Abstract
The association of female reproductive factors (FRFs) with cardiovascular risk factors among different population was variable and inconsistent. The objective of this study was to examine the association between FRFs and hypertension, type 2 diabetes mellitus (DM), and long heart-rate-corrected QT interval (LQTc) in Chinese post-menopausal women (Post-MW). A total of 8046 Post-MW from the China Chaoshan Biobank Cohort Study were included for analysis. Logistic regression and general linear regression models were used to estimate the association between FRFs and hypertension, DM, and LQTc. Compared with women with 0 or 1 live birth, increasing risk of hypertension (odds ratio [OR], 1.51; 95% confidence interval [CI], 1.16–1.96), DM (OR, 1.65; 95% CI, 1.22–2.22), and LQTc (OR, 1.45; 95% CI, 1.01–2.09) were observed in women who had five or more live births. Further analysis demonstrated that the association between parity and hypertension, DM, and LQTc was mediated by lifestyle and dyslipidemia. Women with more live births had increased body mass index and waist circumstance, and were inclined to consume more salty food, animal fat, and alcohol, but less meat, vegetable, fish, plant oil, and tea, compared with that had fewer live births (all P < 0.05).
Similar content being viewed by others
Introduction
Cardiovascular disease (CVD) is increasing rapidly worldwide, especially in developing countries1. In China, CVD is now one of the leading causes of death2. CVD tends to develop about 10 years later in women than in men, with a marked increase after menopause, regardless the age at which menopause occurs3. The most important hormonal change after menopause is the decrease of estrogen4, which could influence the risk of CVD through lipid and carbohydrate metabolism, coagulation parameters, blood pressure and so on5.
Premature menopause has been associated with elevated CVD risk6. Observational studies show that Post-MW using hormone replacement therapy (HRT) has a greatly reduced risk of CVD7. However, some large clinical randomized controlled trials found that HRT failed to decrease the risk of CVD8. Studies that explored the role of surrogate measures of endogenous estrogen, such as parity9,10 and age at menarche11,12, on risk of CVD also provided conflicting conclusion. Interpretations of these conflicting studies are complicated by varying control for ethnicity, socioeconomic status (SES), lifestyle, and other potentially confounding factors.
Hypertension, type 2 diabetes mellitus (hereafter referred to as diabetes mellitus, DM), and long heart-rate-corrected QT (QTc) interval (LQTc)13 are the established cardiovascular risk factors (CRFs) and associated with increased CVD morbidity and mortality. However, limited studies have comprehensively examined the long-term effects of reproductive history on these CRFs in Chinese women after menopause. In this paper, we took advantage of the China Chaoshan Biobank Cohort Study to examine the relationship between female reproductive factors (FRFs) and hypertension, DM, and LQTc in Post-MW. Age at menarche and menopause, parity, way of menopause, and menstrual cycle length, bleeding duration in reproductive age are the major components of FRFs in our study.
Results
A total of 8046 Post-MW (natural menopause 7480, 93%; surgical menopause 566, 7%) were included in this study. Baseline characteristics of subjects are shown in Table 1. The overall prevalence of hypertension, DM, and LQTc among Post-MW of south China were 54.59%, 19.37%, and 9.26%, respectively, and it increased with age (Table 2).
Association of FRFs with hypertension, DM, and LQTc
After adjusting for SES and family history of hypertension and DM, multi-party was positive associated with hypertension, DM, and LQTc. Compared with women with 0 or 1 live birth, increasing risk of hypertension (OR, 1.51; 95% CI, 1.16–1.96), DM (OR, 1.65; 95% CI, 1.22–2.22), and LQTc (OR, 1.45; 95% CI, 1.01–2.09) were observed in women who had five or more live births. Other FRFs had no association with hypertension, DM, and LQTc (see Supplementary Table S1).
In model 2, we additionally adjusted for personal hobbies and dietary habits, and found the associations between parity and hypertension, LQTc was attenuated and no longer statistically significant. Often eating meat (OR, 1.29; 95% CI, 1.07–1.57) were positive associated with hypertension, while often eating fish (OR, 0.79; 95% CI, 0.64–0.96) decreased the risk of hypertension. Tea (OR, 1.48; 95% CI, 1.07–2.05) and alcohol (OR, 0.12; 95% CI, 0.02–0.91) consumption was positive and inversely associated with increased LQTc. Multi-party was still positively associated with DM (P = 0.001). Often eating meat (OR, 1.34; 95% CI, 1.09–1.65) also increased the risk of DM. Smoking had no association with hypertension, DM, and LQTc (see Supplementary Table S2).
In model 3, we further adjusted body mass index (BMI), waist circumference (WC), blood lipids, and uric acid (UA) on the basis of model 2. In this model, the association between parity and DM was attenuated and no longer statistically significant. Higher BMI, WC, total cholesterol (TC), triglycerides (TG), and UA were positive associated with hypertension. Higher WC, TG, and lower high-density lipoprotein cholesterol (HDL-C) were positive associated with DM (see Supplementary Table S3).
Table 3 provides a summary of the results of logistic regression analysis (here we just listed the associations between parity and hypertension, DM, and LQTc, for other FRFs had no association with these CRFs). Decreasing trends of the association between parity and hypertension (model 1: P = 0.004, model 2: P = 0.060, and model 3: P = 0.196), DM (model 1: P < 0.0001, model 2: P = 0.001, and model 3: P = 0.057), and LQTc (model 1: P = 0.047, model 2: P = 0.067, and model 3: P = 0.075) were shown from model 1 to model 3.
Association of parity with hypertension, DM, and LQTc
For other FRFs had no association with hypertension, DM, and LQTc, in this section, we just analyzed the association of parity with hypertension, DM, LQTc, and related risk factors. Women with more live births were older at enrollment and had later age at menarche and higher percentage of natural menopause (all P < 0.0001) than those with fewer live births (Table 4). Though women with more live births had lower percentage of family history of hypertension and DM, they still had higher prevalence of hypertension and DM (all P < 0.0001). The prevalence of LQTc also increased with parity (P < 0.0001). As for personal hobbies, multi-parity women were more likely to smoke (P < 0.0001) and drink (P = 0.021), but consumed less tea (P < 0.0001). Regarding dietary habits, multi-parity women were inclined to eat more salty food and animal fat, but less meat, vegetable, fish, and plant oil (all P < 0.0001).
General linear regression (Table 5) showed that parity were positively associated with BMI (P < 0.0001), WC (P < 0.0001), systolic blood pressure (SBP, P < 0.0001), diastolic blood pressure (DBP, P < 0.0001), fasting blood glucose (FBG, P < 0.0001), low-density lipoprotein cholesterol (LDL-C, P < 0.0001), TG (P < 0.05), and QTc (P = 0.041), and inversely associated with TC (P < 0.0001), HDL-C (P < 0.05), and UA (P < 0.05), after adjustment for confounders.
Discussion
Using data from the China Chaoshan Biobank Cohort Study, we observed that the prevalence of hypertension (54.59%) and DM (19.37%) in this Post-MW was higher than that reported for women in other regions of China14,15. The most possible reason is that the participants in this study were older than those in other studies.
Menarche and menopause are two landmarks in a woman’s reproductive life. Age at menarche and menopause has been showed associated with cardiovascular risk16,17,18. In our study, after adjusting for SES and other FRFs, age at menarche and menopause had no association with hypertension, DM, and LQTc. Study conduct in Fujian19 of China also showed that no significant associations were found between age at menarche and menopause with diabetes. UK Biobank Study20 demonstrated that being multiple birth and premature menarche are associated with premature menopause. We found that parity was positively and negatively correlated with age at menarche and menopause respectively. The effect of age at menarche or menopause on cardiovascular risk may be affected by other factors.
Post-MW with a history of irregular menstrual cycle has been reported had more indications of CVD and were more at risk of suffering cardiovascular events and death21. But the association between menstrual irregularity and CRFs in our study is not significant. The possible explanation may be that our cohort recruited general Post-MW and irregular cycles are not very common and severity among them.
Compared with natural menopause women, that with surgical menopause at same ages has greater risk of CVD6. Women with surgical menopause in our cohort account for 7.0%, and way of menopause (natural or surgical) have no association with CRFs. Our results inconsistent with previous study probably because that surgical menopause woman only account for a small amount of the study population and had little effect on the results. Further studies of large population or case-control design are warranted.
Repeated pregnancies and deliveries may aggravate the strain to cardiovascular system in women with multi-parity22. Study conducted in Hubei23 and Guangzhou24 of China showed that multi-parity was associated with increasing risk of metabolic syndrome (MetS). In the present study, multi-parity was associated with increased risk of hypertension and DM. But after further adjusting for dietary habits, WC, BMI, blood lipid, and UA, the association between parity and CRFs was eliminated, suggesting these associations was mediate in part by biological changes and lifestyle factors. The average pregnancy weight gain (17.1 ± 4.9 kg) among Chinese women25 was much higher than the recommended26. Our study also showed that BMI and WC increased with parity. Body composition indices (WC or BMI) had been discovered to predict MetS in Chinese Post-MW27.
Whole plant foods diet is associated with decreased menopausal symptoms in Post-MW with hypertension28. Our study showed that women with 5 or more live births usually eat less meat, vegetable, fish, and plant oil, but more salty food and animal fat than women with fewer live births. Dietary and lifestyle influence the onset of menopause and reproductive span29. Healthful eating choices play a protective role in reducing the risk of developing diabetes in Post-MW30. Halland et al. also suggests that higher cardiovascular mortality associated with multi-parity is caused by accumulation of negative lifestyle factors31.
Ventricular arrhythmias are the main cause of sudden cardiac death32. An important cause of ventricular arrhythmia is prolongation of ventricular repolarization, which is reflected by a longer QT interval on electrocardiogram33. The prevalence of LQTc and mean QTc increased with parity in the present study. Further analysis adjusting for alcohol and tea consumption found that the association between parity and LQTc was attenuated. Alcohol consumption inversely associated with increased risk of LQTc, consistent with previous studies in the West showing that moderate alcohol use is associated with a lower risk of CVD34. Increased tea consumption has been found with a reduced risk of cardiovascular outcomes and total mortality35. Epigallocatechin-3-gallate (EGCG), major catechin of green tea, could slightly shorten the QT interval in animal model36. However, tea consumption was positive associated with increased risk of LQTc in our study. This is probably because first, the difference between animal and human heart; second, oolong tea is the most widely consumed tea in our study population, which different from green and black tea37.
The strengths of this study are the large population-based material of Post-MW. Although previous studies on FRFs mostly focused on menopause, menarche or parity, we tried to balance that inadequacy by adding menstrual cycle characteristics, way of menopause and analyzed the aforementioned synthetically. We also included careful control of abundant potential confounders in multivariate models to reduce residual confounding, which may not have been considered adequately in previous studies. Previous research on QT interval mainly focused on men, women of reproductive age or animal model, our study first analyzed LQTc in Post-MW.
There are also some limitations to our study. First, information on FRFs was self-reported and therefore misclassification is inevitable. This would tend to attenuate the observed relation between FRFs and CRFs. Second, because of the differences of regions and cultures, the results of our study cannot be automatically generalized to other population.
In summary, our study suggested that multi-parity is associated with increased risk of hypertension, DM, and LQTc. Lifestyle and dyslipidemia may play an important role in the association. Thus, prevention of CRFs in Post-MW should rely on fitness, health dietary, and treatment of hyperlipidaemia. Further studies that include more comprehensive confounders are needed to explore the unclear mechanism underlying the link between FRFs and CRFs or CVD.
Methods
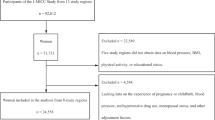
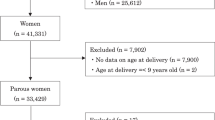
China Chaoshan Biobank Cohort Study
The China Chaoshan Biobank Cohort Study is a large ongoing prospective, community-based study designed to investigate the prevalence of chronic non-communicable diseases and its related risk factors in south China. The study initiated in 2012 by the First Affiliated Hospital of Shantou University Medical College. Ethics approval was obtained from the Ethics Committee of the First Affiliated Hospital of Shantou University Medical College. All methods were performed in accordance with the community monitoring guidelines and regulations of the First Affiliated Hospital of Shantou University Medical College.
All participants gave informed consent prior to the study. As of December 2015, a total of 22303 participants were included in the present cohort. 8046 Post-MW from the cohort was included for the present analysis. Women who received HRT, were pregnant, had malignant tumors, or mental disorders were excluded from the study.
Assessment of hypertension, DM, and LQTc
Hypertension was defined as systolic blood pressure (SBP) ≥140 mmHg, and/or diastolic blood pressure (DBP) ≥90 mmHg, and/or use of antihypertensive medications38. Type 2 diabetes mellitus was defined as fasting blood glucose (FBG) ≥7 mmol/L (126 mg/dL) and/or being on treatment for diabetes39.
Resting heart rates and QT intervals were obtained from the electrocardiograms (ECGs). QT corrected for the length of the previous cycle (QTc) was obtained using Bazett’s formulae40. QTc ≥460 ms was defined as abnormally prolonged.
Assessment of female reproductive factors
Postmenopausal was defined as lack of menstrual bleeding for at least 12 months or a history of hysterectomy and oophorectomy41. Age at menarche and menopause was retrospectively assigned as the self-reported age at the first and last menstrual period. Menstrual cycle length in reproductive age was referred as the number of days from the start of one bleeding period through the day before the start of the next menses. Bleeding duration in reproductive age was referred as the number of days from the start of one menstrual bleeding period through the last day of bleeding. The number of live births was referred to as parity in this paper. The ways of menopause include natural and surgical ways.
Assessment of covariates
Standing height, weight, WC, TC, LDL-C, HDL-C, TG, and UA were obtained from the medical examination. BMI was defined as weight (kg)/height2 (m2). BMI and WC were divided into three groups according to the guidelines for prevention and control of overweight and obesity in Chinese adults42.
Age at enrollment, marital status, occupational type, highest educational attainment, personal and family medical history (including hypertension and diabetes), FRFs, personal hobbies (smoking, alcohol and tea consumption), and dietary habits were collected via questionnaire-based interview. Family medical history included diseases in first-degree relatives including parents, offspring, and siblings. Dietary habits include the eating frequency (sometimes and often) of meat, viscus, vegetable, fish, salty food, plant oil, and animal fat. Current smoking was defined as smoking at least once a day over a period of more than half a year. Current alcohol and tea consumption was defined as drinking alcohol or tea once a week for a period of more than half a year.
Statistical analysis
All statistical analyses were performed in SPSS 19.0 (IBM Corp© 2010) and the probability level accepted for significance was P < 0.05.
Logistic regressions were used to examine the associations between FRFs and hypertension, DM, and LQTc. Results are presented as odds ratios (ORs) with 95% confidence intervals (CIs).
The differences among subjects in different groups were detected using the Kruskal-Wallis test for continuous variables and the χ2 test for categorical variables. A post hoc test using Bonferroni correction was applied, given that the overall test was significant (P < 0.05). Continuous variables were summarized by medians with interquartile ranges (IQRs) (the range between the 25th and 75th percentile). Categorical variables were expressed by percentages.
General linear regression models were created to examine the association of continuous parity (exposure) with each measure of cardiovascular risk factors (outcome variables). Results are presented as least square means (LSMs) with 95% CIs and P values comparing differences across parity were obtained from the models.
Additional Information
How to cite this article: Xu, B. et al. Association of Female Reproductive Factors with Hypertension, Diabetes and LQTc in Chinese Women. Sci. Rep. 7, 42803; doi: 10.1038/srep42803 (2017).
Publisher's note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
Murray, C. J. & Lopez, A. D. Measuring the global burden of disease. N Engl J Med 369, 448–457 (2013).
He, J. et al. Major causes of death among men and women in China. N Engl J Med 353, 1124–1134 (2005).
Lloyd-Jones, D. et al. Heart disease and stroke statistics—2010 update: a report from the American Heart Association. Circulation 121, e46–e215.
de Kleijn, M. J., van der Schouw, Y. T. & van der Graaf, Y. Reproductive history and cardiovascular disease risk in postmenopausal women: a review of the literature. Maturitas 33, 7–36 (1999).
Rackley, C. E. Hormones and coronary atherosclerosis in women. Endocrine 24, 245–250 (2004).
Atsma, F., Bartelink, M. L., Grobbee, D. E. & van der Schouw, Y. T. Postmenopausal status and early menopause as independent risk factors for cardiovascular disease: a meta-analysis. Menopause 13, 265–279 (2006).
Grodstein, F. et al. A prospective, observational study of postmenopausal hormone therapy and primary prevention of cardiovascular disease. Ann Intern Med 133, 933–941 (2000).
Anderson, G. L. et al. Effects of conjugated equine estrogen in postmenopausal women with hysterectomy: the Women’s Health Initiative randomized controlled trial. JAMA 291, 1701–1712 (2004).
Steenland, K., Lally, C. & Thun, M. Parity and coronary heart disease among women in the American Cancer Society CPS II population. Epidemiology 7, 641–643 (1996).
Shen, L. et al. Parity and Risk of Coronary Heart Disease in Middle-aged and Older Chinese Women. Sci Rep 5, 16834 (2015).
Mueller, N. T. et al. Age at menarche and cardiovascular disease mortality in Singaporean Chinese women: the Singapore Chinese Health Study. Ann Epidemiol 22, 717–722 (2012).
Charalampopoulos, D., McLoughlin, A., Elks, C. E. & Ong, K. K. Age at menarche and risks of all-cause and cardiovascular death: a systematic review and meta-analysis. Am J Epidemiol 180, 29–40 (2014).
Zhang, Y. et al. Sex-steroid hormones and electrocardiographic QT-interval duration: findings from the third National Health and Nutrition Examination Survey and the Multi-Ethnic Study of Atherosclerosis. Am J Epidemiol 174, 403–411 (2011).
Xu, B., Xu, Z., Xu, X., Cai, Q. & Xu, Y. Prevalence, awareness, treatment, and control of hypertension among residents in Guangdong Province, China, 2004 to 2007. Circ Cardiovasc Qual Outcomes 6, 217–222 (2013).
Ruan, Y. et al. Epidemiology of Diabetes in Adults Aged 35 and Older from Shanghai, China. Biomed Environ Sci 29, 408–416 (2016).
Zhou, Y. et al. Prevalence and risk factors of hypertension among pre- and post-menopausal women: a cross-sectional study in a rural area of northeast China. Maturitas 80, 282–287 (2015).
Yan, F. et al. Association of the Number of Years Since Menopause with Metabolic Syndrome and Insulin Resistance in Chinese Urban Women. J Womens Health (Larchmt) 24, 843–848 (2015).
Yang, A. et al. Reproductive factors and risk of type 2 diabetes in an occupational cohort of Chinese women. J Diabetes Complications 30, 1217–1222 (2016).
Qiu, C. et al. Associations between age at menarche and menopause with cardiovascular disease, Biobank Study. Sci Rep 6, 24710 (2016).
Ruth, K. S. et al. Events in Early Life are Associated with Female Reproductive Ageing: A UK Biobank Study. Sci. Rep. 6, 24710 (2016).
Wang, E. T. et al. Menstrual irregularity and cardiovascular mortality. J Clin Endocrinol Metab 96, E114–118 (2011).
Grundy, E. & Tomassini, C. Fertility history and health in later life: a record linkage study in England and Wales. Soc Sci Med 61, 217–228 (2005).
Wu, J. et al. Parity and risk of metabolic syndrome among Chinese women. J Womens Health (Larchmt) 24, 602–607 (2015).
Lao, X. Q. et al. Parity and the metabolic syndrome in older Chinese women: the Guangzhou Biobank Cohort Study. Clin Endocrinol (Oxf) 65, 460–469 (2006).
Wang, W. P. et al. [Gestational weight gain and its relationship with the birthweight of offspring]. Zhonghua Fu Chan Ke Za Zhi 48, 321–325 (2013).
Wong, W., Tang, N. L., Lau, T. K. & Wong, T. W. A new recommendation for maternal weight gain in Chinese women. J Am Diet Assoc 100, 791–796 (2000).
Ruan, X. et al. The prevalence of metabolic syndrome in Chinese postmenopausal women and the optimum body composition indices to predict it. Menopause 17, 566–570 (2010).
Liu, Z. M., Ho, S. C., Xie, Y. J. & Woo, J. Whole plant foods intake is associated with fewer menopausal symptoms in Chinese postmenopausal women with prehypertension or untreated hypertension. Menopause 22, 496–504 (2015).
Dorjgochoo, T. et al. Dietary and lifestyle predictors of age at natural menopause and reproductive span in the Shanghai Women’s Health Study. Menopause 15, 924–933 (2008).
Qiao, Y. et al. Racial/ethnic disparities in association between dietary quality and incident diabetes in postmenopausal women in the United States: the Women’s Health Initiative 1993–2005. Ethn Health 19, 328–347 (2014).
Halland, F. et al. Association of Women’s Reproductive History With Long-term Mortality and Effect of Socioeconomic Factors. Obstet Gynecol 126, 1181–1187 (2015).
Josephson, M. & Wellens, H. J. Implantable defibrillators and sudden cardiac death. Circulation 109, 2685–2691 (2004).
Straus, S. M. et al. Prolonged QTc interval and risk of sudden cardiac death in a population of older adults. J Am Coll Cardiol 47, 362–367 (2006).
Ronksley, P. E., Brien, S. E., Turner, B. J., Mukamal, K. J. & Ghali, W. A. Association of alcohol consumption with selected cardiovascular disease outcomes: a systematic review and meta-analysis. BMJ 342, d671 (2011).
Zhang, C. et al. Tea consumption and risk of cardiovascular outcomes and total mortality: a systematic review and meta-analysis of prospective observational studies. Eur J Epidemiol 30, 103–113 (2015).
Kang, J., Cheng, H., Ji, J., Incardona, J. & Rampe, D. In vitro electrocardiographic and cardiac ion channel effects of (-)-epigallocatechin-3-gallate, the main catechin of green tea. J Pharmacol Exp Ther 334, 619–626 (2010).
Cheng, T. O. All teas are not created equal: the Chinese green tea and cardiovascular health. Int J Cardiol 108, 301–308 (2006).
Mancia, G. E. A. 2013 Practice guidelines for the management of arterial hypertension of the European Society of Hypertension (ESH) and the European Society of Cardiology (ESC): ESH/ESC Task Force for the Management of Arterial Hypertension. J Hypertens 31, 1925–1938 (2013).
Ryo, M. & Funahashi, T. [Global diagnosis definition of the metabolic syndrome and its management]. Nihon Rinsho 64 Suppl 9, 463–469 (2006).
Bazett, H. An analysis of the time relationship of electrograms. Heart 7, 353–370 (1920).
Greendale, G. A., Lee, N. P. & Arriola, E. R. The menopause. Lancet 353, 571–580 (1999).
Chen, C., Lu, F. C. & Department of Disease Control Ministry of Health, P. R. C. The guidelines for prevention and control of overweight and obesity in Chinese adults. Biomed Environ Sci 17 Suppl, 1–36 (2004).
Acknowledgements
This study was supported by Shantou University Medical College Clinical Research Enhancement Initiative. We thank all study participants and colleagues of the Department of Community Monitoring of the First Affiliated Hospital of Shantou University Medical College, for their generous help.
Author information
Authors and Affiliations
Contributions
B.X. and X.T. conceived the research question. Y.C. and J.X. carried out the analysis. B.X. completed the first draft of the manuscript. N.L. interpreted and analyzed the ECG data. All authors reviewed the manuscript and approved the final version.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing financial interests.
Supplementary information
Rights and permissions
This work is licensed under a Creative Commons Attribution 4.0 International License. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in the credit line; if the material is not included under the Creative Commons license, users will need to obtain permission from the license holder to reproduce the material. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/
About this article
Cite this article
Xu, B., Chen, Y., Xiong, J. et al. Association of Female Reproductive Factors with Hypertension, Diabetes and LQTc in Chinese Women. Sci Rep 7, 42803 (2017). https://doi.org/10.1038/srep42803
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/srep42803
This article is cited by
-
Parity and incident type 2 diabetes in older Chinese women: Guangzhou Biobank Cohort Study
Scientific Reports (2023)
-
Screening for chronic conditions with reproductive factors using a machine learning based approach
Scientific Reports (2020)
-
Does parity matter in women’s risk of dementia? A COSMIC collaboration cohort study
BMC Medicine (2020)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.