Abstract
Sleep is integral to life and sleep duration is important in sleep quality, physical, and psychological health. Disturbances in sleep duration have been associated with increased risk of metabolic disorders, hypertension, and overall mortality. Sleep disturbance has also been linked with various gastrointestinal disorders. However, the association between sleep and peptic ulcer disease (PUD) has not been evaluated. We investigated the association between sleep duration and PUD. Subjects were included from the fifth Korean National Health and Nutrition Examination Survey conducted from 2008–2009. Individuals with PUD were defined as those with a physician diagnosis of PUD. Daily sleep duration was established by asking participants the amount of time that they slept per day. Multiple logistic regression models were used to evaluate the association of PUD and sleep duration. This study included 14,290 participants (8,209 women). The prevalence of PUD was 5.7% and was higher in men (6.8%) than in women (4.9%). Women who slept ≥9 hours were significantly less likely to have PUD compared to women who slept 7 hours. In men, longer sleep duration (≥9 hours) had a tendency toward PUD prevention. Our results suggest that longer sleep duration may play a protective role for PUD development.
Similar content being viewed by others
Introduction
Sleep is an essential part of human life and sleep duration is an important factor in sleep quality, physical, and psychological health1,2,3,4,5. Previous studies have reported that short or long durations of sleep are associated with an increased risk of obesity, hypertension, type 2 diabetes, metabolic syndrome, and overall mortality1,3,4,6,7,8. Sleep disturbance has also been linked to gastrointestinal diseases9,10. During sleep, defensive mechanisms against peptic ulcer disease (PUD) including gastric mucosal blood flow, gastric bicarbonate efflux, and melatonin secretion have been reported to increase while gastric acid secretion is decreased9,11.
According to a recent systematic analysis for the Global Burden of Disease study, PUD is a common and serious medical problem12,13. The prevalence of PUD is approximately 4.1%, and about 10% of people develop PUD during their lifetime13,14. Though Helicobacter pylori and nonsteroidal anti-inflammatory drugs are the most important risk factors for PUD, no obvious cause is found in 5–20% of PUD patients15. Recent studies suggest that non-organic causes such as psychological stress may play a role in the onset and course of PUD15,16,17.
The association between sleep duration and PUD remains to be fully understood. In this study, we assessed the association between sleep duration and PUD among adults representative of the Korean population.
Results
Characteristics of participants
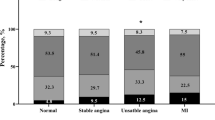
Of the 20,277 KNHANES IV participants, 15,071 were eligible for this study. 14,290 participants (6,081 men and 8,209 women) were included and 781 subjects were excluded due to missing data for variables. The prevalence of PUD in the entire population was 5.7%, and the prevalence of PUD was higher in men (6.8%) than in women (4.9%).
Table 1 shows the clinical characteristics of the study participants by sex. Participants with PUD were older and had a lower education level than participants without PUD for men and women. There were no differences in smoking, drinking and exercise habits between those with and without PUD. However, subjects with PUD indicated that they were under more stress, had suicidal ideation, and more depressive symptoms than those without PUD. The mean sleep duration of participants with PUD was significantly shorter than those without PUD, regardless of sex.
Characteristics of the study population according to sleep duration
The prevalence of PUD and the characteristics of the study population according to sleep duration are presented in Table 2. The reference group was established as men (28.3%) and women (28.4%) who slept 7 hours per day. Drinking and exercise were significantly associated with sleep duration among men. Current smoking and exercise were statistically significant across the sleep duration categories for women. Participants with sleep durations of <5 hours were more likely to be older, obese and under stress compared with any other sleep group. Subjects who had depressive symptoms, and suicidal ideation exhibited a U-shaped prevalence of PUD with sleep duration, regardless of sex.
Associations between sleep duration and PUD
The relationship between sleep duration and PUD after adjustment for multiple risk factors can be seen in Table 3. In age and BMI adjusted logistic regression analysis, women who slept ≥9 hours were less likely to have PUD (Odds Ratio (OR) = 0.59, 95% Confidence Interval (CI) = 0.363–0.950) compared to those who slept 7 hours (reference group). After further adjustment for smoking, drinking, exercise, education, income, and spouse, the negative association between PUD and long sleep duration (≥9 hours) persisted in women (OR = 0.60, 95% CI = 0.369–0.978). When stress and depressive symptoms were added to logistic regression models for full adjustment, women with long sleep duration (≥9 hours) had lower PUD than those with 7 hours sleep (OR = 0.59, 95% CI = 0.362–0.964). Long sleep duration (≥9 hours) had a preventive effect tendency for PUD through all models in men.
When suicidal ideation instead of the depressive symptoms was fitted into the fully adjusted model, the findings did not change substantially (data not shown).
Discussion
In this study, we demonstrated that longer sleep duration is a potential preventive factor for PUD in women. The association between sleep duration and PUD was not significant in men. These associations remained evident even after adjusting for established risk factors, such as old age, smoking, drinking and stress, thus reinforcing our conclusion that longer sleep duration was an independent protective factor for PUD in women. To our knowledge, this is the first population-based study to assess the association between sleep duration and PUD.
Several studies have indicated a relationship between sleep duration and cardiovascular diseases, obesity, hypertension, type 2 diabetes, metabolic syndrome, and overall mortality1,2,3,4,5,6,8. However, the association between sleep duration and PUD has not been evaluated. One study reported a positive association between sleep and peptic ulcer bleeding from a nationwide population base-study18. In this study, patients with sleep apnea had a 2.4-fold higher risk for incident peptic ulcer bleeding18. Hyperactivation of the sympathetic system and increased blood pressure may have caused peptic ulcer bleeding in a manner analogous to stress ulcer formation, which may also have contributed to the increased incidence of PUD in our study19,20.
PUD is clinically important because it is a common disorder with one in ten Americans developing PUD14. The disease adds a substantial burden to patients, health care professionals, and the health care system. The pathogenesis of PUD lies in the imbalance between the gastroduodenal mucosal defense system and gastric acid secretion21. Stress and anxiety were accepted as the main causes of PUD in the mid-20th century22. Considerations of etiology evolved with the discovery of the relationship between Helicobacter pylori and PUD23. However, recent studies suggest that psychological stress may play a role in the onset and the course of PUD15,16,17. Our findings suggest that sleep duration may be a novel risk factor for PUD.
The mechanism underlying the relationship between sleep duration and PUD is not clear, but there are some potential explanations. One is increased gastric mucosal blood flow and decreased gastric acid secretion during sleep. Increased gastric mucosal blood flow accelerates ulcer healing and decreased gastric mucosal blood flow has been reported to cause acute gastric mucosal lesions24. In addition, gastric acid secretion has been reported to decrease in deeper stages of sleep, especially during rapid eye movement while sleeping25. This may be associated with reduction in plasma noradrenaline, gastrin, and histamine levels and increasing gastric mucosal blood flow26.
Another mechanism explaining the relationship between sleep and PUD may be related to melatonin. Melatonin has been reported to be a potent stimulant of bicarbonate and may contribute to the healing of gastric lesions. This may be due to inhibition of gastric acid secretion, enhancement of gastric mucosal blood flow, and influence on prostaglandin-dependent pathways27,28. Melatonin has been demonstrated to have antistress neurohormonal properties and may exert gastrointestinal protection by other mechanisms, including scavenging oxygen radicals and increasing mucosal microcirculation and cell proliferation9,27,28.
Interestingly, we only found a significant association between sleep duration and PUD in women. Consistent with our findings, previous studies have shown sex-dependent associations between sleep duration and hypertension and metabolic syndrome3,29,30,31. Although we could not explain the sex-specific effects of sleep duration on PUD at the present time, it is possible that sex-related hormonal influences, sex differences in stress, and reaction to stress may play a role32. A recent analysis reported that women are more vulnerable to changes in sleep duration33. Another study reported that women were found to secrete melatonin earlier and have a significantly higher melatonin amplitude than men with a similar sleep duration33. This may account for women with longer sleep duration having a reduced risk of PUD, where men had a nonsignificant difference. Measuring melatonin levels may have helped support our study results. Further research between sleep duration, melatonin levels and gender may help explain this in the future.
There were some limitations to this study. First, PUD was defined as previous diagnosis by a physician. PUD requires endoscopic confirmation, which suggests that some of the subjects in our study may not have had PUD. However, the incidence of endoscopically confirmed PUD has been reported to be between 2–10% in Korea, which suggests that our study may not have overestimated PUD incidence34,35,36,37. Also, as the lifetime screening rate for stomach cancer during the study period was about 65%, we believe that many of our subjects had been diagnosed with PUD by endoscopy38. Furthermore, upper gastrointestinal endoscopy is readily available in Korea, costs less than $35 and is offered free of charge in the biennial government or yearly employee health examinations39,40. As such, we believe that the physician reported diagnosis is credible. Second, we relied on self-reported sleep duration instead of objective measures of sleep duration. However, we considered the self-reports sufficient, as previous studies have shown good agreement between self-reported sleep durations and those obtained through actigraphic monitoring41. Third, though age was included in the multivariable analysis, there was a significant age difference between the PUD and non-PUD groups. Older age is associated with aging of the mucosa and increased comorbidities, which may have influenced the outcome42. Fourth, PUD risk factors such as H. pylori status and drug history including non-steroidal anti-inflammatory drugs or antidepressants were not investigated in KNHANES. Despite these limitations, our study has merit, as KNHANES is representative of the entire Korean population and is large enough to provide adequate power.
Conclusions
Our results suggest that longer sleep duration (≥9 hours a day) could play a protective role in the development of PUD. Further prospective longitudinal studies are needed to identify the biological mechanisms underlying sleep duration and PUD risk with better control of confounders in different ethnic or age groups. If sleep duration plays a causative role in PUD, increased sleep could help in the prevention of PUD and improve public health.
Materials and Methods
Data source and subjects
This study was based on data acquired from the fifth Korean National Health and Nutrition Examination Survey (KNHANES IV) conducted from 2008–2009. The KNHANES is a nationwide, cross-sectional survey used to estimate the general health and nutrition status of the Korean population, conducted by the Korea Centers for Disease Control and Prevention (KCDCP). It consisted of a health interview, physical examination, and nutrition survey. Additional details regarding the design and methods of the survey have been described elsewhere43. KNHANES IV used a stratified multistage cluster probability sampling by a rolling sampling method, which was certified as producing representative statistics by the Korean Department of Statistics.
Participants older than 19 years of age were included in this study. Subjects with data missing for variables included in the analysis were excluded. The survey protocol was conducted according to the Declaration of Helsinki and approval for this study was granted by the Institutional Review Board of the Catholic University Medical Center (IRB No. KC15EISI0840). All survey participants signed informed consent forms.
Measurements
Anthropometric measures of the participants were performed by trained personnel. Waist circumference (WC) was measured at the midpoint between the lowest rib and the iliac crest. Blood pressure (BP) was measured in a seated position using a mercury sphygmomanometer (Baumanometer; Baum, Copiague, NY, USA). Three measurements were made with at least five minutes intervals and the mean value of the second and third measurements were used.
Cigarette smoking was classified as current smokers for participants who had smoked ≥100 cigarettes and currently smoked. For alcohol consumption, a heavy drinker was defined as an individual who consumed ≥30 g alcohol/day. The definition of regular exercise was moderate physical activity ≥30 minutes per day for >5 days per week and/or strenuous physical activity for ≥20 minutes per day for >3 days per week. Education level was categorized into less than high school, high school, and college or higher. Marital status was classified as “spouse, yes” for participants who were married and lived with their spouse and “spouse, no” for those who were unmarried, widowed, divorced, or separated. Household income was measured as quartiles based on per capita household income. Stress level was reported as none, mild, moderate and severe during the routine daily life. When a participant checked ‘moderate’ or ‘severe’, this participant was classified as being in the stressful state. Depressive symptoms were determined based on the question, “Have you felt sadness or despair which affected your daily life for more than 2 weeks over the past year?” Suicidal ideation was defined as thoughts of committing suicide during the past year.
Blood samples were collected in the morning after at least eight hours of fasting. Samples were properly processed, refrigerated immediately, and analyzed within 24 hours at the Central Testing Institute in Seoul, Korea. Fasting plasma glucose, total cholesterol, high-density lipoprotein cholesterol, and triglyceride were measured using the Hitachi Automatic Analyzer 7600 (Hitachi, Tokyo, Japan).
Definitions
Individuals with PUD were defined as those with a diagnosis of PUD by a physician. Daily sleep duration was established by asking the open-ended question: “How much time do you usually sleep per day?” Diabetes was classified as fasting plasma glucose ≥126 mg/dL, current antidiabetic medication, or a previous diagnosis of type 2 diabetes by a physician. Individuals with hypertension were defined as those with a systolic BP ≥ 140 mmHg, a diastolic BP ≥ 90 mmHg, or self-reported current use of antihypertensive medications.
Statistical analysis
We used the KNHANES sampling weight variables with stratification, designated by the KCDCP, which were based on the sample design of each survey year. Data are presented as the mean ± standard error (SE) for continuous variables or as proportions (SE) for categorical variables. The means of continuous variables were compared by independent t-tests, and the proportion of categorical variables were tested by Pearson’s chi-square tests.
Prevalence of PUD was measured for each sex, and further determined in each sleep duration group by sex. Multiple logistic regression models were used to evaluate the association of PUD with sleep duration. Three models were constructed: in model 1, adjustments were made for age and body mass index; model 2 included additional adjustments for smoking, drinking, exercise, education, income, and spouse; and in model 3, adjustments for stress and depressive symptoms were added. These anayses were repeated after replacing depressive symptoms with suicidal ideation. Results are presented as odds ratios and 95% confidence intervals. Differences were considered to be significant if the p-value was less than 0.05. Statistical analyses were performed using SAS for Windows (version 9.20, SAS Institute, Cary, NC, USA).
Additional Information
How to cite this article: Ko, S.-H. et al. Women Who Sleep More Have Reduced Risk of Peptic Ulcer Disease; Korean National Health and Nutrition Examination Survey (2008–2009). Sci. Rep. 6, 36925; doi: 10.1038/srep36925 (2016).
Publisher’s note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
Parish, J. M. Sleep-related problems in common medical conditions. Chest 135, 563–572 (2009).
Short, M. A. & Louca, M. Sleep deprivation leads to mood deficits in healthy adolescents. Sleep Med (2015).
Stefani, K. M., Kim, H. C., Kim, J., Oh, K. & Suh, I. The influence of sex and age on the relationship between sleep duration and metabolic syndrome in Korean adults. Diabetes research and clinical practice 102, 250–259 (2013).
Cai, H. et al. Sleep duration and mortality: a prospective study of 113 138 middle-aged and elderly Chinese men and women. Sleep 38, 529–536 (2015).
Ferrie, J. E. et al. A prospective study of change in sleep duration: associations with mortality in the Whitehall II cohort. Sleep 30, 1659–1666 (2007).
Tu, X. et al. Sleep duration and its correlates in middle-aged and elderly Chinese women: the Shanghai Women’s Health Study. Sleep Med 13, 1138–1145 (2012).
Fang, J. et al. Association of sleep duration and hypertension among US adults varies by age and sex. Am J Hypertens 25, 335–341 (2012).
Park, S. E. et al. The association between sleep duration and general and abdominal obesity in Koreans: data from the Korean National Health and Nutrition Examination Survey, 2001 and 2005. Obesity (Silver Spring, Md.) 17, 767–771 (2009).
Brzozowska, I. et al. Mucosal strengthening activity of central and peripheral melatonin in the mechanism of gastric defense. Journal of physiology and pharmacology: an official journal of the Polish Physiological Society 60 Suppl 7, 47–56 (2009).
Konturek, P. C., Brzozowski, T. & Konturek, S. J. Gut clock: implication of circadian rhythms in the gastrointestinal tract. Journal of physiology and pharmacology: an official journal of the Polish Physiological Society 62, 139–150 (2011).
Konturek, S. J., Konturek, P. C., Brzozowski, T. & Bubenik, G. A. Role of melatonin in upper gastrointestinal tract. Journal of physiology and pharmacology: an official journal of the Polish Physiological Society 58 Suppl 6, 23–52 (2007).
GBD 2013 Mortality and Causes of Death Collaborators. Global, regional, and national age-sex specific all-cause and cause-specific mortality for 240 causes of death, 1990-2013: a systematic analysis for the Global Burden of Disease Study 2013. Lancet (London, England) 385, 117–171 (2015).
Snowden, F. M. Emerging and reemerging diseases: a historical perspective. Immunological reviews 225, 9–26 (2008).
Aro, P. et al. Peptic ulcer disease in a general adult population: the Kalixanda study: a random population-based study. American journal of epidemiology 163, 1025–1034 (2006).
Jones, M. P. The role of psychosocial factors in peptic ulcer disease: beyond Helicobacter pylori and NSAIDs. Journal of psychosomatic research 60, 407–412 (2006).
Levenstein, S., Rosenstock, S., Jacobsen, R. K. & Jorgensen, T. Psychological stress increases risk for peptic ulcer, regardless of Helicobacter pylori infection or use of nonsteroidal anti-inflammatory drugs. Clinical gastroenterology and hepatology: the official clinical practice journal of the American Gastroenterological Association 13, 498–506.e491 (2015).
Goodwin, R. D. et al. A link between physician-diagnosed ulcer and anxiety disorders among adults. Annals of epidemiology 23, 189–192 (2013).
Shiao, T. H. et al. Sleep apnea and risk of peptic ulcer bleeding: a nationwide population-based study. The American journal of medicine 126, 249–255, 255.e241 (2013).
Eguchi, K. et al. Short sleep duration as an independent predictor of cardiovascular events in Japanese patients with hypertension. Arch Intern Med 168, 2225–2231 (2008).
Kato, M. et al. Effects of sleep deprivation on neural circulatory control. Hypertension 35, 1173–1175 (2000).
Kemmerly, T. & Kaunitz, J. D. Gastroduodenal mucosal defense. Current opinion in gastroenterology 30, 583–588 (2014).
Alp, M. H., Court, J. H. & Grant, A. K. Personality pattern and emotional stress in the genesis of gastric ulcer. Gut 11, 773–777 (1970).
Marshall, B. J. & Warren, J. R. Unidentified curved bacilli in the stomach of patients with gastritis and peptic ulceration. Lancet (London, England) 1, 1311–1315 (1984).
Kawano, S. & Tsuji, S. Role of mucosal blood flow: a conceptional review in gastric mucosal injury and protection. Journal of gastroenterology and hepatology 15 Suppl, D1–D6 (2000).
Stacher, G., Presslich, B. & Starker, H. Gastric acid secretion and sleep stages during natural night sleep. Gastroenterology 68, 1449–1455 (1975).
Guo, J. S., Chau, J. F., Cho, C. H. & Koo, M. W. Partial sleep deprivation compromises gastric mucosal integrity in rats. Life Sci 77, 220–229 (2005).
Kato, K. et al. Circadian rhythm of melatonin and prostaglandin in modulation of stress-induced gastric mucosal lesions in rats. Alimentary pharmacology & therapeutics 16 Suppl 2, 29–34 (2002).
Sjoblom, M. & Flemstrom, G. Melatonin in the duodenal lumen is a potent stimulant of mucosal bicarbonate secretion. Journal of pineal research 34, 288–293 (2003).
Stranges, S. et al. A population-based study of reduced sleep duration and hypertension: the strongest association may be in premenopausal women. Journal of hypertension 28, 896–902 (2010).
Cappuccio, F. P. et al. Gender-specific associations of short sleep duration with prevalent and incident hypertension: the Whitehall II Study. Hypertension 50, 693–700 (2007).
Choi, J. K. et al. Association between short sleep duration and high incidence of metabolic syndrome in midlife women. The Tohoku journal of experimental medicine 225, 187–193 (2011).
Kajantie, E. & Phillips, D. I. The effects of sex and hormonal status on the physiological response to acute psychosocial stress. Psychoneuroendocrinology 31, 151–178 (2006).
Guidozzi, F. Gender differences in sleep in older men and women. Climacteric: the journal of the International Menopause Society 18, 715–721 (2015).
Kim, H. M. et al. NSAID is inversely associated with asymptomatic gastric ulcer: local health examination data from the Korean National Health Insurance Corporation. Scandinavian journal of gastroenterology 48, 1371–1376 (2013).
Kim, H. S. et al. Prevalence of and risk factors for gastrointestinal diseases in korean americans and native koreans undergoing screening endoscopy. Gut and liver 7, 539–545 (2013).
Kim, J. S. & Kim, B.-W. Epidemiology of Peptic Ulcer Disease in Korea. The Korean Journal of Helicobacter and Upper Gastrointestinal Research 14, 1–5 (2014).
Chung, I.-S. & Kim, B.-W. Peptic Ulcer Diseases in Korea. The Korean Journal of Helicobacter and Upper Gastrointestinal Research 12, 19–22 (2012).
Suh, M. et al. Trends in Cancer Screening Rates among Korean Men and Women: Results of the Korean National Cancer Screening Survey, 2004-2013. Cancer Res Treat 48, 1–10 (2016).
Lee, H. Y., Park, E. C., Jun, J. K., Choi, K. S. & Hahm, M. I. Comparing upper gastrointestinal X-ray and endoscopy for gastric cancer diagnosis in Korea. World journal of gastroenterology: WJG 16, 245–250 (2010).
Choi, K. S. et al. Screening for gastric cancer in Korea: population-based preferences for endoscopy versus upper gastrointestinal series. Cancer Epidemiol Biomarkers Prev 18, 1390–1398 (2009).
Lockley, S. W., Skene, D. J. & Arendt, J. Comparison between subjective and actigraphic measurement of sleep and sleep rhythms. J Sleep Res 8, 175–183 (1999).
Garrow, D. & Delegge, M. H. Risk factors for gastrointestinal ulcer disease in the US population. Digestive diseases and sciences 55, 66–72 (2010).
Yoon, J. Y. et al. Prevalence of dietary supplement use in Korean children and adolescents: insights from Korea National Health and Nutrition Examination Survey 2007–2009. Journal of Korean medical science 27, 512–517 (2012).
Author information
Authors and Affiliations
Contributions
S.-H. Ko, K.-D. Han and M.K. Baeg designed the study. S.-H.-Ko, S.Y. Ko and K.-D. Han performed the analysis. S.-H. Ko and M.K. Baeg wrote the manuscript. S.Y. Ko and M.K. Baeg edited the manuscript.
Ethics declarations
Competing interests
The authors declare no competing financial interests.
Rights and permissions
This work is licensed under a Creative Commons Attribution 4.0 International License. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in the credit line; if the material is not included under the Creative Commons license, users will need to obtain permission from the license holder to reproduce the material. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/
About this article
Cite this article
Ko, SH., Baeg, M., Ko, S. et al. Women Who Sleep More Have Reduced Risk of Peptic Ulcer Disease; Korean National Health and Nutrition Examination Survey (2008–2009). Sci Rep 6, 36925 (2016). https://doi.org/10.1038/srep36925
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/srep36925
This article is cited by
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.