Abstract
The effect of hypoglycemia on the progression of atherosclerosis in patients with type 2 diabetes mellitus (T2DM) remains largely unknown. This is a post hoc analysis of a randomized trial to investigate the relationship between hypoglycemic episodes and changes in carotid intima-media thickness (IMT). Among 274 study subjects, 104 patients experienced hypoglycemic episodes. Increases in the mean IMT and left maximum IMT of the common carotid arteries (CCA) were significantly greater in patients with hypoglycemia compared to those without hypoglycemia. Classification of the patients into three groups according to the frequency of hypoglycemic episodes showed that high frequency of hypoglycemic events was associated with increases in mean IMT-CCA, and left max-IMT-CCA and right max-IMT-CCA. In addition, repetitive episodes of hypoglycemia were associated with a reduction in the beneficial effects of sitagliptin on carotid IMT. Our data suggest that frequency of hypoglycemic episodes was associated with changes in carotid atherosclerosis.
Similar content being viewed by others
Introduction
While type 2 diabetes mellitus (T2DM) is a risk factor for cardiovascular disease (CVD), which is one of the major causes of morbidity and mortality in these patients1, large randomized clinical trials did not show the benefits of strict glycemic control on CVD in patients with established atherosclerosis or longstanding T2DM2,3,4. On the other hand, a recent study reported that the occurrence of hypoglycemia was associated with increased risk of CVD and all-cause mortality in insulin-treated patients with type 1 diabetes mellitus (T1DM) and T2DM5.
Hypoglycemia is a common adverse effect of management for diabetes, especially insulin therapy, and a barrier to optimal glycemic control. Hypoglycemia affects blood constituents6,7, inflammatory cytokine levels8,9, and coagulation and fibrinolysis factors10,11, all of which might promote the progression of atherosclerosis. Indeed, the acute effects of hypoglycemia, such as sympatho-adrenal activation, catecholamine release on inflammation, endothelial injury, and pro-atherothrombotic biomarkers12,13, are well known in patients with T1DM. Also, a cross sectional study demonstrated that repeated episodes of hypoglycemia were associated with preclinical atherosclerosis evaluated by carotid and femoral echography and measurement of flow-mediated brachial dilatation in patients with T1DM14. However, the long-term effect of hypoglycemia on the progression of atherosclerosis remains largely unknown in patients with T2DM.
Sitagliptin, a dipeptidyl peptidase-4 (DPP-4) inhibitor, improves glycemic control without increasing the risk of hypoglycemia15,16. Recently, we reported that sitagliptin treatment attenuated the increases in carotid intima-media thickness (IMT) in insulin-treated patients with T2DM compared with the conventional treatment17. In the same study, we demonstrated that sitagliptin treatment was superior to conventional treatment in terms of HbA1c reduction without increasing the incidence of hypoglycemic episodes, consistent with previous studies18,19,20. However, we have not investigated whether hypoglycemic events are associated with a reduction in the beneficial effects of sitagliptin on the changes in carotid atherosclerosis.
The aim of the present post hoc-analysis was to investigate the relationship between hypoglycemic events and changes in carotid IMT in insulin-treated patients with T2DM.
Results
Participants
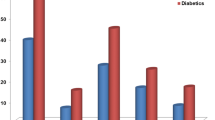
In the original study, 104 of 274 patients experienced hypoglycemia (52 of the sitagliptin group and 52 of the conventional group) over the 104 week follow-up. There was no significant differences in the mean number of hypoglycemic events between the two groups (0.34 ± 0.85 episodes/month/person in the sitagliptin group vs 0.36 ± 0.80 in the conventional group). One episode of severe hypoglycemic event occurred in each group. Subgroup analysis according to the occurrence of hypoglycemia showed that patients with hypoglycemia were older, had lower estimated glomerular filtration rate (eGFR) level, lower C-peptide level and had more frequent use of sulfonylurea and α-glucosidase inhibitors, but were more lean, less likely to be smokers, had lower HbA1c, total-cholesterol, triglyceride, hs-CRP (high-sensitivity C-reactive protein) and interleulin-6, and few use of glinides (Table 1).
Occurrence of hypoglycemia is associated with the changes in carotid IMT
Of the 274 patients in the original study, 243 patients with available carotid IMT data at baseline and 104 weeks were included in this post hoc analysis. Among them, 98 patients experienced hypoglycemia (49 of the sitagliptin group and 49 of the conventional group). In the analysis of covariance models that included the occurrence of hypoglycemia, age, gender, baseline IMT and the original treatment group (model 1), the changes in mean IMT of the common carotid arteries (mean-IMT-CCA) and left maximum IMT of the common carotid artery (max-IMT-CCA), but not right max-IMT-CCA, were significantly higher in patients with hypoglycemia than those without (Table 2). Similar findings were noted even in the adjusted models, including model 2 (model 1+ body mass index (BMI) + current smoking), model 3 (model 2 + HbA1c, total cholesterol, high density lipoprotein-cholesterol, triglyceride and systolic blood pressure), model 4 (model 3+ eGFR + angiotensin-converting enzyme inhibitors/angiotensin II receptor blocker, statins and anti-platelets), model 5 (model 4 + sulfonylurea + glinides + α-glucosidase inhibitors), and model 6 (model 5 + C-peptide + hsCRP + interleukin 6).
Next, we performed subgroup analysis according to type of treatment. As shown in Table 3, the mean-IMT-CCA was significantly increased relative to baseline in patients with hypoglycemia, but not in those without hypoglycemia in the conventional group. In addition, the changes in mean-IMT-CCA and left max-IMT-CCA tended to be greater in patients with hypoglycemia compared to those without. More importantly, in patients without hypoglycemia, the changes in mean-IMT-CCA and left max-IMT-CCA, but not right max-IMT-CCA, were significantly smaller in the sitagliptin treatment group than those in the conventional treatment group, while these findings were not observed in patients with hypoglycemia (Table 3). These data showed that hypoglycemia was associated with a reduction in the beneficial effects of sitagliptin.
Frequency of hypoglycemia is associated with changes in carotid IMT
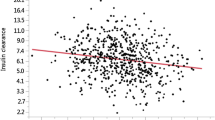
Next, to investigate the relationship between the frequency of hypoglycemia and changes in carotid IMT, we divided patients with the occurrence of hypoglycemia into three groups; patients without hypoglycemia, patients with less than 1 times/month hypoglycemia, and patients with more than 1 times/month hypoglycemia. Trend associations across three groups and changes in IMT were evaluated by univariate and multivariate linear regression analyses (Table 4). The frequency of hypoglycemia was associated with changes in mean-IMT-CCA and left max-IMT-CCA, but not right max-IMT-CCA in unadjusted model (model 1). Almost similar findings were noted even in the adjusted models, including model 2 (model 1 + baseline IMT), model 3 (model 2+ age + gender + the original treatment group), model 4 (model 3+ BMI + current smoking), model 5 (model 4 + HbA1c, total cholesterol, high density lipoprotein-cholesterol, triglyceride and systolic blood pressure), model 6 (model 5 + eGFR + angiotensin-converting enzyme inhibitors/angiotensin II receptor blockers, statins and anti-platelets), model 7 (model 6 + sulfonylurea + glinides + α-glucosidase inhibitors), and model 8 (model 7 + C-peptide + hsCRP + interleukin 6). In addition, analysis of data of the entire population showed that increased frequency of hypoglycemia was associated with changes in mean-IMT-CCA (P for difference among the three groups = 0.002), right max-IMT-CCA (P = 0.032), and left max-IMT-CCA (P = 0.02) (Fig. 1).
Changes in other parameters
The change in HbA1c (value at end of study - value at baseline) was comparable between the hypoglycemia group (−0.2 ± 0.9%) and no-hypoglycemia group (−0.4 ± 1.1%) (Supplementary Table 1). Similarly, there were no differences in changes in other risk factors for atherosclerosis such as hypertension and lipid parameters during the observation period (Supplementary Table 1).
Discussion
Hypoglycemia is a common adverse effect of insulin treatment for T2DM21. Previous studies demonstrated that the frequency of hypoglycemic episodes remains unacceptably high even when DPP-4 inhibitors are added to insulin therapy, although they did not increase the incidence of hypoglycemic episodes18,19,20. The same appears to be true in the present study. Indeed, the high frequency of hypoglycemic events is associated with increases in carotid atherosclerosis. Previous studies identified several factors, such as BP, BMI22 and lipid parameters23, but not hypoglycemic events, to be associated with the changes in carotid artery atherosclerosis in patients with T2DM. Thus, this was the first study to demonstrate that frequent episodes of hypoglycemia are associated with changes in carotid artery atherosclerosis in insulin-treated patients with T2DM.
While most clinical data showing associations between hypoglycemia and adverse CV risk/mortality risk have derived from “serious hypoglycemic” episodes24,25,26, the effect of mild hypoglycemia on adverse CV outcomes remains still unknown. On the other hand, virtually, this study showed the relation between frequency of mild hypoglycemia and changes in IMT because most of the hypoglycemic episodes were mild. In this regard, further prospective large sample size studies are required to address whether mild hypoglycemia is also associated with adverse CV risk/mortality risk
In this study, patients with hypoglycemia were older, suffered more severe renal dysfunction, had less endogenous insulin and more frequent use of sulfonylurea. Thus, it is possible that hypoglycemia is only a maker of patients with advanced stages of T2DM and/or those prone to CVD. However, the occurrence of hypoglycemia was still associated with the changes in carotid IMT even after adjustment for these confounders. Furthermore, the control of atherosclerosis risk factors was not consistently worse in patients with the occurrence of hypoglycemia because they were less obese, were less likely to be smokers, achieved better glycemic and lipid controls and had lower serum levels of inflammatory cytokines, reflecting patients who were at lower risk for CVD. Indeed, almost similar findings were observed in analysis of covariance models after adjustment for those confounding factors. These data support that hypoglycemia by itself seem to be a contributing factor for atherosclerosis.
The mechanism of the deleterious effect of hypoglycemia on carotid vascular wall may be multidimensional and possibly involves changes in blood constituents6,7, inflammation8,9, and coagulation and fibrinolysis10,11, through counter-regulatory defense responses to hypoglycemia. While these responses and changes are transient and play a crucial role in protecting vital organs, previous studies demonstrated that acute insulin-induced hypoglycemia can provoke inflammatory response, platelet aggregation and endothelial dysfunction in patients with T1DM12,27. Thus, the progression of atherosclerosis may be accelerated if hypoglycemic episodes occur frequently. However, repeated episodes of relatively mild hypoglycemia have been shown to reduce the counter-regulatory defense responses to hypoglycemia in intensive treatment of T2DM28. Nevertheless, at least in Goto-Kakizaki rats, diabetic model rats, these responses never disappear and enhance monocyte adhesion to endothelial cells in the aorta, leading to increased intimal thickening29. In agreement with this finding, our data demonstrated that changes in carotid atherosclerosis increased with increased number of hypoglycemic events.
What is the precise mechanism through which repeated episodes of hypoglycemia promote the progression of atherosclerosis? In the present study, we did not find any association between serum biomarkers of inflammation or endothelial injury and frequency of hypoglycemia or carotid IMT changes (data not shown). It is possible that this negative relationship may be due to several limiting features of such biomarkers. Indeed, the amount of such biomarkers is known to be affected by both transient and chronic non-atherosclerotic diseases and drug treatment within a relatively short time30. In the future, it would be interesting to determine whether repeated episodes of hypoglycemia could affect plaque characteristics of the carotid arteries evaluated by sophisticated studies such as Computed Tomography and Magnetic Resonance Imaging. These studies might shed light on pro-inflammatory effects of repetitive hypoglycemia on the vasculature. Another possibility is that hypoglycemia directly induced hypercatecholaminemia by acting on the vascular wall29,31. However, it is difficult to evaluate serum catecholamine levels during hypoglycemia in clinical setting. Further studies are required to clarify the mechanism of the influence of hypoglycemia on the vasculature.
It is reported that glucagon-like peptide-1 (GLP-1) attenuates hypoglycemia-induced oxidative stress, inflammation and endothelial dysfunction in patients with T1DM27. Therefore, there is a great interest in determining whether DPP-4 inhibitors play an important role in protecting against hypoglycemia-induced vascular damages. In this regard, our data suggest that repetitive episodes of hypoglycemia are associated with a reduction in the beneficial effects of sitagliptin on the changes in carotid atherosclerosis. The different results may be due to the different subjects (T1DM vs. T2DM) or different levels of GLP-1 (DPP-4 inhibitor vs. GLP-1). In any case, when DPP-4 inhibitors are used as add-on therapy to insulin therapy, one should take precaution against potential hypoglycemia by, for example, reducing the dose of insulin.
Study limitations
The present study has certain limitations. First, this was a post hoc and exploratory analysis of a randomized unblinded trial and the sample size was relatively small. The analysis is limited by the study design and this make the significance of the findings less clear. Thus, the results should be interpreted with caution. Second, we evaluated self-reported hypoglycemic events through self-monitoring of blood glucose (SMBG) levels and hypoglycemic symptoms. Thus, there may be a risk of underestimation of the incidence of hypoglycemic episodes. In an effort to overcome possible recall bias, we confirmed the occurrence of hypoglycemia at each visit of each patient. Third, we did not evaluate hypoglycemia awareness status. Since some episodes of non-severe hypoglycemia could be asymptomatic, they were unreported by patients. Thus, we could not rule out possible underestimation of the deleterious effects of hypoglycemia on carotid atherosclerosis. Fourth, there were some discrepancies in the results of carotid IMT although the results showed a similar pattern. These differences may be due to the underpowered sample and side difference in IMT-CCA32.
Conclusions
Our data suggest that frequent episodes of hypoglycemia were associated with changes in carotid atherosclerosis in insulin-treated patients with T2DM. Physicians need to take care in avoiding the occurrence of hypoglycemic episodes in the clinical setting in order to minimize the process of atherosclerogenesis.
Methods
Study population
We performed a post hoc analysis from the Sitagliptin Preventive study of Intima-media thickness Evaluation (SPIKE). The study design, inclusion and exclusion criteria, study schedule and measurements were described in detail previously17,33. Briefly, insulin-treated Japanese T2DM patients free of past history of apparent CVD who periodically attended the Outpatient Diabetes Clinics at 12 centers across Japan were asked to participate in this study. A total of 282 participants were randomly allocated to either the sitagliptin group (n = 142) or the conventional treatment group (using drugs other than the DPP-4 inhibitor) (n = 140). Finally, 137 in the sitagliptin group and 137 in the conventional treatment group were included in the full analysis set. Each participant underwent ultrasonography of the carotid arteries including mean-IMT-CCA and in the right and left max-IMT-CCA performed by expert sonographers at the start of the study, and the procedure was repeated after 52 and 104 weeks.
All patients who agreed to participate were entered into the study. The protocol was approved by the Institutional Review Board of each participating institution (Juntendo University Graduate School of Medicine, Osaka University Graduate School of Medicine, Juntendo Tokyo Koto Geriatric Medical Center, Naka Memorial Clinic, Osaka Police Hospital, Osaka General Medical Center, Kansai Rosai Hospital, Sasebo Chuo Hospital, Jiyugaoka Medical Clinic, Ikeda Municipal Hospital) in compliance with the Declaration of Helsinki and current legal regulations in Japan. Written informed consent was obtained from all the participants after full explanation of the study. This study has been registered on the University Hospital Medical Information Network Clinical Trials Registry, which is a non-profit organization in Japan and meets the requirements of the International Committee of Medical Journal Editors (UMIN000007396).
Definition of hypoglycemia
All adverse events including hypoglycemia were recorded at each visit during study, as described previously17. During the study, participants were asked to submit their records of SMBG and whether they had a sign and symptoms of hypoglycemia. Hypoglycemia was defined based on confirmation by measurement of plasma glucose of ≤3.9 mmol/L and/or self-reported probable hypoglycemic symptom. Severe hypoglycemia was defined as events requiring aid of another person to administer treatment.
Measurement of carotid IMT
Ultrasonographic scans of the carotid artery were performed by expert sonographers who were specifically trained to perform the prescribed study examination, as reported previously17,33. To avoid inter-sonographer variability, each participant was examined by the same sonographer with the same equipment throughout all the visits. To avoid inter-reader variability, all scans were electronically stored and emailed to the central office (IMT Evaluation Committee, Osaka, Japan) to be read by a single experienced reader blinded to the clinical features of the patients, in a random order, using automated digital edge-detection software (Intimascope; MediaCross, Tokyo, Japan)17,33. The software system averages 200 points of IMT values in the segment 2 cm proximal to the dilation of the carotid bulb (mean-IMT-CCA). In addition, the greatest thicknesses of IMT, including plaque lesions in the common carotid arteries (max-IMT-CCA) were also measured separately. The reproducibility of IMT measurement was very high as described previously17.
Statistical analysis
Data were reported as mean ± SD. Statistical analysis was performed using analysis of covariance models that included several variables in addition to occurrence of hypoglycemia, such as age, gender and baseline IMT (see Table 2 for details). Baseline and follow-up group comparisons were assessed with the Student’s t-test or Wilcoxon’s rank sum test for continuous variables and Fisher’s exact test for categorical variables. Changes from baseline to treatment visits were assessed with one-sample t-test and Wilcoxon’s signed rank test within the group. We categorized patients into the following three groups according to the number of hypoglycemic episodes during follow-up: 1) those with no episodes, 2) those with less than one episode per month, and 3) those with one or more episodes. Comparisons among the three groups were performed by one-way analysis of variance. Trend associations across the three groups and changes in IMT were evaluated by univariate and multivariate linear regression analyses. All statistical tests were two-sided with 5% significance level. All analyses were performed using the SAS software version 9.4 (SAS Institute, Cary, NC).
Additional Information
How to cite this article: Mita, T. et al. Relationship between frequency of hypoglycemic episodes and changes in carotid atherosclerosis in insulin-treated patients with type 2 diabetes mellitus. Sci. Rep. 7, 39965; doi: 10.1038/srep39965 (2017).
Publisher's note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
Haffner, S. M., Lehto, S., Ronnemaa, T., Pyorala, K. & Laakso, M. Mortality from coronary heart disease in subjects with type 2 diabetes and in nondiabetic subjects with and without prior myocardial infarction. The New England journal of medicine 339, 229–234, doi: 10.1056/NEJM199807233390404 (1998).
Patel, A. et al. Intensive blood glucose control and vascular outcomes in patients with type 2 diabetes. N Engl J Med 358, 2560–2572, doi: NEJMoa0802987 10.1056/NEJMoa0802987 (2008).
Duckworth, W. et al. Glucose control and vascular complications in veterans with type 2 diabetes. N Engl J Med 360, 129–139, doi: NEJMoa0808431 10.1056/NEJMoa0808431 (2009).
Gerstein, H. C. et al. Effects of intensive glucose lowering in type 2 diabetes. N Engl J Med 358, 2545–2559, doi: NEJMoa0802743 10.1056/NEJMoa0802743 (2008).
Khunti, K. et al. Hypoglycemia and risk of cardiovascular disease and all-cause mortality in insulin-treated people with type 1 and type 2 diabetes: a cohort study. Diabetes care 38, 316–322, doi: 10.2337/dc14-0920 (2015).
Frier, B. M. et al. Peripheral blood cell changes in response to acute hypoglycaemia in man. Eur J Clin Invest 13, 33–39 (1983).
Collier, A. et al. Leucocyte mobilization and release of neutrophil elastase following acute insulin-induced hypoglycaemia in normal humans. Diabet Med 7, 506–509 (1990).
Galloway, P. J., Thomson, G. A., Fisher, B. M. & Semple, C. G. Insulin-induced hypoglycemia induces a rise in C-reactive protein. Diabetes Care 23, 861–862 (2000).
Kitabchi, A. E., Umpierrez, G. E., Miles, J. M. & Fisher, J. N. Hyperglycemic crises in adult patients with diabetes. Diabetes Care 32, 1335–1343, doi: 32/7/1335 10.2337/dc09-9032 (2009).
Dalsgaard-Nielsen, J., Madsbad, S. & Hilsted, J. Changes in platelet function, blood coagulation and fibrinolysis during insulin-induced hypoglycaemia in juvenile diabetics and normal subjects. Thromb Haemost 47, 254–258 (1982).
Fisher, B. M., Hepburn, D. A., Smith, J. G. & Frier, B. M. Responses of peripheral blood cells to acute insulin-induced hypoglycaemia in humans: effect of alpha-adrenergic blockade. Horm Metab Res Suppl 26, 109–110 (1992).
Wright, R. J. et al. Effects of acute insulin-induced hypoglycemia on indices of inflammation: putative mechanism for aggravating vascular disease in diabetes. Diabetes care 33, 1591–1597, doi: 10.2337/dc10-0013 (2010).
Gogitidze Joy, N. et al. Effects of acute hypoglycemia on inflammatory and pro-atherothrombotic biomarkers in individuals with type 1 diabetes and healthy individuals. Diabetes care 33, 1529–1535, doi: 10.2337/dc09-0354 (2010).
Gimenez, M. et al. Repeated episodes of hypoglycemia as a potential aggravating factor for preclinical atherosclerosis in subjects with type 1 diabetes. Diabetes care 34, 198–203, doi: 10.2337/dc10-1371 (2011).
Katsuno, T., Ikeda, H., Ida, K., Miyagawa, J. & Namba, M. Add-on therapy with the DPP-4 inhibitor sitagliptin improves glycemic control in insulin-treated Japanese patients with type 2 diabetes mellitus. Endocrine journal 60, 733–742 (2013).
Shimoda, S. et al. Efficacy and safety of sitagliptin as add-on therapy on glycemic control and blood glucose fluctuation in Japanese type 2 diabetes subjects ongoing with multiple daily insulin injections therapy. Endocrine journal 60, 1207–1214 (2013).
Mita, T. et al. Sitagliptin Attenuates the Progression of Carotid Intima-Media Thickening in Insulin-Treated Patients With Type 2 Diabetes: The Sitagliptin Preventive Study of Intima-Media Thickness Evaluation (SPIKE): A Randomized Controlled Trial. Diabetes care 39, 455–464, doi: 10.2337/dc15-2145 (2016).
Sato, S. et al. Efficacy and safety of sitagliptin added to insulin in Japanese patients with type 2 diabetes: the EDIT randomized trial. PloS one 10, e0121988, doi: 10.1371/journal.pone.0121988 (2015).
Fonseca, V. et al. Addition of vildagliptin to insulin improves glycaemic control in type 2 diabetes. Diabetologia 50, 1148–1155, doi: 10.1007/s00125-007-0633-0 (2007).
Rosenstock, J. et al. Alogliptin added to insulin therapy in patients with type 2 diabetes reduces HbA(1C) without causing weight gain or increased hypoglycaemia. Diabetes, obesity & metabolism 11, 1145–1152, doi: 10.1111/j.1463-1326.2009.01124.x (2009).
Elliott, L., Fidler, C., Ditchfield, A. & Stissing, T. Hypoglycemia Event Rates: A Comparison Between Real-World Data and Randomized Controlled Trial Populations in Insulin-Treated Diabetes. Diabetes therapy: research, treatment and education of diabetes and related disorders, doi: 10.1007/s13300-016-0157-z (2016).
Bosevski, M. & Stojanovska, L. Progression of carotid-artery disease in type 2 diabetic patients: a cohort prospective study. Vascular health and risk management 11, 549–553, doi: 10.2147/VHRM.S79079 (2015).
Chin, S. O. et al. Risk factors for the progression of intima-media thickness of carotid arteries: a 2-year follow-up study in patients with newly diagnosed type 2 diabetes. Diabetes & metabolism journal 37, 365–374, doi: 10.4093/dmj.2013.37.5.365 (2013).
Goto, A., Arah, O. A., Goto, M., Terauchi, Y. & Noda, M. Severe hypoglycaemia and cardiovascular disease: systematic review and meta-analysis with bias analysis. Bmj 347, f4533, doi: 10.1136/bmj.f4533 (2013).
Zoungas, S. et al. Severe hypoglycemia and risks of vascular events and death. The New England journal of medicine 363, 1410–1418, doi: 10.1056/NEJMoa1003795 (2010).
Bonds, D. E. et al. The association between symptomatic, severe hypoglycaemia and mortality in type 2 diabetes: retrospective epidemiological analysis of the ACCORD study. Bmj 340, b4909, doi: 10.1136/bmj.b4909 (2010).
Ceriello, A. et al. Vitamin C further improves the protective effect of glucagon-like peptide-1 on acute hypoglycemia-induced oxidative stress, inflammation, and endothelial dysfunction in type 1 diabetes. Diabetes care 36, 4104–4108, doi: 10.2337/dc13-0750 (2013).
Davis, S. N., Mann, S., Briscoe, V. J., Ertl, A. C. & Tate, D. B. Effects of intensive therapy and antecedent hypoglycemia on counterregulatory responses to hypoglycemia in type 2 diabetes. Diabetes 58, 701–709, doi: db08-1230 10.2337/db08-1230 (2009).
Jin, W. L. et al. Repetitive hypoglycaemia increases serum adrenaline and induces monocyte adhesion to the endothelium in rat thoracic aorta. Diabetologia 54, 1921–1929, doi: 10.1007/s00125-011-2141-5 (2011).
Soeki, T. & Sata, M. Inflammatory Biomarkers and Atherosclerosis. International heart journal, doi: 10.1536/ihj.15-346 (2016).
Yasunari, E. et al. Repetitive hypoglycemia increases circulating adrenaline level with resultant worsening of intimal thickening after vascular injury in male Goto-Kakizaki rat carotid artery. Endocrinology 155, 2244–2253, doi: 10.1210/en.2013-1628 (2014).
Plasencia Martinez, J. M., Garcia Santos, J. M., Paredes Martinez, M. L. & Pastor, A. M. Carotid intima-media thickness and hemodynamic parameters: reproducibility of manual measurements with Doppler ultrasound. Medical ultrasonography 17, 167–174, doi: 10.11152/mu.2013.2066.172.ci-m (2015).
Mita, T. et al. Rationale, design, and baseline characteristics of a clinical trial for prevention of atherosclerosis in patients with insulin-treated type 2 diabetes mellitus using DPP-4 inhibitor: the Sitagliptin Preventive study of Intima-media thickness Evaluation (SPIKE). Diabetology & metabolic syndrome 6, 35, doi: 10.1186/1758-5996-6-35 (2014).
Acknowledgements
The authors thank all the collaborators, the clinical staff and members of and members of the committee (Yoshimitsu Yamasaki, Nishi-Umeda Clinic for Asian Medical Collaboration; Kazunori Shimada and Hirotoshi Ohmura, Department of Neurology, Juntendo University Graduate school of Medicine; and Ryota Tanaka, Department of Cardiovascular Medicine, Juntendo University Graduate school of Medicine) for their assistance with the execution and completion of the clinical trial. Financial support for this study was provided by the Japan Society for Patients Reported Outcome research fund from Mitsubishi Tanabe, Ono and Novo Nordisk.
Author information
Authors and Affiliations
Contributions
The authors meet the criteria for authorship recommended by the International Committee of Medical Journal Editors and take full responsibility for all contents of the manuscript and editorial decisions. All authors (T.M., N.Ka., T.S., H.Y., N.K., T.O., H.K., K.K., Y.U., M.G., I.S. and H.W.) contributed to the study design and were involved at all stages of the study and manuscript development. T.M. and N.Ka. drafted the manuscript. M.G. contributed to analysis of research data. All authors (T.M., N.Ka., T.S., H.Y., N.K., T.O., H.K., K.K., Y.U., M.G., I.S. and H.W.) were involved in analysis and interpretation of data, reviewed/edited the manuscript and approved the final manuscript. I.S. and H.W. are the principal guarantors of this work and have full access to all the data and take responsibility for the integrity of the data and accuracy of data analysis.
Corresponding author
Ethics declarations
Competing interests
TM received research funds from MSD and Takeda Pharma K.K. and has received lecture fees from AstraZeneca K.K., Boehringer Ingelheim, Eli Lilly, Kowa Pharmaceutical Co., Mitsubishi Tanabe Pharma Co., MSD, Ono Pharmaceutical Co., and Takeda Pharmaceutical Co. NKa is a staff member of the endowed chair (Department of Metabolism and Atherosclerosis) established by funds from Kowa Pharmaceutical Co., has received research funds from MSD and lecture fees from Astellas Pharma Inc., AstraZeneca K.K., Boehringer Ingelheim, Daiichi Sankyo Inc., Dainippon Sumitomo Pharma Co., Eisai Co., Eli Lilly, Kowa Pharmaceutical Co., Mitsubishi Tanabe Pharma Co., Novartis Pharmaceuticals, Novo Nordisk Pharma, Ono Pharmaceutical Co., Otsuka Pharmaceutical, Shionogi & Co., Takeda Pharmaceutical Co., Sanofi-Aventis, and Shionogi & Co. TS has received lecture fees from Boehringer Ingelheim, Sanofi-Aventis, Novo Nordisk Pharma, Novartis Pharmaceuticals, Eli Lilly, Abbott Japan, Takeda Pharmaceutical Co., Sanwakagaku Kenkyusho, Mitsubishi Tanabe Pharma Co., Daiichi Sankyo Inc., Astellas Pharma Inc., Ono Pharmaceutical Co., MSD, Shionogi, Pharma, and Taisho Toyama Pharmaceutical Co. NKu has received lecture fees from Sanofi-Aventis and Novartis Pharmaceuticals. TOs has received lecture fees from Novo Nordisk, Inc., Astellas Pharma, Inc., Mitsubishi Tanabe Pharma, Sanwakagaku Kenkyusho, Takeda Pharmaceutical Co., Kowa Co. and research funds from Novo Nordisk, Inc., Astellas Pharma, Inc., Mitsubishi Tanabe Pharma, Sanwakagaku Kenkyusho, Kowa Co. Novo Nordisk Pharma, Dainippon Sumitomo Pharma., Eli Lilly Taisho Pharmaceutical Co., Ltd., GlaxoSmithKline, Sumitomo Dainippon Pharma Co., Ltd., Astellas Pharma US, Inc., Bayer HealthCare, and AbbVie GK. KK has received lecture fees from Boehringer Ingelheim, Sanofi-Aventis, Novo Nordisk Pharma, Novartis Pharmaceuticals, Eli Lilly, Takeda Pharmaceutical Co., MSD, Kowa Co., Mitsubishi Tanabe Pharma and research funds from Sysmex Co. HK has received lecture fees from Boehringer Ingelheim, Sanofi-Aventis, Ono Pharmaceutical Co., MSD, Novo Nordisk Pharma, Novartis Pharmaceuticals, Daiichi Sankyo Inc., Takeda Pharmaceutical Co., Kissei Pharmaceutical Co., Dainippon Sumitomo Pharma Co., Mitsubishi Tanabe Pharma Co., Kyowa Kirin, Eli Lilly, Pfizer, Astrazeneca, Astellas Pharma Inc. and research funds from Takeda Pharmaceutical Co., MSD, Mochida Pharmaceutical Co. Sanofi-Aventis, Novartis Pharmaceuticals, Novo Nordisk Pharma, Eli Lilly, Daiichi Sankyo Inc., Shionogi Pharma, Teijin Pharma, Dainippon Sumitomo Pharma Co., Otsuka Pharmaceutical, Kissei Pharmaceutical Co., Mitsubishi Tanabe Pharma Co., Ono Pharmaceutical Co., Astrazeneca, Astellas Pharma Inc., and Kyowa Hakko Kirin Co. KK has received lecture fees from Boehringer Ingelheim, Sanofi-Aventis, Novo Nordisk Pharma, Novartis Pharmaceuticals, Eli Lilly, Takeda Pharmaceutical Co., MSD, Kowa Co., Mitsubishi Tanabe Pharma and research funds from Sysmex Co. MG received lecture fees from Novartis and Tiho Pharma K.K. and received travel fees from Takeda Pharmaceutical Co. and writing fee from Kowa Co., Ltd. IS has received lecture fees from Astellas Pharma Inc., AstraZeneca K.K., MSD K.K., Ono Pharmaceutical Co., Kyowa Hakko Kirin Co., Kowa Pharmaceutical Co., Sanofi K.K., Sanwa Kagaku Kenkyusho Co., Daiichi Sankyo Co., Takeda Pharma K.K., Mitsubishi Tanabe Pharma Co., Teijin Pharma, Eli Lilly Japan K.K., Nippon Boehringer Ingelheim Co., Novartis Pharma K.K., Novo Nordisk Pharma, Bayer Yakuhin, Pfizer Japan Inc., Bristol-Myers K.K., Mochida Pharmaceutical Co., Shionogi & Co., Taisho Toyama Pharmaceutical Co., Shionogi & Co., and research funds from Astellas Pharma Inc., AstraZeneca K.K., Eisai Co., MSD K.K, Otsuka Pharmaceutical Co., Ono Pharmaceutical Co., Kaken Pharmaceutical Co., Kissei Pharmaceutical Co., Kyowa Hakko Kirin Co., Sanofi K.K., Shionogi & Co., Daiichi Sankyo Co., Dainippon Sumitomo Pharma Co., Takeda Pharma K.K., Mitsubishi Tanabe Pharma Co., Teijin Pharma, Nippon Boehringer Ingelheim Co., Novartis Pharma K.K., Novo Nordisk Pharma, Pfizer Japan Inc., Bristol-Myers K.K., Mochida Pharmaceutical Co., Eli Lilly Japan K.K, Kowa Co., Ltd., Kowa Pharmaceutical Co., and Taisho Toyama Pharmaceutical Co. HW has received lecture fees from Novo Nordisk, Inc., Eli Lilly and Company, Sanofi, Dainippon Sumitomo Pharma Co., Fujifilm, Bayer Health Care, Kissei Pharmaceutical Company, Mochida Pharmaceutical Company, MSD, Takeda Pharmaceutical Company, Boehringer Ingelheim Pharmaceuticals, Inc., Daiichi-Sankyo, Ono Pharmaceutical Co., Ltd., Novartis Pharmaceuticals Corporation, Mitsubishi Tanabe Pharma Corporation, AstraZeneca LP, Kyowa Hakko Kirin Comapany, Ltd, Sanwa Kagaku Kenkyusyo Company, Ltd., Kowa Company Ltd, Astellas Pharma, Inc., advisory fees from Novo Nordisk, Inc., Mochida Pharma Company, AstraZeneca LP, Kowa Company, Astellas Pharma, Inc., Sanofi, Boehringer Ingelheim Pharmaceuticals, Inc., MSD, Mitsubishi Tanabe Pharma Corporation, Novartis Pharmaceuticals Corporation, Dainippon Sumitomo Pharma Co, Takeda Pharmaceutical Company, Ono Pharmaceutical Co, Pfizer, Inc., Kowa Company and research funds from Boehringer Ingelheim, Pfizer, Mochida Pharmaceutical Co., Sanofi-Aventis, Novo Nordisk Pharma, Novartis Pharmaceuticals, Sanwakagaku Kenkyusho, Terumo Corp. Eli Lilly, Mitsubishi Tanabe Pharma, Daiichi Sankyo Inc., Takeda Pharmaceutical Co., MSD, Shionogi, Pharma, Dainippon Sumitomo Pharma, Kissei Pharma, and Astrazeneca.
Rights and permissions
This work is licensed under a Creative Commons Attribution 4.0 International License. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in the credit line; if the material is not included under the Creative Commons license, users will need to obtain permission from the license holder to reproduce the material. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/
About this article
Cite this article
Mita, T., Katakami, N., Shiraiwa, T. et al. Relationship between frequency of hypoglycemic episodes and changes in carotid atherosclerosis in insulin-treated patients with type 2 diabetes mellitus. Sci Rep 7, 39965 (2017). https://doi.org/10.1038/srep39965
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/srep39965
This article is cited by
-
Associations between continuous glucose monitoring-derived metrics and arterial stiffness in Japanese patients with type 2 diabetes
Cardiovascular Diabetology (2021)
-
Efficacy and safety of a combination of an insulin secretagogue and a dipeptidyl peptidase-4 inhibitor in Japanese patients with type 2 diabetes mellitus; the repaglinide glucose oscillation study in Fukuoka (REGO-F)
Diabetology International (2020)
-
Dose-Dependent Effect of Sitagliptin on Carotid Atherosclerosis in Patients with Type 2 Diabetes Mellitus Receiving Insulin Treatment: A Post Hoc Analysis
Diabetes Therapy (2017)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.