Abstract
It is unclear whether osteoporosis itself is a main risk factor for delayed wound healing after tooth extraction in humans. In this study, we evaluated the association between experience of delayed wound healing after last tooth extraction and self-reported kyphosis, with the possibility of having vertebral fractures, in Japanese patients. Among the 1,504 patients who responded to the structured questionnaire survey, 518 patients (134 men and 384 women) aged 55–97 years finally participated in this study. Patients who self-reported mild-moderate kyphosis were more likely to have problematic delayed wound healing after last tooth extraction than those who reported severe kyphosis (odds ratio [OR] 4.98; 95% confidence interval [CI], 1.86–13.38 and OR 2.30; 95% CI, 0.52–10.22, respectively) (p for trend = 0.005). Japanese patients with vertebral fractures may have a higher risk of having problematic delayed wound healing after tooth extraction.
Similar content being viewed by others
Introduction
Marx and Ruggiero et al. reported that Bisphosphonates (BP) treatment may increase the risk of osteonecrosis of the jaws (ONJ) in osteoporosis (OP) and oncology patients1,2, and the latter defined delayed wound healing after tooth extraction as ONJ2. Thus, views on the use of BPs for patients with OP vary among physicians, dentists, and patients. In 2015, the incidence of ONJ in OP patients was reported to be 0.001–0.01%, which may be only slightly higher than the frequency observed in the general population3. However, because of the paucity of prospective cohort data, it is difficult to accurately evaluate ONJ incidence3. The number of reports on ONJ increased until 2010, whereupon it plateaued. Conversely, numerous reports on BP-related ONJ (BRONJ) have been published since 2015, which includes international consensus report of ONJ3. Also, there have been many reports on the ONJ potentially caused by denosumab which inhibits bone metabolism like BP recently.
The diagnostic guideline of chronic disease is based on the threshold of surrogate markers that show increased risks of disease development as a complication. OP has been defined as “a skeletal disorder characterized by compromised bone strength, predisposing a person to increased risk of fracture”4. The surrogate marker for OP is bone mineral density (BMD), and BMD values with presence of high fracture risk are the diagnostic guideline of OP. According to the treatment recommendations of the National Osteoporosis Foundation (NOF), initial pharmacologic treatment factors could be hip or vertebral (clinical or asymptomatic) fractures5. Thus, the most apparent diagnostic evidence of OP is the complication of fragile fracture.
Several reports suggested that despite the high prevalence of vertebral fracture, many vertebral fractures remain undiagnosed. Because vertebral fractures are diagnosed using radiography, even patients without factures must be exposed to radiation6,7. Therefore, it is important to explore alternatives to radiography for diagnosing asymptomatic vertebral fracture, especially when considering large number of these patients8.
A recent questionnaire-based survey by the Japanese Society for Oral and Maxillofacial Surgeons indicated the rapid increase of ONJ (approximately 20-fold for patients both using and not using BP) in Japan when they compared the number of ONJ cases reported in 2006–2008 with that in 2011–2013 (unpublished data). BPs have been approved in Japan since 2001. ONJ overdiagnosis may occur because ONJ is broadly recognized among the dentists who may not be familiar with ONJ and likely to overdiagnose it.
Until recently, a large number of studies have addressed the potential role of BPs on jaw bones. However, there has been no strict control group with respect to OP characteristics against the patient’s group. Furthermore, the pathophysiology of ONJ is not well understood. Tanoue et al. recently demonstrated that bone formation was not impeded by short-term alendoronate treatment but was enhanced during wound healing after tooth extraction9. They concluded that alendoronate did not alter bone fill in extraction sockets. Additionally, some studies including randomized, placebo-controlled trials suggested that oral BP treatment may improve clinical outcomes of non-surgical periodontal therapy10,11. These results suggested that OP itself may be a main risk factor for delayed wound healing after tooth extraction. Therefore, both infection and delayed wound healing after tooth extraction may lead to an increased risk of prolonged bone repair and osteomyelitis of the jaws in OP patients.
Some studies have reported OP itself as a risk factor of ONJ3,12. However, to our knowledge, no previous study has reported the association between OP and delayed wound healing after tooth extraction. Approximately two thirds of women with radiographic evidence of vertebral fracture are unaware of the fracture13. However, we recently demonstrated that a self-reported kyphosis may be a useful marker for identifying postmenopausal women with asymptomatic vertebral fractures14. Therefore, in this study, we evaluated the association between self-reported experience of delayed wound healing after tooth extraction and self-reported kyphosis, which represents the potential presence of vertebral fractures, in Japanese men and women.
Results
Participants
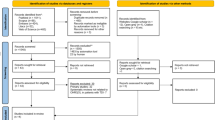
During the study period, a total of 1,504 patients from 8 clinics or hospitals responded to a structured questionnaire with written informed consent. Of these, 617 patients who had missing or unclear responses in their questionnaires were excluded from this study. Of the remaining 887 patients, 369 patients who were treated using OP medications before their last tooth extractions were also excluded. Finally, 518 patients (134 men and 384 women) aged 55–97 years participated in this study. Patient characteristics are shown in Table 1. Regarding the time of last tooth extraction, 102 (19.7%) patients had undergone last tooth extraction <1 year previously, 69 (13.3%) patients between 1 and 3 years previously, and 347 (67.0%) patients >3 years previously. Three, three, and 25 patients experienced delayed wound healing after extraction, respectively.
Association between delayed wound healing and self-reported kyphosis
ANOVA revealed significant differences in age (p = 0.011), height (p = 0.012), weight (p = 0.001), and number of teeth lost throughout the patient’s lifetime (p = 0.028) among the three self-reported kyphosis categories (Table 2). Additionally, self-reported kyphosis category was significantly associated with a self-reported periodontal condition (p = 0.040), history of smoking (p = 0.004) and delayed wound healing after last tooth extraction (p = 0.002). However, there was no significant association between time of last tooth extraction and self-reported kyphosis category (p = 0.703).
Stepwise logistic regression analysis with forward selection revealed that the odds ratio of having delayed wound healing after last tooth extraction according to steroid use was 4.60 (95% CI, 1.14–18.46) (Table 3). Moreover, the odds ratios for having delayed wound healing after last tooth extraction according to self-reported mild-moderate and severe kyphosis were 4.98 (95% CI, 1.86–13.38) and 2.30 (95% CI, 0.52–10.22), respectively (p for trend = 0.005).
Discussion
To our knowledge, this is the first study demonstrating the association between experience of delayed wound healing after tooth extraction and self-reported kyphosis. Patients with self-reported mild-to-moderate kyphosis had an approximately 5-fold higher risk of delayed wound healing after last tooth extraction compared with those with self-reported no kyphosis. Our results revealed the possibility that vertebral fracture associated with OP might cause an increased risk of delayed wound healing after tooth extraction. Moreover, as a previous study defined delayed wound healing after tooth extraction as ONJ2, OP itself might lead to a risk of ONJ.
Japanese dentists generally worry about performing minor oral surgeries such as tooth extraction, which is considered a potential risk factor for ONJ15, because they believe that ONJ is a severe adverse event that cannot be treated. Moreover, Japanese dentists have recently tended to avoid tooth extraction for OP patients who have used BPs and/or other OP agents, such as vitamin D16. It has also been reported that delay of tooth extraction due to BP drug holiday increases the occurrence of ONJ16. These facts may contribute to the recent rapid increase of ONJ cases in Japan (unpublished data). However, a study demonstrated that >90% of OP patients treated with oral BPs could be cured, whereas 50% of oncology patients treated with intravenous BPs did not show improvement17.
Huang et al., using data from the National Health Insurance system of Taiwan, concluded that OP patients had a significantly higher risk of ONJ than healthy persons (adjusted hazard ratio 2.05; 95% CI, 1.58–2.65)12. Moreover, dental history, such as tooth extraction, may play an important role in the incidence of ONJ, while BPs have a synergistic effect. Conversely, Tennis et al. reported that in their sex- and age-matched OP cohort (n = 31,244), the ONJ incidence was 0.26 per 1,000 person-years (95% CI, 0.06–0.47) for patients not exposed to BPs, which decreased to 0.15 (95% CI, 0.00–0.36) after oral BP use18. Additionally, Cartsos et al. reported that the OR was 0.65 (96% CI, 0.54–0.79) in oral BP-treated OP patients with ONJ in their cohort of 714,217 patients19. These results showed that oral BP use may actually decrease the incidence of ONJ. However, the predominant concern in these previous studies is the lack of a strict control group with similar OP characteristics as the patient group. Therefore, studies that categorize patients using BMD values and/or fragility fractures, such as this study, are required.
In this study, patients with self-reported mild-to-moderate kyphosis had an approximately 5-fold higher risk of delayed wound healing after last tooth extraction (p = 0.001). In a previous study, patients who self-reported mild-to-moderate and severe kyphosis had a higher risk of vertebral fractures (OR 2.1; 95% CI, 1.4–3.3 and OR 4.2; 95% CI, 1.8–9.5, respectively)14. These findings suggest that subjects with vertebral fractures might have an increased risk of delayed wound healing. However, the lack of a significant association between self-reported severe kyphosis and experience of delayed wound healing may contradict this possibility. The small number of patients with self-reported severe kyphosis may have influenced the results. Additionally, in the crude data (see Table 2), there was no significant difference in age and number of teeth lost between subjects with self-reported no and mild-to-moderate kyphosis, whereas a significant difference was observed in the number of teeth lost between subjects with self-reported no and severe kyphosis. This result was consistent with a recent study20. The small number of remaining teeth may result in a decreased risk of infection. It is therefore possible that subjects with self-reported severe kyphosis may have a lower risk of oral cavity infection.
Various risk factors, such as glucocorticoid use, have been reported to affect healing failure after tooth extraction21,22. In this study, steroid use was significantly associated with an increased risk of delayed wound healing. Almazrooa and Woo described the causes of ONJ as follows: systemic steroids; radiation; bacterial, viral and deep fungal infections; direct chemical toxicity; trauma; avascular necrosis for temporomandibular joint; neuralgia-inducing cavitational osteonecrosis; osteomyelitis associated with sclerotic osseous diseases; and malignancy21. Powel et al. described that most osteonecrosis cases are secondary to systemically administered corticosteroids and/or high-dose therapy, particularly in patients with underlying comorbidities including connective tissue diseases, hyperlipidemia, or previous trauma22. Our finding regarding steroid use is consistent with previous reports. However, a history of diabetes mellitus was not associated with delayed wound healing. Additionally, Huang et al. described that the traditional view that people with diabetes have increased risk of delayed healing was not supported in their study23. Fernandes et al. also reported that although patients with type 2 diabetes mellitus may have impaired neutrophil function, this condition was not associated with an increased risk of experiencing postoperative complications24.
It remains unclear whether OP is associated with delayed wound healing after tooth extraction, although OP is associated with the progression of periodontal disease and subsequent tooth loss, especially in postmenopausal women25. Using an ovariectomy (OVX) rat model, Zecchin et al. concluded that the absence of estrogen may contribute to delayed alveolar wound healing after tooth extraction by interfering with extracellular matrix turnover26. Pereira et al. also reported that initial molecular changes observed in the absence of estrogen led to delayed alveolar wound healing in OVX rats27. Shum et al. demonstrated that OP was associated with severe periodontal disease, representing severe clinical attachment loss and interproximal gingival recession, in older Chinese men28. Famili et al. showed that men with prostate cancer undergoing androgen deprivation therapy were more likely to have periodontal disease than men not such therapy29. The etiologies of OP and decreased estrogen and/or androgen concentration might contribute to an increased risk of oral cavity infection.
There are some limitations associated with this study. The primary limitation is that patient responses concerning kyphosis were not obtained at the time of last tooth extraction. Although we selected last tooth extraction to reduce recall bias as much as possible, 347 (67.3%) of all respondents underwent last tooth extraction ≥3 years before the questionnaire survey. Of the 23 subjects who reported mild-to-moderate kyphosis and had experienced delayed wound healing after last tooth extraction, 17 (74%) had undergone tooth extraction more than 3 years previously. Some of these 23 subjects might have had no self-reported kyphosis when their teeth were extracted. Of the five patients who self-reported no kyphosis and had delayed wound healing, three patients underwent extraction more than 3 years previously.
The second limitation is the validity of self-reported delayed wound healing after tooth extraction. It is possible that patients might not associated wound healing failure with dental treatment received. Rather, patients may compare the wound healing status after the last tooth extraction with previous extractions. Additionally, the feeling of problematic delayed wound healing is subjective. However, the lack of significant differences in age, number of teeth lost, and daily number of tooth brushing between subjects with self-reported no and mild-to-moderate kyphosis may suggest little difference in the feeling of problematic delayed wound healing after last tooth extraction.
Ideally, a standard duration of wound healing after tooth extraction is desirable. However, the duration of wound healing after tooth extraction varies among patients according to their underlying conditions. The duration of primary wound healing is typically considered to be within 1 month. Hasegawa et al. found that the duration of primary wound healing after tooth extraction in 378 patients who received oral BP therapy was primarily within 4 weeks (94.4% of patients)30. Although problematic delayed wound healing after tooth extraction is clinically important, it is unknown whether a patient’s perception of delayed wound healing is associated with prolonged duration of wound healing.
The third limitation is the validity of self-reported kyphosis in men. The association between self-reported kyphosis and risk of having vertebral fractures in women, but not in men, was recently demonstrated14. The prevalence of Japanese OP patients aged ≥40 years was 3.4% of men and 19.2% of women31. However, the prevalence of patients with lumbar spondylosis was greater among men than women. Self-reported kyphosis is influenced by lumbar spondylosis and spinal degeneration in men. This may contribute to the lack of a significant association between self-reported severe kyphosis and delayed wound healing, although patients with self-reported severe kyphosis had a higher risk of having problematic delayed wound healing after tooth extraction (OR 2.30; 95% CI, 0.52–10.22).
The strength of this study was the comparison of patients with a strict control group using the self–reported kyphosis questionnaire. In previous studies of ONJ, control groups that evaluated the osteoporotic condition were not included. Huang et al. concluded that OP patients had a significantly higher risk of ONJ than healthy persons, and BP therapy had a synergistic effect12. Although their study did not evaluate OP, the authors showed the possibility that patients treated with BP might have had severe OP accompanied by fractures. Thus, it remains inconclusive whether BP increases ONJ.
In this study, subjects with self-reported mild-to-moderate kyphosis had a significantly higher risk of problematic delayed wound healing after last tooth extraction compared with those with self-reported no kyphosis. Therefore, patients with vertebral fractures associated with OP may be at greater risk of ONJ after tooth extraction. Further studies including patients with concurrent vertebral fractures and delayed wound healing after tooth extraction are necessary to confirm our findings.
Methods
Questionnaire-based survey
All patients aged ≥ 50 years who visited our 8 clinics or hospitals from June to August 2014 were invited to complete a structured questionnaire. Patients who had been treated using OP medications (such as BPs) before last tooth extraction, refused to provide written informed consent, and/or had hip fracture when answering the structured questionnaire were excluded from the study. The status of OP medication use was confirmed in each clinic or hospital. Patients who provided many missing or unclear responses were also excluded from the study. The structured questionnaire aimed at collecting the following information: presence of problematic delayed wound healing after last tooth extraction, self-reported kyphosis, number of teeth lost throughout the patient’s lifetime, self-reported periodontal condition, daily number of tooth brushing, history of smoking, history of diabetes mellitus, steroid use, rheumatoid arthritis, and time of last tooth extraction (<1 year, 1–3 years, >3 years). Self-reported kyphosis was defined using three categories as previously described14: none, mild-moderate, and severe. Self-reported periodontal condition was divided into two categories: no periodontal symptom and some symptoms like bleeding (with and without brushing), swelling and/or tooth mobility according to our previous study32. To reduce recall bias, the presence of delayed wound healing was determined for last tooth extraction.
The Ethics Committee of Matsumoto Dental University reviewed and approved the study protocol. The methods were carried out in accordance with the relevant guidelines. Written informed consent was obtained from all participants.
Statistical analysis
Continuous variables are expressed as means ± standard deviation (SD). The chi-squared test or one-way analysis of variance (ANOVA) was used to investigate differences in age, gender (women), height (cm), weight (kg), number of teeth lost throughout the patient’s lifetime, self-reported periodontal condition (no or some symptoms), daily frequency of tooth brushing, history of smoking (yes or no), diabetes mellitus (yes or no), steroid use (yes or no), rheumatoid arthritis (yes or no), delayed wound healing after last tooth extraction (yes or no), and time of last tooth extraction (<1 year, 1–3 years, >3 years) among the three self-reported kyphosis categories.
Stepwise logistic regression analysis with forward selection, adjusted for age, gender (women), height (cm), weight (kg), number of teeth lost throughout the patient’s lifetime, self-reported periodontal condition (binary), daily number of tooth brushing, history of smoking (binary), diabetes mellitus (binary), steroid use (binary), and rheumatoid arthritis (binary), was used to calculate odds ratios (OR) and 95% confidence intervals (CI) of delayed wound healing after last tooth extraction according to the self-reported kyphosis category. Data were analyzed using the Statistical Package for the Social Sciences (SPSS, version 22.0; IBM Inc., Chicago, IL, USA). P-values < 0.05 were considered statistically significant.
Additional Information
How to cite this article: Taguchi, A. et al. Delayed wound healing after tooth extraction and self-reported kyphosis in Japanese men and women. Sci. Rep. 6, 36309; doi: 10.1038/srep36309 (2016).
Publisher’s note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
Marx, R. E. Pamidronate (Aredia) and zoledronate (Zometa) induced avascular necrosis of the jaws: a growing epidemic. J. Oral. Maxillofac. Surg. 61, 1115–1117 (2003).
Ruggiero, S. L. et al. Osteonecrosis of the jaws associated with the use of bisphosphonates: a review of 63 cases. J. Oral. Maxillofac. Surg. 62, 527–534 (2004).
Khan, A. A. et al. Diagnosis and management of osteonecrosis of the jaw: a systematic review and international consensus. J. Bone. Miner. Res. 30, 3–23 (2015).
NIH Consensus Development Panel. Osteoporosis prevention, diagnosis, and therapy. JAMA 285, 785–795 (2001).
Cosman, F. et al. Clinician’s guide to prevention and treatment of osteoporosis. Osteoporos. Int. 25, 2359–2381 (2014).
Ross, P. D. Clinical consequences of vertebral fractures. Am. J. Med. 10, 30S–42S (1997).
Guermazi, A. et al. Identification of vertebral fractures in osteoporosis. Semin. Musculoskelet. Radiol. 6, 241–2252 (2002).
Ashar, B. H. et al. Current evidence for the use of emerging radiologic technologies for disease screening. Am. J. Manag. Care 11, 385–392 (2005).
Tanoue, R., Koi, K. & Yamashita, J. Effect of alendronate on bone formation during tooth extraction wound healing. J. Dent. Res. 94, 1251–1258 (2015).
Lane, N. et al. Bisphosphonate therapy improves the outcome of conventional periodontal treatment: results of a 12-month, randomized, placebo-controlled study. J. Periodontol. 76, 1113–1122 (2005).
Bhavsar, N. V. et al. Clinical and radiographic evaluation of effect of risedronate 5 mg as an adjunct to treatment of chronic periodontitis in postmenopausal women (12-month study). Osteoporos. Int., in press.
Huang, Y. F. et al. Impact of bisphosphonate-related osteonecrosis of the jaw on osteoporotic patients after dental extraction: a population-based cohort study. PLoS One 16, e0120756 (2015).
Kendler, D. L. et al. Vertebral fractures: Clinical importance and management. Am. J. Med. 129, 221.e1–221.e10 (2016).
Kamimura, M. et al. Associations of self-reported height loss and kyphosis with vertebral fractures in Japanese women 60 years and older: a cross-sectional survey. Sci. Rep. 6, 29199 (2016).
Marx, R. E., Sawatari, Y., Fortin, M. & Broumand, V. Bisphosphonate-induced exposed bone (osteonecrosis/osteopetrosis) of the jaws: risk factors, recognition, prevention, and treatment. J. Oral. Maxillofac. Surg. 63, 1567–1575 (2005).
Taguchi, A., Shiraki, M., Sugimoto, T., Ohta, H. & Soen, S. Japan Osteoporosis Society. Lack of cooperation between physicians and dentists during osteoporosis treatment may increase fractures and osteonecrosis of the jaw. Curr. Med. Res. Opin. 32, 1261–1268 (2016).
Shintani, T. et al. Comparison of the prognosis of bisphosphonate-related osteonecrosis of the jaw caused by oral and intravenous bisphosphonates. Int. J. Oral. Maxillofac. Surg. 44, 840–844 (2015).
Tennis, P. et al. Incidence of osteonecrosis of the jaw among users of bisphosphonates with selected cancers or osteoporosis. Pharmacoepidemiol. Drug Saf. 21, 810–817 (2012).
Cartsos, V. M., Zhu, S. & Zavras, A. I. Bisphosphonate use and the risk of adverse jaw outcomes: a medical claims study of 714,217 people. J. Am. Dent. Assoc. 139, 23–30 (2008).
Taguchi, A. et al. Association of self-reported height loss and kyphosis with loss of teeth in Japanese elderly. Oral. Health. Dent. Manag. 15, 69–74 (2016).
Almazrooa, S. A. & Woo, S. B. Bisphosphonate and nonbisphosphonate-associated osteonecrosis of the jaw: a review. J. Am. Dent. Assoc. 140, 864–875 (2009).
Powell, C., Chang, C., Naguwa, S. M., Cheema, G. & Gershwin, M. E. Steroid induced osteonecrosis: An analysis of steroid dosing risk. Autoimmun. Rev. 9, 721–743 (2010).
Huang, S., Dang, H., Huynh, W., Sambrook, P. J. & Goss, A. N. The healing of dental extraction sockets in patients with Type 2 diabetes on oral hypoglycaemics: a prospective cohort. Aust. Dent. J. 58, 89–93 (2013).
Fernandes, K. S., Glick, M., de Souza, M. S., Kokron, C. M. & Gallottini, M. Association between immunologic parameters, glycemic control, and postextraction complications in patients with type 2 diabetes. J. Am. Dent. Assoc. 146, 592–599 (2015).
Tak, I. H. et al. The association between periodontal disease, tooth loss and bone mineral density in a Korean population. J. Clin. Periodontol. 41, 1139–1144 (2014).
Zecchin, K. G., Pereira, M. C., Coletta, R. D., Graner, E. & Jorge, J. Ovariectomy reduces the gelatinolytic activity and expression of matrix metalloproteinases and collagen in rat molar extraction wounds. Calcif. Tissue Int. 76, 136–145 (2005).
Pereira, M. C., Zecchin, K. G., Campagnoli, E. B. & Jorge, J. Ovariectomy delays alveolar wound healing after molar extractions in rats. J. Oral. Maxillofac. Surg. 65, 2248–2253 (2007).
Shum, I. et al. Periodontal conditions in elderly men with and without osteoporosis or osteopenia. J. Periodontol. 81, 1396–1402 (2010).
Famili, P., Cauley, J. A. & Greenspan, S. L. The effect of androgen deprivation therapy on periodontal disease in men with prostate cancer. J. Urol. 177, 921–924 (2007).
Hasegawa, T. et al. The observational study of delayed wound healing after tooth extraction in patients receiving oral bisphosphonate therapy. J. Craniomaxillofac. Surg. 41, 558–563 (2013).
Yoshimura, N. et al. Prevalence of knee osteoarthritis, lumbar spondylosis, and osteoporosis in Japanese men and women: the research on osteoarthritis/osteoporosis against disability study. J. Bone. Miner. Metab. 27, 620–628 (2009).
Taguchi, A. et al. Relationship between self-reported periodontal status and skeletal bone mineral density in Japanese postmenopausal women. Menopause 12, 144–148 (2005).
Author information
Authors and Affiliations
Contributions
A.T., M.K. and Y.N. wrote the main manuscript text. A.T., N.S. and S.I. performed statistical analyses. M.K., Y.N., N.S., A.I., H.M., T.F., R.A., K.T., S.G. and K.M. collected samples. A.T., M.K., Y.N., S.I., S.U. and H.K. discussed all of the data. A.T., M.K. and N.S. prepared the Tables 1–3. All authors reviewed the manuscript.
Ethics declarations
Competing interests
The authors declare no competing financial interests.
Rights and permissions
This work is licensed under a Creative Commons Attribution 4.0 International License. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in the credit line; if the material is not included under the Creative Commons license, users will need to obtain permission from the license holder to reproduce the material. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/
About this article
Cite this article
Taguchi, A., Kamimura, M., Nakamura, Y. et al. Delayed wound healing after tooth extraction and self-reported kyphosis in Japanese men and women. Sci Rep 6, 36309 (2016). https://doi.org/10.1038/srep36309
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/srep36309
This article is cited by
-
Fragility fractures and delayed wound healing after tooth extraction in Japanese older adults
Journal of Bone and Mineral Metabolism (2020)
-
Long waiting time before tooth extraction may increase delayed wound healing in elderly Japanese
Osteoporosis International (2019)
-
Significant improvement of bone mineral density and bone turnover markers by denosumab therapy in bisphosphonate-unresponsive patients: response to comments
Osteoporosis International (2017)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.