Abstract
Epidemiologic and clinical data suggest that Helicobacter pylori infection is a contributing factor in the progression of atherosclerosis. However, the specific cardiovascular disease risk factors associated with H. pylori remain unclear. We performed a cross-sectional study of 37,263 consecutive healthy subjects who underwent a routine health check-up. In multivariable log Poisson regression models adjusted for potential confounders, the associations of H. pylori seropositivity with higher LDL-C (relative risk [RR], 1.21; 95% confidence interval [CI], 1.12–1.30) and lower HDL-C level (RR, 1.10; 95% CI, 1.01–1.18) were significant and independent. In multiple linear regression analyses, H. pylori infection was significantly associated with higher total cholesterol level (coefficient = 2.114, P < 0.001), higher LDL-C level (coefficient = 3.339, P < 0.001), lower HDL-C level (coefficient = −1.237, P < 0.001), and higher diastolic blood pressure (coefficient = 0.539, P = 0.001). In contrast, H. pylori infection was not associated with obesity-related parameters (body mass index, waist circumference), glucose tolerance (fasting glucose, glycated hemoglobin), and systolic blood pressure. We found that H. pylori infection was significantly and independently associated with dyslipidemia, but not with other cardiometabolic risk factors, after adjusting for potential risk factors of atherosclerosis.
Similar content being viewed by others
Introduction
Helicobacter pylori colonizes the stomach of at least half the world’s population and is a key constituent of the human microbiome. Infection is usually acquired early in life and, when left untreated, persists throughout the life of the host1,2. Clinical manifestations of H. pylori infection include peptic ulcer disease, non-cardia gastric adenocarcinoma, and gastric mucosa-associated lymphoid tissue lymphoma. Nonetheless, most individuals with H. pylori infection remain asymptomatic throughout life despite chronic gastritis1,3,4.
Over the past few decades, a large amount of epidemiologic and clinical data regarding associations with non-gastric systemic diseases and H. pylori infection have been reported, including cardiovascular disease and its risk factors5,6,7. A number of epidemiologic studies report a significant correlation of cardiovascular disease or its risk factors with H. pylori infection6,8,9,10,11. However, the results of several other studies failed to confirm the association12,13,14. The inconsistent findings of these studies may be explained by varying study methodologies, such as different study population, limited sample size, or inadequate consideration of potential confounders. In particular, most previous studies did not controll for socioeconomic status, which is significantly related with prevalence of H. pylori infection15,16. Moreover, socioeconomic status, especially education level, is a significant predictor for cardiovascular disease and its risk factors17.
In addition, there are several studies regarding the role of H. pylori in risk factors of cardiovascular disease including type 2 diabetes, hypertension, dyslipidemia, obesity or metabolic syndrome5,7,18,19,20. However, only a few studies have investigated the relationships of H. pylori infection with each risk factor of cardiovascular disease. Therefore, we aimed to assess the association between H. pylori infection and each cardiometabolic risk factors in a large asymptomatic population, with control for potential confounders.
Results
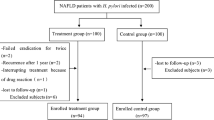
Clinical and demographic characteristics according to H. pylori serostatus
Of the 37,263 subjects, 20,932 (56.2%) were men and 16,331 (43.8%) were women, with a mean age of 49.6 years. The subjects were categorized into either H. pylori seronegative or H. pylori seropositive groups; the prevalence of H. pylori infection was 59.0%. The overall prevalence of metabolic syndrome was 12.7% (n = 4,716). The clinical and demographic characteristics of the H. pylori seropositive and seronegative groups are shown in Table 1. The proportion of men was significantly higher in the H. pylori seropositive group. The mean age of the seropositive group was higher than the seronegative group. Heavy alcohol consumers were more likely to be seropositive. Hypertension, diabetes, and dyslipidemia were more prevalent in the seropositive group. In addition, the seropositive group was more likely to exercise regularly. The values of metabolic parameters, including body mass index (BMI), waist circumference, systolic blood pressure, diastolic blood pressure, total cholesterol, low-density lipoprotein cholesterol (LDL-C), triglycerides, fasting plasma glucose (FPG), and glycated hemoglobin (HbA1c), were significantly higher in the seropositive group; high-density lipoprotein cholesterol (HDL-C) level was significantly lower in the seropositive group. In addition, the overall prevalence of metabolic syndrome was 12.7%, and the prevalence rate of metabolic syndrome was significantly higher in the seropositive group. Clinical and demographic characteristics according to metabolic syndrome status are available in supplementary Table 1.
Multivariable analyses of the association between H. pylori infection and metabolic syndrome
Possible predictors of metabolic syndrome from multivariable analysis are presented in Table 2. Factors significantly associated with the presence of metabolic syndrome included age, male sex, current smoker, BMI, body fat percentage, and alanine aminotransferase (ALT) and uric acid levels; in contrast, high education level and high income had a protective effect against metabolic syndrome. However, H. pylori seropositivity was not associated with the presence of metabolic syndrome.
Multivariable analyses of the association between H. pylori infection and each metabolic risk factor
In examining the association of H. pylori infection with each metabolic risk factor, we conducted multivariable logistic regression analysis with variables selected in univariable analysis. The selected variables included age, sex, current smoker, heavy alcohol consumer, regular exercise, education level, income, BMI, body fat rate, glomerular filtration rate (GFR), ALT, uric acid, high-sensitivity C-reactive protein (HS-CRP) levels, and H. pylori seropositivity. As shown in Table 3, H. pylori seropositivity was not a risk factor for central obesity as indicated waist circumference, higher blood pressure (BP), and higher FPG. In contrast, H. pylori seropositivity was a significant risk factor for higher LDL-C (relative risk [RR], 1.21; 95% confidence interval [CI], 1.12–1.30; P < 0.001) and lower HDL-C level (RR, 1.10; 95% CI, 1.01–1.18; P = 0.021), but was not associated with higher triglyceride level (Table 4).
Multivariable analyses of the relationship between H. pylori infection and risk factors of cardiovascular disease
The relationship of H. pylori seropositivity and cardiovascular risk factors were assessed by multiple linear regression analysis. In evaluating the relationship of H. pylori seropositivity with cardiovascular risk factors, we performed multivariable analysis after adjusting for potential confounders including age, sex, education level, income level, smoking status, alcohol consumption, and physical inactivity. H. pylori seropositivity showed a significant relationship with higher total cholesterol level (coefficient = 2.114, P < 0.001), higher LDL-C level (coefficient = 3.339, P < 0.001), lower HDL-C level (coefficient = −1.237, P < 0.001), and higher diastolic BP (coefficient = 0.539, P = 0.001; Fig. 1). In contrast, there was no positive relationship between H. pylori seropositivity and obesity-related parameters (BMI, waist circumference), glucose tolerance (FPG, HbA1c), systolic BP, and triglyceride level (Table 5).
(A) Histogram of predicted total cholesterol by H. pylori status; (B) Histogram of predicted low-density lipoprotein cholesterol by H. pylori status; (C) Histogram of predicted high-density lipoprotein cholesterol by H. pylori status; (D) Histogram of predicted diastolic blood pressure by H. pylori status
Discussion
In this large cross-sectional study of asymptomatic men and women undergoing routine health check-up, we investigated the association of H. pylori infection with risk factors for cardiovascular disease. H. pylori infection was a significant and independent risk factor for dyslipidemia including high LDL-C and low HDL-C levels, but not for other cardiovascular risk factors, after adjusting for potential confounders. These results support that H. pylori infection has a role in promoting atherosclerosis through dyslipidemia.
There is debate concerning the effect of H. pylori infection on obesity. A meta-analysis of 18 epidemiological studies involving a total of 10,000 subjects claimed a strong correlation between H. pylori infection and obesity as defined by high BMI21. In contrast, a recent systemic review of 49 studies with a total of 99,463 subjects demonstrated that the prevalence of H. pylori infection is inversely associated with the prevalence of obesity and overweight19. This result is consistent with recent observations from controlled trials that patients who underwent H. pylori eradication developed significant weight gain as compared to subjects with untreated H. pylori colonization22,23. One possible mechanism for significant weight gain after H. pylori eradication is H. pylori-induced increases in ghrelin, which signals hunger and appetite24,25. In the present study, H. pylori infection was not associated with general obesity as determined using BMI or central obesity measures such as waist circumference, after adjusting for potential confounding factors. It is interesting that central obesity, considered a core component of metabolic syndrome, was not associated with H. pylori infection.
The link between H. pylori and diabetes and glucose intolerance also remains controversial. A recent meta-analysis of 41 studies including a total of 14,080 patients revealed a higher prevalence rate of H. pylori in type 2 diabetes patients than in non-diabetic patients26. In contrast, a large well-designed study in Australia demonstrated that H. pylori infection was not different between diabetic and non-diabetic patients27,28. The discrepancies are likely due to adjustments for potential confounders, the method used to define diabetic status, and the limited sample sizes. In addition, the accuracy of self-reported data on diabetes depends on the subjects’ knowledge and understanding of the relevant information; thus, diabetes can be easily misclassified. In the present study, we used laboratory markers of diabetes, such as FPG and HbA1c, and conducted the analysis after controlling for all possible confounders. The present study found no association between H. pylori infection and glucose intolerance or diabetes mellitus.
Previous studies regarding the association of H. pylori infection with lipid metabolism showed relatively consistent evidence, but conflicting results also exist5,7,18,29,30. Especially, low socioeconomic level and crowded living conditions are important risk factors in H. pylori infection15,16. Also, low socioeconomic status tends to relate to an increased risk in dyslipidemia and cardiovascular disease9,17. Therefore, consideration of socioeconomic status as a potential confounding factor is important for studying the association of H. pylori with cardiovascular disease and its risk factors. However, most previous studies concerning the association between H. pylori and dyslipidemia controlled for socioeconomic status. In this study, we found that subjects with H. pylori infection had higher total cholesterol and LDL-C, as well as lower HDL-C, regardless of other potential confounding factors such as age, sex, socioeconomic status, BMI, smoking status, alcohol consumption, and amount of exercise. The alterations of lipid profile may be mediated by inflammatory cytokines such as interleukin-1, interleukin-6, or tumor necrosis factor-α through a chronic inflammatory condition induce by H. pylori31,32.
Metabolic syndrome is a multifactorial condition in which H. pylori infection seems to play a minor role. The prevalence of H. pylori infection is decreasing in developed countries; thus, it might not correspond with the recent increase in the global prevalence of metabolic syndrome or obesity-related morbidities33. Nevertheless, the present results elucidate the role of H. pylori infection in cardiovascular disease and its risk factors. Few studies have discussed the potentially different impacts that H. pylori infection has on each cardiovascular risk factors. Shin et al. compared the association between metabolic syndrome and H. pylori infection diagnosed by serologic and histologic status. The study found that the metabolic syndrome was more strongly associated with histologic positivity than serologic positivity. Among the cardiometabolic parameters, central obesity, low HDL-C levels, and high blood pressure were significantly associated with H. pylori infection after adjusting for age, sex, smoking status, alcohol consumption, and economic status34. In contrast, our study assessed H. pylori infection status solely with serologic test. However, we evaluated the association between H. pylori seropositivity and the cardiometabolic risk factors, paying particular attention to careful control for known risk factors and confounders including age, sex, smoking status, alcohol consumption, socioeconomic status, physical activity, and body mass index. Physical inactivity and obesity are established risk factors of metabolic syndrome and cardiovascular disease35,36,37. The current study provides evidence that H. pylori infection is associated with dyslipidemia such as higher total cholesterol and LDL-C, as well as lower HDL-C, regardless of potential confounders and putative risk factors. However, there were no evidence of the associations between H. pylori infection and other cardiovascular risk factors such as central obesity and glucose tolerance.
Several limitations need to be a considered in the interpretation of results. First, the evaluation of H. pylori infection status was done solely with serum IgG to H. pylori measured by enzyme-linked immunosorbent assay, without other laboratory assessments such as a rapid urease test or urease breath test. Accordingly, the possibility of false-negative or false-positive results cannot be completely excluded. However, the serum IgG antibody test to H. pylori is a relative highly sensitive and cheap mass screening tool that can be used easily in areas with a high prevalence of H. pylori infection. Second, although we measured for several important confounding factors in the multivariable analysis, we cannot exclude the possibility of residual confounders due to factors measured with error or unmeasured factors such as dietary factors.
In this large cross-sectional study, after adjusting for potential confounding factors, H. pylori infection was significantly and independently associated with dyslipidemia, including higher total cholesterol and LDL-C and lower HDL-C levels, but not with other cardiovascular risk factors. A larger body of evidence implies that H. pylori infection is a causal risk factor for cardiovascular disease; the current study provides strong evidence that H. pylori modifies the lipid profile that eventually promotes atherosclerosis. Eradication of H. pylori should be considered for patients with H. pylori infection and dyslipidemia, particularly in groups at high risk for cardiovascular disease.
Methods
Study population
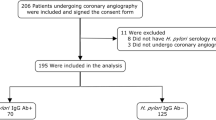
We performed a cross-sectional study of healthy subjects who underwent a routine health check-up, including an H. pylori-specific immunoglobulin G antibody (IgG) test, at the Center for Health Promotion, Samsung Medical Center in South Korea. Regular health check-ups are very common in South Korea owing to the Industrial Safety and Health Law; the National Cancer Screening Program recommends biennial health examinations, including for several cancers38.
This study included 38,426 consecutive healthy subjects who underwent a health screening examination with serum IgG anti-H. pylori test between January 2004 and December 2007. Those who had missing data (n = 1,163; e.g., BP, FBG, LDL-C, HDL-C, triglycerides, waist circumference, and BMI) or had a history of cancer were excluded, resulting in a final sample of 37,263 subjects. This study was approved by the Institutional Review Board of the Samsung Medical Center and was conducted in accordance with the Declaration of Helsinki. The Institutional Review Board approval was obtained without specific informed consent because the study used only de-identified data that were collected for clinical purposes as part of the health screening check-up. However, informed consent was obtained from all subjects for their examinations at the health check-up.
Data collection
The comprehensive health screening program included demographic characteristics, anthropometric data, serum biochemical measurements, and an epidemiological questionnaire assessing smoking, alcohol consumption, physical activity, education level, income, medication history, and personal medical history39. The personal medical histories were used to collect information regarding history of hypertension, diabetes mellitus, dyslipidemia, and cardiovascular and cerebrovascular disease. Education levels were stratified as low (elementary school or less), medium (middle or high school), or high (college or higher) and income was stratified into tertiles (lowest tertile, middle tertile, highest tertile). The medication history included current and regular use of medications for hypertension, diabetes, and dyslipidemia. Height and weight were measured in the morning to the nearest 0.1 kg and 0.1 cm, respectively; the measurements were taken with subjects wearing light clothing and barefoot. BMI was calculated as weight in kilograms divided by height in square meters (kg/m2), and waist circumference was measured, in a horizontal plane, half way between the lowest margin of the twelfth rib and the superior iliac crest. Body fat percentage was measured using bioelectrical impedance analysis (Inbody 720 machine, Biospace, Seoul, Korea). Systolic BP and diastolic BP were measured after the subjects rested for at least 5 minutes in a sitting position. Smoking status was assessed as never smoker, former smoker, or current smoker; alcohol consumption was assessed as never or occasionally (once or twice per month), once or twice per week, three or four times per week, or five or more times per week. Regular exercise was defined as physical activity of at least moderate intensity at least 30 minutes ≥3 days per week.
After a ≥12 hours fast, fasting blood samples were obtained from the antecubital vein, and were used to determine the serum levels of FPG, HbA1c, total cholesterol, LDL-C, and HDL-C, triglycerides, and HS-CRP. HbA1c was measured by using a high-performance liquid chromatography method with a Tosoh Glycohemoglobin Analyzer (Tosoh Bioscience Inc, Tokyo, Japan). Serum glucose was measured by using the hexokinase/glucose-6-phosphate dehydrogenase method with a Hitachi 7600 Modular Dp-110 autoanalyzer (Hitachi, Tokyo, Japan). Total cholesterol, LDL-C, HDL-C, and triglycerides were measured by using enzymatic or colorimetric methods. Serum IgG antibody to H. pylori was measured by an enzyme-linked immunosorbent assay, GAP test IgG kit (Bio-Rad Laboratories Inc, Hercules, Calif). H. pylori infection was defined as a positive enzyme-linked immunosorbent assay result.
The definition of metabolic syndrome was based on the NCEP ATP III criteria except for the cut off values of waist circumference, which were defined according to the Korean Society for the Study of Obesity40,41. Individuals with at least three of the following five traits were classified as having metabolic syndrome: (1) central obesity, defined as a waist circumference ≥90 cm for men and ≥85 cm for women; (2) high serum triglycerides, defined as ≥ mg/dL (1.7 mmol/L) or drug treatment for this lipid abnormality; (3) low HDL-C, defined as ≤40 mg/dL (1.0 mmol/L) for men and ≤50 mg/dL (1.3 mmol/L) for women or drug treatment for this lipid abnormality; (4) high BP, defined as BP ≥130/85 mmHg or drug treatment for previously diagnosed hypertension; and (5) high FPG, defined as >100 mg/dL (5.6 mmol/L) or drug treatment for previously diagnosed diabetes.
Statistical analysis
Continuous variables are reported as means ± standard deviation, whereas categorical variables are presented as percentages. Continuous variables were compared between groups using the Wilcoxon rank sum test, whereas categorical variables were compared using the chi-squared test. The associations of H. pylori seropositivity with traditional risk factors of atherosclerosis and each factor of metabolic syndrome were assessed by means of relative risks (RRs) with 95% confidence intervals (CIs) using univariable and multivariable log Poisson regression analyses. Variables with P value <0.1 in the univariable analysis were selected for the multivariable analysis. The variables used for the multivariable analysis included age, sex, education level, income, BMI, body fat percentage, smoking status, alcohol consumption, physical activity, GFR, ALT, HS-CRP. The relationship between H. pylori seropositivity and each risk factor of atherosclerosis was then investigated using multiple linear regression analysis after adjusting for potential confounders including age, sex, education level, income, smoking status, alcohol consumption, and physical activity. A P-value <0.05 was considered statistically significant; statistical analyses were performed using SAS version 9.4 (SAS Institute, Cary, NC).
Additional Information
How to cite this article: Kim, T. J. et al. Helicobacter pylori is associated with dyslipidemia but not with other risk factors of cardiovascular disease. Sci. Rep. 6, 38015; doi: 10.1038/srep38015 (2016).
Publisher's note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
Ernst, P. B., Peura, D. A. & Crowe, S. E. The translation of Helicobacter pylori basic research to patient care. Gastroenterology 130, 188–206 (2006).
Everhart, J. E. Recent developments in the epidemiology of Helicobacter pylori. Gastroenterol Clin North Am 29, 559–578 (2000).
Schubert, M. L. & Peura, D. A. Control of gastric acid secretion in health and disease. Gastroenterology 134, 1842–1860 (2008).
Suerbaum, S. & Michetti, P. Helicobacter pylori infection. N Engl J Med 347, 1175–1186 (2002).
Gunji, T. et al. Helicobacter pylori infection is significantly associated with metabolic syndrome in the Japanese population. Am J Gastroenterol 103, 3005–3010 (2008).
Ozdogru, I. et al. The relationship between Helicobacter pylori IgG titre and coronary atherosclerosis. Acta Cardiol 62, 501–505 (2007).
Satoh, H., Saijo, Y., Yoshioka, E. & Tsutsui, H. Helicobacter Pylori infection is a significant risk for modified lipid profile in Japanese male subjects. J Atheroscler Thromb 17, 1041–1048 (2010).
Laek, B. et al. The prospective association of Chlamydia pneumoniae and four other pathogens with development of coronary artery calcium: the multi-ethnic study of atherosclerosis (MESA). Atherosclerosis 230, 268–274 (2013).
Mendall, M. A. et al. Relation of Helicobacter pylori infection and coronary heart disease. Br Heart J 71, 437–439 (1994).
Park, M. J. et al. Association between Helicobacter pylori Seropositivity and the Coronary Artery Calcium Score in a Screening Population. Gut Liver 5, 321–327 (2011).
Tsai, C. J. & Huang, T. Y. Relation of Helicobacter pylori infection and angiographically demonstrated coronary artery disease. Dig Dis Sci 45, 1227–1232 (2000).
Gillum, R. F. Infection with Helicobacter pylori, coronary heart disease, cardiovascular risk factors, and systemic inflammation: the Third National Health and Nutrition Examination Survey. J Natl Med Assoc 96, 1470–1476 (2004).
Rothenbacher, D. et al. Helicobacter pylori heat shock protein 60 and risk of coronary heart disease: a case control study with focus on markers of systemic inflammation and lipids. Atherosclerosis 156, 193–199 (2001).
Sotiropoulos, A. et al. Seropositivity to Chlamydia pneumoniae or Helicobacter pylori and coronary artery disease. Int J Cardiol 109, 420–421 (2006).
Malaty, H. M. & Graham, D. Y. Importance of childhood socioeconomic status on the current prevalence of Helicobacter pylori infection. Gut 35, 742–745 (1994).
Moayyedi, P. et al. Relation of adult lifestyle and socioeconomic factors to the prevalence of Helicobacter pylori infection. Int J Epidemiol 31, 624–631 (2002).
Winkleby, M. A., Jatulis, D. E., Frank, E. & Fortmann, S. P. Socioeconomic status and health: how education, income, and occupation contribute to risk factors for cardiovascular disease. Am J Public Health 82, 816–820 (1992).
Chen, T. P. et al. Helicobacter Pylori Infection is Positively Associated with Metabolic Syndrome in Taiwanese Adults: a Cross-Sectional Study. Helicobacter 20, 184–191 (2015).
Hsieh, M. C. et al. Helicobacter pylori infection associated with high HbA1c and type 2 diabetes. Eur J Clin Invest 43, 949–956 (2013).
Polyzos, S. A., Kountouras, J., Zavos, C. & Deretzi, G. The association between Helicobacter pylori infection and insulin resistance: a systematic review. Helicobacter 16, 79–88 (2011).
Danesh, J. & Peto, R. Risk factors for coronary heart disease and infection with Helicobacter pylori: meta-analysis of 18 studies. BMJ 316, 1130–1132 (1998).
Lane, J. A. et al. Randomised clinical trial: Helicobacter pylori eradication is associated with a significantly increased body mass index in a placebo-controlled study. Aliment Pharmacol Ther 33, 922–929 (2011).
Kamada, T., Sugiu, K. & Haruma, K. Development of obesity and hyperlipidemia after eradication of Helicobacter pylori. Nihon Rinsho 63 Suppl 11, 536–538 (2005).
Isomoto, H. et al. The Relationship between Plasma and Gastric Ghrelin Levels and Strain Diversity in Helicobacter pylori Virulence. Am J Gastroenterol 100, 1425–1427 (2005).
Azuma, T. et al. Gastric leptin and Helicobacter pylori infection. Gut 49, 324–329 (2001).
Zhou, X., Zhang, C., Wu, J. & Zhang, G. Association between Helicobacter pylori infection and diabetes mellitus: a meta-analysis of observational studies. Diabetes Res Clin Pract 99, 200–208 (2013).
Xia, H. H. et al. Helicobacter pylori infection is not associated with diabetes mellitus, nor with upper gastrointestinal symptoms in diabetes mellitus. Am J Gastroenterol 96, 1039–1046 (2001).
Dore, M. P. et al. Diabetes mellitus and Helicobacter pylori infection. Nutrition 16, 407–410 (2000).
Elizalde, J. I. et al. Influence of Helicobacter pylori infection and eradication on blood lipids and fibrinogen. Aliment Pharmacol Ther 16, 577–586 (2002).
Adiloglu, A. K., Can, R., Kinay, O. & Aridogan, B. C. Infection with Chlamydia pneumoniae but not Helicobacter pylori is related to elevated apolipoprotein B levels. Acta Cardiol 60, 599–604 (2005).
Georges, J. L. et al. Impact of pathogen burden in patients with coronary artery disease in relation to systemic inflammation and variation in genes encoding cytokines. Am J Cardiol 92, 515–521 (2003).
Feingold, K. R. & Grunfeld, C. Role of cytokines in inducing hyperlipidemia. Diabetes 41 Suppl 2, 97–101 (1992).
Lender, N. et al. Review article: Associations between Helicobacter pylori and obesity--an ecological study. Aliment Pharmacol Ther 40, 24–31 (2014).
Shin, D. W. et al. Association between metabolic syndrome and Helicobacter pylori infection diagnosed by histologic status and serological status. J Clin Gastroenterol 46, 840–845 (2012).
Faam, B. et al. Leisure-time physical activity and its association with metabolic risk factors in Iranian adults: Tehran Lipid and Glucose Study, 2005–2008. Prev Chronic Dis 10, E36 (2013).
Ahmed, H. M., Blaha, M. J., Nasir, K., Rivera, J. J. & Blumenthal, R. S. Effects of physical activity on cardiovascular disease. Am J Cardiol 109, 288–295 (2012).
Grundy, S. M. Obesity, metabolic syndrome, and cardiovascular disease. J Clin Endocrinol Metab 89, 2595–2600 (2004).
Kim, Y., Jun, J. K., Choi, K. S., Lee, H. Y. & Park, E. C. Overview of the National Cancer screening programme and the cancer screening status in Korea. Asian Pac J Cancer Prev 12, 725–730 (2011).
Rampal, S. et al. Association between markers of glucose metabolism and risk of colorectal adenoma. Gastroenterology 147, 78–87, e73 (2014).
Alberti, K. G. et al. Harmonizing the metabolic syndrome: a joint interim statement of the International Diabetes Federation Task Force on Epidemiology and Prevention; National Heart, Lung, and Blood Institute; American Heart Association; World Heart Federation; International Atherosclerosis Society; and International Association for the Study of Obesity. Circulation 120, 1640–1645 (2009).
Lee, S. Y. et al. Appropriate waist circumference cutoff points for central obesity in Korean adults. Diabetes Res Clin Pract 75, 72–80 (2007).
Author information
Authors and Affiliations
Contributions
H.L.: Study concept and design. T.J.K., M.K., J.E.K., Y.W.M., and B.H.M.: Acquisition, analysis, or interpretation of data. T.J.K.: Drafting of the manuscript. J.H.L., H.J.S., Y.H.C., and P.L.R.: Critical revision of the manuscript for important intellectual content. S.Y.B. and S.H.A.: Statistical analysis. P.L.R. and J.J.K.: Study supervision.
Ethics declarations
Competing interests
The authors declare no competing financial interests.
Rights and permissions
This work is licensed under a Creative Commons Attribution 4.0 International License. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in the credit line; if the material is not included under the Creative Commons license, users will need to obtain permission from the license holder to reproduce the material. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/
About this article
Cite this article
Kim, T., Lee, H., Kang, M. et al. Helicobacter pylori is associated with dyslipidemia but not with other risk factors of cardiovascular disease. Sci Rep 6, 38015 (2016). https://doi.org/10.1038/srep38015
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/srep38015
This article is cited by
-
Relationship between active Helicobacter pylori infection and risk factors of cardiovascular diseases, a cross-sectional hospital-based study in a Sub-Saharan setting
BMC Infectious Diseases (2022)
-
Association between Helicobacter pylori infection and non-alcoholic fatty liver disease in North Chinese: a cross-sectional study
Scientific Reports (2019)
-
Positive Association Between Helicobacter pylori Infection and Metabolic Syndrome in a Korean Population: A Multicenter Nationwide Study
Digestive Diseases and Sciences (2019)
-
Lipid testing in infectious diseases: possible role in diagnosis and prognosis
Infection (2017)
-
A cohort study on Helicobacter pylori infection associated with nonalcoholic fatty liver disease
Journal of Gastroenterology (2017)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.