Abstract
Giant cell tumors of the bone (GCTBs) are commonly diagnosed in Asian populations, usually around the knee. Herein, we aimed to determine the clinical characteristics, local recurrence rates, and relevant risk factors of primary GCTB around the knee. Univariate and multivariate survival analyses were used to identify the risk factors for local recurrence. Four hundred ten patients with primary GCTB around the knee, treated between March 2000 and June 2014, were recruited from 7 institutions in China. The overall local recurrence rate was 23.4%, but was higher in patients aged 20–39 years (28.5%; P = 0.039). The local recurrence rate was the highest in patients treated with intralesional curettage (53.4%), and the lowest in those treated with resection (4.9%). We found a higher risk of tumor recurrence in the proximal fibula compared to the distal femur (hazard ratio: 28.52, 95% confidence interval: 5.88–138.39; P < 0.0001), and in patients treated with curettage compared to those treated with resection (hazard ratio: 12.07, 95% confidence interval: 4.99–29.18; P < 0.0001). Thus, the tumor location must be considered when selecting the optimal surgical treatment approach to reduce the risk of local recurrence and preserve joint function, especially in young patients.
Similar content being viewed by others
Introduction
A giant cell tumor of the bone (GCTB) is a primary intramedullary bone tumor composed of mononuclear and giant multinucleated cells that resemble osteoclasts1. GCTB is one of the most widely investigated yet perplexing bone tumors. It accounts for 3–8% of primary bone tumors in Western countries; however, it is more common in Asia, where it accounts for approximately 20% of primary bone tumors2,3,4,5,6,7. GCTB is most commonly diagnosed in individuals aged 20–40 years, and >50% of cases occur around the knee2,3,8,9,10,11.
The postoperative recurrence rates of GCTB have been reported to be 10–65%4,5,12,13,14,15,16. A previous study from China reported a 12.4% local recurrence rate in patients with primary GCTB located in an extremity6. However, this rate was based on data obtained from patients at a single institution over a long time period. On the other hand, large-sample multicentre studies for this type of disease are still lacking, especially for GCTBs occurring at single locations.
Therefore, we conducted a multicentre, nationwide study in China to determine the clinical characteristics, local recurrence rates, and relevant risk factors for primary GCTBs occurring around the knee, and to clarify the appropriate surgical approach for reducing the local recurrence rate and protecting limb function.
Results
Demographic and Clinical Characteristics
Table 1 presents the demographic and clinical features of patients with primary GCTB around the knee. Of the included 410 patients, 217 (53%) were men and 193 (47%) were women (male:female ratio, 1.12:1). The mean (standard deviation) age at diagnosis was 35.7 (13.4) years; the majority of patients (57%) were aged between 20 and 39 years. Moreover, GCTB around the knee was more likely to occur in the right-side (53%), and locate distal femur (52%); 48% of the total tumors were categorized as Campanacci grade III tumors. The prevalence of pathological fractures was 34%. In terms of surgery, 24%, 46%, and 30% of patients were treated with intralesional curettage, curettage combined with resection, and en bloc marginal resection, respectively. In terms of the use of adjuvant treatments, polymethylmethacrylate (PMMA), phenol, electrotome, hydrogen peroxide, zinc chloride, and alcohol were used in 24.9%, 17%, 30%, 21%, 15%, and 13% of cases, respectively.
Local Recurrence Rate According to Clinical Characteristics
As shown in Table 2, the overall local recurrence rate was 23% (26% in men and 21% in women; P = 0.294). Furthermore, the side and location of the tumor, Campanacci grade, presence of pathological fractures, and use of polymethylmethacrylate (PMMA) did not influence the local recurrence rate. However, the rate was significantly higher in patients aged 20–39 years (29%; P = 0.039) and in patients treated with intralesional curettage (53%; P < 0.0001).
Risk Factors for Local Recurrence
Univariate analysis revealed that local recurrence was significantly associated with tumor location (log rank = 34.599; P < 0.0001) and surgical treatment (log rank = 43.076; P < 0.0001). Tumors located in the proximal fibula had a significantly higher local recurrence rate than those located in the distal femur (hazard ratio [HR]: 21.54, 95% confidence interval [CI]: 4.89–94.78). Moreover, the rate of local recurrence was significantly higher in patients who underwent intralesional curettage (HR: 11.25, 95% CI: 4.69–26.97) or curettage combined with resection (HR: 5.85, 95% CI: 2.45–13.96) compared to those who underwent en bloc marginal resection (all P < 0.0001; Table 3, Figs 1 and 2).
Kaplan-Meier curve of the cumulative rate without local recurrence by surgical approach.
Reference as en-bloc resection and marginal resection, there was a HR (95% CI) of 11.25 (4.69, 26.97) in intracystic curettage, and 5.85 (2.45, 13.96) in resection partly with intracystic curettage, all P < 0.0001.
Multivariate analysis indicated that tumor location and surgical treatment were independent risk factors for local recurrence. Tumors located in the proximal fibula had a significantly higher rate of local recurrence compared to those in the distal femur (HR: 28.52, 95% CI: 5.88–138.39). Additionally, treatment with intralesional curettage (HR: 12.07, 95% CI: 4.99–29.18) and curettage combined with resection (HR: 6.39, 95% CI: 2.66–15.36) were associated with significantly higher recurrence rates compared to en bloc marginal resection (all P < 0.0001; Table 3).
Functional Outcomes
The Musculoskeletal Tumor Society (MSTS) scores were significantly lower in patients with local recurrence than in those without, with median (range) scores of 25.5 (0–30) and 28.0 (1–30), respectively (P = 0.032). The median (range) MSTS scores were 28.0 (13–30), 28.0 (17–30), and 26.0 (0–30) in patients treated with intralesional curettage, curettage combined with resection, and en bloc marginal resection, respectively (P = 0.400).
Giant Cell Tumor Metastases
Among patients who received at least 12 months of follow-up, 4 developed metastasis (2 cases of pulmonary metastasis, 1 of thoracic vertebra metastasis, and 1 of multifocal bone metastasis). Of these, 3 patients died due to metastatic cancer, including 1 female patient with bilateral pulmonary metastasis, 1 male patient with thoracic vertebra metastasis, and 1 male patient with multifocal bone metastasis. The remaining male patient with unilateral pulmonary metastasis is alive after receiving lesion resection. The pulmonary and overall metastasis rates of GCTB around the knee were 0.7% and 1.3%, respectively.
Discussion
To the best of our knowledge, this is the first multicentre study to assess the clinical and epidemiological features, local recurrence rates, and factors associated with local recurrence among patients with primary GCTB around the knee by using a representative multicentre GCTB registry in China.
In Western countries, GCTB has been reported to be more likely to occur in women than in men. One previous study reported incidence rates in men and women of 48.5% and 51.5%, respectively17, while another reported rates of 44% and 56%, respectively18. However, several other studies have reported that GCTB occurs predominately in men, with male:female ratios ranging from 1.27:1 to 1.77:16,9,19,20,21. Consistent with the latter studies, we found that GCTB around the knee predominantly occurred in men, with a male:female ratio of 1.12:1. Of note, the male:female ratio in the general population of China was 1.05:1 in 201422, indicating that the higher ratio of male patients with GCTB around the knee is likely not simply reflecting the demographical distribution of the general population. Instead, we postulate that the difference in prevalence according to sex between Asian and Western individuals may be attributed to ethnicity.
GCTB is a highly controversial bone tumor in terms of its pathogenesis, and the reported local recurrence rates range widely, from 12% to 49%23,24,25,26,27. Previous studies have noted that undergoing surgery was associated with local GCTB recurrence5,25,28,29. In particular, curettage has been shown to be strongly associated with an increased risk of local recurrence. In one study, the local recurrence rate in patients with GCTB of the extremities was 2.4-fold higher in those who were treated with curettage (27%) than in those who underwent resection (12%)28. In another study, these rates were 25% and 5%, respectively4. However, in a series of primary GCTB cases in Canada, the local recurrence rates were 17% overall, 18% in the curettage group, and 16% in the resection group; thus, curettage was not a risk factor for local recurrence in that study30. In our study, the local recurrence rates in patients with primary GCTB around the knee were 23% overall, 53% for intralesional curettage, 28% for curettage combined with resection, and 5% for en bloc marginal resection. Compared to en bloc marginal resection, the risk of local recurrence increased by 11.1-fold for intralesional curettage and by 5.4-fold for curettage combined with resection.
Some authors have reported that the recurrence rate varies depending on the tumor location14,15,21. For example, the reported recurrence rate in the distal part of the radius ranges from 20% to 88.9%18,31,32. However, the local recurrence rates around the knee according to location have not been previously reported. In the present study, we found a 27.5-fold increased risk of local recurrence in patients with tumors located in the proximal fibula compared to in the distal femur. The higher rate of local recurrence in the proximal fibula may be explained by its unique anatomical position, as it is surrounded by the peroneal artery and anterior tibial artery and vein; therefore, tumors in the proximal fibula are commonly treated by curettage. On the other hand, it is not possible to remove tumors in the proximal fibula using a high-speed burr, owing to limited bone and thin bone shell. Moreover, as the fibula is not a weight-bearing bone, there is little impact on its functionality after resection, and we therefore recommend that giant cell tumors located in the proximal fibula should be resected.
Previous studies have reported a larger prevalence of Campanacci grade II tumors33,34,35. In contrast, we found higher proportions of both grade II and grade III GCTBs, accounting for 39% and 48% of the cases in the present study, respectively. These data are consistent with those from a previous report from China6.
The associations of local recurrence with Campanacci grade and pathological fractures remain uncertain. Several studies have reported that grade III disease is associated with a high recurrence rate5,21,36,37,38. However, a series from China found a significantly lower recurrence rate for giant cell Campanacci grade III tumors6. Similarly, we found that Campanacci grade III tumors exhibited the lowest rate of recurrence (22%), although the difference was not statistically significant. Furthermore, pathological fracture was not associated with local recurrence in this study. This may be explained by the greater proportion of patients with Campanacci grade III tumors (47.5%) who underwent resection compared to those with grade I (9.6%) and grade II tumors (15.0%).In addition, patients with pathological fracture were treated in two stages in this study; first, the fracture was treated through external fixation, and then, the tumor resection was completed. Patients with primary GCTB around the knee did not receive hip replacements in the present study. Thus, a lower local recurrence rate was not associated with tumor severity (grade III) or presence of pathological fracture.
Finally, the prevalence of pathological fractures was 34% in the present study. The pulmonary metastasis rate of GCTB around the knee was 0.7%, while the overall metastasis rate was 1.3%, and these rates were lower than those reported previously5,6.
PMMA is the most common adjuvant used to fill the tumor cavity, and hypothetically, lowers the risk of local recurrence through its hyperthermic properties39. However, in this study, we did not observe a lower local recurrence rate in patients who received PMMA compared to those who did not.
There are some limitations of the present study. First, this was a retrospective multicentre study, and the identification standards for radiological data and clinical staging may have differed among the included institutions. However, this limitation was addressed by using a predefined standardized treatment procedure devised by the Giant Cell Tumor Group of China (GTOC), a committee of experts, and by conducting extensive investigator training at the 7 participating centres. Second, the number of patients was small owing to the low prevalence of GCTB, and all patients were recruited from the 7 centres in China that participated in the study; hence, the included patients might not be representative of all GCTB patients in China.
Conclusion
To our knowledge, this is the first study based on a large, multicentre GCTB registry system to describe the clinical and epidemiological characteristics and outcomes in GCTB patients in China, and to evaluate the local recurrence rate, including the relevant risk factors, in primary GCTB around the knee. We found that GCTB around the knee occurred more often in men and in young individuals. Simultaneously, we found a higher local recurrence rate in patients aged 20–39 years and in those treated with intralesional curettage. Moreover, the tumor location and type of surgical intervention were independent risk factors for local recurrence; undergoing intralesional curettage and having tumors located in the proximal fibula increased the risk of local recurrence in patients with primary GCTB around the knee. The anatomical position of the proximal fibula may contribute to this increased risk of local recurrence, as it is surrounded by the peroneal artery and anterior tibial artery and vein. Thus, it is crucial to select the appropriate surgical treatment approach by considering the tumor location in order to reduce the risk of local recurrence and preserve knee function, especially for young patients with high-risk tumor locations.
Methods
Patient Selection
We recruited patients with primary GCTB around the knee, including the distal femur, proximal tibia, proximal fibular, and patella, from the GTOC between March 2000 and February 2015. The GTOC is an association of physicians from orthopaedic oncology centres located in different regions of China, who treat giant cell tumors. Seven centres established the GTOC in 2005, with 5 more joining in 2016; the data from these centres were thus not included in the present study. The aim of this group is to standardize the diagnosis and treatment of giant cell tumors in China. The current standardized procedure was devised by GTOC experts by taking into account the presence of pathological fracture, shifting of the articular surface, the Campanacci grade, the growth level of the tumor (whether the tumor has grown with or without breaking through the articular surface), and tumor volume.
We reviewed the patients’ medical records retrospectively. All the patients with a confirmed diagnosis of GCTB were included in this study. As a result, we extracted 510 patients with a confirmed histological diagnosis of benign GCTB. Of these, 410 (80.4%) patients with primary GCTB around the knee were recruited for this study, while 100 (19.6%) with recurrent tumors and who were treated elsewhere were excluded. Moreover, we excluded patients who were suspected of having GCTB preoperatively but whose diagnoses were not confirmed postoperatively, and cases of recurrent GCTB that were treated non-surgically were also not analysed in this study.
In the present study, we excluded pregnant women with GCTB owing to poor outcomes. There were 8 pregnant patients diagnosed with GCTB. Of these, 5 patients had tumors in the distal femur, and 3 had tumors in the proximal femur. Generally, the recurrence of GCTB occurred within 2 years after resection. However, in this study, local recurrence occurred after 8 years in 1 pregnant patient; the cause was unclear.
The clinical and imaging data of primary GCTBs around the knee were reviewed retrospectively.
The following information was recorded for all patients: tumor side (left or right), tumor location (distal femur, proximal tibia, proximal fibula, and patella), Campanacci stage (grade I, II, or III), pathological fracture (yes or no), surgical treatment method (intralesional curettage, curettage combined with resection, or en bloc marginal resection), and application of PMMA cement.
All investigative protocols were approved by the ethics committee of Tianjin Hospital. The procedures were performed according to approved guidelines, and written informed consent was obtained from each patient.
Surgical Treatment
The surgical techniques were based on the severity of the tumor and included intralesional curettage, curettage combined with resection, and en bloc marginal resection20. One or more adjuvants, including PMMA, phenol, electrotome, hydrogen peroxide, zinc chloride, and alcohol, were used during the surgical procedures.
Intralesional curettage was indicated for patients with a localized lesion,that is, lesions without a comminuted pathological fracture in the backbone, without an intra-articular fracture following obvious shifting of the articular surface, without a tumor breaking through the articular surface, classified as Campanacci grade I/II, and with the appropriate tumor volume. With this procedure, a window in the cortical bone is created and the mass is resected by using a series of curettes of various sizes. The residual tumor cavity is then polished with a high-speed burr until reaching the normal cortical bone. Subsequently, allogeneic particle bone is grafted to fill the residual tumor cavity, and the excised section that created the original cortical bone window is finally reattached (Fig. 3).
The diagrammatic drawing of intracystic curettage: (a) Indications: with a localized lesion, no broken or mild broken the cortical bone, without obvious soft tissue mass. (b) A window in the cortical bone was made. (c) To remove mass using a series of curettes of various sizes. (d) To polish the residual tumor cavity with a high-speed burring until reaching the normal cortical bone. (e) To fill the residual tumor cavity with allogenic particle bone graft and covered the windowed cortical bone.
Moreover, PMMA cement and a steel plate were used to fill tumor cavities, especially for cases with large tumor volumes.
Curettage combined with resection was performed in patients with extensive lesions, including lesions classified as Campanacci grade III, with a large tumor volume or focus, a tumor breaking through the articular surface, and involving the articular cavity. In this procedure, the cortical bone and soft tissue mass are removed, and the tumor cavity is excavated using a curette and high-speed burr. Subsequently, cavitary bone defects are filled with allogeneic particle bone grafts, and an anatomical bone plate is used for internal fixation (Fig. 4).
The diagrammatic drawing of curettage combined with resection: (a) Indications: with an extensive lesion, with around soft tissue mass, the part broken cortical bone without possible of reserve, with a tumor involved the articular cavity or cruciate ligament. (b) To remove the cortical bone and soft tissue mass without possible of reserve, and continued to dispose the tumor cavity using curette and a high-speed burr. (c) To fill the cavitary bone defects with allogenic particle bone graft, and internal fixation using an anatomical bone plate.
En bloc marginal resection was indicated for patients with extensive bone cortex lesions along with large soft tissue masses. With this procedure, the osteotomy plane is confirmed via preoperative magnetic resonance imaging and the tumor is resected en bloc. An articulated prosthesis is used to reconstruct the knee (Fig. 5).
The diagrammatic drawing of en bloc marginal resection: (a) Indications: with extensive bone cortex lesions together with around large soft tissue mass. An osteotomy plane was confirmed based on preoperative magnetic resonance imaging (dashed line indicated the osteotomy plane). (b) To resect the en bloc tumor, and to reconstruct the knee using an articulated prosthesis.
Follow-up and Functional Outcomes
Patients were followed-up every 3 months for the first 2 years post-surgery, every 6 months for the following 3 years, and finally every 12 months in the subsequent 5 years. Telephone interviews were available only after 5 years of follow-up. The MSTS score (total possible score = 30) was used to assess functional outcomes40.
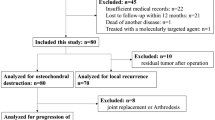
Of the 410 included patients, 304 completed ≥12 months of follow-up (response rate, 74.1%), with a median follow-up time of 55 months (range, 12–188 months). Of these patients, 252 (82.9%) received face-to-face follow-up with physical and radiological examinations at the 7 participating hospitals; 52 (17.1%) were also contacted via telephone, with their physical and radiological examinations performed at local hospitals (Fig. 6).
Flow chat of patients’ selection.
Of the 410 included patients, 304 completed ≥12 months of follow-up (response rate, 74.1%), with a median follow-up time of 55 months (range, 12–188 months). Of these patients, 252 (82.9%) received face-to-face follow-up with physical and radiological examinations at the 7 participating hospitals; 52 (17.1%) were also contacted via telephone, with their physical and radiological examinations performed at local hospitals.
Statistical Methods
Clinical features were assessed, including the tumor side and location, Campanacci grade, presence of pathological fracture, and treatment technique. The local recurrence rates and relevant risk factors were analysed according to the clinical characteristics in patients with at least 12 months of follow-up. Continuous variables are summarized as means (standard deviations) or medians (ranges), and differences between the groups were assessed using the Student t-test or Mann-Whitney U test, as appropriate. Categorical variables are presented as case numbers (percentages), and the chi-square test was used to assess the differences in clinical characteristics and surgical treatment according to local recurrence. Kaplan-Meier survival estimates were used for univariate survival analyses, while the Cox proportional hazards regression model was used for multivariate analysis of risk factors for local recurrence that were found to be significant in the univariate analysis. Risk factors for local recurrence are presented using HRs with 95% CIs. All statistical analyses were performed using SPSS version 15.0 (SPSS Inc., Chicago, IL), and two-tailed P values <0.05 were considered statistically significant.
Additional Information
How to cite this article: Hu, P. et al. Recurrence Rates and Risk Factors for Primary Giant Cell Tumors around the Knee: A Multicentre Retrospective Study in China. Sci. Rep. 6, 36332; doi: 10.1038/srep36332 (2016).
Publisher’s note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
Campanacci, M. In Bone and soft tissue tumors: clinical features, imaging, pathology and treatment 2nd edn (Springer, 1999).
van der Heijden, L., Dijkstra, P. D., Campanacci, D. A., Gibbons, C. L. & van de Sande, M. A. Giant cell tumor with pathologic fracture: should we curette or resect? Clin Orthop Relat Res . 471, 820–829 (2013).
Hu, Y., Chen, Y. & Lun, D. The establishing and verification of clinical scoring system for giant cell tumor. Chinse Journal of Orthopadics . 3l, 105–112 (2011).
Klenke, F. M., Wenger, D. E., Inwards, C. Y., Rose, P. S. & Sim, F. H. Giant cell tumor of bone: risk factors for recurrence. Clin Onhop Relat Res. 469, 591–599 (2011).
Tureotte, R. E. Giant cell tumor of bone. Onhop Clin Noah Am . 37, 35–51 (2006).
Niu, X. et al. Giant Cell Tumor of the Extremity: Retrospective Analysis of 621 Chinese Patients from One Institution. J Bone Joint Surg Am . 94, 461–467 (2012).
Thomas, D. M. & Skubitz, T. Giant-cell tumour of bone. Current Opinion in Oncology . 21, 338–344 (2009).
von Steyern, F. V. et al. Giant-cell tumor of the knee: the condition of the cartilage after treatment by curettage and cementing. J Bone Joint Surg Br . 89, 361–365 (2007).
Puthoor, D. K. & Puthezhath, K. Management of giant cell tumor of bone: computerized tomography based selection strategy and approaching the lesion through the site of cortical break. Orthop Surg . 4, 76–82 (2012).
Ansari, M. T., Prakash, P. K. & Machhindra, M. V. Wrist preserving surgery for multifocal giant cell tumor of carpal bones in a skeletally immature patient: a case report. Orthop Surg . 6, 322–325 (2014).
Xie, M. et al. Giant cell tumor of the tendon sheath of the toe. Orthop Surg . 3, 211–215 (2011).
Karpik, M. Giant Cell Tumor (tumor gigantocellularis, osteoclastoma)–epidemiology, diagnosis, treatment. Ortop Traumatol Rehabil. 12, 207–215 (2010).
Muramatsu, K., Ihara, K. & Taguchi, T. Treatment of Giant Cell Tumor of Long Bones: Clinical Outcome and Reconstructive Strategy for Lower and Upper Limbs. Orthopedics . 32, 491–497 (2009).
Balke, M. et al. Giant cell tumor of bone: treatment and outcome of 214 cases. J Cancer Res Clin Oncol . 134, 969–978 (2008).
Errani, C. et al. Giant cell tumor of the extremity: a review of 349 cases from a single institution. Cancer Treat Rev . 36, 1–7 (2010).
Larsson, S. E., Lorentzon, R. & Boquist, L. Giant-cell tumor of bone. A demographic, clinical, and histopathological study of all cases recorded in the Swedish Cancer Registry for the years 1958 through 1968. J Bone Joint Surg Am. 57, 167–173 (1975).
Dahlin, D. C. Giant cell tumor of bone: highlights of 407 cases. AJR Am J Roentgenol . 144, 955–960 (1985).
Campanacci, M., Baldini, N., Boriani, S. & Sudanese, A. Giant-cell tumor of bone. J Bone Joint Surg Am . 69, 106–114 (1987).
Gupta, R. et al. Clinicopathologic profile of 470 giant cell tumors of bone from a cancer hospital in western India. Ann Diagn Pathol . 12, 239–248 (2008).
Enneking, W. F. Giant cell tumor. In Musculoskeletal tumor surgery. 1435–1468 (Churchill-Livingstone, 1983).
O’Donnell, R. J. et al. Recurrence of giant-cell tumors of the long bones after curettage and packing with cement. J Bone Joint Surg Am . 76, 1827–1833 (1994).
National Bureau of Statistics of China. Population. In China Statistical Yearbook 33–52 (China Statistics Press, 2015).
Hu, Y. The prognosis factors of surgical treatment in patients with giant cell tumor of bone around the knee. Chin J Orthop . 32, 1083–1090 (2012).
Vult von Steyern, F. et al. Treatment of local recurrences of giant cell tumour in long bones after curettage and cementing. A Scandinavian Sarcoma Group study. J Bone Joint Surg Br . 88, 531–535 (2006).
Saiz, P. et al. Results of giant cell tumor of bone treated with intralesional excision. Clin Orthop Relat Res . 424, 221–226 (2004).
Sung, H. W. et al. Giant-cell tumor of bone: analysis of two hundred and eight cases in Chinese patients. J Bone Joint Surg Am . 64, 755–761 (1982).
Blackley, H. R. et al. Treatment of giant-cell tumors of long bones with curettage and bone-grafting. J Bone Joint Surg Am . 81, 811–820 (1999).
Kivioja, A. H. et al. Cement is recommended in intralesional surgery of giant cell tumors: A scandinavian sarcoma group study of 294 patients followed for a median time of 5 years. Acta Orthopaedica . 79, 86–93 (2008).
Algawahmed, H., Turcotte, R., Farrokhyar, F. & Ghert, M. High-speed burring with and without the use of surgical adjuvants in the intralesional management of giant cell tumor of bone: a systematic review and meta-analysis. Sarcoma . 2010, 586090 (2010).
Turcotte, R. E. et al. Giant cell tumor of long bone: a Canadian Sarcoma Group study. Clin Onhop Relat Res. 397, 248–258 (2002).
Saglik, Y. et al. Giant cell tumor of bone. Bull Hosp Jt Dis . 58, 98–104 (1999).
Richardson, M. J. & Dickinson, I. C. Giant cell tumour of bone. Bull Hosp Jt Dis . 57, 6–10 (1998).
Bini, S. A., Gill, K. & Johnston, J. O. Giant cell tumor of bone: Curettage and cement reconstruction. Clin Orthop . 321, 245–250 (1995).
Mjoberg, B., Pettersson, H., Rosenqvist, R. & Rydholm, A. Bone cement, thermal injury and the radiolucent zone. Acta Orthop Scand . 55, 597–600 (1984).
Nelson, D. A., Barker, M. E. & Hamlin, B. H. Thermal effects of acrylic cementation at bone tumour sites. Int J Hyperthermia . 13, 287–306 (1997).
Prosser, G. H., Baloch, K. G., Tillman, R. M., Carter, S. R. & Grimer, R. J. Does curettage without adjuvant therapy provide low recurrence rates in giant-cell tumors of bone? Clin Orthop Relat Res . 435, 211–218 (2005).
Rooney, R. J., Asirvatham, R., Lifeso, R. M., Ali, M. A. & Parikh, S. Giant cell tumour of bone. A surgical approach to grade III tumours. Int Orthop . 17, 87–92 (1993).
Jeys, L. M. et al. Impending fractures in giant cell tumours of the distal femur: incidence and outcome. Int Orthop . 30,135–138 (2006).
van der Heijden, L. et al. The clinical approach toward giant cell tumor of bone. Oncologist . 19, 550–561 (2014).
Enneking, W. F., Dunham, W., Gebhardt, M. C., Malawar, M. & Pritchard, D. J. A system for the functional evaluation of reconstructive procedures after surgical treatment of tumors of the musculoskeletal system. Clin Orthop Relat Res . 286, 241–246 (1993).
Acknowledgements
We thank all the participants of this study and the local doctors for their enthusiasm, tireless work, and sustained support.
Author information
Authors and Affiliations
Contributions
Y.Z. and Y.H. was involved in the conception and design, data collection, data interpretation, and critical review of this article. P.H. was involved in the data interpretation and drafting of this manuscript. F.L., L.Z., H.Z., X.Y., Z.W., S.W., Z.Y., S.G. and G.Z. were involved in the data collection, case diagnosis, and approval of this article. J.W. and X.N. were involved in the conception and design, data analysis, data interpretation, and critical review of this article.
Ethics declarations
Competing interests
The authors declare no competing financial interests.
Rights and permissions
This work is licensed under a Creative Commons Attribution 4.0 International License. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in the credit line; if the material is not included under the Creative Commons license, users will need to obtain permission from the license holder to reproduce the material. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/
About this article
Cite this article
Hu, P., Zhao, L., Zhang, H. et al. Recurrence Rates and Risk Factors for Primary Giant Cell Tumors around the Knee: A Multicentre Retrospective Study in China. Sci Rep 6, 36332 (2016). https://doi.org/10.1038/srep36332
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/srep36332
This article is cited by
-
Giant cell tumors of the distal ulna: long-term recurrence rate and functional outcomes of en bloc resection versus curettage in a multicenter study
Journal of Orthopaedic Surgery and Research (2023)
-
The expression changes of PD-L1 and immune response mediators are related to the severity of primary bone tumors
Scientific Reports (2023)
-
Giant cell tumor of bone in the pediatric population: a retrospective study highlighting cases of metaphyseal only location and increased local recurrence rates in skeletally immature patients
Skeletal Radiology (2023)
-
“A New Clinical and Radiological Classification of Grading GCT and Its Impact on the Management”
Indian Journal of Orthopaedics (2023)
-
Effect of bisphosphonates on bone giant cell tumor recurrence: a meta-analysis
Beni-Suef University Journal of Basic and Applied Sciences (2022)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.