Abstract
The association between neutrophil-to-lymphocyte ratio (NLR) and differentiated thyroid cancer (DTC) is undecided. To rectify this question, we conducted a systematic meta-analysis based on 7 prospective cohort studies published between 2013 and 2015, comprising 7349 patients. Six of these cohorts included pretreatment (baseline) NLR data for patients with thyroid nodules. The meta-analysis of these 6 cohorts showed that the NLR of patients with DTC (4617 cases) was statistically similar to patients with benign nodules only (1666 cases), with a mean difference (MD) of 0.19 (95% CI: −0.09 to 0.46; I2 = 93%; P < 0.001). No significant difference in NLR was found between patients with DTC and patients with benign nodules. Two studies addressed an association between NLR and papillary thyroid carcinoma in patients stratified by age <45 and ≥45 years (496 and 891 cases, respectively); the pooled MD was 0.09 (95% CI: −0.37 to 0.55; I2 = 92.2%, P < 0.001). An elevated NLR seems not a reliable indicator of progressing DTC in patients with goiters, and there was no difference in NLR between patients aged <45 years and those aged ≥45 years. Well-designed and large-scale investigations are warranted to understand the value of NLR in the prognosis of DTC.
Similar content being viewed by others
Introduction
Thyroid nodules are very common, found in more than 50% of patients when using ultrasonography1. While the prevalence of thyroid nodules in the population is increasing, only 5% to 10% harbor malignant disease2. Still, there is a pressing need to correctly identify the nature of thyroid nodules3, because thyroid cancer is the most common endocrine malignancy4 and often presents in thyroid nodules. Differentiated thyroid cancers (DTCs) account for approximately 95% of all thyroid cancer and generally have a favorable prognosis5. Thyroid cancer is closely associated with inflammation6, and several studies suggest that there is a higher incidence of DTC in patients with thyroiditis7,8.
In a variety of cancers, hematological components of the systemic inflammatory response have been shown to have prognostic value, especially the neutrophil-to-lymphocyte ratio (NLR)9. NLR is inexpensive to determine and can be routinely measured in day-to-day oncological practice9, and it may be useful for identifying high-risk patients10. Consequently, many researchers have explored the association between the NLR and thyroid cancer.
According our literature search, Seretis et al.11 was the first to report that the preoperative NLR was significantly elevated in patients with papillary thyroid microcarcinomas or thyroid cancer. They proposed that the NLR was an easily accessible biomarker for detecting incidental papillary thyroid microcarcinoma. The studies of Kim et al.12 and Kocer et al.13 were in accord with this, but Liu et al.’s14 only for patients 45 years and older. However, Liu et al.14 and Kim et al.15 found that there was no difference in the NLRs between patients with benign or malignant thyroid nodules in the overall population.
Thus, the association between NLR and DTC remains controversial. The conflicting data among the above studies may be due to limited sample sizes, the demographic differences in populations, or both. To explore the potential association between NLR and DTC, we conducted a rigorous systematic meta-analysis of relevant prospective cohort studies.
Results
Study selection and characteristics
The initial search retrieved 23 studies (Fig. 1). After screening the titles or abstracts, 14 studies were excluded for being duplicate reports or irrelevant. Three more reports were discarded for the following reasons: one did not provide standard deviations of the NLR values of patients with benign nodules or thyroid cancer; 2 failed to provide NLR data for both benign nodules and thyroid cancer. One study was added from a reference list12.
Therefore, 7 studies comprising 7349 patients, published between 2013 and 2015, were included in the present meta-analysis4,12,13,14,15,16,17 (Table 1). Three studies were conducted in Korea12,15,16,17, three studies were performed in China, and one in Turkey13. NOS18 scores of the studies ranged from 7 to 8, with a mean value of 7.71.
NLR in patients with DTC or benign nodules
Six studies contained pretreatment (baseline) NLR data for patients with thyroid nodules4,12,13,14,16,17. A meta-analysis of these 6 cohorts showed that the NLR values of patients with DTC and those with benign nodules were statistically similar (mean difference [MD] = 0.19; 95% confidence interval [CI]: −0.09 to 0.46; Fig. 2a), although there was heterogeneity among the studies (Cochran’s Q test and Higgins I-squared statistic [I2 ] = 93%, P < 0.001).
Then we conducted subgroup analyses based on confounders, such as study location and tumor type. Stratified by location, we found that for patients in China4,14,16 the pooled MD was 0.07 (95% CI: −0.03 to 0.17, I2 = 24.4%, P = 0.267; Fig. 3a). For patients in Korea12,17, the pooled MD was −0.07 (95% CI: −0.16 to 0.01, I2 = 0.0%, P = 0.855). Subgroup analyses by papillary thyroid carcinoma (PTC)12,13,14,16,17 indicated that the pooled mean difference was 0.05 (95% CI: −0.05 to 0.08, I2 = 90.4%, P < 0.001; Fig. 2b).
NLR in patients with PTC stratified by age
Two studies14,15 contained NLR data for PTC patients aged <45 years (496 cases) or ≥45 years (891 cases). The pooled MD between the age groups was 0.09 (95% CI: −0.37 to 0.55, I2 = 92.2%, P < 0.001; Fig. 3b).
Heterogeneity
To investigate the influence of individual data sets on the pooled mean differences, each cohort included in our meta-analysis was deleted in turn in separate analyses. Results of sensitivity analyses indicated the robustness of our findings (Estimate: 0.17, 95% CI: −0.52 to 0.40) (Fig. 4a). By excluding one of the studies13, the heterogeneity was reduced significantly (I2 = 40%, P = 0.16) and the mean difference was nil (95% CI: −0.08 to 0.07).
Publication bias
The publication bias estimate is mainly used to evaluate the reliability of the meta-analysis results, especially when a statistically significant difference is shown. The assessment of publication bias using Begg’s test suggested that was no significant publication bias in the studies (P = 0.26; Fig. 4b).
Discussion
This meta-analysis aimed to examine the associations between pretreatment NLR and DTC. To the best of our knowledge, the present study is the first meta-analysis to investigate a potential association between them. Our study combined the outcomes of 6283 patients with thyroid nodules (4617 DTC and 1666 benign nodules) from 6 individual studies4,12,13,14,16,17. The meta-analysis showed that the pretreatment NLR values were not significantly different between patients with DTC and those with benign nodules. The subgroup and sensitivity analyses showed that the study of Kocer et al.13 was the source of heterogeneity, because its sample was much smaller than that of the others. The results were not weakened by subgroup analyses stratified by study location or tumor type. Although Kocer et al.’s13 report suggested that NLRs were significantly higher in patients with PTC than in patients with benign nodules, we noted that the age of the PTC patients (53.57 ± 13.32 y) appeared older than the age of patients with benign nodules (49.25 ± 13.15 y), although the article did not provide the P-value. These results suggest that an elevated NLR is neither a sensitive nor a specific indicator of progressing DTC in patients with goiters. Although Cho et al.17 pointed out that the NLR was a meaningful diagnostic tool for discriminating poorly differentiated thyroid cancer (n = 14) from anaplastic thyroid cancer (n = 7), their results were too limited by the small sample size and require further validation.
As reported in several studies, NLR correlated with thyroid cancer characteristics, such as tumor size, patient’s age, and the clinical stage parameters of thyroid cancer. Age is an important prognostic factor for patients with PTC17. Seretis et al.11, Liu et al.14, and Lang et al.16 found that older patients with PTC had significantly higher NLRs. However, Kim et al.15 found that the preoperative NLR was significantly lower in patients older than 45 years. Consequently, we pooled the only 2 studies that investigated age14,15 and found no difference in NLR value between patients aged younger or older than 45 years. Liu et al.4 found that the preoperative NLR correlated with DTC tumor size. Because there was limited data from the available studies, except regarding age, we did not conduct a pooled analysis of the correlation between elevated NLR and clinicopathological characteristics. However, Liu et al.14 and Kim et al.15 showed that tumor size, extra thyroidal invasion, and lymph node metastasis was not associated with the NLR value.
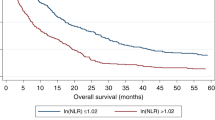
The prognosis of patients with cancer is not determined solely by tumor characteristics, but also by other factors related to the patient’s condition12. More recently, several meta-analyses reported the prognostic value of NLR in a variety of cancers19. Since PTCs have a favorable prognosis, 5 years may be considered too short to evaluate the prognostic implications12. Thus, there are too few studies to provide sufficient evidence for the prognostic value of NLR for PTC. Liu et al.4 pointed out that a high preoperative NLR was associated with a high American Thyroid Association (ATA) risk of recurrence in patients with differentiated thyroid cancer. With only 15 disease-specific events (1 distant metastasis and 14 locoregional recurrences), Kim et al.12 reported that in stage III-IV patients the 5-year disease-free survival rate was significantly worse in patients with NLR ≥ 1.5 than in those with NLR < 1.5. However, according to Lang et al.’s report16 a higher NLR did not predict a worse disease-free survival or higher risk of occult central nodal metastasis in cN0 PTC. This is not contrary to the fact that a higher NLR may imply a poorer tumor profile and prognosis. One possible reason may be because the prognosis of DTC, especially for PTC, is generally very good and so its NLR is expected to be low and within a narrow range.
In addition to the intrinsic defects associated with meta-analyses19, the present study is limited by significant heterogeneity among the studies that was due to sample size. Secondly, we did not analyze a correlation between the NLR and clinicopathological parameters of patients, such as lymph node metastasis, grade of differentiation, or tumor stage. Although age may affect the NLR, only 2 studies reported the relevant information, which was pooled with significant heterogeneity. Finally, in several reports the prognostic value of NLR for a variety of cancers was reported, and the data specifically for DTC was insufficient to analyze the prognostic value of NLR.
Despite the several limitations, our meta-analysis also had some advantages. First, the results were similar when the data were analyzed by subgroup, which indicates robustness of the statistical power of the results. Secondly, the sensitivity analysis did not significantly alter the results, supporting their stability. In addition, all the Newcastle-Ottawa quality assessment scale (NOS) scores of study quality were ≥7, which also supports the creditability of the results of the meta-analysis. Finally, although there were only 7 studies, the pooled sample was very large (nearly 7000 cases).
In conclusion, our results indicate that the NLR of patients with DTC is not significantly different from that of patients with benign nodules. An elevated NLR seems not a reliable indicator of progressing DTC in patients with goiters. In addition, there was no difference in NLR value between patients aged less than 45 years and those older than 45 years. More well-designed and large-scale investigations are warranted to understand better the value of the NLR in the prognosis of DTC.
Methods
Publication search
This meta-analysis was executed in accordance with guidelines of the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA)20. The following databases were searched for eligible studies up to 6 April 2016, without language restrictions: PubMed, Cochrane Library, EMBASE, Wan Fang Database, VIP Database for Chinese Technical Periodicals, and China National Knowledge Infrastructure. The terms used in the systematic literature search were: (“thyroid cancer” or “thyroid carcinoma”) and (“NLR” or “neutrophil to lymphocyte ratio” or “neutrophil lymphocyte ratio” or “‘neutrophil-lymphocyte-ratio”). Other resources were manually searched for any relevant records that were potentially missed. Moreover, reference lists of retrieved articles were reviewed for any studies that were not identified from the preliminary literature searches.
Study selection criteria
Studies were included if they met the following criteria: patients with thyroid cancer that was histopathologically confirmed; NLR values were reported or obtained by communication with the authors; and evaluated the correlation between NLR and thyroid cancer. Articles were excluded from the meta-analysis if they were: letters; conference abstracts; editorials; review articles; not in the English or Chinese languages; animal, or irrelevant; or contained overlapping or duplicate data.
Quality assessment
The quality of the studies was assessed according to NOS18. This scale includes 3 aspects of evaluation: selection, comparability, and outcomes between the case and control groups. Studies that scored ≥6 were considered high quality. Any disagreement between the investigators was resolved by discussion.
Data extraction
Two investigators independently evaluated and extracted the data. All studies were double-checked by both investigators, and disagreements were resolved by consensus. The extracted data elements of this review were: publication details (first author’s last name, publication year, and origin of the studied population); characteristics of the studied population (sample size, age, and stage of disease); and mean and standard deviation of the NLR for thyroid nodules. If data for the mean and standard deviation were not available, we contacted the author for the original data.
Statistical analysis
We used the mean differences with 95% CIs to calculate continuous data and identify differences in NLR values among groups of patients. A test of heterogeneity of the pooled results was performed using I2. I2 > 50% was considered significant heterogeneity. Both random effects (DerSimonian-Laird method) and fixed-effects (Mantel–Haenszel method) models were used to generate the pooled mean differences and 95% CIs. Because of a tendency toward heterogeneity among primary studies, the random-effects model was chosen because it is usually more conservative. We also investigated reasons for inter-study heterogeneity using subgroup analyses.
Sensitivity analyses were conducted to evaluate the stability of the results. Publication bias was evaluated using Begg’s funnel plot. All statistical tests were 2-sided and the significance level was set at 5% (P < 0.05). All analyses were conducted using STATA 12.0 software (STATA, College Station, TX).
Additional Information
How to cite this article: Liu, J.-F. et al. Association between neutrophil-to-lymphocyte ratio and differentiated thyroid cancer: a meta-analysis. Sci. Rep. 6, 38551; doi: 10.1038/srep38551 (2016).
Publisher's note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
Luo, J., McManus, C., Chen, H. & Sippel, R. S. Are there predictors of malignancy in patients with multinodular goiter? The Journal of surgical research 174, 207–210, doi: 10.1016/j.jss.2011.11.1035 (2012).
Dean, D. S. & Gharib, H. Epidemiology of thyroid nodules. Best practice & research. Clinical endocrinology & metabolism 22, 901–911, doi: 10.1016/j.beem.2008.09.019 (2008).
Zhou, G. J., Xiao, M., Zhao, L. N., Tang, J. G. & Zhang, L. MicroRNAs as novel biomarkers for the differentiation of malignant versus benign thyroid lesions: a meta-analysis. Genetics and molecular research: GMR 14, 7279–7289, doi: 10.4238/2015.July.3.3 (2015).
Liu, C. L. et al. Blood neutrophil-to-lymphocyte ratio correlates with tumor size in patients with differentiated thyroid cancer. Journal of surgical oncology 107, 493–497, doi: 10.1002/jso.23270 (2013).
Hundahl, S. A., Fleming, I. D., Fremgen, A. M. & Menck, H. R. A National Cancer Data Base report on 53,856 cases of thyroid carcinoma treated in the U.S. 1985–1995 [see commetns]. Cancer 83, 2638–2648 (1998).
Guarino, V., Castellone, M. D., Avilla, E. & Melillo, R. M. Thyroid cancer and inflammation. Molecular and cellular endocrinology 321, 94–102, doi: 10.1016/j.mce.2009.10.003 (2010).
Larson, S. D. et al. Increased incidence of well-differentiated thyroid cancer associated with Hashimoto thyroiditis and the role of the PI3k/Akt pathway. Journal of the American College of Surgeons 204, 764–773; discussion 773–765, doi: 10.1016/j.jamcollsurg.2006.12.037 (2007).
Bradly, D. P., Reddy, V., Prinz, R. A. & Gattuso, P. Incidental papillary carcinoma in patients treated surgically for benign thyroid diseases. Surgery 146, 1099–1104, doi: 10.1016/j.surg.2009.09.025 (2009).
Proctor, M. J. et al. A derived neutrophil to lymphocyte ratio predicts survival in patients with cancer. British journal of cancer 107, 695–699, doi: 10.1038/bjc.2012.292 (2012).
Clarke, S. J. et al. Use of inflammatory markers to guide cancer treatment. Clinical pharmacology and therapeutics 90, 475–478, doi: 10.1038/clpt.2011.122 (2011).
Seretis, C. et al. The significance of neutrophil/lymphocyte ratio as a possible marker of underlying papillary microcarcinomas in thyroidal goiters: a pilot study. American journal of surgery 205, 691–696, doi: 10.1016/j.amjsurg.2012.08.006 (2013).
Kim, J. Y. et al. Prognostic importance of baseline neutrophil to lymphocyte ratio in patients with advanced papillary thyroid carcinomas. Endocrine 46, 526–531, doi: 10.1007/s12020-013-0089-6 (2014).
Kocer, D., Karakukcu, C., Karaman, H., Gokay, F. & Bayram, F. May the neutrophil/lymphocyte ratio be a predictor in the differentiation of different thyroid disorders? Asian Pacific journal of cancer prevention: APJCP 16, 3875–3879 (2015).
Liu, J. et al. The Neutrophil-to-Lymphocyte Ratio Correlates with Age in Patients with Papillary Thyroid Carcinoma. ORL; journal for oto-rhino-laryngology and its related specialties 77, 109–116, doi: 10.1159/000375534 (2015).
Kim, S. M. et al. Association of the Preoperative Neutrophil-to-ymphocyte Count Ratio and Platelet-to-Lymphocyte Count Ratio with Clinicopathological Characteristics in Patients with Papillary Thyroid Cancer. Endocrinology and metabolism 30, 494–501, doi: 10.3803/EnM.2015.30.4.494 (2015).
Lang, B. H. et al. Does preoperative neutrophil lymphocyte ratio predict risk of recurrence and occult central nodal metastasis in papillary thyroid carcinoma? World journal of surgery 38, 2605–2612, doi: 10.1007/s00268-014-2630-z (2014).
Cho, J. S., Park, M. H., Ryu, Y. J. & Yoon, J. H. The neutrophil to lymphocyte ratio can discriminate anaplastic thyroid cancer against poorly or well differentiated cancer. Annals of surgical treatment and research 88, 187–192, doi: 10.4174/astr.2015.88.4.187 (2015).
Wells, G. et al. The Newcastle–Ottawa Scale (NOS) for assessing the quality of nonrandomised studies in meta-analyses 2010 (2011).
Gu, X. B., Tian, T., Tian, X. J. & Zhang, X. J. Prognostic significance of neutrophil-to-lymphocyte ratio in non-small cell lung cancer: a meta-analysis. Scientific reports 5, 12493, doi: 10.1038/srep12493 (2015).
Moher, D., Liberati, A., Tetzlaff, J., Altman, D. G. & Group, P. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Bmj 339, b2535, doi: 10.1136/bmj.b2535 (2009).
Acknowledgements
This work was supported by the Medical Association of Sichuan Province(No. S15077).
Author information
Authors and Affiliations
Contributions
The experiments were conceived and designed by J.F. Liu, B. Luo, and H. Lv. The experiments were performed by J.F. Liu, B. Luo, D. Lv, and H. Lv. In addition, J.T. Du, X.M. Jing, N.J. Yang, C. Li, and S.X. Wang analyzed the data. The reagents, materials, and tools of analysis were contributed by J.T. Du, S.X. Wang, and X.X. Li. The paper was written by J.F. Liu, B. Luo, C. Li, and H. Lv. The full-text articles were retrieved by X.X.L.
Ethics declarations
Competing interests
The authors declare no competing financial interests.
Rights and permissions
This work is licensed under a Creative Commons Attribution 4.0 International License. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in the credit line; if the material is not included under the Creative Commons license, users will need to obtain permission from the license holder to reproduce the material. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/
About this article
Cite this article
Liu, JF., Ba, L., Lv, H. et al. Association between neutrophil-to-lymphocyte ratio and differentiated thyroid cancer: a meta-analysis. Sci Rep 6, 38551 (2016). https://doi.org/10.1038/srep38551
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/srep38551
This article is cited by
-
Role of neutrophil-to-lymphocyte ratio and platelet-to-lymphocyte ratio as potential biomarkers in Behçet’s disease: a meta-analysis
Zeitschrift für Rheumatologie (2024)
-
Platelet lymphocyte ratio, lymphocyte monocyte ratio, mean platelet volume, and neutrophil lymphocyte ratio in Behcet’s disease and their relation to disease activity
Egyptian Rheumatology and Rehabilitation (2023)
-
Multimodal data-driven prognostic model for predicting new-onset ST-elevation myocardial infarction following emergency percutaneous coronary intervention
Inflammation Research (2023)
-
Diagnostic and prognostic value of blood inflammation and biochemical indicators for intrahepatic cholestasis of pregnancy in Chinese pregnant women
Scientific Reports (2022)
-
Delta Neutrophil Index and Neutrophil‐to‐Lymphocyte Ratio in the Differentiation of Thyroid Malignancy and Nodular Goiter
World Journal of Surgery (2021)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.