Abstract
The prognostic role of N-terminal pro-brain natriuretic peptide (NT-proBNP) in the general population remains controversial. We conducted this meta-analysis to investigate the association between baseline NT-proBNP concentrations and cardiovascular or all-cause mortality in the general population. PubMed and Embase databases were systematically searched from their inception to August 2016. Prospective observational studies that investigated the association between baseline NT-proBNP concentrations and cardiovascular or all-cause mortality in the general population were eligible. A summary of the hazard ratio (HR) and 95% confidence interval (CI) of mortality were calculated by the highest versus the lowest category of NT-proBNP concentrations. Eleven studies with a total of 25,715 individuals were included. Compared individuals in the highest with those in the lowest category of NT-proBNP, the pooled HR was 2.44 (95% CI 2.11–2.83) for all-cause mortality, 3.77 (95% CI 2.85–5.00) for cardiovascular mortality, and 2.35 (95% CI 1.45–3.82) for coronary heart disease mortality, respectively. Subgroup analyses indicated that the effects of NT-proBNP on the risk of cardiovascular mortality (RR 2.27) and all-cause mortality (RR 3.00) appeared to be slightly lower among men. Elevated NT-proBNP concentrations appeared to be independently associated with increased risk of cardiovascular and all-cause mortality in the general population.
Similar content being viewed by others
Introduction
N-terminal pro-brain natriuretic peptide (NT-proBNP) is a prohormone with a 76 amino acid N-terminal inactive protein that is cleaved from the molecule to release brain natriuretic peptide (BNP)1. BNP and NT-proBNP are synthesized in response to ventricular stretch and ischemic injury2. Measurement of circulating BNP and NT-proBNP concentrations have been recommended in the diagnosis and management of heart failure3,4. Determining the NT-proBNP concentrations is recommended because of its more stable form and longer half-life5. Even in the absence of heart failure, elevated circulating NT-proBNP concentrations have also emerged as a serologic marker for the assessment of cardiovascular disease6.
Numerous studies have assessed the predictive value of circulating NT-proBNP concentrations in the general population7,8,9,10,11,12,13,14,15. However, the role of NT-proBNP as a predictor of mortality in the general population is conflicting16,17. In addition, the magnitude of the association between elevated NT-proBNP concentrations and risk of mortality varied across studies due to distinct study designs and studied populations. Currently, no previous a meta-analysis has evaluated this association in the general population. We therefore performed the current meta-analysis of the available prospective observational studies to investigate the association between baseline NT-proBNP concentrations and cardiovascular or all-cause mortality in the general population.
Results
Literature search and study characteristics
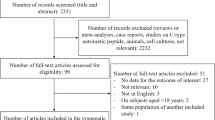
The initial electronic search yielded 828 citations. After screening the titles and abstracts, 66 articles were reviewed for more detailed evaluation, and 55 articles were further excluded mainly due to participants from a high cardiovascular risk or preexisting disease population. Finally, 11 studies7,8,9,10,11,12,13,14,15,16,17 were selected in this meta-analysis. The flow chart of the study selection is shown in Fig. 1.
The main characteristics of the included studies are summarized in Table 1. The included studies were published from 2005 to 2016. Of 11 studies, six studies7,8,9,12,14,16 were conducted in Europe, three10,13,17 in the USA, and two in Asia11,15. Sample sizes ranged from 506 to 11,193 with a total of 25,715 participants. Follow-up durations varied from 4.8 to 11.9 years. Three studies7,8,11 only consisted of men. All the included studies measured NT-proBNP concentrations by an electrochemiluminescence immunoassay performed on a Roche analyzer. The overall quality of most studies was high with NOS stars ranging from 5 to 8.
All-cause mortality
Data on all-cause mortality were available from 8 studies7,8,9,13,14,15,16,17. A total of 2,623 total death events were reported from 16,653 participants. As shown in Fig. 2, there was no evidence of significant heterogeneity across studies (I2 = 0%, p = 0.727). When compared with the lowest NT-proBNP concentrations, individuals with the highest NT-proBNP concentrations at baseline were significantly associated with an increased risk of all-cause mortality (HR 2.44; 95% CI 2.11–2.83) in a fixed-effect model. Evaluation of publication bias indicated that the both of Begg’s test (p = 0.266) and Egger’s test (p = 0.330) were not significant for the all-cause mortality. Sensitivity analyses showed that there were few changes in pooled risk estimates when any single study was removed at each turn.
Cardiovascular mortality
Eight studies8,9,10,11,12,13,14,16 provided the data on cardiovascular mortality. A total of 1,396 cardiovascular death events were reported from 22,887 participants. As shown in Fig. 3, a significant degree of study heterogeneity was noted (I2 = 45.4%, p = 0.076). When compared with the lowest NT-proBNP concentrations, individuals with the highest concentrations of NT-proBNP were associated with greater risk of cardiovascular mortality (HR 3.77; 95% CI 2.85–5.00) in a random-effects model. No evidence of publication bias was observed (p = 0.902 for Begg’s tests; p = 0.141 for Egger’s test).
Coronary heart disease (CHD) mortality
Data on CHD mortality were only available from 2 studies12,13. As shown in Fig. 4, there was no evidence of significant heterogeneity between two studies (I2 = 0%, p = 0.478). The pooled HR for mortality due to CHD was 2.35 (95% CI 1.45–3.82) in a fixed-effect model.
Subgroup analyses
Subgroup analyses indicated that the association between elevated NT-proBNP concentrations and risk of cardiovascular and all-cause mortality was consistently observed in each subgroup (Table 2). The risk of cardiovascular and all-cause mortality was higher in studies with a follow-up duration ≤5 years or mean age ≥70 years. The risk of cardiovascular and all-cause mortality was lower in studies enrolling only men or use of NT-proBNP cutoff value.
Discussion
NT-proBNP has been shown to predict poor prognosis in a variety of settings, including heart failure18, acute coronary syndromes19, stable coronary artery disease20, or stroke21. This meta-analysis goes beyond these established cardiovascular diseases and especially extends to the setting of the general population. The current meta-analysis demonstrates that elevated NT-proBNP concentrations appeared to be independently associated with increased risk for CHD, cardiovascular and all-cause mortality in the general population. Individuals in the highest NT-proBNP concentrations significantly increased 2.35-fold CHD mortality, 3.77-fold cardiovascular mortality, and 2.44-fold all-cause mortality after adjustment for other traditional risk factors.
Age, gender, renal impairment, and obesity may affect the circulating concentrations of NT-proBNP. NT-proBNP concentrations varied by the age of the study population11,22. This meta-analysis included studies spanning a wide range of age. Our subgroup analysis showed that the prognostic value of cardiovascular and all-cause mortality risk was stronger for participants with mean age ≥70 years than those with a mean age <70 years, particularly for cardiovascular mortality (RR 5.10 vs.3.40). Zhu et al.’s study15 also suggested that NT-proBNP concentrations were an independent predictor of all-cause mortality in participants with age >65 years but not age <65 years. Stratified analysis by gender showed that the effects of elevated NT-proBNP concentrations on cardiovascular and all-cause mortality risk appeared to be slightly lower in men than the both gender groups. This result may be explained by the women had significantly higher concentrations of NT-proBNP than the men23. Therefore, gender specific analysis of NT-proBNP concentrations on subsequent mortality risk is required in the future studies. In addition, the risk of cardiovascular and all-cause mortality was higher in studies with a follow-up duration ≤5 years than in those with >5 years of follow-up, suggesting death events mainly occured in the early follow-up duration.
NT-proBNP was at least partially cleared from the circulation by the kidney24. Circulating concentrations of NT-proBNP are typically higher in patients with chronic kidney disease (CKD) than in those without CKD25,26. Therefore, CKD may be an important confounding factor that affecting the association between NT-proBNP and mortality risk. However, our subgroup analysis revealed that whether adjustment for renal function was not found to significantly alter the prognostic value of the NT-proBNP. These findings suggested the association between NT-proBNP and mortality risk was independent of CKD.
Obesity must be taken into account for clinical interpretation of NT-proBNP. There was a paradoxical association between obesity and prognosis in patients with heart failure27. Overweight and obese adults had a lower NT-proBNP concentrations than those in the normal weight28,29. NT-proBNP concentrations appeared to be inversely correlated with obesity30. The inverse relationship between the NT-proBNP concentrations and body mass index (BMI) might be explained by an increase in the degradation of the adipose tissue peptide31. Therefore, obesity may have confounded the association of NT-proBNP concentrations with cardiovascular or all-cause mortality. However, we could not conduct a subgroup analysis by obesity (e.g. BMI ≥ 30 kg/m2 vs. BMI < 30 kg/m2) because the included studies did not report the risk estimate by the category of body weight. Future studies are recommended to report risk estimate of cardiovascular or all-cause mortality with the category of BMI or waist circumference.
Several studies also investigated the relationship between circulating NT-proBNP concentrations and mortality risk based on continuous data analysis. Per 1 SD or per 1 unit increase in log NT-proBNP concentrations was associated with an increase risk of cardiovascular and all-cause mortality after adjustment for other traditional risk factors32,33,34,35,36. In addition, individuals with increasing NT-proBNP concentrations (≥100%) also had markedly increased all-cause mortality compared with those with unchanged37,38. Findings in continuous NT-proBNP analysis further supported the prognostic value of NT-proBNP on the mortality risk.
Data on comparison of NT-proBNP relative to BNP concentrations as predictors of mortality in the general population were unavailable. NT-proBNP seemed to be superior to BNP for predicting cardiovascular events in the general population39 and patients with stable coronary heart disease40. This finding may be correlated to NT-proBNP has a longer half life than BNP and higher plasma concentrations41. Several possible mechanisms can explain the prognostic value of circulating NT-proBNP concentrations in the general population. First, higher NT-proBNP concentrations may reflect the presence of structural heart disease or cardiac remodeling resulting from increased cardiac stretch42. Second, elevated NT-proBNP concentrations may link with the degree of systemic atherosclerosis43.
Several potential limitations should be mentioned. First, circulating concentrations of NT-proBNP were determined at a single measurement at baseline and without observed the dynamic changes. The concentrations NT-proBNP could be changed by modifications in lifestyle or medication during the follow-up10 and misclassification of NT-proBNP category was possible. Therefore, NT-proBNP might not optimally stratify long-term clinical endpoints. Second, the findings from the subgroup analysis may be reliable because of the relatively small number of included studies analyzed. Third, the majority of the included studies pertained to the older participants; hence generalization of our findings to the middle-aged individuals might be limited. Fourth, results of publication bias may be unreliable mainly due to the studies’ number of cardiovascular and all-cause mortality was less than 10. Finally, as for the thresholds for higher concentrations of NT-proBNP markedly varied across studies, we were unable to define the optimal thresholds for NT-proBNP.
In conclusion, this meta-analysis suggests that individuals with elevated NT-proBNP concentrations appeared to be independently associated with an increased risk for CHD, cardiovascular and all-cause mortality in the general population. Future more well-designed prospective studies are necessary to investigate the gender-specific effects of NT-proBNP on mortality risk.
Methods
Search strategy
This meta-analysis was performed according to the guidelines of the Meta-analysis of Observational Studies in Epidemiology44. A systematic electronic literature search was conducted in PubMed and Embase databases from inception to August 2016 without restriction. The following search terms were used: N-terminal pro-brain natriuretic peptide OR NT-proBNP OR BNP AND “mortality” OR “death” AND “prospective studies” OR “longitudinal study” OR “follow-up”. Reference lists from identified studies were manually scanning to identify any additional articles.
Study selection
The eligible studies had to satisfy the following inclusion criteria:1) prospective observational design with participants in the general population (participants not from disease-specific populations); and 2) reported adjusted hazard ratio (HR) or risk ratio (RR) and corresponding 95% confidence interval (CI) of cardiovascular or all-cause mortality comparing the highest to the lowest category of baseline NT-proBNP concentrations. If multiple articles from the same population, the study with larger sample size and longer follow-up duration were selected. Exclusion criteria included: 1) participants from a high cardiovascular risk or preexisting disease population; 2) circulating BNP concentration as exposure; 3) only reported risk estimate based on continuous variable of NT-proBNP concentrations; and 4) conference abstracts, review, or case-control study.
Data extraction and quality assessment
Data extracted from each study included: first author’s surname, publication year, geographic region, study design, sample sizes, mean age or age range of the participants, gender, method of NT-proBNP detection, cutoff value of NT-proBNP, number of death events, fully adjusted HR with corresponding 95% CI, duration of follow-up, and degree of adjustment for potential confounders. Two independent authors (ZH Geng and L Huang) independently extracted the data. Disagreements were resolved by discussion or consensus from a third author (MB Song). If the original data were incomplete, the corresponding author was contacted by e-mail. Methodological quality was evaluated with the 9-star Newcastle-Ottawa Scale (NOS) for the cohort studies45. Domains of quality assessment included selection of the study groups, comparability of groups, and ascertainment of outcomes. If the studies achieved six stars or more, we grouped them as high quality.
Statistical analyses
The most fully adjusted HR or RR and 95% CI were used to calculate the pooled effects. HR and RR were assumed to approximate the same measure of the risk estimate. The pooled risk estimate was calculated by the highest versus the lowest category of NT-proBNP concentrations. Cochrane Q test and I2 statistics were used to measure the heterogeneity across studies. Statistically significant heterogeneity was defined as p < 0.10 for the Cochrane Q test and I2 > 50%. A random effect model was used when there was evidence of significant heterogeneity; otherwise, a fixed-effects model was utilized46. Subgroup analyses were conducted by the number of participants, region, duration of follow-up, and NOS scores. We conducted a sensitivity analysis to assess the robustness of the overall risk estimate by sequentially excluding a single study at each turn. Potential publication bias was evaluated using the Begg’s rank correlation test47 and Egger’s regression test48, with both P values > 0.10 considered as not significant. All analyses were performed with Stata software 12.0 (Stata, College Station, TX, USA).
Additional Information
How to cite this article: Geng, Z. et al. N-terminal pro-brain natriuretic peptide and cardiovascular or all-cause mortality in the general population: A meta-analysis. Sci. Rep. 7, 41504; doi: 10.1038/srep41504 (2017).
Publisher's note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
Yandle, T. G. & Richards, A. M. B-type Natriuretic Peptide circulating forms: Analytical and bioactivity issues. Clin Chim Acta 448, 195–205 (2015).
Daniels, L. B. & Maisel, A. S. Natriuretic peptides. J Am Coll Cardiol 50, 2357–68 (2007).
Maisel, A. S. et al. Rapid measurement of B-type natriuretic peptide in the emergency diagnosis of heart failure. N Engl J Med 347, 161–7 (2002).
Oremus, M. et al. A systematic review of BNP and NT-proBNP in the management of heart failure: overview and methods. Heart Fail Rev 19, 413–9 (2014).
Piechota, M., Banach, M., Jacon, A. & Rysz, J. Natriuretic peptides in cardiovascular diseases. Cell Mol Biol Lett 13, 155–81 (2008).
Di Angelantonio, E. et al. B-type natriuretic peptides and cardiovascular risk: systematic review and meta-analysis of 40 prospective studies. Circulation 120, 2177–87 (2009).
Kistorp, C. et al. N-terminal pro-brain natriuretic peptide, C-reactive protein, and urinary albumin levels as predictors of mortality and cardiovascular events in older adults. JAMA 293, 1609–16 (2005).
Laukkanen, J. A. et al. Plasma N-terminal fragments of natriuretic propeptides predict the risk of cardiovascular events and mortality in middle-aged men. Eur Heart J 27, 1230–7 (2006).
Zethelius, B. et al. Use of multiple biomarkers to improve the prediction of death from cardiovascular causes. N Engl J Med 358, 2107–16 (2008).
deFilippi, C. R., Christenson, R. H., Gottdiener, J. S., Kop, W. J. & Seliger, S. L. Dynamic cardiovascular risk assessment in elderly people. The role of repeated N-terminal pro-B-type natriuretic peptide testing. J Am Coll Cardiol 55, 441–50 (2010).
Doi, Y. et al. N-terminal pro-brain natriuretic peptide and risk of cardiovascular events in a Japanese community: the Hisayama study. Arterioscler Thromb Vasc Biol 31, 2997–3003 (2011).
Wannamethee, S. G. et al. N-terminal pro-brain natriuretic Peptide is a more useful predictor of cardiovascular disease risk than C-reactive protein in older men with and without pre-existing cardiovascular disease. J Am Coll Cardiol 58, 56–64 (2011).
Oluleye, O. W., Folsom, A. R., Nambi, V., Lutsey, P. L. & Ballantyne, C. M. Troponin T, B-type natriuretic peptide, C-reactive protein, and cause-specific mortality. Ann Epidemiol 23, 66–73 (2013).
van Peet, P. G., de Craen, A. J., Gussekloo, J. & de Ruijter, W. Plasma NT-proBNP as predictor of change in functional status, cardiovascular morbidity and mortality in the oldest old: the Leiden 85-plus study. Age (Dordr) 36, 9660 (2014).
Zhu, Q. et al. The prognostic value of the plasma N-terminal pro-brain natriuretic peptide level on all-cause death and major cardiovascular events in a community-based population. Clin Interv Aging 11, 245–53 (2016).
Marz, W. et al. N-terminal pro-B-type natriuretic peptide predicts total and cardiovascular mortality in individuals with or without stable coronary artery disease: the Ludwigshafen Risk and Cardiovascular Health Study. Clin Chem 53, 1075–83 (2007).
McKie, P. M. et al. The prognostic value of N-terminal pro-B-type natriuretic peptide for death and cardiovascular events in healthy normal and stage A/B heart failure subjects. J Am Coll Cardiol 55, 2140–7 (2010).
Yoo, B. S. Clinical Significance of B-type Natriuretic Peptide in Heart Failure. J Lifestyle Med 4, 34–8 (2014).
Zeng, X., Li, L. & Su, Q. The prognostic value of N-terminal pro-brain natriuretic peptide in non-ST elevation acute coronary syndromes: a meta-analysis. Clin Chem Lab Med 50, 731–9 (2012).
Wei, G., Yaqi, R., Ningfu, W. & Xuwei, H. N-terminal prohormone B-type natriuretic peptide and cardiovascular risk in stable coronary artery disease: a meta-analysis of nine prospective studies. Rev Cardiovasc Med 14, e92–8 (2013).
Garcia-Berrocoso, T. et al. B-type natriuretic peptides and mortality after stroke: a systematic review and meta-analysis. Neurology 81, 1976–85 (2013).
Clerico, A. et al. The circulating levels of cardiac natriuretic hormones in healthy adults: effects of age and sex. Clin Chem Lab Med 40, 371–7 (2002).
Galasko, G. I., Lahiri, A., Barnes, S. C., Collinson, P. & Senior, R. What is the normal range for N-terminal pro-brain natriuretic peptide? How well does this normal range screen for cardiovascular disease? Eur Heart J 26, 2269–76 (2005).
Schou, M. et al. Kidneys extract BNP and NT-proBNP in healthy young men. J Appl Physiol (1985) 99, 1676–80 (2005).
Wallen, T. et al. Brain natriuretic peptide in an elderly population. J Intern Med 242, 307–11 (1997).
DeFilippi, C., van Kimmenade, R. R. & Pinto, Y. M. Amino-terminal pro-B-type natriuretic peptide testing in renal disease. Am J Cardiol 101, 82–8 (2008).
Alagiakrishnan, K., Banach, M., Ahmed, A. & Aronow, W. S. Complex relationship of obesity and obesity paradox in heart failure - higher risk of developing heart failure and better outcomes in established heart failure. Ann Med 48, 603–613 (2016).
Mangge, H. et al. N-terminal pro-B-type natriuretic peptide in early and advanced phases of obesity. Clin Chem Lab Med 49, 1539–45 (2011).
Lorgis, L. et al. Impact of obesity on the prognostic value of the N-terminal pro-B-type natriuretic peptide (NT-proBNP) in patients with acute myocardial infarction. Heart 97, 551–6 (2011).
Zhu, W. H. et al. Correlation between B type natriuretic peptide and metabolic risk factors. Arch Med Sci 12, 334–40 (2016).
Daniels, L. B. et al. How obesity affects the cut-points for B-type natriuretic peptide in the diagnosis of acute heart failure. Results from the Breathing Not Properly Multinational Study. Am Heart J 151, 999–1005 (2006).
McKie, P. M. et al. Amino-terminal pro-B-type natriuretic peptide and B-type natriuretic peptide: biomarkers for mortality in a large community-based cohort free of heart failure. Hypertension 47, 874–80 (2006).
Daniels, L. B., Laughlin, G. A., Clopton, P., Maisel, A. S. & Barrett-Connor, E. Minimally elevated cardiac troponin T and elevated N-terminal pro-B-type natriuretic peptide predict mortality in older adults: results from the Rancho Bernardo Study. J Am Coll Cardiol 52, 450–9 (2008).
Everett, B. M., Ridker, P. M., Cook, N. R. & Pradhan, A. D. Usefulness of B-type Natriuretic Peptides to Predict Cardiovascular Events in Women (from the Women’s Health Study). Am J Cardiol 116, 532–7 (2015).
Welsh, P. et al. N-terminal pro-B-type natriuretic peptide and the prediction of primary cardiovascular events: results from 15-year follow-up of WOSCOPS. Eur Heart J 34, 443–50 (2013).
Dallmeier, D. et al. Sex-specific associations of established and emerging cardiac biomarkers with all-cause mortality in older adults: the ActiFE study. Clin Chem 61, 389–99 (2015).
Eggers, K. M., Venge, P. & Lind, L. Prognostic usefulness of the change in N-terminal pro B-type natriuretic peptide levels to predict mortality in a single community cohort aged >/=70 years. Am J Cardiol 111, 131–6 (2013).
Linssen, G. C. et al. N-terminal pro-B-type natriuretic peptide is an independent predictor of cardiovascular morbidity and mortality in the general population. Eur Heart J 31, 120–7 (2010).
Kara, K. et al. NT-proBNP is superior to BNP for predicting first cardiovascular events in the general population: the Heinz Nixdorf Recall Study. Int J Cardiol 183, 155–61 (2015).
Mishra, R. K. et al. B-type natriuretic peptides for the prediction of cardiovascular events in patients with stable coronary heart disease: the Heart and Soul Study. J Am Heart Assoc 3 (2014).
Panagopoulou, V. et al. NTproBNP: an important biomarker in cardiac diseases. Curr Top Med Chem 13, 82–94 (2013).
Nadir, M. A. et al. Improving the primary prevention of cardiovascular events by using biomarkers to identify individuals with silent heart disease. J Am Coll Cardiol 60, 960–8 (2012).
Senmaru, T. et al. N-terminal pro-brain natriuretic peptide could be a marker of subclinical atherosclerosis in patients with type 2 diabetes. Heart Vessels 28, 151–6 (2013).
Stroup, D. F. et al. Meta-analysis of observational studies in epidemiology: a proposal for reporting. Meta-analysis Of Observational Studies in Epidemiology (MOOSE) group. JAMA 283, 2008–12 (2000).
Wells, G. et al. The Newcastle–Ottawa Scale (NOS) for assessing the quality if nonrandomized studies in meta-analyses. http://www.ohri.ca/programs/clinical_epidemiology/oxford.asp (accessed March 6, 2016)
Higgins, J. P. T. & Green, S. e. Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 [updated March 2011]. The Cochrane Collaboration, 2011. Available from www.cochrane-handbook.org. (accessed March 9, 2016).
Begg, C. B. & Mazumdar, M. Operating characteristics of a rank correlation test for publication bias. Biometrics 50, 1088–101 (1994).
Egger, M., Davey Smith, G., Schneider, M. & Minder, C. Bias in meta-analysis detected by a simple, graphical test. BMJ 315, 629–34 (1997).
Author information
Authors and Affiliations
Contributions
Z.H. Geng and L. Huang made the literature research, extracted data, and performed the statistical analysis. MB Song evaluated the quality of the included study and drafted the manuscript. YM Song designed this study, interpreted the results, and revised the manuscript. All the listed authors reviewed and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing financial interests.
Rights and permissions
This work is licensed under a Creative Commons Attribution 4.0 International License. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in the credit line; if the material is not included under the Creative Commons license, users will need to obtain permission from the license holder to reproduce the material. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/
About this article
Cite this article
Geng, Z., Huang, L., Song, M. et al. N-terminal pro-brain natriuretic peptide and cardiovascular or all-cause mortality in the general population: A meta-analysis. Sci Rep 7, 41504 (2017). https://doi.org/10.1038/srep41504
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/srep41504
This article is cited by
-
NT-proBNP as a surrogate for unknown heart failure and its predictive power for peripheral artery disease outcome and phenotype
Scientific Reports (2023)
-
The abnormal distribution of peripheral B1 cells and transition B cells in patients with idiopathic dilated cardiomyopathy: a pilot study
BMC Cardiovascular Disorders (2022)
-
Cardiac biomarkers in pediatric CKD—a prospective follow-up study
Pediatric Nephrology (2022)
-
Urinary N-terminal pro–B-type natriuretic peptide as a biomarker for cardiovascular events in a general Japanese population: the Hisayama Study
Environmental Health and Preventive Medicine (2021)
-
Factors associated with non-invasive mechanical ventilation failure in patients with hematological neoplasia and their association with outcomes
Journal of Intensive Care (2020)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.