Abstract
This study aimed to determine the trends in prevalence of childhood overweight and malnutrition in a large Chinese ethnic minority population from 1991 to 2010. In the Chinese National Survey on Students’ Constitution and Health from 1991 to 2010, multistage stratified sampling was conducted in the series of cross-sectional studies. Participants were 7–18-year-old students randomly selected by sex and region, and included Han and 26 ethnic minorities. During the survey period, the overall prevalence of overweight increased from 5.8% to 13.5%, and malnutrition trend increased from 3.6% to 4.1% in ethnic minority children and adolescents. Moreover, Korean and Mongol children were more likely than Han children to be obese (Korean: RR = 1.52; 95% CI: 1.48–1.56; Mongol: RR = 1.24; 95% CI: 1.20–1.28). Among these minorities, the Dongxiang and Li children were more likely to be malnourished (Li: RR = 1.47; 95% CI: 1.37–1.57; Dongxiang: RR = 1.45; 95% CI: 1.34–1.58). Shui, Khalkhas, Lisu, and Monguor children were less likely to be overweight and malnourished compared with the Hans. The prevalence of overweight among ethnicities increased yearly while that for malnutrition has fluctuated over the past few decades.
Similar content being viewed by others
Introduction
Overweight and malnutrition are major health concerns in many low- and middle-income countries, including China1,2. Overweight children and adolescents are more likely to have metabolic abnormalities including increased blood cholesterol, triacylglyceride and glucose levels, insulin resistance, and hypertension3,4. Obesity in childhood may lead to a range of adult chronic diseases and conditions, such as cardiovascular diseases, diabetes, and premature death5. Furthermore, an unhealthy figure caused by overweight or dysplasia by malnutrition adversely influences children’s mental health6,7. Conversely, malnutrition among children and adolescents could affect their physical growth and physical work capacity8. Particularly, severe malnutrition in the teenage years could delay or cause problems with the development of secondary sex characters9. Malnutrition is also an underlying risk factor for morbidity and mortality of many diseases in both children and adults5. Childhood malnutrition has been reportedly associated with socioeconomic disadvantages, such as low adult income, poor economic growth, and intergenerational transmission of poverty10. Therefore, health-care expenditure to solve or alleviate overweight and malnutrition in children and adolescents is always a heavy financial burden nationally.
Many studies have reported the prevalence of overweight and obesity among children and adolescents in China, but those on malnutrition remain sparse. Concerns are increasing regarding epidemic trends in overweight and obesity, especially among the Hans. However, the prevalence rates of overweight and malnutrition among minorities remain unknown, with the exception of some studies on Tibetan, Mongolian and Uygur children11,12,13. The overall population of 55 ethnic minorities has exceeded 100,000,000 people, accounting for 8% of China’s entire population. Examining both overweight and malnutrition among ethnic minorities using nationally representative samples allows us to recognize growth and development problems experienced by children and adolescents in China.
Thus, this study aims to describe the prevalence rates of overweight and malnutrition among school-aged children and adolescents from different ethnic groups.
Methods
Data sources and sampling frame
The Chinese National Surveys on Students’ Constitution and Health (CNSSCH) is a series of complex multistage, cross-sectional, nationwide surveys on the physical fitness and health status of students in China. Becoming a continuous survey in 1985, the CNSSCH has released data every 5 years since, with currently six completed surveys.
In this study, Han participants were school students aged 7–18 years, randomly selected from 31 mainland provinces. The participants were classified by gender and region (urban or rural) within each province, and divided into four groups with equal sample sizes from three socioeconomic classes (upper, middle, and lower). The prevalence of overweight among Han children and adolescents has been reported elsewhere14.
Participants of ethnic minorities were primary and secondary school students aged 7–18 years, randomly selected from 13 provinces. Mongolian, Hui, Uyghur, Zhuang and Korean student participants were classified by gender and region (urban and rural). Other ethnic minorities were classified by gender only, not by region (Supplementary Figure 1), and were therefore categorized into other areas. We define rural areas as scattered settlements consisting of labourers engaged in agricultural production. Urban areas are defined as settlements that give priority to non-agricultural economy, including cities and towns. Other areas (other ethnic minorities) are ethnic enclaves where ethnic minorities live together and cannot be categorized into urban or rural areas. This report is based on survey data collected in 1991 (N = 55451), 1995 (N = 54276), 2000 (N = 58551), 2005 (N = 73122), and 2010 (N = 80082).
Our study was approved by the ethics committee of the Medical College of Soochow University in Suzhou, Jiangsu, China, and followed the tenets of the Declaration of Helsinki. Verbal informed consent was obtained from all students aged 7–18 years and from their parents after the nature of the study had been explained.
Clinical measurements
Data were obtained from normal students who were well-developed, physically and psychologically healthy, and able to participate in various sports activities. Students who had multiple organ dysfunction (such as heart, liver, spleen and kidney), physical disability and deformation, acute diseases (such as high fever and diarrhoea without recovery of physical strength), and females who were menstruating were excluded from participating in the fitness test of the survey. Height (cm) and weight (kg) were measured by the same trained technicians. Weight was measured to the nearest 0.1 kg using a balance-beam scale while the participants were wearing lightweight clothing. Height was measured to the nearest of 0.1 cm with a portable stadiometer while the participants were barefoot (Supplementary Tables 2, 3, 4 and 5). Weight categories among children and adolescents were based on standardized weight-for-height criteria from the sex-and-age-specific 80th percentile weight to the same height population. The standards were created from 1985 CNSSCH data. Overweight was defined as >110% of the standard weight-for-height, after adjusting for age and sex15. Malnutrition was defined as <80% of the standard weight-for-height.
Data analysis
We estimated distributions of overweight and malnutrition by gender and residence (urban, rural, or other area). P < 0.05 was considered statistically significant. To test for trends in the prevalence rates of overweight and malnutrition among children and adolescents during 1991–2010, we used generalized linear models (GLM) with a log function based on binomial distribution. The GLM was also used to generate rate ratios (RR, i.e., prevalence ratio and risk ratio) between the Han and ethnic minority groups, after adjusting for age, group, sex, and region. The overall prevalence rate of ethnic minority groups was normalized by means of weighting by the population of ethnicities from China’s 2010 census data. Age-adjusted prevalence of every ethnic minority was also directly adjusted according to China’s 2010 census population age structure. Data were analysed using SAS (Version 9.1; SAS Institute Inc., Cary, NC., USA) statistical software.
Results
Overall trend for overweight and malnutrition
From 1991 to 2010, the overall prevalence of overweight significantly increased among ethnic minority children and adolescents from 5.8% to 13.5% (RR, 1.24; 95% CI, 1.23–1.25) (Table 1). However, the overall malnutrition prevalence increased in 1995 but decreased in 2005 (Table 2). Although overweight and malnutrition affected fewer male participants than female, a higher prevalence of overweight was found in males than females since 2005.
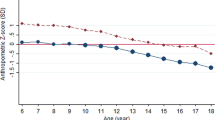
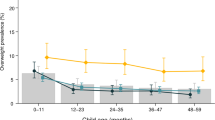
A lower rate of prevalence for overweight and malnutrition was found among children living in rural regions compared with those living in urban regions (overweight: RR, 0.84; 95% CI, 0.81–0.87; malnutrition: RR, 0.88; 95% CI, 0.87–0.90). Likewise, a lower rate of prevalence in other regions was found when compared with that in urban regions (overweight: RR, 0.64; 95% CI, 0.62–0.65; malnutrition: RR, 0.88; 95% CI, 0.86–0.91) (Table 3). The prevalence of overweight increased in all age groups from 1991 to 2010, among which the 10–12-year age group had the highest overweight prevalence (RR, 1.40; 95% CI, 1.36–1.44). However, in these same years, the prevalence of malnutrition remained stable and the highest prevalence of malnutrition occurred in the 13–15-year age group (RR, 3.30; 95% CI, 3.21–3.29) (Fig. 1 and Table 3).
Ethnic Characteristics
In 2010, the Koreans had the highest overall prevalence of overweight at 30.6% (95% CI, 29.4–31.9%), followed by the Mongolians at 22.3% (95% CI, 21.0–23.7%) (Table 4). Among ethnic minorities, the Lis had the lowest overweight prevalence (3.7%) and the highest prevalence of malnutrition (10.7%). The Shui, Khalkhas, Lisu, and Monguor children were found to have a low prevalence for overweight and malnutrition (Table 4 and Fig. 2). The Li (10.7%), Salar (10.0%), and Dai children (8.2%) ranked in the top three minority groups for overall malnutrition prevalence. Meanwhile, the Vas (0.7%) had the lowest overall prevalence of malnutrition. The prevalence of overweight and malnutrition in the Han children was 19.2% and 4.2%, respectively (Table 4).
From 1991 to 2010, the Koreans and Mongolians were more likely than the Hans to be obese (Korean: RR, 1.52; 95% CI, 1.48–1.56; Mongol: RR, 1.24; 95% CI, 1.20–1.28). The overall RR for the minority/Han children for overweight was 0.53 (95% CI, 0.52–0.54). Among these minorities, the Dai, Salar, Zhuang, Zang, Dongxiang, and Li were more likely to be malnourished than other minorities. The overall RR for minority/Han children for malnutrition was 0.81 (95% CI, 0.79–0.83) (Table 5).
Further analysis of the trend among the outliers in Fig. 2 showed the prevalence of overweight among the Koreans was obviously increasing and a rising trend was also shown among the Li, Salar, Qiang, and Va children from 1991 to 2010. In the same period, the prevalence of malnutrition was increasing among the Lis, while the prevalence of malnutrition fluctuated slightly among the Korean, Salar, Qiang, and Va children from 1991 to 2010 (Supplementary Tables 6 and 7).
Discussion
In this nationwide health survey of Chinese children, we observed that the prevalence of overweight in ethnic minorities had increased over the past few decades. Compared with the Hans and excluding Korean and Mongolian children, most ethnic minorities had a lower risk for the prevalence of overweight. The results also indicated that the children living in urban areas had a higher prevalence of overweight than their rural counterparts. Girls had a higher prevalence of malnutrition than boys. Moreover, most minorities had a lower risk for the prevalence of malnutrition among children and adolescents compared with the Hans from 1991 to 2010. Although the overweight prevalence among ethnic minorities was increasing yearly, the trend for malnutrition fluctuated.
Ethnic minorities had a lower prevalence of overweight overall compared with the Hans. A main reason for this may be due to genetic differences between the Hans and some ethnic minorities. For example, the Q27E genotype and allele frequency distribution differs among the Hans and Uyghurs. ADRB2 is associated with fat mobilization and stimulus generated by heat, and its genetic polymorphisms are significantly susceptible to obesity in the human body. Among these polymorphisms, Q27E is most common and is related to diseases such as obesity, primary hypertension, and type 2 diabetes16. Furthermore, ethnic groups differ in their dietary habits. Some minorities, such as the Uyghurs and Huis, do not eat pork, owing to their religious beliefs. The Lisu like to eat sour fish and meat made directly from raw materials. The Dais are fond of eating chopped raw beef with seasoning. The Zangs like to eat unseasoned dried beef. Additionally, some minorities, such as the Hanis and Bouyeis, reside in areas with poor transportation, limited communication with the outside world, and in living conditions that are dated and relatively poor. Furthermore, positive physical exercise, which is popular among minorities, could reduce the prevalence of overweight and obesity. For example, the Bamboo Dance is a traditional pastime for the Lis and requires agility to master. The risk of being overweight among the Lis was found to be the lowest.
However, due to the development of local tourism, frequent cultural exchanges, and economic exchanges between the Han and ethnic minorities, the recent prevalence of overweight among ethnic minorities was found to rise. The Mongol and Korean children had a higher overall prevalence of overweight than the Han children, which could be due to different factors. Mongolians living in the plateau region consume a large amount of red meat in order to adapt to the high altitude and frigid weather17. Additionally, with accelerated urbanization and economic development in China, socioeconomic status has improved among the Mongolians and Koreans.
Children and adolescents in most ethnic minorities were at a lower risk for malnutrition compared with the Han children from 1991 to 2010. China has adhered to the policy of national equality and unity for an extended period. Furthermore, the Chinese government greatly supports the development of ethnic minorities and has intensified reform and opening-up among minorities. For example, the government gives preferential policies and several subsidies to ethnic minorities. The government also engages in the construction of infrastructures among ethnic minorities, such as hospitals, and trade development, which helps decrease poverty. However, national finance cannot support the entire Han population that lies below the poverty line. Thus, more parents than in the past work far from their hometowns and consequently cannot care for their children. This is a possible reason why the Hans were found to have a relatively high rate of malnutrition compared with ethnic minorities from 1991 to 2010.
The differences among age groups, similar to that of other nations, are more likely caused by children’s growth and sexual maturity than environmental and behavioural factors. Furthermore, we used a statistical definition of obesity and malnutrition that was based on a comparison with the 1985 reference population represented in the CNSSCH growth charts. The charts were created for comparing within specific sex and age groups and not for comparing across sex and age groups. Age differences in prevalence reflect differences from the original reference population. Therefore, we did not focus on the variation from age, and examined the trend of overweight and malnutrition among ethnic minority children, after adjusting for age group as a confounder.
In 1995, the prevalence of malnutrition was high among minorities in the 13–15- and 16–18-year age groups. Mongolian, Shui, Tujia, Bai, Dai, and Yi children were not included in the 1995 survey. The prevalence of malnutrition among the Zang, Uyghur, and Zhuang children in 1995 was higher than that in previous years. Moreover, the Mongolians, Yis, Uyghurs, and Zhuangs had relatively heavier weight. These data may contribute to findings that the prevalence of malnutrition was high among minorities in certain age groups in 1995.
In general, minorities with greater overweight prevalences were less likely to be affected by malnutrition prevalence. Interestingly, results from the Shui, Khalkhas, Lisu, and Monguor children were inconsistent with this finding. The Khalkhas and Monguors are nomadic ethnicities, whereas the Shuis and Lisus livelihoods are based on agriculture, which requires physical strength. This may be the reason why these four ethnicities had a higher prevalence of malnutrition than other minorities.
In China, the overweight prevalence among ethnic minorities increased yearly and the trend of malnutrition fluctuated. However, in developed countries, a stable prevalence of childhood overweight and obesity over the past 15 years has been reported, while the prevalence of malnutrition has been found to be increasing, especially in girls18. In a large national survey of Australian school students, the prevalence of overweight and obesity did not increase in the adolescent population overall between 2006 and 201219. In Amsterdam, the prevalence of moderate thinness seems to be increasing20. Among 8–15-year-old Bulgarians, an increase in the incidence and prevalence of underweight was observed, with a high percentage of girls aged 14–15 years who were underweight21. India is facing similar challenges to China regarding the epidemic trends of overweight and malnutrition. The prevalence of obesity in India has remained somewhat constant over the last couple of decades. However, overweight and combined overweight/obesity prevalence showed an increasing trend22. In India, the prevalence of undernutrition remained high despite slowly declining over the past two decades23. One study found that one-fifth of Malaysian primary school children were overweight. This finding was comparable to that found in Singapore and Thailand, but was relatively higher than that of Indonesia and Vietnam24. However, based on the most recent and representative estimates available in Malaysia, the prevalence of underweight is higher than that of overweight25. Moreover, in the urban Pakistan, a four-fold increase in the number of overweight school-aged children in the past 5 years was found, highlighting the alarmingly rapid rise in childhood overweight and obesity26. The situation of overweight and malnutrition in neighbouring countries is also serious.
From a public health perspective, it is important to monitor and mitigate trends in overweight and malnutrition among children and adolescents. Non-communicable diseases (NCD) killed 38 million people globally in 2012, accounting for 68% of total annual death worldwide27. The increasing trend of obesity, both in adults and children, is directly responsible for the rapid increase in NCDs28. Moreover, malnutrition is a risk factor for NCDs related to ageing29. Thus, by reducing the prevalence of overweight and malnutrition, the burden of chronic disease can also be reduced, and the life expectancy of humans can be extended.
We acknowledge study limitations. First, this study analysed the Han and 26 other ethnic minority groups, but did not include another 29 ethnic minority groups. However, the remaining ethnic minorities account for <15% of the entire ethnic group population. Second, all Han participants in the 1991 survey were selected from a high socioeconomic population. Therefore, the prevalence of malnutrition is likely underestimated, and the trend of overweight likely overrated. Third, the definitions used for overweight and malnutrition in this article were not global criterions. Although different definitions of overweight and malnutrition in children and adolescents are used worldwide, they may be unsuitable for China’s children and adolescents. However, the standard weight-for-height references were created from the 1985 CNSSCH data (237,476 males and 233,639 females, aged 7–22 years), which had the largest sample size among the six existing surveys. The World Health Organization further recommends using these weight-for-height references. Since 1985, the standard weight-for-height references have been widely used for evaluating children’s nutritional status, and overweight and malnutrition in China.
We observed that the overweight prevalence among ethnic minorities was increasing yearly and that the trend of malnutrition fluctuated. We also examined the relationship between overweight and malnutrition among ethnic minorities. The results of this study could help the Chinese government to better understand the prevalence of overweight and malnutrition among ethnic minorities and take measures to improve the present situation.
Additional Information
How to cite this article: Guo, S. et al. Prevalence of overweight and malnutrition among ethnic minority children and adolescents in China, 1991–2010. Sci. Rep. 6, 37491; doi: 10.1038/srep37491 (2016).
Publisher's note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
Zhuo, Q. et al. Geographic variation in the prevalence of overweight and economic status in Chinese adults. Br. J. Nutr. 102, 413–418 (2009).
Black, R. E. et al. Maternal and child undernutrition and overweight in low-income and middle-income countries. Lancet 382, 427–451 (2013).
Biro, F. M. & Wien, M. Childhood obesity and adult morbidities. Am. J. Clin. Nutr. 91, 1499S–1505S (2010).
Nasreddine, L., Ouaijan, K., Mansour, M., Adra, N., Sinno, D. & Hwalla, N. Metabolic syndrome and insulin resistance in obese prepubertal children in Lebanon: a primary health concern. Ann. Nutr. Metab. 57, 135–142 (2010).
Ashaba, S., Rukundo, G. Z., Beinempaka, F., Ntaro, M. & LeBlanc, J. C. Maternal depression and malnutrition in children in southwest Uganda: a case control study. BMC Public Health 15, 1303 (2015).
Russell-Mayhew, S., McVey, G., Bardick, A. & Ireland, A. Mental health, wellness, and childhood overweight/obesity. J Obes 2012, 281801 (2012).
Franzek, E. J., Sprangers, N., Janssens, A. C., Van Duijn, C. M. & Van De Wetering, B. J. Prenatal exposure to the 1944–45 Dutch ‘hunger winter’ and addiction later in life. Addiction 103, 433–438 (2008).
Pelletier, D. L. & Frongillo, E. A. Changes in child survival are strongly associated with changes in malnutrition in developing countries. J. Nutr. 133, 107–119 (2003).
Mahgoub S. E. et al. Extent types of and the factors related to malnutrition among children under three years of age in Botswana. AJFAND 6, (2006). (Kenya).
Tette, E. M., Sifah, E. K. & Nartey, E. T. Factors affecting malnutrition in children and the uptake of interventions to prevent the condition. BMC Pediatr 15, 189 (2015).
Ma, J. et al. [Secular changes on the morphological development and nutrition status of Tibetan students from 1985 to 2005]. Zhonghua Liu Xing Bing Xue Za Zhi 30, 1030–1033 (2009).
Huang, Z. Y. et al. [Trends of overweight and obesity in aged 7 to 18 Mongolian ethnic children and adolescents from 1985–2010]. Zhonghua Liu Xing Bing Xue Za Zhi 33, 201–206 (2012).
Liu, C. et al. [Prevalence on overweight and obesity in Han, Uygur and Hazakh in adults from Xinjiang]. Zhonghua Liu Xing Bing Xue Za Zhi 31, 1139–1143 (2010).
Sun, H., Ma, Y., Han, D., Pan, C. W. & Xu, Y. Prevalence and trends in obesity among China’s children and adolescents, 1985–2010. PLoS ONE 9, e105469 (2014).
Working Group on Physical Health of Chinese school students (1987) Report on the physical fitness and health surveillance of Chinese school students. Beijing: People’s Education Press. (Chinese).
Jiao, Y. et al. Association between gene polymorphism of β2 adrenergic receptor and obesity in Uyghur minority. Medical Journal of Xian Jiaotong University 32, 691–693 (Chinese) (2011).
Nashundalai. Analysis of risk factors of primary hypertension among Mongol minority based on KLK-1 gene polymorphism. Jilin University (2013). (Chinese)
Sigmund, E., Sigmundová, D., Badura, P., Kalman, M., Hamrik, Z. & Pavelka, J. Temporal Trends in Overweight and Obesity, Physical Activity and Screen Time among Czech Adolescents from 2002 to 2014: A National Health Behaviour in School-Aged Children Study. Int J Environ Res Public Health 12, 11848–11868 (2015).
O’Dea, J. A. & Dibley, M. J. Prevalence of obesity, overweight and thinness in Australian children and adolescents by socioeconomic status and ethnic/cultural group in 2006 and 2012. Int J Public Health 59, 819–828 (2014).
Franssen, S. J., van der Wal, M. F., Jansen, P. & van Eijsden, M. [Thinness and overweight in children from Amsterdam: a trend analysis and forecast]. Ned Tijdschr Geneeskd 159, A8967 (2015).
Mladenova, S. et al. Prevalence of underweight, overweight, general and central obesity among 8–15-years old Bulgarian children and adolescents (Smolyan region, 2012–2014). Nutr Hosp 31, 2419–2427 (2015).
Ranjani, H. et al. Epidemiology of childhood overweight & obesity in India: A systematic review. Indian J. Med. Res. 143, 160–174 (2016).
Matsuzaki, M. et al. Adolescent undernutrition and early adulthood bone mass in an urbanizing rural community in India. Arch Osteoporos 10, 232 (2015).
Naidu, B. M. et al. Overweight among primary school-age children in Malaysia. Asia Pac J Clin Nutr 22, 408–415 (2013).
Khambalia, A. Z., Lim, S. S., Gill, T. & Bulgiba, A. M. Prevalence and sociodemographic factors of malnutrition among children in Malaysia. Food Nutr Bull 33, 31–42 (2012).
Mushtaq, M. U., Gull, S., Abdullah, H. M., Shahid, U., Shad, M. A. & Akram, J. Prevalence and socioeconomic correlates of overweight and obesity among Pakistani primary school children. BMC Public Health 11, 724 (2011).
Nam, E. W. et al. Obesity and Hypertension among School-going Adolescents in Peru. J Lifestyle Med 5, 60–67 (2015).
Misra, A. & Khurana, L. Obesity-related non-communicable diseases: South Asians vs White Caucasians. Int J Obes (Lond) 35, 167–187 (2011).
Bárbara, P. C. A. et al. Nutritional Risk is Associated with Chronic Musculoskeletal Pain in Community-dwelling Older Persons: The PAINEL Study. J Nutr Gerontol Geriatr 35, 43–51 (2016).
Acknowledgements
This study was funded by National Natural Science Foundation of China (81402761), the Foundation Research Project of Jiangsu Province (BK20140361), Priority Academic Program Development of Jiangsu Higher Education Institutions (PAPD), Jiangsu Key Laboratory of Preventive and Translational Medicine for Geriatric Diseases (KJS1513) and Science and Technology Program of Xiangcheng district, Suzhou (XJ201454).
Author information
Authors and Affiliations
Contributions
H.P.S. and C.W.P. designed the experiments; S.F.G. and Q.H.M. collected the samples; C.H.Z. analyzed the data; S.F.G. wrote the manuscript; All authors reviewed the manuscript.
Ethics declarations
Competing interests
The authors declare no competing financial interests.
Electronic supplementary material
Rights and permissions
This work is licensed under a Creative Commons Attribution 4.0 International License. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in the credit line; if the material is not included under the Creative Commons license, users will need to obtain permission from the license holder to reproduce the material. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/
About this article
Cite this article
Guo, S., Zhao, C., Ma, Q. et al. Prevalence of overweight and malnutrition among ethnic minority children and adolescents in China, 1991–2010. Sci Rep 6, 37491 (2016). https://doi.org/10.1038/srep37491
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/srep37491
This article is cited by
-
Associations of outdoor activity and screen time with adiposity: findings from rural Chinese adolescents with relatively low adiposity risks
BMC Public Health (2020)
-
Prevalence of excess body weight and underweight among 26 Chinese ethnic minority children and adolescents in 2014: a cross-sectional observational study
BMC Public Health (2018)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.