ZO-1 expression, but this detrimental role was abrogated by pre-incubation with LCS. Similar results were observed in immunofluorescent staining, which were shown in Fig. 3D. Non-infected Caco-2 exhibited continuous expression of ZO-1 between adjacent cells, and showed a typical “chicken-wire” shape with a continuous lining (red arrow). However, infection with E. coli K1 induced different degrees of morphological damage (yellow arrow). Pre-incubation with LCS significantly inhibited E. coli-induced destruction of ZO-1 tight junction morphology. Thus, we concluded that pre-treatment with LCS protected the intestinal barrier integrity against E. coli K1-caused injury.
Effect of LCS on bacterial intestinal colonization, gut barrier injury and systemic infection during E. coli K1 infection in neonatal rats
To examine the protective effect of LCS against neonatal E. coli K1 bacteremia and meningitis in vivo, we induced systemic E. coli K1 infection in neonatal rats via feeding live E. coli K1 as described previously11,40. In this animal model, the course of E. coli K1 infection mimics the natural route of intestinal colonization, translocation, bacteremia, sepsis and meningitis found in the human neonates. At the beginning of the experiments, all rat pups (1-day-postpartum, P1) from four litters were randomly divided into four groups and received PBS, 20% MRS, 10% or 20% LCS by oral gavage (twice a day for three days). Then systemic infection was induced by oral gavage with 5 × 109 colony-forming unit (CFU) of E. coli K1 and the protective effects of LCS against bacterial intestinal colonization, gut barrier injury and systemic infection were evaluated as described in Methods. As shown in Fig. 4A, feeding E. coli K1 to PBS- or MRS-treated pups led to almost 100% intestinal colonization within 24 h after infection and persisted throughout the period of observation (6 days). In contrast, only 73% pups in 10% LCS treated group and 47% pups in 20% LCS treated group were colonized with E. coli within 24 h after infection. These results indicated that pre-treatment with LCS delayed the intestinal colonization of E. coli K1. Next, we evaluated the intestinal barrier permeability using fluorescein isothiocyanate (FITC)-dextran. Results showed that the pups which were pre-treated with LCS have lower serum levels of FITC-dextran than that in untreated pups (Fig. 4B), indicating that LCS could prevent E. coli-induced intestinal barrier injury.
Rat pups were pretreated with PBS, MRS, 10% or 20% LCS for 3 days. Then all pups were infected with E. coli K1 (5 × 109 CFU) by oral gavage. MRS (LGG’s medium) was used as a control. (A) The percentage of rat pups colonized with E. coli. All values represent the means of triplicate determinations. (B) Pups were treated as described above, intestinal permeability was evaluated using FITC-dextran. The results are expressed as relative content, taking the value for the control (un-infected pups) as 1. *P < 0.05, ***P < 0.001.
The numbers of E. coli K1 in blood, liver, spleen and cerebrospinal fluid (CSF) were detected as described in Methods. Our results showed that E. coli K1 CFU counts in blood, liver, spleen and CSF were significantly decreased in rat pups that were pre-treated with LCS (Fig. 5A–D). Taken together, these data suggested that LCS could raise the resistance of neonatal rats to gut-derived E. coli K1 infection.
Rats were treated as described in Fig. 4. E. coli K1 were recovered 60 hours after infection from the blood (A), liver (B), spleen (C) and CSF (D). All data were expressed as means ± standard deviation. *P < 0.05, **P < 0.01, ***P < 0.001.
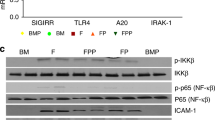
LCS enhances the neonatal resistance to E. coli K1 infection via promoting postnatal maturation of intestinal defense
Birchenough GM et al. found that 9-day-old (P9) Wistar rat pups were more resistant to gut-derived E. coli K1 infection than two-day-old (P2) pups40. In our study, similar result was observed in Sprague Dawley (SD) rat pups. As shown in Fig. 6A–C, P3 pups, which were infected with E. coli K1 showed higher mortality, bacteremia and gut barrier permeability compared with P5, P7 and P9 pups. P9 pups were refractory to E. coli K1 infection with lowest mortality, bacteremia and intestinal barrier permeability. These results suggested that neonatal intestinal defense progress rapidly after birth. Importantly, we could notice that, on pre-treatment with LCS for three days, P3 pups could exhibit resistance to E. coli K1 infection similar with the P7 pups (Fig. 6A–C). Thus, we speculated that LCS has considerable potential to promote the maturation of neonatal intestinal defense. Based on these observations, we hypothesize that improvement in the maturation of intestinal defense could represent the underlying mechanism to explain the contribution of LCS to neonatal resistance against oral E. coli K1 infection. Further to test this hypothesis, we firstly explored whether administration with LCS promotes intestinal epithelial cell proliferation and differentiation via detecting the expression of Ki67 and MUC2 in the small intestine and colon respectively. As shown in Fig. 7A and B, the expression levels of Ki67 and MUC2 were significantly increased in the intestine tissues of LCS treated pups.
P3, P5, P7, P9 and LCS-treated (pre-treatment for 3 days) P3 pups were fed with 5 × 109 CFU E. coli K1. (A) Percentage of survival (%) of pups. All the pups were monitored for a period of 7 days. (B) The number of E. coli K1 recovery from blood of neonatal rats. (C) Serum FITC-dextran was quantified as a measure of intestinal permeability. The results are expressed as relative content, taking the value for the P3 pups as 1. P1 pups were treated with or without 20% LCS for 3 days. (D) Ileum tissues were processed with PAS stain. (E) The percentage of PAS-positive cells per villus was calculated. (F) FITC-dextran assay was performed to evaluate the gut barrier formation in vivo. All data were expressed as means ± standard deviation. *P < 0.05, **P < 0.01.
P1 rat pups were treated with or without 20% LCS for 3 days. Immunostaining of Ki67 (A) and MUC2 (B) revealed an increase in the positive signals in intestine tissues of LCS-treated pups, compared with the untreated pups. Semiquantitative determination of Ki67 and MUC2 positive signals (right panel) was performed using Image J. **P < 0.01.
Mucin, immunoglobulin A (IgA) and barrier function are key components of the intestinal defense. Thus, we next compared the production of mucin and IgA and formation of intestinal barrier function between LCS treated and untreated pups. Results showed that LCS treated pups have a higher expression level of mucin and IgA levels (Figs 6D,E and 8A). To evaluate the formation of intestinal barrier function, the gut permeability and expression of tight junction protein ZO-1 were detected. Intestinal permeability assay showed that LCS treated pups have lower intestinal permeability than that in untreated pups (Fig. 6F). Meanwhile, immunohistochemical staining showed that pre-treatment with LCS increased ZO-1 expression on the membrane of ileum (Fig. 8B). Overall, these results suggested that LCS could accelerate the development of neonatal intestinal defense.
P1 pups were treated as described in Fig. 7. Immunostaining of IgA (A) and ZO-1 (B) revealed an increase in the positive signals in intestine tissues of LCS-treated pups, compared with the untreated pups. Semiquantitative determination of IgA and ZO-1 positive signals (right panel) was performed using Image J. *P < 0.05, **P < 0.01.
Discussion
In the present study, we intended to make a strategy shift from treatment to prevention of the neonatal systemic E. coli K1 infection through the use of probiotic culture product to enhance the intestinal defense, which is a unique preventive barrier against natural E. coli K1 infection. Our data showed that pre-treatment with LCS is able to delay E. coli K1 intestinal colonization, inhibit bacterial translocation and dissemination, and reduce bacteremia and meningitis in neonatal rats. These results suggested that administration with LCS enhances the resistance of neonatal rats to E. coli K1 infection. Further study found that LCS promotes intestinal proliferation and differentiation, accelerate intestinal barrier formation and increase mucin and IgA production in the gut of neonatal rat. These data indicated that neonatal administration with LCS accelerates the maturation of intestinal defense and confers a high resistance to intestinal infection. To the best of our knowledge, this is the first study reporting such beneficial effect of probiotic culture product on maturation of neonatal intestinal defense. Collectively, our data not only indicated that LCS has a great potential in preventing neonatal E. coli K1 sepsis and meningitis, but also has a potential to become an effective prophylaxis for immature intestine-associated diseases, such as inflammatory bowel disease, infectious enteritis and necrotizing enterocolitis.
Probiotics secrete many kinds of antimicrobial substances that inhibit pathogenic infection by direct killing effect, including bacteriocins, reuterin, organic acid, hydrogen peroxide and some heat-resistant small peptides41. It has been established that the antimicrobial activity of LGG is executed entirely through secreted cell-free supernatants41. In this study, we have found the inhibitory effect of LCS on bacterial adhesion and invasion. This effect, however, is unlikely to execute via direct inhibition on the growth of bacteria, because the concentrations of LCS used here, did not show any extracellular antimicrobial activity (Fig. 1E). In contrast, the anti-adhesion mechanism was based on indirect enhancement of mucin production that separated the pathogen from Caco-2 cells (Fig. 2E and F). Because LCS has no direct antibacterial activity to pathogens, it is unlikely to develop the microbial resistance. Meanwhile, this indirect mechanism makes LCS exert a preventive effect on most of gut-derived pathogenic infections rather than only E. coli. Furthermore, we found that LCS could also promote mucin production in the intestinal tract of neonatal rats (Fig. 6D and E), which is much significant during the neonatal period. Firstly, during neaonatal period, a protective intestinal mucus barrier always not fully developed40, and the up-regulated mucin production will form a physical barrier to protect the underlying epithelium from the attachment of pathogens. Secondly, mucin could provide carbon, nitrogen, and sulfur source for intestinal microbiota, especially Akkermansia muciniphila, which could through a turnover of mucus (degrade mucins and simulate mucin production), maintain the mucus thickness to protect the intestinal barrier42.
Intestinal epithelial barrier is formed and maintained by tight junction complexes, which plays a significant role as access point that checks bacterial translocation across the cell barrier. Disruption of the integrity of this barrier occurs in several diseases, such as inflammatory bowel disease43, necrotizing enterocolitis44 and certain bacterial and virus infections45. Numerous studies have reported the protective effect of live probiotics on the pathogen-induced tight junction injury in vitro and in vivo. For example, Johnson-Henry KC et al. showed that live LGG, but not heat-inactivated LGG protected polarized MDCK-I and T84 epithelial cell against Enterohemorrhagic E. coli-caused changes in TEER, dextran permeability, and redistribution of ZO-1 and claudin-146. However, evidence on probiotic-derived product exerting protective effect against pathogen-caused tight junction injury is still lacking. In the present study, we observed that pre-treatment with LCS could alleviate E. coli K1-induced reduction of TEER values and ZO-1 expression in Caco-2 monolayer (Fig. 3A,C and D). These results indicated that LCS could prevent from E. coli K1-induced tight junction damage, as well as convincingly suggested that LGG culture supernatant has the similar protective effect on intestinal epithelial barrier as live LGG.
The immature intestinal defense in the neonatal period may provide opportunities for pathogenic translocation across the gut barrier into the blood stream, leading to systemic inflammation and infection15,44,47. In our study, we observed that feeding of E. coli K1 to P3 pups led to about 87% death within 7 days, with the higher intestinal permeability and more serious bacteremia than that in P5, P7 and P9 pups (Fig. 6A–C). The same phenomenon occurs in humans, because human neonates are also most susceptible to E. coli K1 infection during the early neonatal period48. Importantly, these results indicated that the intestinal defense is undergoing rapid maturation after birth. Interestingly, when pre-treated with LCS for three days, P3 pups exhibited the same resistance to oral E. coli K1 infection as P7 pups (Fig. 6A–C), indicating that LCS has potential to promote maturation of neonatal intestinal defense. Subsequently, we found that expression levels of Ki67 and MUC2, the maker of cell proliferation and intestinal differentiation respectively49, were significantly higher in LCS treated pups than those in untreated pups (Fig. 7A and B). Moreover, we observed that LCS could modulate important intestinal defense including ZO-1, mucin, IgA and barrier permeability (Figs 6D–F, 8A and B). These data suggested that LCS is able to accelerate the maturation of neonatal intestinal defense, and thereby reduce the susceptibility of neonates to E. coli K1 infection. These results were consisted with a previous study that, neonatal mice which colonization with live LGG had more sophisticated intestinal functions and were less susceptible to dextran sodium sulfate-induced colitis50 than the mice without LGG colonization. In another study, Ravi M. Patel et al. reported that neonatal colonization of mice with live or heat-killed LGG accelerates maturation of intestinal barrier function by promoting claudin 3 expression44. However, the authors found that administration with high-dose live LGG (109 CFU/day for 7 days) lead to an increased mortality in 1-week-old mice. This paper highlight the safety concerns about the application of live probiotics in neonates. Indeed, according to the regulations of Food and Drug Administration in the United States, routine use of live organisms to immunocompromised premature infants is prohibited51. In this study, we found that LGG culture supernatant has shown a progressive effect on maturation of neonatal intestinal functions similar to live LGG, and thus support the application of probiotic-derived factors to replace live probiotic to avoid the potential risks if necessary.
Gut microbiome is largely subjected to dynamic changes after birth, and temporally take part in maturation of the intestinal immune system52. A recent study done by Deshmukh HS et al. demonstrated that a balanced intestinal microbiota plays key roles in neonatal resistance to E. coli K1 sepsis52. Thus, it is interesting to explore the effect of LCS on formation of neonatal intestinal microbiota. We speculated that LCS has a great potential to promote development of neonatal intestinal microbiota. Two rational bases supported this hypothesis. Firstly, it is established that besides protecting the enterocyte from pathogenic assault, mucus also provide glycan-dependent anchoring sites and nutrients to intestinal commensal microbiota53. Thus, it is possible that LCS-induced mucin production may help the colonization of commensal bacteria. Secondly, IgA, the important defense in intestinal mucosa to prevent the pathogen from attaching to the enterocyte, has been demonstrated that could promote the establishment of microbiota composition and maintains the diversity of microbiota54. Moreover, research has shown that IgA is able to maintain the homeostasis of gut flora using an “immune exclusion” strategy to exclude the pathogenic microbes and control the commensal microbes55. Thus, induced IgA expression by LCS may play an important role in formation, development and maintenance of intestinal microbiota composition. Further study should focus on exploring the relationship between LCS and formation of neonatal intestinal microbiota.
In the present study, we suggested that LCS has a promising application in preventing neonatal intestinal infection. However, it is unclear which LCS components exert the beneficial effects. LCS is a complex mixture containing lots of substances, including lipids, organic acids, proteins and other small molecules. Due to the complexity and uncertainty, it is necessary to keep an eye on the side effects of LCS. To date, p40 and p75 are two most characterized proteins purified from LGG-derived soluble factors and both of them have beneficial effects on intestinal barrier functions. However, p40 showed more potent effects than p7556. More recently, it has been established that p40 can induce IgA and MUC2 production in intestinal tissues through active epidermal growth factor receptor (EGFR)57,58. Furthermore, using sodium dodecyl sulfate-polyacrylamide gel electrophoresis (SDS-PAGE) analysis, we also detected two bands, ~40 KDa and ~75 KDa, exist in LCS in our study (data not shown). In accordance with our findings, it is reasonable to speculate that p40 may be the major active ingredient in LCS to exhibit the beneficial effects towards infectious pathogens.
In summary, our data suggested that LCS could prevent neonatal gut-derived E. coli K1 infection through promoting the maturation of neonatal intestinal defense. We believed that LCS has a great potential to become an alternative treatment option for preventing neonatal E. coli K1 sepsis and meningitis. Furthermore, our data also confirmed that supernatant from certain probiotic could exert beneficial effects similar with their live probiotic counterparts. Further identification of the active ingredients in LCS is required to develop newer prophylaxis for preventing neonatal sepsis and meningitis.
Methods
Ethics statement
All research involving animals has been approved by the ethics committee and performed strictly according to the guidelines for animal care in Southern Medical University (SMU, Guangzhou, China). Timed-pregnant SD rats were obtained from Animal Experimental Center of SMU and bred in-house. All supplements including food, water, and enrichment were autoclaved, and animals were kept in the animal facility. All surgeries were performed under anesthesia with ketamine and lidocaine, and utmost efforts were taken to minimize suffering.
Bacterial strains, cell lines and cultures
The probiotic strain LGG (ATCC 53103) and pathogen E. coli K1 were kindly provided by Prof. Sheng-He Huang (University of Southern California, USA). E. coli K1 is a clinical isolate [E. coli RS218 (O18:K1:H7)] with rifampicin-resistance from the CSF of a neonate with meningitis11. LGG was grown in De Man, Rogosa, and Sharpe (MRS) broth (Oxoid, Hampshire, UK) at 37 °C for 24 hours. E. coli K1 was grown for 14 h at 37 °C in brain heart infusion (BHI) broth in the presence of rifampicin (100 μg/ml). LCS was prepared by centrifugation at 10,000 rpm for 1 minute (m) at 4 °C and dual filtration through 0.22 μm millipore filters. To avoid the detrimental effect of acidic compounds, LCS was concentrated using 3 kDa spin columns and diluted into cell culture medium or PBS at appropriate pH value (7–8) for subsequent experiments. To exclude the potential impact of probiotic culture medium, MRS were processed as LCS and served as controls in certain experiments. Caco-2 was purchased from Shanghai Institute of Cell Biology (Shanghai, China) and routinely cultured in Eagle’s Minimum Essential Medium with 10% heat inactivated fetal bovine serum and streptomycin (100 mg/ml) and penicillin G (50 mg/ml) at 37 °C in 5% CO2.
Adhesion and invasion assays
Caco-2 cells were grown in a 24-well tissue culture plate (105 cells per well) at a minimum of 12 days to allow them fully differentiate11. Before the adhesion assays, Caco-2 were pre-incubated with cell culture medium, 2% MRS, 0.5% LCS, 1% LCS or 2% LCS (dilution in cell culture medium) for 3 h. After treatment, cell monolayers were washed with phosphate buffered saline (PBS) three times and examined under the microscope. No morphologic changes were observed. Adhesion assays were performed in Caco-2 as previously described11,59. In brief, approximately 107 CFU E. coli K1 were added to Caco-2 monolayer with a multiplicity of infection (MOI) = 100. The monolayers were incubated for 3 h at 37 °C. After incubation, the monolayers were washed three times with PBS and lysed by 0.5% Triton X-100 for 8 m. The bacteria were collected and enumerated by BHI agar plates with rifampicin (100 μg/ml). Each assay was performed in triplicate wells and repeated three times. The results were expressed as a percentage of the control (E. coli infection only).
For invasion assays, Caco-2 monolayers were infected with E. coli K1 as described as above. To eliminate any extracellular bacteria, the monolayers were incubated with experimental medium containing gentamicin (100 μg/ml) for 1 h at 37 °C. Then monolayers were washed three times with PBS and lysed by 0.5% Triton X-100 for 8 m. Intracellular bacteria were determined as mentioned above. Each assay was performed in triplicate wells and repeated three times. The results were expressed as a percentage of the control (E. coli infection only).
We used the NAC (Sigma-Aldrich, St. Louis, USA) to quantify E. coli K1 which was trapped in mucin or adhered to Caco-2 cells34. Caco-2 monolayers were infected with E. coli K1 as described in adhesion assays. Then infected monolayers were incubated with NAC (10 mM in PBS containing 0.2 μM CaCl2, 0.5 mM MgCl2 and 15 mM glucose) to remove the mucin layer (contains E. coli K1). Cells were washed four times with PBS to remove NAC and lysed with 0.5% Triton X-100 for 8 m. The number of associated bacteria was enumerated by BHI agar plate with rifampicin (100 μg/ml). To evaluate the bacteria trapped into mucus, removed mucin layers were collected and plated on BHI agar plates with rifampin (100 μg/ml) for counting. Each assay was performed in triplicate wells and repeated three times. Data are expressed as the percentage of trapped E. coli K1 or adhered E. coli K1 among the added bacteria.
Bacterial translocation and TEER measurements
Caco-2 cells were grown in Transwell inserts (6.5 mm diameter, 3 μm pore size, Corning Costar Corp., USA) for at least 21 days to differentiate and to form tight junctions. This polarized monolayer mimics the pathogen translocation across the gut barrier (upper chamber) into the blood circulation (lower chamber). To determine whether LCS have protective effect on intestinal barrier against E. coli K1 infection, Caco-2 monolayers growth on Transwell insert were pre-incubated with cell culture medium, 2% MRS, 1% LCS, or 2% LCS for 3 h at 37 °C and 5% CO2. Then E. coli K1 (MOI = 100) were added to the upper chamber of Transwell inserts. TEER values were measured at 0, 1, 2, 3, 4, and 5 h post infection using a Millicell electrical resistance apparatus (EVOMAX, World Precision Instruments, USA). The bacteria translocated from the upper chamber to the lower chamber at 5 h post infection were quantified by plating on BHI agar with rifampicin (100 μg/ml) and incubated at 37 °C overnight.
PAS assay
Caco-2 monolayers grown in 6-well plate were treated with different levels of E. coli K1 (MOI = 50, 100 or 200) or LCS (1% or 2%) or infected with E. coli K1 as mentioned in the adhesion assay. Then treated monolayers were collected and lysed in lysis buffer to obtain soluble ingredients. Mucin production in soluble fractions was measured as described by Wang LH et al.58. In brief, 0.1% periodic acid was added to each sample and incubated for 2 h at 37 °C. Then Schiff reagent was added and incubated for 30 m in dark at room temperature. Optical density of each sample was assessed using a microtitre plate reader set at 550 nm. All samples were analyzed in triplicate.
PAS staining
Caco-2 cells grown in 24-well plate were infected with E. coli K1 as described in the adhesion assay. Then monolayers were harvested and fixed in 4% paraformaldehyde at room temperature for 20 m. PAS staining was performed according to the manufacturer’s instructions of PAS kit (Solarbio Science & Technology Co., Ltd, Beijing, China). The PAS-stained wells were counterstained with hematoxylin and observed using light microscopy. For PAS staining of intestinal tissues, 0035 μm sections were fixed in 4% formaldehyde and paraffin-embedded. PAS staining was conducted as described above.
Neonatal rat model of hematogenous E. coli K1 systemic infection
Systemic E. coli K1 infection was induced using specific pathogen free SD rats as described previously with minor modifications11,40. Litters were retained with their natural mothers after birth. Four litters (10 pups per litter) were pooled and randomly distributed into four groups. Pups were fed with 100 ul of PBS, 20% MRS, 10% LCS or 20% LCS (dilution in PBS) twice a day for three days. Then all pups were gavage with 100 μl of E. coli K1 (5 × 109 CFU). Sixty hours post infection, blood, liver and spleen were extracted aseptically after anaesthetizing the rats with ketamine and lidocaine. CSF samples were collected as described previously60. Bacteria were quantified in homogenized tissues by serial dilution culture on BHI agar plates with rifampicin (100 μg/ml). Gastrointestinal tract colonization of E. coli K1 was determined at 24 h intervals by culture of perianal swabs on MacConkey’s agar as described previously61.
Intestinal permeability was determined as previously described62. Briefly, pups were given FITC dextran (MW 4000 at 60 mg/100 g, Sigma) by gavage 4 h before sacrifice. Blood was collected from heart puncture and FITC concentrations were measured using a fluorescence spectrophotometer at an excitation wavelength of 485 nm and emission wavelength of 535 nm.
Histopathological examination and immunohistochemical staining
For the immunohistochemical staining, 5 μm paraffin-embedded sections were deparaffinized and antigen was retrieved. Sections were blocked in 1% normal goat serum and incubated overnight at 4 °C with antibody specific for MUC2, ZO-1, Ki67 and IgA (all from Abcam, Cambridge, UK) respectively. The primary antibodies were visualized using horseradish peroxidase (HRP)-coupled second antibodies with 50 mM Tris-HCl buffer (pH 7.4) containing DAB (3,3′-diaminobenzidine) and H2O2, and the sections were lightly counterstained with hemotoxylin.
Quantification of immunoreactive signal was performed using National Institutes of Health image analysis software Image J63. In brief, the red-green-blue (RGB) bitmap images were firstly converted to 8-bit grayscale, then the threshold was modulated to display only positive signals and eliminate the background. The same cutoff value of threshold was used to analyze all the slides stained concurrently. The staining intensity measurements were calculated for the total area (total intensity/mm2). A total of five sections for each group were analyzed. We expressed the results as the relative area, taking the value of the control (untreated P3 pups) as 1.
Western blotting analysis
To assess the expression of ZO-1 and MUC2 in Caco-2, cells were collected and lysed on ice in radio-immunoprecipitation assay buffer and boiled at 100 °C for 10 min. Equal amounts of proteins were separated on SDS polyacrylamide gels and transferred onto polyvinylidene difluoride (PVDF) membranes (Millipore). The membranes were incubated with a rabbit anti-ZO-1 antibody (1:200) or rabbit anti-MUC2 antibody (1:2000). Expression of primary antibodies was visualized using HRP-coupled second antibodies and enhanced chemiluminescence reagent kit (Bio-Rad Laboratories, USA). A goat polyclonal anti-β-actin antibody (1:1500) was used as a loading control. Each western blot assay was repeated at least three times.
Immunofluorescence analysis
Caco-2 monolayers were fixed in 4% paraformaldehyde for 10 min at room temperature. Cells were blocked in 5% normal goat serum in PBS for 1 h at room temperature. Then monolayers were probed with a rabbit anti-ZO-1 antibody for 12 h at 4 °C followed by incubation with Alexa Fluor 568-coupled goat anti-rabbit secondary antibody (Invitrogen, Carlsbad, CA) at room temperature in dark for 1 h. Slides were mounted and observed using fluorescence microscopy (Nikon Eclipse: TE 2000-E, Japan).
Statistical Analysis
Data are shown in mean ± standard deviation and analyzed by one-way analysis of variance (ANOVA) tests. All statistical analyses were carried out using SPSS 13.0 (SPSS Inc., Chicago, IL, USA) and P < 0.05 was considered to be statistically significant.
Additional Information
How to cite this article: He, X. et al. Lactobacillus rhamnosus GG supernatant enhance neonatal resistance to systemic Escherichia coli K1 infection by accelerating development of intestinal defense. Sci. Rep. 7, 43305; doi: 10.1038/srep43305 (2017).
Publisher's note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
Stoll, B. J. et al. Trends in Care Practices, Morbidity, and Mortality of Extremely Preterm Neonates, 1993-2012. Journal of the American Medical Association 314, 1039–1051 (2015).
Furyk, J. S., Swann, O. & Molyneux, E. Systematic review: neonatal meningitis in the developing world. Tropical Medicine & International Health Tm & Ih 16, 672–679 (2011).
Brouwer, M. C., Tunkel, A. R. & Van, d. B. D. Epidemiology, diagnosis, and antimicrobial treatment of acute bacterial meningitis. Clinical Microbiology Reviews 23, 467–492 (2010).
Leib, S. L. & Täuber, M. G. Pathogenesis of bacterial meningitis. Infectious Disease Clinics of North America 13, 527–548 (1999).
Kim, K. S. Current concepts on the pathogenesis of Escherichia coli meningitis: implications for therapy and prevention. Current Opinion in Infectious Diseases 25, 273–278 (2012).
Cornette, L. Prolonged initial empirical antibiotic treatment is associated with adverse outcomes in premature infants. Journal of Pediatrics 159, 720–725 (2011).
Kim, K. S. Pathogenesis of bacterial meningitis: from bacteraemia to neuronal injury. Nature Reviews Neuroscience 4, 376–385 (2003).
Witcomb, L. A., Collins, J. W., Mccarthy, A. J., Frankel, G. & Taylor, P. W. Bioluminescent Imaging Reveals Novel Patterns of Colonization and Invasion in Systemic Escherichia coli K1 Experimental Infection in the Neonatal Rat. Infection & Immunity 83, 4528–4540 (2015).
Yousuf, F. A. et al. Interactions of neuropathogenic Escherichia coli K1 (RS218) and its derivatives lacking genomic islands with phagocytic Acanthamoeba castellanii and nonphagocytic brain endothelial cells. Biomed Research International 2014, 265424–265424 (2014).
Wang, S. et al. Pathogenic Triad in Bacterial Meningitis: Pathogen Invasion, NF-κB Activation, and Leukocyte Transmigration that Occur at the Blood-Brain Barrier. Frontiers in Microbiology 7, 10.3389/fmicb.2016.00148 (2016).
Huang, S. H., He, L., Zhou, Y., Wu, C. H. & Jong, A. Lactobacillus rhamnosus GG Suppresses Meningitic E. coli K1 Penetration across Human Intestinal Epithelial Cells In Vitro and Protects Neonatal Rats against Experimental Hematogenous Meningitis. International Journal of Microbiology 2009, 10.1155/2009/647862 (2009).
Hotel, A. C. P. Health and Nutritional Properties of Probiotics in Food Including Powder Milk with Live Lactic Acid Bacteria – Joint FAO/WHO Expert Consultation. 2014 (2001).
Delzenne, N. M., Neyrinck, A. M., Bäckhed, F. & Cani, P. D. Targeting gut microbiota in obesity: effects of prebiotics and probiotics. Nature Reviews Endocrinology 4, 639–646 (2011).
Harb, H. et al. Neonatal supplementation of processed supernatant from Lactobacillus rhamnosus GG improves allergic airway inflammation in mice later in life. Clinical & Experimental Allergy 43, 353–364 (2013).
Jakaitis, B. M. & Denning, P. W. Commensal and probiotic bacteria may prevent NEC by maturing intestinal host defenses. Pathophysiology 21, 47–54 (2014).
Yang, X. et al. High protective efficacy of rice bran against human rotavirus diarrhea via enhancing probiotic growth, gut barrier function, and innate immunity. Scientific Reports 5, 10.1038/srep15004 (2015).
Khailova, L., Frank, D. N., Dominguez, J. A. & Wischmeyer, P. E. Probiotic administration reduces mortality and improves intestinal epithelial homeostasis in experimental sepsis. Anesthesiology 119, 166–177 (2013).
Khailova, L., Petrie, B., Baird, C. H., Dominguez Rieg, J. A. & Wischmeyer, P. E. Lactobacillus rhamnosus GG and Bifidobacterium longum attenuate lung injury and inflammatory response in experimental sepsis. Plos One 9, e97861 (2014).
Saini, R., Saini, S. & Sharma, S. Potential of probiotics in controlling cardiovascular diseases. Journal of Cardiovascular Disease Research 1, 213–214 (2010).
Howarth, G. S. & Wang, H. Role of endogenous microbiota, probiotics and their biological products in human health. Nutrients 5, 58–81 (2013).
Howarth, G. S. Probiotic-derived factors: probiotaceuticals? Journal of Nutrition 140, 229–230 (2010).
Robin, F. et al. Lactobacillus rhamnosus meningitis following recurrent episodes of bacteremia in a child undergoing allogeneic hematopoietic stem cell transplantation. Journal of Clinical Microbiology 48, 4317–4319 (2010).
Kulkarni, H. S. & Khoury, C. C. Sepsis associated with Lactobacillus bacteremia in a patient with ischemic colitis. Indian journal of critical care medicine: peer-reviewed, official publication of Indian Society of Critical Care Medicine 18, 606–608 (2014).
Gouriet, F., Million, M., Henri, M., Fournier, P. E. & Raoult, D. Lactobacillus rhamnosus bacteremia: an emerging clinical entity. European Journal of Clinical Microbiology & Infectious Diseases 31, 2469–2480 (2012).
Besselink, M. G. et al. Probiotic prophylaxis in predicted severe acute pancreatitis: a randomised, double-blind, placebo-controlled trial. Lancet 371, 651–659 (2008).
Nougayrède, J. P. et al. Escherichia coli Induces DNA Double-Strand Breaks in Eukaryotic Cells. Science 313, 848–851 (2006).
Cuevas-Ramos, G. & Isberg, R. R. Escherichia coli induces DNA damage in vivo and triggers genomic instability in mammalian cells. Proceedings of the National Academy of Sciences of the United States of America 107, 11537–11542 (2010).
Million, M. & Raoult, D. Publication biases in probiotics. European Journal of Epidemiology 27, 885–886 (2012).
Tsilingiri, K. et al. Probiotic and postbiotic activity in health and disease: comparison on a novel polarised ex-vivo organ culture model. Gut 61, 1007–1015 (2012).
Tsilingiri, K. & Rescigno, M. Postbiotics: what else? Beneficial microbes 4, 101–107 (2012).
Patel, R. M. & Denning, P. W. Therapeutic use of prebiotics, probiotics, and postbiotics to prevent necrotizing enterocolitis: what is the current evidence? Clinics in perinatology 40, 11–25 (2013).
Cicenia, A. et al. Postbiotic activities of lactobacilli-derived factors. Journal of clinical gastroenterology 48, S18–S22 (2014).
Fong, F. L. Y., Kirjavainen, P. V. & Elnezami, H. Immunomodulation of Lactobacillus rhamnosus GG (LGG)-derived soluble factors on antigen-presenting cells of healthy blood donors. Scientific Reports 6, 10.1038/srep22845 (2016).
Valeri, M. et al. Pathogenic E. coli Exploits SslE Mucinase Activity to Translocate through the Mucosal Barrier and Get Access to Host Cells. Plos One 10, 10.1371/journal.pone.0117486 (2015).
Wang, Y. et al. Lactobacillus rhamnosus GG culture supernatant ameliorates acute alcohol-induced intestinal permeability and liver injury. Ajp Gastrointestinal & Liver Physiology 303, 32–41 (2012).
Yoda, K. et al. Lactobacillus GG-fermented milk prevents DSS-induced colitis and regulates intestinal epithelial homeostasis through activation of epidermal growth factor receptor. European Journal of Nutrition 53, 105–115 (2014).
Seth, A., Yan, F., Polk, D. B. & Rao, R. K. Probiotics ameliorate the hydrogen peroxide-induced epithelial barrier disruption by a PKC- and MAP kinase-dependent mechanism. Ajp Gastrointestinal & Liver Physiology 294, G1060–1069 (2008).
Chen, R. C. et al. Lactobacillus rhamnosus GG supernatant promotes intestinal barrier function, balances T reg and T H 17 cells and ameliorates hepatic injury in a mouse model of chronic-binge alcohol feeding. Toxicology Letters 241, 103–110 (2015).
Zhang, M. et al. Enhanced AMPK phosphorylation contributes to the beneficial effects of Lactobacillus rhamnosus GG supernatant on chronic alcohol-induced fatty liver disease. Journal of Nutritional Biochemistry 26, 337–344 (2014).
Birchenough, G. M. et al. Altered Innate Defenses in the Neonatal Gastrointestinal Tract in Response to Colonization by Neuropathogenic Escherichia coli. Infection & Immunity 81, 3264–3275 (2013).
Moal, V. L. & Servin, A. L. Anti-infective activities of lactobacillus strains in the human intestinal microbiota: from probiotics to gastrointestinal anti-infectious biotherapeutic agents. Clinical Microbiology Reviews 27, 167–199 (2014).
Derrien, M., Belzer, C. & Vos, W. M. D. Akkermansia muciniphila and its role in regulating host functions. Microbial Pathogenesis 2016, 10.1016/j.micpath.2016.02.005 (2016).
Xavier, R. J. & Podolsky, D. K. Unravelling the pathogenesis of inflammatory bowel disease. Nature 448, 427–434 (2007).
Patel, R. M. et al. Probiotic Bacteria Induce Maturation of Intestinal Claudin 3 Expression and Barrier Function. American Journal of Pathology 180, 626–635 (2012).
Clayburgh, D. R., Shen, L. & Turner, J. R. A porous defense: the leaky epithelial barrier in intestinal disease. Laboratory investigation; a journal of technical methods and pathology 84, 282–291 (2004).
Johnsonhenry, K. C., Donato, K. A., Shentu, G., Gordanpour, M. & Sherman, P. M. Lactobacillus rhamnosus Strain GG Prevents Enterohemorrhagic Escherichia coli O157:H7-Induced Changes in Epithelial Barrier Function. Infection & Immunity 76, 1340–1348 (2008).
Piena-Spoel, M., Albers, M. J. I. J., Kate, J. T. & Tibboel, D. Intestinal permeability in newborns with necrotizing enterocolitis and controls: Does the sugar absorption test provide guidelines for the time to (re-)introduce enteral nutrition? ☆. Journal of Pediatric Surgery 36, 587–592 (2001).
Holt, D. E., Halket, S., Louvois, J. D. & Harvey, D. Neonatal meningitis in England and Wales: 10 years on. Archives of Disease in Childhood Fetal & Neonatal Edition 84, 85–89 (2001).
Hahn, H. P. et al. Intestinal differentiation in metaplastic, non-goblet columnar epithelium in the esophagus. American Journal of Surgical Pathology 33, 1006–1015 (2009).
Yan, F. et al. Neonatal colonization of mice with LGG promotes intestinal development and decreases susceptibility to colitis in adulthood. Mucosal Immunology 2016, 10.1038/mi.2016.43. (2016).
Weng, M., Ganguli, K., Zhu, W., Shi, H. N. & Walker, W. A. Conditioned medium from Bifidobacteria infantis protects against Cronobacter sakazakii-induced intestinal inflammation in newborn mice. American Journal of Physiology Gastrointestinal & Liver Physiology 306, 779–787 (2014).
Deshmukh, H. S. et al. The microbiota regulates neutrophil homeostasis and host resistance to Escherichia coli K1 sepsis in neonatal mice. Nature Medicine 20, 141–151 (2014).
Gutzeit, C., Magri, G. & Cerutti, A. Intestinal IgA production and its role in host-microbe interaction. Immunological Reviews 260, 76–85 (2014).
Fransen, F. et al. BALB/c and C57BL/6 Mice Differ in Polyreactive IgA Abundance, which Impacts the Generation of Antigen-Specific IgA and Microbiota Diversity. Immunity 43, 527–540 (2015).
Macpherson, A. J., Mccoy, K. D., Johansen, F. E. & Brandtzaeg, P. The immune geography of IgA induction and function. Mucosal Immunology 1, 11–22 (2008).
Yan, F. & Polk, D. B. Lactobacillus rhamnosus GG: An Updated Strategy to Use Microbial Products to Promote Health. Functional Food Reviews 4, 77–84 (2012).
Wang, Y. et al. An LGG-derived protein promotes IgA production through upregulation of APRIL expression in intestinal epithelial cells. Mucosal Immunology. 7, 10.1038/mi.2016.57 (2016).
Wang, L. et al. Activation of epidermal growth factor receptor mediates mucin production stimulated by p40, a Lactobacillus rhamnosus GG-derived protein. Journal of Biological Chemistry 289, 20234–20244 (2014).
Yu, J. Y. et al. Mucin2 is required for probiotic agents-mediated blocking effects on meningitic E. coli-induced pathogenicities. Journal of Microbiology & Biotechnology 25, 10.4014/jmb.1502.02010 (2015).
Yu, J. Y. et al. Repositioning of Memantine as a Potential Novel Therapeutic Agent against Meningitic E. coli-Induced Pathogenicities through Disease-Associated Alpha7 Cholinergic Pathway and RNA Sequencing-Based Transcriptome Analysis of Host Inflammatory Responses. Plos One 10, 10.1371/journal.pone.0121911 (2015).
Dalgakiran, F., Witcomb, L. A., Mccarthy, A. J., Birchenough, G. M. & Taylor, P. W. Non-Invasive Model of Neuropathogenic Escherichia coli Infection in the Neonatal Rat. Journal of Visualized Experiments Jove 92, e52018–e52018 (2014).
Wang, H. et al. Pro-inflammatory miR-223 mediates the cross-talk between the IL23 pathway and the intestinal barrier in inflammatory bowel disease. Genome Biology 17, 1–15 (2016).
Reid, W. C. et al. Characterization of neuropathology in the HIV-1 transgenic rat at different ages. Journal of Neuroimmunology 292, 116–125 (2016).
Acknowledgements
This project was financially supported by the Grant from School of Public Health of Southern Medical University, China (Grant No. GW201601).
Author information
Authors and Affiliations
Contributions
H.C., S.H., X.H., S.P. and Q.Z. conceived and designed the experiment, X.H., Q.Z., J.Q., L.D., D.C. and T.W. performed the experiment, X.H., Q.Z., S.P., J.Q., L.D., D.C., T.W., Z.Z. and W.Y. analyzed the data, S.H. contributed reagents/materials/analysis tools, X.H., Q.Z., S.P., S.B., W.Y. and H.C. participated in its design and coordination and helped to draft the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing financial interests.
Rights and permissions
This work is licensed under a Creative Commons Attribution 4.0 International License. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in the credit line; if the material is not included under the Creative Commons license, users will need to obtain permission from the license holder to reproduce the material. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/
About this article
Cite this article
He, X., Zeng, Q., Puthiyakunnon, S. et al. Lactobacillus rhamnosus GG supernatant enhance neonatal resistance to systemic Escherichia coli K1 infection by accelerating development of intestinal defense. Sci Rep 7, 43305 (2017). https://doi.org/10.1038/srep43305
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/srep43305
This article is cited by
-
Effects of dietary Lactobacillus rhamnosus GG supplementation on the production performance, egg quality, eggshell ultrastructure, and lipid metabolism of late-phase laying hens
BMC Veterinary Research (2023)
-
In Vitro and In Vivo Evaluation of Lacticaseibacillus rhamnosus GG and Bifidobacterium lactis Bb12 Against Avian Pathogenic Escherichia coli and Identification of Novel Probiotic-Derived Bioactive Peptides
Probiotics and Antimicrobial Proteins (2022)
-
Postbiotics-parabiotics: the new horizons in microbial biotherapy and functional foods
Microbial Cell Factories (2020)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.