Abstract
Acute lymphoblastic leukemia (ALL) is a heterogeneous disease, and the long-term survival varies with different ages. We performed a retrospective analysis of 122 newly diagnosed adults with standard-risk ALL treated with Escherichia coli asparaginase (E. coli-asparaginase, n = 50) and polyethylene glycol-conjugated asparaginase (PEG-asparaginase, n = 72). No treatment-related mortality (TRM) occurred in the E. coli-asparaginase group, and 3 TRM events occurred in the PEG-asparaginase group without relation to asparaginase. In addition, 22 (44.0%) and 48 (66.7%) patients achieved a complete response (CR) on day 14 in the E. coli-asparaginase and PEG-asparaginase groups, respectively (P = 0.032). No different 5-year event-free survival (EFS) or overall survival (OS) rate (P = 0.632 and 0.769) was observed. Multivariate analysis revealed later CR (P = 0.008) and older age (P = 0.049) as adverse prognostic factors for both EFS and OS. In addition, we specifically monitored the known adverse effects of asparaginase, and no asparaginase-related death was observed. Allergy occurred in 9 patients using E. coli-asparaginase, and no patient in the PEG-asparaginase group suffered from allergies (P <0.001). The incidence of other asparaginase-related toxicities was similar. We conclude that PEG-asparaginase can be safely and effectively used as asparaginase in adults with newly diagnosed standard-risk ALL.
Similar content being viewed by others
Introduction
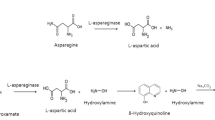
Acute lymphoblastic leukemia (ALL) is a heterogeneous disease, and outcomes vary by age, immunophenotype, and cytogenetic and molecular features. Asparaginase, a bacterial enzyme that depletes serum asparagine, is a standard component in most combination chemotherapy protocols for ALL1 both in children2,3,4,5,6 and adults7,8. ALL cells lack asparagine synthetase and are dependent on the plasma levels of this amino acid for survival9,10. Plasma asparagine depletion leads to inhibition of protein synthesis, which results in inhibition of nucleotide synthesis and subsequent apoptotic cell death of the leukemic cells1,11. Three types of asparaginase are currently available; these asparaginases are derived from two different bacterial sources: Escherichia coli and Erwinia chrysanthemi12,13,14. Native Escherichia coli asparaginase (E. coli-asparaginase) and polyethylene glycol-conjugated asparaginase (PEG-asparaginase) are both derived from Escherichia coli, whereas Erwinia asparaginase is derived from Erwinia chrysanthemi12,13,14. The most commonly used form of asparaginase is E. coli-asparaginase14.
A major limitation of E. coli-asparaginase is the development of hypersensitivity, which is reported in 15 to 73% of cases12,14,15,16. Other side effects, such as thrombosis, pancreatitis, hyperglycemia, hepatotoxicity, and abnormalities of lipid metabolism, also contribute to the limitations12,17,18. Compared with E. coli-asparaginase, PEG-asparaginase produces prolonged depletion of asparagine and is associated with reduced incidence of certain toxicities (i.e., hypersensitivity reactions), thereby making it preferable for use in ALL treatment19,20,21.
The development of treatment for children has improved with each successive study, with long-term survival achieved in more than 80% of patients22,23,24. Similarly, steady improvements in the cure rate for adults have been achieved through accurate diagnoses; the use of intensive combination chemotherapy; attention to potential sanctuary sites, such as the central nervous system (CNS); and the appropriate use of allogeneic hematopoietic stem-cell transplant (allo-HSCT). However, the long overall survival (OS) and event-free survival (EFS) of ALL in adults remain poor compared with children, and no clear consensus has been reached as to whether allo-HSCT is advantageous compared with the most effective available chemotherapy for consolidation of adults with standard-risk ALL while in the first complete response (CR1)25,26,27.
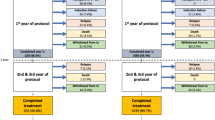
Since 2005, adults in our center with standard-risk ALL, as defined according to the criteria of the United Kingdom Medical Research Council Adult Leukemia Working Party and Eastern Cooperative Oncology Group (MRC UKALL XII/ECOG) E2993 protocol28,29, have received induction, intensification, consolidation, and maintenance therapy using the MRC UKALL XII/ECOG E2993-based regimen, including E. coli-asparaginase or PEG-asparaginase as asparaginase (Table 1). However, allo-HSCT was not recommended after CR1. Given that limited information has been reported on the comparison between E. coli-asparaginase and PEG-asparaginase in adults with newly diagnosed ALL to date, we investigated this issue in our single-center series.
Results
Patient characteristics
From January 2005 to January 2013, 59 patients first received E. coli-asparaginase, and 9 patients were excluded due to allergy to E. coli-asparaginase and switched to Erwinia asparaginase. In addition, none of the 9 patients experienced a subsequent allergic event while receiving Erwinia asparaginase. In total, 72 patients received PEG-asparaginase, and no patients suffered from allergy. Thus, a total of 122 patients with standard-risk ALL were included. The median age in the E. coli-asparaginase and PEG-asparaginase groups was 27 years (range 18–35) and 26 years (range 18–35), respectively (P = 0.822). Correspondingly, the median white blood cell (WBC) of the two groups was 26.25 (0.50–94.06) × 109/L and 26.92 (1.08–99.74) × 109/L, with no difference between the two groups (P = 0.379). The baseline characteristics for patients receiving E. coli-asparaginase and PEG-asparaginase regimens are presented in Table 2. No significant differences were observed between the two groups with respect to age, sex, immunophenotype, Eastern Cooperative Oncology Group (ECOG) performance status, extramedullary leukemia, and cerebrospinal fluid (CSF) positivity at diagnosis.
Toxicity and clinical management
Asparaginase-related toxic events, including pancreatitis, transaminitis, hyperbilirubinemia, hypoalbuminemia, hyperglycemia, hypertriglyceridemia, hypofibrinogenemia and deep vein thrombosis (DVT), were comparable and without statistical differences (Table 3). No asparaginase-related toxic deaths were observed in either group.
All patients suffered from grade IV myelosuppression, which included the lowest WBC counts of 0.05–0.89 × 109/L (median 0.42 × 109/L) and 0.03–0.96 × 109/L (median 0.39 × 109/L), hemoglobin level of 49–63 g/L (median 57 g/L) and 52–61 g/L (median 56 g/L), and platelet count of 2–24 × 109/L (median 13 × 109/L) and 4–22 (median 13 × 109/L) in the two groups, respectively. Other non-specific toxicities, including hair loss, nausea and vomiting, oral ulcers, fever, bacteremia, and the use of intravenous antifungal therapy for suspected invasive fungal disease, were similar for both groups (data not shown).
No treatment-related mortality (TRM) occurred in the E. coli-asparaginase group. In contrast, 3 TRM events occurred in the PEG-asparaginase group without relation to asparaginase. The 3 deaths were considered to be directly related to grade 4 myelosuppression and sepsis in the consolidation therapy (2 in cycle 1 and 1 in cycle 3).
Grade 3/4 pancreatitis was managed with delay asparaginase, alimentation, analgesia, octreotide, and antibiotics. These measures are effective when initiated upon the first symptoms and signs of acute pancreatitis. Moreover, the asparaginase treatment was delayed but not reduced in dose when grade 3/4 hepatotoxicity developed. Careful monitoring was conducted when toxicity resolves to grade 1/2, and cryoprecipitate infusion was administered when serum fibrinogen was less than 50 mg/dL. Patients suffering from thrombotic complications were anticoagulated with low-molecular-weight heparin and subsequent warfarin without terminating the use of asparaginase.
Response, survival, relapse and follow-up treatment
Comparison of outcomes for the E. coli-asparaginase and PEG-asparaginase groups is presented in Table 4. In total, 22 patients (44.0%) achieved early CR on day 14 in the E. coli-asparaginase group, whereas 48 (66.7%) patients achieved early CR in the PEG-asparaginase group (P = 0.016), indicating a more rapid clearance of blasts on day 14 in the PEG-asparaginase arm. At a median follow-up of 41.2 (17.7–86.8) and 43.6 (18.4–85.2) months in E. coli-asparaginase and PEG-asparaginase groups from the treatment commencement, respectively, no significant difference was observed in 5-year EFS: 46.9% for PEG-asparaginase group versus 43.6% for E. coli-asparaginase group (P = 0.632) (Fig. 1). Similarly, no difference was observed when comparing 5-year OS (48.1% and 46.2% for PEG-asparaginase and E. coli-asparaginase groups, respectively (P = 0.769) (Fig. 2)), despite the superior early response of induction therapy with PEG-asparaginase (increased CR frequency on day 14 during induction 1).
Since January 2009, minimal residual disease (MRD) by multiparameter flow cytometry (MFC) was performed on remission bone marrow specimens at the time of achievement of CR and then every cycle of therapy. In total, 69 patients were evaluable in the MRD assessment (29 in E. coli-asparaginase group and 40 in PEG-asparaginase group). In the E. coli-asparaginase group, MRD negativity was noted in 22 (75.9%) patients after 1 cycle and 24 (82.8%) patients after 2 or more cycles. In addition, MRD negativity was achieved by 30 (75.0%) patients after 1 cycle and 33 (82.5%) patients after 2 or more cycles in the PEG-asparaginase group. For the patients evaluable in the MRD assessment, MRD at the end of cycle 1 had a significant impact on survival (data not shown). Due to inadequate MRD data, additional survival analysis of MRD in the total cohort was not conducted.
Relapses were observed in 22/50 (44.0%) in the E. coli-asparaginase group and 33/72 (45.8%) in the PEG-asparaginase group (P = 0.856). Among the relapsing patients in the E. coli-asparaginase group, 12/22 (54.5%) were able to achieve a second CR (CR2) after re-induction chemotherapy, and 10 patients in CR2 were subsequently able to proceed to allo-HSCT. In comparison, for the 33 relapsing patients in the PEG-asparaginase group, 15/33 (45.5%) achieved CR2, and 11 patients in CR2 went on allo-HSCT. The median OS of patients post-relapse was 13 months (range 2–31 months) in the E. coli-asparaginase group and 11 months (range 2–32 months) in the PEG-asparaginase group.
Prognostic factors
Table 5 displays the results of the univariate and multivariate analyses of the potential predictors of EFS and OS. Multivariate analysis using the forward conditional Cox region model identified later CR (relative risk = 2.082, 95% CI 1.208–3.587, P = 0.008) and older age (relative risk = 1.758, 95% CI 1.003–3.083, P = 0.049) as two adverse factors for EFS. Similarly, in the multivariate analysis for OS, later CR (relative risk = 1.964, 95% CI 1.082–3.564, P = 0.026) and older age (relative risk = 2.208, 95% CI 1.226–3.976, P = 0.008) were also identified as significant independent worse predictors of OS.
Discussion
Currently, approximately 50% of adults with standard-risk ALL are cured with modern intensive chemotherapy that continues for 2 to 3 years of total therapy. Late treatment-related complications are uncommon after chemotherapy alone. Thus, the chronic disease burdens and diminished quality of life associated with allo-HSCT can be avoided. In addition, monitoring for MRD may identify a selected subset of ALL patients in CR1 who are likely to relapse and would most likely benefit from an early allo-HSCT30. Allo-HSCT can rescue some patients in CR2. Hence, chemotherapy with intensification, consolidation, and maintenance rather than allo-HSCT is recommended for adults with standard-risk ALL after CR1 at our department.
The implementation of regimens in adults with ALL has not been well studied, particularly for asparaginase, which is standard in children. E. coli-asparaginase and PEG-asparaginase have major differences in pharmacokinetic parameters and immunogenicity4,13. To date, no studies have compared E. coli-asparaginase with PEG-asparaginase based on their outcome and toxicities in adults with standard-risk ALL. Therefore, we conducted this retrospective study to evaluate the efficacy, safety, and toxicity of E. coli-asparaginase and PEG-asparaginase in these patients.
Of all the pharmacokinetic data, perhaps the most important characteristic of the PEG-asparaginase is the prolonged half-life. PEG-asparaginase has a t1/2 of approximately 6 days, which is far longer than that of the E. coli-asparaginase. Doses of PEG-asparaginase that have been used in ALL are 2000 to 2500 IU/m2, and dosing intervals ranged within 2 weeks31,32. Several initial studies suggested that the present dose and substitution used is 2000 to 2500 IU/m2 for each series of 6 to 9 doses of E. coli-asparaginase33. Thus, we used 3 doses of PEG-asparaginase at 2000 IU/m2 instead of 18 doses of E. coli-asparaginase at intervals of 2 weeks. Previous studies indicated that most patients with E. coli-asparaginase allergy also have a neutralizing antibody to the enzyme, resulting in sub-therapeutic systemic asparaginase activity even if allergic symptoms are prevented by the use of antihistamines and other premedications34,35,36,37,38. Erwinia asparaginase is an alternative preparation that is antigenically distinct from E. coli-asparaginase and PEG-asparaginase and has been administered to patients who experienced allergy to E. coli-asparaginase and PEG-asparaginase39,40. Thus, the development of allergy to E. coli-asparaginase required a change to Erwinia asparaginase in our department.
No TRM event occurred in the E. coli-asparaginase group, and 3 TRM events occurred in the PEG-asparaginase group without relation to asparaginase. In addition, we monitored the known adverse effects of asparaginase, and no asparaginase-related deaths were observed. A total of 9 patients using E. coli-asparaginase had grade 1/2 allergic reactions, whereas no patient using PEG-asparaginase experienced allergic reactions. The incidence of allergy was increased in the E. coli-asparaginase group compared with the PEG-asparaginase group with statistical significance (P < 0.001).
In our present retrospective study, no grade 1/2 pancreatitis was observed, and the incidence of grade 3/4 pancreatitis in the two groups was 9.8% vs. 5.8%, P = 0.715 (Table 3), which appeared to be consistent with some other studies with adult ALL17,41 and no greater than the value observed in pediatric patients3,4,6. Although three decades have elapsed since asparaginase-related pancreatitis was first described, the mechanism of this toxicity remains unknown42.
No statistical significance was observed in the incidence of hyperglycemia and hypertriglyceridemia in either grade 1/2 or grade 3/4 (Table 3). The incidence rates of hyperglycemia and hypertriglyceridemia in both groups were also similar with some previous studies17,43,44. Furthermore, two endocrine complications were commonly observed in induction regimen (data not shown), which included a large dose of prednisone. Similarly, the concomitant use of both drugs synergistically increases the occurrence of hyperglycemia and hypertriglyceridemia45.
The most common toxicities were hepatic (hyperbilirubinemia, transaminitis, hypoalbuminemia, and hypofibrinogenemia). No differences were observed regarding the incidence of these hepatic toxicities between the two groups (Table 3). The mechanism of asparaginase-related hepatotoxicity is hypothesized to be caused by the declined protein synthesis or impaired liver mitochondrial function46,47. However, determining the reasons for liver toxicity when the underlying disease, infection, co-morbidities, and other hepatotoxic agents can all be inciting factors is difficult. As recommended by other clinical experiences and the literature to date48,49, we would delay but not reduce the dose of asparaginase when grade 3/4 hepatotoxicity developed and subsequently rechallenge with careful monitoring when toxicity resolves to grade 1/2 because the injury to the liver itself is transient. Conservative use of cryoprecipitate was administered when serum fibrinogen was less than 50 mg/dL.
Thrombosis was uncommon in our study, and all the thrombotic events were related to venous catheters. The incidence was lower than some previous reports on the toxicity of asparaginase17,50,51, which may be explained by avoiding routinely infusing cryoprecipitate only when fibrinogen level was less than 50 mg/dL, according to the recommendation from the French CAPELAL study51. Routine administration of cryoprecipitate was not beneficial in preventing thrombosis in a pediatric study52 because cryoprecipitate contains high concentrations of factor VIII and is therefore particularly thrombogenic. No clear conclusion is available in the literature regarding whether further administration of asparaginase should be terminated when thrombosis occurs in adults. Asparaginase was continued after effective anticoagulation without recurrence of complications in the CAPELAL study51. Thus, we continued the use of asparaginase with anticoagulation therapy and closely monitored the patients when thrombosis occurred.
Importantly, statistically significant superiority was documented for PEG-asparaginase compared with E. coli-asparaginase in terms of the clearance of lymphoblasts from day 14 bone marrow aspirates in our adults. The reason for the difference is unknown but could be from persistent, high asparaginase activity in the PEG-asparaginase patients. However, our study is not sufficient to detect a superior EFS or OS in the PEG-asparaginase group. At a median follow-up of 43.6 months in the PEG-asparaginase group, a 5-year EFS rate of 46.9% and a 5-year OS rate of 48.1% were observed. Moreover, 5-year EFS and 5-year OS rates of 43.6% and 46.2%, respectively, were observed in the E. coli-asparaginase group, with a median follow-up of 41.2 months. Our survival data were similar to the data for other standard-risk ALL patients (only receiving chemotherapy after CR1) from several clinical trials in which no significant benefit for allo-HCT was observed compared with chemotherapy with respect to EFS and OS among standard-risk ALL patients53,54,55,56.
We also conducted univariate and multivariate analyses of the potential predictors of EFS and OS in adults with standard-risk ALL. Later CR and older age were suggested as adverse independent prognostic factors. Early response to treatment is one of the most important prognostic factors in children with ALL, which was assessed by day 7 and 14 bone marrow morphology or day 7 peripheral blast count6. This conclusion also applies equally to adults with standard-risk ALL. Age is also one of the most important prognostic factors in the total cohort of ALL because the prevalence of high-risk biological leukemia (e.g., BCR-ABL and MLL rearrangements) and unfavorable factors, such as high WBC count, increase with age. Nevertheless, in the absence of the known risk and unfavourable factors mentioned above, age can also indicate prognosis in adults with standard-risk ALL, which may be explained by the poor adherence to and tolerance of therapy or other unknown worse biological factors in the older subgroup.
As mentioned above, early CR was associated with improved EFS and OS upon multivariate analysis. Patients using PEG-asparaginase achieved a higher early CR rate that did not transform into superior EFS or OS. Various reasons may contribute to the inconsistency. Our study was a retrospective study in a single center with a small sample size. No TRM event occurred in the E. coli-asparaginase group, whereas 3 TRM events occurred without relapse in PEG-asparaginase group. The follow-up treatments after relapse were not comparable and were performed at the discretion of the treating physician on the basis of donor availability.
MRD by MFC was performed since January 2009. In total, 69 patients received MRD assessment. In these patients mentioned above, MRD at the end of cycle 1 had a significant impact on survival. Due to inadequate MRD data for all patients, a comparison of MRD status between the two groups was not conducted. In addition, MRD was not evaluated in the multivariate analysis. Further efforts are still needed to develop a precise risk stratification including MRD to distinguish patients who need allo-HSCT treatment in CR1.
Several limitations in our present analysis are discussed below. It is important to note that this was a retrospective study in a single center, and the sample size was small. Moreover, due to the retrospective character of this analysis, the monitoring of toxicities might not be standard in some patients and toxicities were likely underestimated. In addition, we have no laboratory data on the monitoring of asparaginase trough levels and effective serum asparagine depletion from our patients treated with PEG-asparaginase and E. coli-asparaginase. Future prospective randomized clinical trials may be warranted to compare the efficacy and safety of the two asparaginase preparations and to optimize the dose and the frequency and route of administration of PEG-asparaginase in adults with newly diagnosed ALL.
In conclusion, PEG-asparaginase administered in the context of the UKALLXII/ECOG E2993-based chemotherapy regimen at 2000 IU/m2 per dose is safe for adults with standard-risk ALL, and substitution of PEG-asparaginase for E. coli-asparaginase during induction and intensification conferred a statistically significant advantage in the CR rate on day 14 but was not sufficient to detect a difference in the EFS and OS. Therefore, PEG-asparaginase may have the same efficacy as E. coli-asparaginase and be safely used as another choice of asparaginase in adults with standard-risk ALL given its more rapid clearance of lymphoblasts on day 14, reduced incidence of allergy, and similar long-term outcome and convenience.
Methods
Patients
This study was a retrospective study that involved adult patients with newly diagnosed standard-risk ALL defined according to the UKALLXII/ECOG E2993 protocol and satisfying the following criteria28: Philadelphia chromosome, negative; age, ≤35 years; time taken to achieve CR, ≤4 weeks; WBC count, <30 × 109/L for B-lineage ALL and <100 × 109/L for T-lineage ALL, excluding t(4;11) MLL translocation, complex karyotype (≥5 chromosomal abnormalities), and low hypodiploidy (30–39 chromosomes)/near triploidy (60–78 chromosomes). Patients were treated with induction, intensification, consolidation, and maintenance regimens at the Department of Hematologic Oncology, Cancer Center, Sun Yat-sen University between January 2005 and January 2013. All patients were diagnosed on the basis of clinical features, bone marrow cytology, flow cytometric evaluation, and cytogenetic and molecular biology detection. Pertinent data were obtained from clinical files and the electronic database.
The study was approved by the Ethical committee of Sun Yat-sen University Cancer Center, and written informed consent was provided by the patients. All experiments were performed in accordance with relevant guidelines and regulations.
Treatment
Patients included for analysis received phase 1 of induction therapy. Bone marrow aspirates were conducted at entry and on day 14 and day 28 of induction 1. Patients who did not achieve CR on day 28 were excluded. Included patients went on to phase 2 of induction, intensification, consolidation, and maintenance using the UKALLXII/ECOG E2993-based regimen28 incorporating 18 doses of E. coli-asparaginase or 3 doses of PEG-asparaginase into the chemotherapy of induction and intensification, respectively (Table 1). The development of allergy to E. coli-asparaginase or PEG-asparaginase required a change to Erwinia asparaginase, and the patients were excluded.
Regarding relapsed patients, second-line chemotherapy regimens and allo-HSCT were performed at the discretion of the treating physician and on the basis of donor availability.
Toxicity and laboratory monitoring
TRM was defined as death within 30 days or during hospitalization. Toxicities during each cycle were abstracted by a single investigator from the biochemistry panel results (at least once weekly) and diagnoses in the medical chart. Toxicities were graded prospectively according to the National Cancer Institute Common Terminology Criteria for Adverse Events version 4.0. Specific events of interest were allergy, pancreatitis, transaminitis, hyperbilirubinemia, hypoalbuminemia, hyperglycemia, hypertriglyceridemia, hypofibrinogenemia, and DVT during the asparaginase-containing phases of chemotherapy.
Response criteria and MRD assessment
Patients were considered in CR when bone marrow cellularity was greater than 20% with maturation of all cell lines and less than 5% blasts. Granulocyte count was greater than 1.5 × 109/L, platelet count was greater than 100 × 109/L, leukemic blasts were absent from the peripheral blood, and any detectable extramedullary leukemia had resolved. Isolated and stable splenomegaly was not considered extramedullary disease.
Since January 2009, MRD by MFC was performed on remission bone marrow specimens at the time of achievement of CR and then every cycle of therapy as previously described57. Initially, a 15-marker, 6-color panel was used; later, an 8-color panel was used. MRD positivity was defined on MFC scatter plots as a cluster of at least 20 cells exhibiting altered expression of two or more antigens. The sensitivity of this MRD assay is 0.01%.
Statistical analysis
Statistical group comparisons of categorical variables were performed using the χ2 test/Fisher’s exact test, and quantitative data, such as age and WBC count, were analysed using the non-parametric Mann–Whitney U-test test. Analysis of clinical outcomes included early response rates during induction at day 14 and relapse rate. We also examined the OS and EFS. OS was calculated from the time of diagnosis of death from any cause. EFS was the time to defined events, death, or recurrence of disease. Kaplan–Meier estimates were computed for OS and EFS. For patients without an event, observation was censored at the last contact date. The Kaplan–Meier method and log-rank test were also applied for univariate analyses of the impacts of several clinical characteristics on survival. Variables, which were significant at P < 0.05 in univariate analysis, were used in the multivariate analysis. Multivariate analysis was used to assess the prognostic impact of selected variables according to the Cox regression model. Statistical analysis was performed using the SPPS statistical package (SPPS V21.0).
Additional Information
How to cite this article: Liu, W.-J. et al. Use of PEG-asparaginase in newly diagnosed adults with standard-risk acute lymphoblastic leukemia compared with E. coli-asparaginase: a retrospective single-center study. Sci. Rep. 6, 39463; doi: 10.1038/srep39463 (2016).
Publisher's note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
van den Berg, H. Asparaginase revisited. Leukemia & lymphoma 52, 168–178, doi: 10.3109/10428194.2010.537796 (2011).
Asselin, B. L. et al. In vitro and in vivo killing of acute lymphoblastic leukemia cells by L-asparaginase. Cancer research 49, 4363–4368 (1989).
Ettinger, L. J., Kurtzberg, J., Voute, P. A., Jurgens, H. & Halpern, S. L. An open-label, multicenter study of polyethylene glycol-L-asparaginase for the treatment of acute lymphoblastic leukemia. Cancer 75, 1176–1181 (1995).
Muller, H. J. et al. Pegylated asparaginase (Oncaspar) in children with ALL: drug monitoring in reinduction according to the ALL/NHL-BFM 95 protocols. British journal of haematology 110, 379–384 (2000).
Rizzari, C. et al. A pharmacological study on pegylated asparaginase used in front-line treatment of children with acute lymphoblastic leukemia. Haematologica 91, 24–31 (2006).
Avramis, V. I. et al. A randomized comparison of native Escherichia coli asparaginase and polyethylene glycol conjugated asparaginase for treatment of children with newly diagnosed standard-risk acute lymphoblastic leukemia: a Children’s Cancer Group study. Blood 99, 1986–1994 (2002).
Rosen, O. et al. Pegylated asparaginase in combination with high-dose methotrexate for consolidation in adult acute lymphoblastic leukaemia in first remission: a pilot study. British journal of haematology 123, 836–841 (2003).
Larson, R. A. et al. A five-drug remission induction regimen with intensive consolidation for adults with acute lymphoblastic leukemia: cancer and leukemia group B study 8811. Blood 85, 2025–2037 (1995).
Haskell, C. M. & Canellos, G. P. l-asparaginase resistance in human leukemia–asparagine synthetase. Biochemical pharmacology 18, 2578–2580 (1969).
Cooney, D. A. & Handschumacher, R. E. L-asparaginase and L-asparagine metabolism. Annual review of pharmacology 10, 421–440, doi: 10.1146/annurev.pa.10.040170.002225 (1970).
Nandy, P., Periclou, A. P. & Avramis, V. I. The synergism of 6-mercaptopurine plus cytosine arabinoside followed by PEG-asparaginase in human leukemia cell lines (CCRF/CEM/0 and (CCRF/CEM/ara-C/7A) is due to increased cellular apoptosis. Anticancer research 18, 727–737 (1998).
Pieters, R. et al. L-asparaginase treatment in acute lymphoblastic leukemia: a focus on Erwinia asparaginase. Cancer 117, 238–249, doi: 10.1002/cncr.25489 (2011).
Kurtzberg, J. Asparaginase. In: Holland, J. F., Bast, F. E. I. R. C. Jr. et al.Cancer Medicine. 4th. Vol. 1027–1035 (Williams & Wilkens, 1997).
Batool, T., Makky, E. A., Jalal, M. & Yusoff, M. M. A Comprehensive Review on L-Asparaginase and Its Applications. Applied biochemistry and biotechnology 178, 900–923, doi: 10.1007/s12010-015-1917-3 (2016).
Schorin, M. A. et al. Treatment of childhood acute lymphoblastic leukemia: results of Dana-Farber Cancer Institute/Children’s Hospital Acute Lymphoblastic Leukemia Consortium Protocol 85-01. Journal of clinical oncology: official journal of the American Society of Clinical Oncology 12, 740–747 (1994).
Killander, D. et al. Hypersensitive reactions and antibody formation during L-asparaginase treatment of children and adults with acute leukemia. Cancer 37, 220–228 (1976).
Stock, W. et al. Prevention and management of asparaginase/pegasparaginase-associated toxicities in adults and older adolescents: recommendations of an expert panel. Leukemia & lymphoma 52, 2237–2253, doi: 10.3109/10428194.2011.596963 (2011).
Truelove, E., Fielding, A. K. & Hunt, B. J. The coagulopathy and thrombotic risk associated with L-asparaginase treatment in adults with acute lymphoblastic leukaemia. Leukemia 27, 553–559, doi: 10.1038/leu.2012.290 (2013).
Avramis, V. I. Asparaginases: biochemical pharmacology and modes of drug resistance. Anticancer research 32, 2423–2437 (2012).
Douer, D. et al. Pharmacodynamics and safety of intravenous pegaspargase during remission induction in adults aged 55 years or younger with newly diagnosed acute lymphoblastic leukemia. Blood 109, 2744–2750, doi: 10.1182/blood-2006-07-035006 (2007).
Patel, B. et al. Pegylated-asparaginase during induction therapy for adult acute lymphoblastic leukaemia: toxicity data from the UKALL14 trial. Leukemia, doi: 10.1038/leu.2016.219 (2016).
Duval, M. et al. Comparison of Escherichia coli-asparaginase with Erwinia-asparaginase in the treatment of childhood lymphoid malignancies: results of a randomized European Organisation for Research and Treatment of Cancer-Children’s Leukemia Group phase 3 trial. Blood 99, 2734–2739 (2002).
Schrappe, M. et al. Improved outcome in childhood acute lymphoblastic leukemia despite reduced use of anthracyclines and cranial radiotherapy: results of trial ALL-BFM 90. German-Austrian-Swiss ALL-BFM Study Group. Blood 95, 3310–3322 (2000).
Chessells, J. M. et al. The impact of age on outcome in lymphoblastic leukaemia; MRC UKALL X and XA compared: a report from the MRC Paediatric and Adult Working Parties. Leukemia 12, 463–473 (1998).
Hahn, T. et al. The role of cytotoxic therapy with hematopoietic stem cell transplantation in the therapy of acute lymphoblastic leukemia in adults: an evidence-based review. Biology of blood and marrow transplantation: journal of the American Society for Blood and Marrow Transplantation 12, 1–30, doi: 10.1016/j.bbmt.2005.10.018 (2006).
Horowitz, M. M. et al. Chemotherapy compared with bone marrow transplantation for adults with acute lymphoblastic leukemia in first remission. Annals of internal medicine 115, 13–18 (1991).
Ferrando, A. A. et al. Prognostic importance of TLX1 (HOX11) oncogene expression in adults with T-cell acute lymphoblastic leukaemia. Lancet 363, 535–536, doi: 10.1016/S0140-6736(04)15542-6 (2004).
Rowe, J. M. et al. Induction therapy for adults with acute lymphoblastic leukemia: results of more than 1500 patients from the international ALL trial: MRC UKALL XII/ECOG E2993. Blood 106, 3760–3767, doi: 10.1182/blood-2005-04-1623 (2005).
Moorman, A. V. et al. Karyotype is an independent prognostic factor in adult acute lymphoblastic leukemia (ALL): analysis of cytogenetic data from patients treated on the Medical Research Council (MRC) UKALLXII/Eastern Cooperative Oncology Group (ECOG) 2993 trial. Blood 109, 3189–3197, doi: 10.1182/blood-2006-10-051912 (2007).
Bruggemann, M. et al. Clinical significance of minimal residual disease quantification in adult patients with standard-risk acute lymphoblastic leukemia. Blood 107, 1116–1123, doi: 10.1182/blood-2005-07-2708 (2006).
Wetzler, M. et al. Effective asparagine depletion with pegylated asparaginase results in improved outcomes in adult acute lymphoblastic leukemia: Cancer and Leukemia Group B Study 9511. Blood 109, 4164–4167, doi: 10.1182/blood-2006-09-045351 (2007).
DeAngelo, D. J., D., S., Silverman, L. B. et al. A multicenter phase II study using a dose intensified pediatric regimen in adults with untreated acute lymphoblastic leukemia. Blood 110, 2007 (abstr 587) (2007).
Avramis, V. I. & Panosyan, E. H. Pharmacokinetic/pharmacodynamic relationships of asparaginase formulations: the past, the present and recommendations for the future. Clinical pharmacokinetics 44, 367–393, doi: 10.2165/00003088-200544040-00003 (2005).
Wang, B. et al. Evaluation of immunologic crossreaction of antiasparaginase antibodies in acute lymphoblastic leukemia (ALL) and lymphoma patients. Leukemia 17, 1583–1588, doi: 10.1038/sj.leu.2403011 (2003).
Woo, M. H. et al. Anti-asparaginase antibodies following E. coli asparaginase therapy in pediatric acute lymphoblastic leukemia. Leukemia 12, 1527–1533 (1998).
Hak, L. J. et al. Asparaginase pharmacodynamics differ by formulation among children with newly diagnosed acute lymphoblastic leukemia. Leukemia 18, 1072–1077, doi: 10.1038/sj.leu.2403351 (2004).
Zalewska-Szewczyk, B., Andrzejewski, W. & Bodalski, J. Development of anti-asparaginase antibodies in childhood acute lymphoblastic leukemia. Pediatric blood & cancer 43, 600–602, doi: 10.1002/pbc.20064 (2004).
Amylon, M. D. et al. Intensive high-dose asparaginase consolidation improves survival for pediatric patients with T cell acute lymphoblastic leukemia and advanced stage lymphoblastic lymphoma: a Pediatric Oncology Group study. Leukemia 13, 335–342 (1999).
Billett, A. L., Carls, A., Gelber, R. D. & Sallan, S. E. Allergic reactions to Erwinia asparaginase in children with acute lymphoblastic leukemia who had previous allergic reactions to Escherichia coli asparaginase. Cancer 70, 201–206 (1992).
Wacker, P. et al. Allergic reactions to E. coli L-asparaginase do not affect outcome in childhood B-precursor acute lymphoblastic leukemia: a Children’s Oncology Group Study. Journal of pediatric hematology/oncology 29, 627–632, doi: 10.1097/MPH.0b013e3181483df1 (2007).
Buie, L. W., Moore, J. & van Deventer, H. Successful use of octreotide as a chemoprotectant for prevention of PEG-asparaginase-induced pancreatitis. Pharmacotherapy 34, e149–151, doi: 10.1002/phar.1460 (2014).
Knoderer, H. M., Robarge, J. & Flockhart, D. A. Predicting asparaginase-associated pancreatitis. Pediatric blood & cancer 49, 634–639, doi: 10.1002/pbc.21037 (2007).
Aldoss, I. et al. Toxicity profile of repeated doses of PEG-asparaginase incorporated into a pediatric-type regimen for adult acute lymphoblastic leukemia. European journal of haematology, doi: 10.1111/ejh.12600 (2015).
Tong, W. H. et al. The toxicity of very prolonged courses of PEGasparaginase or Erwinia asparaginase in relation to asparaginase activity, with a special focus on dyslipidemia. Haematologica 99, 1716–1721, doi: 10.3324/haematol.2014.109413 (2014).
Khan, A., Adachi, M. & Hill, J. M. Potentiation of diabetogenic effect of L-asparaginase by prednisolone. Hormone and metabolic research = Hormon- und Stoffwechselforschung = Hormones et metabolisme 2, 275–276, doi: 10.1055/s-0028-1095058 (1970).
Sahoo, S. & Hart, J. Histopathological features of L-asparaginase-induced liver disease. Seminars in liver disease 23, 295–299, doi: 10.1055/s-2003-42647 (2003).
Schein, P. S., Rakieten, N., Gordon, B. M., Davis, R. D. & Rall, D. P. The toxicity of Escherichia coli L-asparaginase. Cancer research 29, 426–434 (1969).
Zeidan, A., Wang, E. S. & Wetzler, M. Pegasparaginase: where do we stand? Expert opinion on biological therapy 9, 111–119, doi: 10.1517/14712590802586058 (2009).
Graham, M. L. Pegaspargase: a review of clinical studies. Advanced drug delivery reviews 55, 1293–1302 (2003).
Grace, R. F. et al. The frequency and management of asparaginase-related thrombosis in paediatric and adult patients with acute lymphoblastic leukaemia treated on Dana-Farber Cancer Institute consortium protocols. British journal of haematology 152, 452–459, doi: 10.1111/j.1365-2141.2010.08524.x (2011).
Hunault-Berger, M. et al. Changes in antithrombin and fibrinogen levels during induction chemotherapy with L-asparaginase in adult patients with acute lymphoblastic leukemia or lymphoblastic lymphoma. Use of supportive coagulation therapy and clinical outcome: the CAPELAL study. Haematologica 93, 1488–1494, doi: 10.3324/haematol.12948 (2008).
Abbott, L. S. et al. The impact of prophylactic fresh-frozen plasma and cryoprecipitate on the incidence of central nervous system thrombosis and hemorrhage in children with acute lymphoblastic leukemia receiving asparaginase. Blood 114, 5146–5151, doi: 10.1182/blood-2009-07-231084 (2009).
Ribera, J. M. et al. Comparison of intensive chemotherapy, allogeneic or autologous stem cell transplantation as post-remission treatment for adult patients with high-risk acute lymphoblastic leukemia. Results of the PETHEMA ALL-93 trial. Haematologica 90, 1346–1356 (2005).
Fiere, D. et al. Adult acute lymphoblastic leukemia: a multicentric randomized trial testing bone marrow transplantation as postremission therapy. The French Group on Therapy for Adult Acute Lymphoblastic Leukemia. Journal of clinical oncology: official journal of the American Society of Clinical Oncology 11, 1990–2001 (1993).
Thiebaut, A. et al. Adult acute lymphocytic leukemia study testing chemotherapy and autologous and allogeneic transplantation. A follow-up report of the French protocol LALA 87. Hematology/oncology clinics of North America 14, 1353–1366, x (2000).
Sebban, C. et al. Allogeneic bone marrow transplantation in adult acute lymphoblastic leukemia in first complete remission: a comparative study. French Group of Therapy of Adult Acute Lymphoblastic Leukemia. Journal of clinical oncology: official journal of the American Society of Clinical Oncology 12, 2580–2587 (1994).
Ravandi, F. et al. Detection of MRD may predict the outcome of patients with Philadelphia chromosome-positive ALL treated with tyrosine kinase inhibitors plus chemotherapy. Blood 122, 1214–1221, doi: 10.1182/blood-2012-11-466482 (2013).
Acknowledgements
The authors would like to thank the staff members of the Department of Hematologic Oncology, Cancer Center, Sun Yat-sen University, for their valuable suggestions and assistance.
Author information
Authors and Affiliations
Contributions
W.L. analysed the data and wrote the manuscript with H.W. and W.W. W.L. and H.W. assembled the data. W.L., H.W., W.W. and Y.L. conceived the study. M.Z., C.L. and J.W. participated in the data screening and collection. All authors have read and approved the final manuscript.
Ethics declarations
Competing interests
The authors declare no competing financial interests.
Rights and permissions
This work is licensed under a Creative Commons Attribution 4.0 International License. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in the credit line; if the material is not included under the Creative Commons license, users will need to obtain permission from the license holder to reproduce the material. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/
About this article
Cite this article
Liu, Wj., Wang, H., Wang, Wd. et al. Use of PEG-asparaginase in newly diagnosed adults with standard-risk acute lymphoblastic leukemia compared with E. coli-asparaginase: a retrospective single-center study. Sci Rep 6, 39463 (2016). https://doi.org/10.1038/srep39463
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/srep39463
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.