Abstract
Prospective epidemiologic studies that investigated the association between body mass index (BMI) and non-melanoma skin cancer (NMSC) yielded inconsistent findings. A dose-response meta-analysis was conducted to quantitatively summarize the evidence. PubMed and Embase databases were searched for relevant studies. Study-specific relative risk (RR) and 95% confidence interval (CI) for an increase in BMI of 5 kg/m2 was computed with the generalized least squares trend estimation, and these risk estimates were combined with the random-effects model. Nine publications were included in the final analyses, consisting of 18 independent cohorts with 22 risk estimates (971,795 participants and 50,561 NMSC cases). Results of the dose-response analyses showed a nonlinear inverse relationship between BMI and NMSC (RR = 0.88, 95% CI: 0.85–0.91, I2 = 71.2%, P-nonlinearity <0.001), which persisted when limiting to the studies with adjustment for important potential confounders including sun exposure and sensitivity factors. The risk estimates were very similar for squamous cell carcinoma and basal cell carcinoma. Sex appeared a source of heterogeneity (P-difference = 0.06), with a weaker, but still significant inverse association in men than in women. This dose-response meta-analysis suggests a nonlinear inverse association between BMI and NMSC.
Similar content being viewed by others
Introduction
Non-melanoma skin cancer (NMSC), generally referring to squamous cell carcinoma (SCC) and basal cell carcinoma (BCC), ranks the most frequently diagnosed cancer worldwide. Unlike other cancers for which the incidence rates has become stabilized or declined, the incidence of NMSC is still increasing, in particular among younger populations1,2. Although the mortality rate of NMSC is much lower than that of melanoma, the high incidence lead to a considerable number of cases, and therefore an important challenge in health management and enormous burden in terms of healthcare costs3. In the US alone, it is estimated that in 2012 there were more than 5.4 million NMSCs and 3.3 million persons treated for NMSC2. More than 80% of NMSC incidence could be attributed to ambient ultraviolet (UV) radiation4, and several host features such as fair skin, red hair, melanocytic nevi, and family history have also been identified as risk factors5,6. The effectiveness of skin cancer screening on reducing mortality is suggested to be low7. Thus, identifying other exposures, especially modifiable factors (e.g., diet and lifestyle) that influence the risk for this malignancy is important for reducing the public health burden.
Obesity, as measured by body mass index (BMI), is an established risk factor for various chronic diseases such as type 2 diabetes, cardiovascular disease, and cancers at various sites, as well as all-cause mortality8. Regarding the association with skin cancer, previous meta-analyses reported increased risk of melanoma associated with a higher BMI in men but not in women5,9. Given that melanoma and NMSC share risk factors5, it is plausible that excess body weight would also be associated with NMSC risk. There have been a number of prospective observational studies that investigated this association, but their findings are inconsistent10,11,12,13,14,15,16,17,18. Indeed, some10,11,16,18, but not other studies12,13,14,15 have demonstrated an unexpectedly inverse association between measured/self-reported BMI and NMSC risk. The reasons for the heterogeneity among these studies are unclear, and whether there is a dose-response association, or whether such an inverse association is simply explained by confounders of sun exposure and sensitivity measures remain to be elucidated (obese individuals have less sun exposure than lean ones because of a lower frequency of outdoors18). Therefore, we performed a dose-response meta-analysis of prospective studies to investigate the relationship between BMI and risk of NMSC.
Methods
Literature search
Potentially relevant publications were searched on PubMed and Embase databases from inception to 30 June, 2016. The detailed literature search strategy is reported in Supplementary Table S1, with core search involving NMSC and its subtype (SCC and BCC), anthropometric factors, and study design. The references of retrieved full publications were also carefully hand searched for additional studies.
Study selection
Studies were eligible for inclusion if they met the following criteria: (1) the study design was prospective (e.g., prospective cohort, nested case-control, or case-cohort design); (2) the exposure of interest was BMI (in kg/m2), or obesity status measured by BMI; (3) the outcome of interest was NMSC or its subtype; and (4) relative risks (RRs) and 95% confidence intervals (CIs) were reported for continuous BMI (e.g., per unit increase), or for at least 3 quantitative categories of BMI. When the same study was reported in overlapping publications, the one containing the largest number of NMSCs was included.
Data extraction and quality assessment
For study included, the following characteristics were collected a standardized data-collection form: the first author’s last name, publication year, study name, country, average (mean or median) duration of follow-up, sex and age of participants, number of cases and participants, methods for BMI measurement, categories of BMI with corresponding RR and 95% CI, and potential confounders accounted for in the statistical analyses. Two authors (ZD and LG) independently conducted literature search, study selection, and data abstraction, with any disagreement resolved by consensus. Instead of assessing methodologic quality of the primary studies by a quality score, we investigated whether the summary risk estimates were significantly influenced by some study and population characteristics (e.g., follow-up duration, method for exposure assessment, and adjustment for important confounders) which may be indicators of study quality19.
Statistical analysis
In this meta-analysis, we used the most fully adjusted risk estimates, and reported summary RR of NMSC for each 5 kg/m2 increase in BMI. When only results for categorized BMI were reported, the method of generalized least squares trend estimation proposed by Greenland and Longnecker20 and Orsini et al.21 was employed to estimate study-specific slopes and 95% CIs from the correlated logs of the RRs and CIs across BMI categories. Accordingly, categorized BMI values, distributions of cases and person-years, and RRs with 95% CIs were extracted from each study. When the number of cases or person-years in each exposure category was not reported, the data were estimated from total number of cases or person-years. The median or mean BMI in each category were used as the average levels. When the median or mean value per category was not reported, the midpoint of the upper and lower boundaries was considered average values. If the highest or lowest category was open-ended, the width of the interval was assumed to be the same as in the closest category. Afterward, study-specific risk estimates were combined with a random-effects model, taking into account both within- and between-study variation22. Results presented by sex or by NMSC subtype in original studies were treated as independent reports.
To explore potential sources of heterogeneity, subgroup analyses were performed by geographic area, sex of participants, NMSC subtype (SCC and BCC), methods for BMI measurement, and adjustment for important confounders. Further sex-specific analyses were conducted for SCC and BCC. A potential nonlinear association between BMI and risk of NMSC were investigated using restricted cubic splines with three knots at percentiles 10%, 50%, and 90% of the distribution23. A P value for non-linearity was calculated by testing the null hypothesis that the coefficient of the second spline is equal to 0. Heterogeneity among studies was assessed with the Q and I2 statistics24. For the Q statistic, a P < 0.1 was considered significant heterogeneity. Potential publication bias was assessed by a combination of Begg rank correlation test, Egger linear regression test, and Begg’s funnel plot25,26. All analyses were performed using STATA12.0.
Results
Study selection and characteristics
The flow diagram of study selection is reported in Supplementary Figure S1. Our initial search yielded 1215 independent citations, of which 32 full publications remained after title and/or abstract reading. Twenty three of these full publications were rejected mainly because of a retrospective study design, or a lack of results reported for BMI and/or NMSC. Of note, 1 report27 was excluded because only results for total skin cancer were available, and another report28 was excluded because the same study population was used in a later publication16 with larger events.
Finally, 9 publications10,11,12,13,14,15,16,17,18 that evaluated the association of BMI with risk of NMSC were included in this meta-analysis, consisting of 1 nested case-control study13 of sex-same twins, 1 pooled analysis14 of 7 cohorts from 3 European countries, 1 pooled analysis10 of 2 cohorts (the Copenhagen General Population Study and the Copenhagen City Heart Study), and 7 independent prospective cohort studies11,12,15,16,17,18 (the Health Professionals Follow-up Study and the Nurses’ Health Study were reported in 1 publication16). Therefore, a total of 18 cohorts were included in this meta-analysis, consisting of 22 independent reports with 971,795 participants and 50,561 NMSC cases (3332 SCC and 33,721 BCC). The primary studies were mostly from Europe10,13,14,17 or US11,16,18, with the exceptions of 2 Australia studies12,15. BMI was either self-reported, or measured by investigators. The study duration, sample size, and potential confounders adjusted for varied substantially among individual studies. Three of the original studies were observational analyses of clinical trials on cancer prevention (skin cancer12,15 or female breast cancer18). The characteristics of the included studies are reported in Supplementary Table S2.
Overall analyses
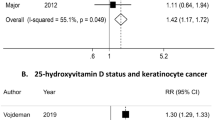
A dose-response meta-analysis of the included studies showed that the summary RR of NMSC was 0.88 (95% CI: 0.85–0.91) for each 5 kg/m2 increase in BMI, with considerable heterogeneity (Pheterogeneity < 0.001, I2 = 71.2%) (Fig. 1A). There was evidence of a nonlinear relationship between BMI and risk of NMSC, with the curve becoming steeper and almost linear after the BMI of 28 kg/m2 (Fig. 1B). Both Begg rank correlation test and Egger linear regression test suggested little evidence of publication bias (both P values > 0.50), which was supported by a visual inspection of the Begg funnel plot that showed no obvious asymmetry (Supplementary Figure S2).
Subgroup and sensitivity analyses
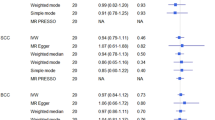
Results of subgroup analysis performed to explore potential sources of heterogeneity according to pre-specified factors are reported in Table 1. The magnitude of the association was very similar for SCC and BCC. There was evidence that geographic area partly contributed to the heterogeneity amongst studies, with an inverse BMI-NMSC association among US and European studies, but not among studies from Australia (Pdifference = 0.05 when comparing European and Australia studies). There also a suggestion of an effect modification by sex (Pdifference = 0.06), with a weaker but still significant association in men than in women (Fig. 1A and Table 1). This sex-specific difference appeared more evident for SCC than for BCC (Fig. 2, Fig. 3 and Table 1). There was evidence that the association varied by whether adjustment for alcohol consumption had been made (Pdifference = 0.004), but only 3 reports were included in the group with adjustment. Of note, the association did not differ according to adjustment or not for several well known risk factors for NMSC such as family history and indicators of sun exposure and sun sensitivity. Excluding the 3 studies (7 reports) where participants were generated from clinical prevention trials, the summary RR was 0.86 (95% CI: 0.83–0.90), with substantial heterogeneity (I2 = 77.0%).
Discussion
In this dose-response meta-analysis of prospective studies involving 18 independent cohorts with nearly 1 million participants and over 50,000 NMSC cases, we found that BMI was nonlinearly, inversely associated with risk of NMSC. The association was similar for SCC and BCC, and persisted when limiting to the studies with adjustment for important potential confounders including sun exposure and sun sensitivity measures. We also found that the inverse association in women was more evident than in men.
Potential biological mechanisms under the observed inverse association between BMI and NMSC risk are poorly understood. Some investigators attributed this association to the residual confounding by sun exposure16,17,18. Obese compared with lean individuals are less active outdoor, and therefore less sun exposure18, leading to a lower risk of NMSC. However, our meta-regression analyses suggested that neither adjustment for physical activity, nor adjustment for sun exposure and sensitivity significantly influenced the magnitude of the association. Moreover, UV radiation appears to affect SCC more strongly than on BCC29,30,31. If the inverse BMI-NMSC association could be simply explained by residual confounder of sun exposure, per unit increase in BMI would be expected to be associated with greater reductions in SCC than in BCC. However, risks of SCC and BCC associated with increasing BMI were very similar in this meta-analysis. Using a Mendelian randomization design is an approach to exclude potential confounders. There is only 1 prospective study that used such a design, showing that an increase in genetically determined BMI of 10 kg/m2 was non-significantly inversely associated with NMSC risk (RR = 0.71, 95% CI: 0.26–1.93)10.
Gerstenblith et al.11 argued that adipose tissue related high estrogen may partly be responsible for the inverse association of BMI with NMSC risk. We considered, but not limited to the following evidence that supports this argument: (1) women relative to men have much lower risk of NMSC32, suggesting that women may have some protections; (2) animal studies showed that withdrawal of ovary dramatically increased susceptibility to NMSC in female mice33, and estrogen receptor-β agonist remarkably decreased UV-induced skin cancer34; and (3) There is evidence that estrogen may promote wound healing and delay or even reverse skin aging through multiple mechanisms (e.g., reduction of inflammation and oxidative damage)35,36. Another hormone that is significantly higher in women than in men is adipokine, leptin, which has also been suggested to promote wound repair in the skin (e.g., by accelerating proliferation and enhancing angiogenesis around the wounded)37, and to improve, preserve and restore skin regeneration38. For men and women having an equivalent amount of excess weight, women carry more subcutaneous fat which a major producer of leptin, and this might partly explain the sex-specific difference in the association of BMI with NMSC risk in this study.
Evidence from case-control studies on BMI and NMSC has been limited, and some also suggested a sex-specific difference. In a small, hospital-based case-control study of 77 NMSC39, being obese was inversely associated with BCC (odds ratios [OR] = 0.53, 95% CI: 0.05–5.24), but was positively associated with total NMSC (OR = 1.51, 95% CI: 0.27–8.50). In another hospital-based study of 528 BCC40, women in the fourth quartile of BMI had a 34% (OR = 0.66, 95% CI: 0.35–1.22) non-significantly lower risk of BCC as compared with women in the first quartile, whereas the corresponding OR for men was 0.97 (95% CI: 0.58–1.63). In a population-based case-control study of 1276 NMSC41, obesity was associated with a non-significant increase in risk of NMSC in men (OR = 1.25, 95% CI: 0.94–1.64); conversely, a trend towards reduced risk was found in women (OR = 0.79, 95% CI: 0.62–1.01).
This meta-analysis presents several strengths. Limiting our analyses to prospective studies eliminated reverse causality because BMI was determined before the diagnosis of cancer. The large number of cases strengthened the statistical power to detect a weak association. Our linear and nonlinear dose-response analyses enabled us to better understand the shape of the association. Moreover, the stability of our results was supported by the stratified analyses according to various important study characteristics. Heterogeneity and publication bias are two important concerns for a meta-analysis of published literature, because different studies would vary by population and methodological characteristics, and small studies with null results have less chance to be published. However, with commonly used statistical methods, we found little evidence of publication bias. We were also able to identify potential sources of heterogeneity by performing meta-regression analyses.
However, this study is not without limitations. As a meta-analysis of observational studies, the problem of potential confounders is the first consideration. Although the summary risk estimates were not altered when restricting to the studies with sun exposure and sensitivity adjustment, residual confounding arising from measurement errors of sun exposure (and also other factors) remained. Original studies generally used self-reported questionnaires to collect lifestyle information, and the way in which they asked about the duration and density of the exposure varied across different questionnaires; moreover, other problems such as the use of sunscreen and the degree to which clothing covers the body surface were less or not considered in these cohorts. Therefore, future prospective studies with more accurate measures of factors related to both BMI and sun exposure, and those studies using a Mendelian randomization design are needed to further address the impacts of these confounders on the association.
In summary, findings from this meta-analysis of prospective studies suggest that BMI is nonlinearly and inversely association with risk of NMSC. The inverse association is similar with SCC and BCC, but it appears stronger in women than in men. Potential mechanism underlying the association remains to be determined. Despite that we and others have observed lower risks of specific cancers (e.g., NMSC and lung cancer42) associated with a higher BMI, these findings should not affect current preventive strategies on obesity, which is an important cause of serious public health concerns worldwide8.
Additional Information
How to cite this article: Zhou, D. et al. Body mass index and risk of non-melanoma skin cancer: cumulative evidence from prospective studies. Sci. Rep. 6, 37691; doi: 10.1038/srep37691 (2016).
Publisher's note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
Deady, S., Sharp, L. & Comber, H. Increasing skin cancer incidence in young, affluent, urban populations: a challenge for prevention. Br J Dermatol 171, 324–31 (2014).
Rogers, H. W., Weinstock, M. A., Feldman, S. R. & Coldiron, B. M. Incidence Estimate of Nonmelanoma Skin Cancer (Keratinocyte Carcinomas) in the U.S. Population, 2012. JAMA Dermatol 151, 1081–6 (2015).
Cakir, B. O., Adamson, P. & Cingi, C. Epidemiology and economic burden of nonmelanoma skin cancer. Facial Plast Surg Clin North Am 20, 419–22 (2012).
Xiang, F., Lucas, R., Hales, S. & Neale, R. Incidence of nonmelanoma skin cancer in relation to ambient UV radiation in white populations, 1978-2012: empirical relationships. JAMA Dermatol 150, 1063–71 (2014).
Linares, M. A., Zakaria, A. & Nizran, P. Skin Cancer. Prim Care 42, 645–59 (2015).
Wu, S., Han, J., Laden, F. & Qureshi, A. A. Long-term ultraviolet flux, other potential risk factors, and skin cancer risk: a cohort study. Cancer Epidemiol Biomarkers Prev 23, 1080–9 (2014).
Wernli, K. J. et al. Screening for Skin Cancer in Adults: Updated Evidence Report and Systematic Review for the US Preventive Services Task Force. JAMA 316, 436–47 (2016).
Global, B. M. I. M. C. Body-mass index and all-cause mortality: individual-participant-data meta-analysis of 239 prospective studies in four continents. Lancet 388, 776–86 (2016).
Renehan, A. G., Tyson, M., Egger, M., Heller, R. F. & Zwahlen, M. Body-mass index and incidence of cancer: a systematic review and meta-analysis of prospective observational studies. Lancet 371, 569–78 (2008).
Benn, M., Tybjaerg-Hansen, A., Smith, G. D. & Nordestgaard, B. G. High body mass index and cancer risk-a Mendelian randomisation study. Eur J Epidemiol 31, 879–92 (2016).
Gerstenblith, M. R. et al. Basal cell carcinoma and anthropometric factors in the U.S. radiologic technologists cohort study. Int J Cancer 131, E149–55 (2012).
Lahmann, P. H., Hughes, M. C., Williams, G. M. & Green, A. C. A prospective study of measured body size and height and risk of keratinocyte cancers and melanoma. Cancer Epidemiol 40, 119–25 (2016).
Milan, T., Verkasalo, P. K., Kaprio, J. & Koskenvuo, M. Lifestyle differences in twin pairs discordant for basal cell carcinoma of the skin. Br J Dermatol 149, 115–23 (2003).
Nagel, G. et al. Metabolic risk factors and skin cancer in the Metabolic Syndrome and Cancer Project (Me-Can). Br J Dermatol 167, 59–67 (2012).
Olsen, C. M., Hughes, M. C., Pandeya, N. & Green, A. C. Anthropometric measures in relation to basal cell carcinoma: a longitudinal study. BMC Cancer 6, 82 (2006).
Pothiawala, S., Qureshi, A. A., Li, Y. & Han, J. Obesity and the incidence of skin cancer in US Caucasians. Cancer Causes Control 23, 717–26 (2012).
Praestegaard, C. et al. Obesity and risks for malignant melanoma and non-melanoma skin cancer: results from a large Danish prospective cohort study. J Invest Dermatol 135, 901–4 (2015).
Tang, J. Y. et al. Lower skin cancer risk in women with higher body mass index: the women’s health initiative observational study. Cancer Epidemiol Biomarkers Prev 22, 2412–5 (2013).
Stroup, D. F. et al. Meta-analysis of observational studies in epidemiology: a proposal for reporting. Meta-analysis Of Observational Studies in Epidemiology (MOOSE) group. JAMA 283, 2008–12 (2000).
Greenland, S. & Longnecker, M. P. Methods for trend estimation from summarized dose-response data, with applications to meta-analysis. Am J Epidemiol 135, 1301–9 (1992).
Orsini, N., Bellocco, R. & Greenland, S. Generalized least squares for trend estimation of summarized dose-respose data. Stata J 6, 40–57 (2006).
DerSimonian, R. & Laird, N. Meta-analysis in clinical trials. Control Clin Trials 7, 177–88 (1986).
Orsini, N., Li, R., Wolk, A., Khudyakov, P. & Spiegelman, D. Meta-analysis for linear and nonlinear dose-response relations: examples, an evaluation of approximations, and software. American journal of epidemiology 175, 66–73 (2012).
Higgins, J. P. & Thompson, S. G. Quantifying heterogeneity in a meta-analysis. Stat Med 21, 1539–58 (2002).
Egger, M., Davey Smith, G., Schneider, M. & Minder, C. Bias in meta-analysis detected by a simple, graphical test. BMJ 315, 629–34 (1997).
Begg, C. B. & Mazumdar, M. Operating characteristics of a rank correlation test for publication bias. Biometrics 50, 1088–101 (1994).
Gray, L., Lee, I. M., Sesso, H. D. & Batty, G. D. Association of body mass index in early adulthood and middle age with future site-specific cancer mortality: the Harvard Alumni Health Study. Ann Oncol 23, 754–9 (2012).
van Dam, R. M. et al. Risk factors for basal cell carcinoma of the skin in men: results from the health professionals follow-up study. Am J Epidemiol 150, 459–68 (1999).
Ramos, J., Villa, J., Ruiz, A., Armstrong, R. & Matta, J. UV dose determines key characteristics of nonmelanoma skin cancer. Cancer Epidemiol Biomarkers Prev 13, 2006–11 (2004).
Magnus, K. The Nordic profile of skin cancer incidence. A comparative epidemiological study of the three main types of skin cancer. Int J Cancer 47, 12–9 (1991).
Wu, S. et al. Cumulative ultraviolet radiation flux in adulthood and risk of incident skin cancers in women. Br J Cancer 110, 1855–61 (2014).
Preston, D. S. & Stern, R. S. Nonmelanoma cancers of the skin. N Engl J Med 327, 1649–62 (1992).
Mancuso, M. et al. Modulation of basal and squamous cell carcinoma by endogenous estrogen in mouse models of skin cancer. Carcinogenesis 30, 340–7 (2009).
Chaudhary, S. C. et al. Erb-041, an estrogen receptor-beta agonist, inhibits skin photocarcinogenesis in SKH-1 hairless mice by downregulating the WNT signaling pathway. Cancer Prev Res (Phila) 7, 186–98 (2014).
Thornton, M. J. Estrogens and aging skin. Dermatoendocrinol 5, 264–70 (2013).
Emmerson, E. & Hardman, M. J. The role of estrogen deficiency in skin ageing and wound healing. Biogerontology 13, 3–20 (2012).
Tadokoro, S. et al. Leptin promotes wound healing in the skin. PLoS One 10, e0121242 (2015).
Poeggeler, B. et al. Leptin and the skin: a new frontier. Exp Dermatol 19, 12–8 (2010).
Gilbody, J. S., Aitken, J. & Green, A. What causes basal cell carcinoma to be the commonest cancer? Aust J Public Health 18, 218–21 (1994).
Pelucchi, C., Naldi, L., Di Landro, A. & La Vecchia, C. & Oncology Study Group of Italian Group for Epidemiologic Research in, D. Anthropometric measures, medical history and risk of basal cell carcinoma in an Italian case-control study. Dermatology 216, 271–6 (2008).
Machova, L. et al. Association between obesity and cancer incidence in the population of the District Sumperk, Czech Republic. Onkologie 30, 538–42 (2007).
Yang, Y. et al. Obesity and incidence of lung cancer: a meta-analysis. Int J Cancer 132, 1162–9 (2013).
Acknowledgements
This study was supported by National Natural Science Foundation of China (81471870).
Author information
Authors and Affiliations
Contributions
All authors contributed to study design; Z.D. and L.G. searched the databases, assessed eligibility, and collected data; Z.D. and W.J. analyzed data and prepared tables and figures; Z.D. wrote the manuscript; and all authors contributed to the interpretation of results and the revision of manuscript.
Ethics declarations
Competing interests
The authors declare no competing financial interests.
Electronic supplementary material
Rights and permissions
This work is licensed under a Creative Commons Attribution 4.0 International License. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in the credit line; if the material is not included under the Creative Commons license, users will need to obtain permission from the license holder to reproduce the material. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/
About this article
Cite this article
Zhou, D., Wu, J. & Luo, G. Body mass index and risk of non-melanoma skin cancer: cumulative evidence from prospective studies. Sci Rep 6, 37691 (2016). https://doi.org/10.1038/srep37691
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/srep37691
This article is cited by
-
Components of genetic associations across 2,138 phenotypes in the UK Biobank highlight adipocyte biology
Nature Communications (2019)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.