Abstract
In order to prevent cardiovascular endpoints, control of diabetes, hypertension and hypercholesterolemia is a necessity as those risk factors frequently occur in combination. Prevalence trends of concurrent diabetes, hypertension and hypercholesterolemia in 36,673 subjects were obtained from the National Health and Nutrition Examination Survey (NHANES) from 1999–2012. The prevalence of concurrent diabetes, hypertension and hypercholesterolemia increased from 3% in 1999–2000 to 6.3% in 2011–2012 (P < 0.001). The diabetes with concurrent hypertension or hypercholesterolemia incidences also increased significantly, while the occurrence of concurrent hypertension and hypercholesterolemia was stable over the study period. Overall medical drug treatments for concurrent diabetes, hypertension, hypercholesterolemia were improved from 69.8% in 1999–2006, to 82.4% in 2007–2012 (P = 0.002). Treatment cost coverage rates in any combinations with diabetes were 79–82.4% and 90.7% in the subgroup of concurrent hypertension and hypercholesterolemia. General treatment goal achievement rates were <25%, the lowest rate being 14.2% in the subject groups with three combined risk factors. The treatment goal achievement rates in two subgroups with concurrent diabetes were 20.1% (with hypertension) and 17% (with hypercholesterolemia) and 24.5% in the group without diabetes. Cost coverage improved in all combinations, but the general treatment goal achievement rates were low, especially in the groups with concurrent diabetes.
Similar content being viewed by others
Introduction
It is well documented that cardiovascular disease affects about two million American individuals each year and is the leading cause of mortality in the United States, making it a major medical challenge1.
The cardiovascular risks include hypertension, dyslipidemia, diabetes, obesity, smoking, age, etc. Three medical conditions namely diabetes, hypertension and hypercholesterolemia are recognized as major risk factors not only for cardiovascular disease but also for stroke and other conditions2,3,4,5,6,7. These three conditions present great challenges and constitute a heavy burden on health care in the United States and worldwide as well8,9,10.
During recent decades, there has been a substantial increase in the prevalence of diabetes along with obesity in adults in the United States. Although the control of diabetes has significantly improved, it still presents a major challenge11,12. The prevalence of hypertension was reported to be stable over time, while the treatment and control of hypertension has greatly improved13,14,15. However, the prevalence of hypercholesterolemia has remained at almost epidemic levels16,17,18. Furthermore, while significant improvements have been made in the therapeutic control of hypercholesterolemia, they are still less than satisfactory and the implementation of nationwide education programs to encouraging awareness of the severe risks associated with hypercholesterolemia have not been effective.
Although each of the three conditions produces unique cardiovascular risk factors, increasingly two or more are frequently found within one individual. For example, of hypertensive patients, 60% of them also present with diabetes, and 73% with dyslipidemia19. Of diabetic patients, 30% of them may also have dyslipidemia20. Data from the National Health Interview Survey (NHIS) found that approximately 26% of US adults had multiple (≥2) chronic conditions21. Any form of two or more of these conditions frequently coexisted22,23,24. Previous studies have indicated that the presence of multiple risk factors additively increases the risk of cardiovascular diseases25. While traditional disease management and epidemiology studies have focused on individual disease, there is robust evidence that concurrent comorbidities, especially the presence of any form of combination of diabetes, hypertension and dyslipidemia, has an even higher risk for the development of cardiovascular and renal diseases than each condition alone. Their impact on CVD events is thought to be additive26. Robust evidence supports the integrated management and measurement of cost effective risk factors, especially abnormalities in blood glucose, blood pressure and blood lipids27,28,29.
It is of great clinical interest for physicians and clinicians to study concurrent diabetes, hypertension and hypercholesterolemia in patients as it represents a unique clinical panorama, with important consequences for the patients. For concurrent diabetes and hypertension, the optimal selection of anti-hypertensive drugs and the optimal target are different from a patient suffering solely from hypertension, as recommended by the American Diabetes Association (ADA)30,31. The same also applies to concurrent diabetes and hypercholesterolemia. For treatment of concurrent hypercholesterolemia and diabetes, the target is more strict compared to hypercholesterolemia without diabetes, as recommended by the American College of Cardiology (ACA)/American Heart Association (AHA)32,33. For concurrent hypertension and hypercholesterolemia, this subgroup of patients would manifest itself with higher body mass indexes and being more prone to insulin resistance, compared to patients with hypertension alone24.
Unfortunately, there is a paucity of data available about the prevalence of concurrent comorbidities. There has been only one study concerning the prevalence of diabetes, hypertension and hypercholesterolemia in Switzerland; however, the authors reported the situation for each disease separately34. Two publications documented the prevalence of a combination of hypertension and dyslipidemia in the United Kingdom35 and the U.S.36, respectively, but they did not uncover a trend over time or the combined presence of diabetes.
The primary objectives of this investigation were to estimate the national trends in the prevalence, management and control of a combination of diabetes, hypertension and hypercholesterolemia in U.S. adults from 1999 to 2012. Combinations of any two conditions were also examined, as those groups might be of special interest to specialists.
Methods
Data
The National Health and Nutrition Examination Survey (NHANES) is a cross-sectional survey conducted by the National Center for Health Statistics, a branch of the Centers for Disease Control and Prevention (CDC). The study was approved by the National Center for Health Statistics Institutional Ethics Review Board, and all adult participants provided written informed consent37. All methods were performed in accordance with the Declaration of Helsinki regarding ethical standards for research involving human subjects. NHANES uses a complex, multistage and stratified sampling design to select a sample representative of the civilian and non-institutionalized resident population of the United States. The sampling procedure consists of four stages: primary sampling units (mostly counties), segments, households and individuals, respectively. Participants in NHANES filled in s at home, followed by physical and laboratory examinations at a mobile examination center. The NHANES questionnaires, laboratory tests and examinations have been previously described in the literature38.
NHANES interviewed and examined some 5,000 participants annually and the survey data released on a 2-year cycle. Response rates for participation in both interviews and physical examinations were similar across cycles and ranged from 75% to 80%39. The current investigation was based on NHANES data from 1999 to 2012, including all adult participants (aged ≥20 years), with complete data related to the definitions of diabetes, hypertension and hypercholesterolemia (vide infra). Pregnant women were excluded from the analysis.
Definitions
Diabetes was defined as a self-reported diagnosis by the participants or hemoglobin A1c (HbA1c) ≥6.5% or both. Self-reported diabetes was defined as the participant answered yes to at least one of the survey questions “Doctor said you have diabetes”, “now taking insulin” and “now taking diabetic pills to lower your blood sugar?” 25.6% of the diabetes cases were self-reported. HbA1c was measured in whole blood samples using high-performance liquid chromatography, performed on instruments certified by the National Glycohemoglobin Standardization Program and standardized to the reference method used in the Diabetes Control and Complications Trial11. We did not distinguish between type 1 and 2 diabetes.
Hypertension was defined as a systolic blood pressure (SBP) ≥140 mmHg or a diastolic blood pressure (DBP) ≥90 mmHg, or patients being treated with antihypertensive medication. The use of antihypertensive medication was defined as the participant answered yes to the survey question (Are you now taking prescribed medicine for HBP?). 38.8% of the hypertension cases were self-reported. Systolic and diastolic blood pressure levels were measured three to four times by mercury sphygmomanometer using a standard protocol to reduce variability. SBP and DBP were calculated by averaging multiple measurements.
Although low-density lipoprotein cholesterol (LDL) has been widely used as the standard biomarker for diagnosing lipid abnormalities, it was only measured in a subsample of the NHANES participants. To maximize the sample size, total serum cholesterol was used to define hypercholesterolemia. More specifically, hypercholesterolemia was defined as total serum cholesterol ≥200 mg/dL or on any concurrent pharmacologic lipid-lowering treatment or both. The use of therapy was based on an affirmative response to the survey question (Are you now following this advice to take prescribed medicine?). 17.0% of the hyperlipidemia cases were self-reported.
Treatment of diabetes was defined as a participant on insulin or other oral anti-diabetic drugs. Treatment of hypertension was defined as a patient taking antihypertensive medication. Treatment of hypercholesterolemia was defined as a patient taking prescribed lipid-lowering medication. The diabetes treatment goal achievement was defined as a HbA1c LEVEL <0.5%. The hypertension treatment goal achievement was defined as a SBP <140 mmHg and a DBP <90 mmHg, and the cholesterol treatment goal achievement was defined as total cholesterol <200 mg/dL.
The presence of combined conditions was defined as a participant who had multiple conditions at the same time. Treatment of combined conditions was defined as the participant receiving treatment for all their diagnosed conditions. Successful treatment of combined conditions was defined as all conditions under control.
Demographic and social-economic characteristics considered in the analyses included age, gender, race or ethnicity, body mass index (BMI), education level, income level and marital status. BMI was calculated from the measured height and weight and categorized into the following categories: <25, (25, 30) and ≥30 kg/m2. Race/ethnicity was self-reported as non-Hispanic white, non-Hispanic black, Mexican American, other Hispanic and non-Hispanic other. Education levels were classified into three categories: <high school, high school and >high school diploma. Income levels were based on the measure of income-to-poverty ratio and were classified into (0, 1.30), (1.30, 3.50) and >3.50 according to the Supplemental Nutrition Assistance Program (SNAP, formerly the Food Stamp Program) guidelines by the U.S. Department of Health and Human Service40. Married status was dichotomized into married/living with partner or other.
Statistical Analysis
In general, participant characteristics were summarized as means ± standard deviations, medians and inter-quartile ranges or frequencies and percentages as appropriate on the 2-year survey cycle. The prevalence rate of each combined conditions was estimated per survey cycle. According to the NHANES Analytic and Reporting Guidelines, the estimation of the prevalence took into account selection probabilities, complex sample design and non-response and non-coverage by using appropriate sample weights to ensure unbiased estimation41,42. Standard errors associated with the prevalence estimates were obtained using Taylor series linearization. The trends of the prevalence over time were examined by using logistic regression models, which included the median year of the survey cycle as a continuous covariate. The models further controlled the participant’s characteristics. Subgroup analysis was performed for different demographic or social-economic strata by specifying the DOMAIN statement for the SURVEY procedure in SAS. The trends for each subgroup controlled for all other characteristics. The p values for trend were calculated based on testing null hypothesis that the slope of linear regression (prevalence was outcome and cycle year was a continuous predictor) was 0.
For management and control analyses, the denominator was the number of participants with corresponding concurrent conditions. Since these groups have much smaller sample sizes, we combined all 2-year survey cycles into two larger cohorts (1999–2006 and 2007–2012) for better estimation of the parameters for management and control. Statistical significance was established with a two-sided P-value < 0.05. The analysis results were not adjusted for multiple comparisons. All analyses were conducted using SAS 9.3 (Cary, NC) and R-studio (Boston, MA).
Results
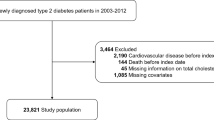
NHANES surveyed a total of 71,916 participants from 1999 to 2012, and 36,673 were included in the analysis. Figure 1 shows the number of NHANES participants and the participants who met the inclusion criteria for the 2-year survey cycle. The average sample size was 5,239 per survey cycle (range 4,597–6,150). The mean age was 50.7 years, 49.8% were male, 47.5% were non-Hispanic white and 20.8% were non-Hispanic black, 46.3% received above high-school diploma education, 59% were married or living with partners, and 30.8% were below the poverty ratio based on the SNAP criteria (Table 1). Overall, there was little change in the demographic and social-economic characteristics of the survey participants over time. Obesity (BMI ≥30 kg/m2) increased from 30.4% in 1999–2000 to 38.1% in 2007–2008, and then decreased to 32.3% in 2011–2012.
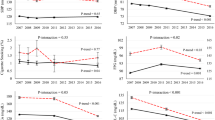
The overall prevalence of concurrent hypertension, hypercholesterolemia and diabetes increased significantly over the study period, from 3% (95% CI; 2.3%, 3.8%) in 1999–2000 to 6.3% (95% CI; 5.3%, 7.3%) in 2011–2012 (P < 0.001 for linear trend while adjusting for demographic characteristics, Table 2). The prevalence almost doubled in both gender groups. It was stable and below 1% among young adults (age <40 years), but increased 107% and 73% in the 40–60 and 60+ year groups, respectively (P < 0.01 for trends). After 2009, the prevalence reached above 14% for the 60+ year group. The increasing trend was also found in all race and education categories, except no statistical significance was established for the groups of other Hispanics and non-Hispanic others. The non-Hispanic black group exhibited a doubling in prevalence from 1999 to 2008 and stayed above 10% since then. While the prevalence did not reach a statistically significant increase in the overweight group (P = 0.64 for trend) after adjusting for other characteristics, it increased from 0.6% to 2.2% in the normal BMI group (P = 0.003 for trend) and from 5.6% to 11.9% in the obesity group (P < 0.001 for trend).
Slope analyses of the subgroups revealed, that only BMI showed a significant correlation (P < 0.001). The overall prevalence rates of the conditions of concurrent hypertension and diabetes, and concurrent hypercholesterolemia and diabetes also increased significantly during the study period (P < 0.001 for both trends). They increased, respectively, from 4.8% (95% CI; 3.7%, 5.9%) and 5.2% (95% CI; 4.1%, 6.2%) in 1999–2000 to 8.1% (95% CI; 6.9%, 9.3%) and 9.0% (95% CI; 7.7%, 10.3%) in 2011–2012 (Supplementary Tables 1 and 2). The significance increments were also detected in most subgroups. The prevalence of concurrent hypertension and diabetes doubled from 4.2% in 1999–2000 to 8.4% in 2011–2012 among male adults while female adults showed a doubling in the prevalence of current hypercholesterolemia and diabetes (4.6% to 9.2%) during the same period. Both combinations were over 15% in 2011–2012 in the obesity group. On the other hand, the overall prevalence of concurrent hypertension and hypercholesterolemia was stable over the study period, which was, however, much higher than the rates of the other two combinations. The prevalence was 19.9% (95% CI; 17.5%, 22.4%) in 1999–2000, 22.6% (95% CI; 22.5%, 24.7%) in 2003–2004 and 23.1% (95% CI; 20.4%, 25.8%) in 2011–2012. The P-value was 0.73 for testing a linear trend after adjusting for participant covariates. The prevalence was also stable and remained high in all subgroups (Supplementary Table 3).
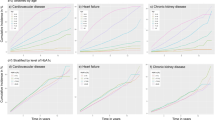
The overall medical treatment rate of concurrent hypertension, hypercholesterolemia and diabetes was 69.8% (95% CI; 64.3%, 75.3%) in 1999–2006 and increased to 82.4% (95% CI; 78.9%, 85.8%) in 2007–2012 (P = 0.002 for trend, Table 3). Treatment also improved significantly in males <60 years old, non-Hispanic white, other Hispanic, high income, highly educated, unmarried or obese participants. Treatment did not change among non-Hispanic blacks, and decreased among participants with a BMI <25 Kg/m2. Overall treatment of the combination of hypertension and diabetes improved from 73.6% in 199–2006 to 79.2% in 2007–2012 (P = 0.01 for trend, Supplementary Table 4). Treatment of the combination of hypercholesterolemia and diabetes also improved but did not reach statistical significance (P = 0.08). For these combinations of two conditions, treatment generally improved in males, non-Hispanic white and obese participants (Supplementary Table 4). No significant improvement was found for the treatment of the combination of hypertension and hypercholesterolemia (P = 0.41), which was, however, already close to 90% during the study period. The treatment also did not show a significant increase in all the subgroups except for participants with a low education level.
Simultaneous goal achievement of diabetes mellitus, hypertension, and hypercholesterolemia was significantly improved over time, from 7.3% (95% CI; 4.7%, 10%) in 1999–2006 to 14.2% (95% CI; 10.8%, 17.5%) in 2007–2012 (P = 0.03 for a trend, Table 4). Goal attainments also improved significantly in Mexican Americans, non-Hispanic blacks, low income and low education groups. For combinations of two conditions, simultaneous treatment goal achievements improved for hypercholesterolemia with diabetes or hypertension but not for hypertension and diabetes (Supplementary Table 5). The control rate of hypertension and hypercholesterolemia improved in all subgroups.
Discussion
From our study, there was a significant increase from 3% to 6.3% in the prevalence of a combination of diabetes, hypertension and hypercholesterolemia between 1999 and 2012 among the U.S. adult population. This finding suggests that more than 12 million adults were living with these three conditions simultaneously in 2012. Among these conditions, a rapid increase in the prevalence of diabetes was becoming a driving force among the major risk factors for cardiovascular disease. From our analysis, significant increment in prevalence could be seen in any concurrent situations with diabetes, while the prevalence of hypertension combined with hypercholesterolemia remained stably high, without significant increment during the last fourteen years, due to a high baseline level.
There are considerable disparities revealed by demographic and social-economic factors. Significantly increased prevalence was found in subgroups including both gender, middle and older age groups (>40 years), non-Hispanic White and non-Hispanic black, and BMI >30 kg/m2 in groups with any combination of diabetes. Specifically, in 2011–2012, 14.7% of the elderly group (60+ years) had all three conditions, compared with 6.1% in the 20–60 year old group. The elderly group clearly had poorer treatment achievements, suggesting a heavy and increasing burden on healthcare given the aging population. Better approaches for multiple conditions are urgently needed for the growing elderly population. It was found that SES (social economic status, including education and income level) was inversely correlated with the prevalence of cardiovascular risk factors. The higher the SES status the lower risk was. Nevertheless, the prevalence of risk factors in groups with any combination of diabetes increased in the past fourteen years within all SES subgroups. A better understanding of the reasons for these differences may lead to novel public health prevention programs.
With the rapid development of diabetes, the medicine treatment rate was increased significantly during the past fourteen years. Generally, the treatment rate for all comorbid situations grew from <70% to >80%. Significant increments were found in male patients, age <60 years, non-Hispanic White, and those with a higher SES and BMI. On the other hand, those with higher age (>60 years) and a lower SES had more medical cost coverages than before, though without statistical significance, suggesting more effort might be needed for those subgroups.
In sub-analysis for different combinations of the three major risk factors, a similar trend was found. The most significant increase was found in a combination of hypertension and diabetes, hypercholesterolemia and diabetes especially in males non-Hispanic White BMI >30 kg/m2, while we did not find a significant increment in medical treatment rates for hypertension and hypercholesterolemia, due to the higher cost coverage level at baseline. The general medical treatment rates in subgroups, with any combination of factors with diabetes, were around 79% in 2007–2012, although significantly higher than in 1999–2006, but still lower compared to 90.7% for the medicine treatment rate of hypertension and hypercholesterolemia in 2007–2012. These findings imply that more treatment cost coverage for diabetes should be implemented in order to better improve the current status of the rapidly growing diabetic population.
Although 82.4% of subjects with three conditions combined had medicine treatment cost coverage, only 14.2% of them had reached the target goals, meaning that the majority did not succeed in reducing their cardiovascular risks well enough. In a sub-analysis for those with any of the two conditions, the goal achievement rates were around 17–24.5%. Generally speaking, the goal attainment rates for all these cardiovascular risks were far from satisfactory. We detected a statistically significant increment in successful medication control rates in two subgroups with hypercholesterolemia. However, only 25% of subjects with hypertension and hypercholesterolemia reached their treatment goal, 20% in the hypertension and diabetes group and <20% in the hypercholesterolemia and diabetes group.
In conclusion, due to the rapid development of diabetes, the cardiovascular risks associated with this condition have increased accordingly in any combination of disease with diabetes, while no dramatic growth was found in subjects who did not have diabetes. As a result, the treatment cost coverage has lagged far behind especially in the groups with diabetes. More strikingly, treatment goal attainment rates in any groups with combination of diabetes were even lower than in those groups without diabetes.
The main strength of this study was the use of a large, continuous, national representative survey. All survey measurements and data were collected with standardized methods over time. The findings in this paper are subject to several limitations. First, we did not distinguish between undiagnosed and diagnosed conditions. Second, definitions of these conditions are continuously changing and may also be stratified. For example, hypertension could be defined as BP ≥130/80 mmHg for diabetic subjects36. The new guidelines from the Eight Joint National Committee on High Blood Pressure recommends treating hypertension for 60+ year old adults with a BP ≥150/90 mmHg43. Finally, the study data rely on self-reported information and may be subject to recall and social desirability bias.
In summary, more intensive treatment regimens are needed for patients with a combination of diabetes, hypertension and hypercholesterolemia, in order to curb the cardiovascular endpoints expected in the near future, as the majority of them did not meet their treatment targets. As an urgent priority, treatment adjustment or intensification for diabetic patients may be required as the treatment goal achievement rate of these subjects was even lower compared to those without diabetes.
Additional Information
How to cite this article: Song, Y. et al. Increasing trend of diabetes combined with hypertension or hypercholesterolemia: NHANES data analysis 1999–2012. Sci. Rep. 6, 36093; doi: 10.1038/srep36093 (2016).
Publisher’s note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
Centers for Disease, C. & Prevention. CDC Grand Rounds: the million hearts initiative. MMWR Morb Mortal Wkly Rep 61, 1017–1021 (2012).
Wilson, P. W. Diabetes mellitus and coronary heart disease. Am J Kidney Dis 32, S89–100 (1998).
Keil, U. et al. Classical risk factors and their impact on incident non-fatal and fatal myocardial infarction and all-cause mortality in southern Germany. Results from the MONICA Augsburg cohort study 1984–1992. Monitoring Trends and Determinants in Cardiovascular Diseases. Eur Heart J 19, 1197–1207 (1998).
Smith, S. C. Jr. Screening for high-risk cardiovascular disease: a challenge for the guidelines: comment on “systematic review of guidelines on cardiovascular risk assessment: which recommendations should clinicians follow for a cardiovascular health check?” Arch Intern Med 170, 40–42 (2010).
Verschuren, W. M. et al. Serum total cholesterol and long-term coronary heart disease mortality in different cultures. Twenty-five-year follow-up of the seven countries study. Jama 274, 131–136 (1995).
Sacco, R. L. et al. American Heart Association Prevention Conference. IV. Prevention and Rehabilitation of Stroke. Risk factors . Stroke 28, 1507–1517 (1997).
Wilson, P. W. et al. Prediction of coronary heart disease using risk factor categories. Circulation 97, 1837–1847 (1998).
Kearney, P. M. et al. Global burden of hypertension: analysis of worldwide data. Lancet 365, 217–223 (2005).
Seaquist, E. R. Addressing the burden of diabetes. Jama 311, 2267–2268 (2014).
Reddy, K. Global perspective on cardiovascular disease. In: Evidence-Based Cardiology. Yusuf, S., Cairns, J. A., Camm, A. J., Fallen, E. L., Gersh, B. J. (Eds). Wiley-Blackwell, London, UK (2009).
Selvin, E., Parrinello, C. M., Sacks, D. B. & Coresh, J. Trends in prevalence and control of diabetes in the United States, 1988–1994 and 1999–2010. Ann Intern Med 160, 517–525 (2014).
An, R. Prevalence and Trends of Adult Obesity in the US, 1999–2012. ISRN Obes 2014, 185132 (2014).
Wolf-Maier, K. et al. Hypertension prevalence and blood pressure levels in 6 European countries, Canada, and the United States. Jama 289, 2363–2369 (2003).
Hajjar, I. & Kotchen, T. A. Trends in prevalence, awareness, treatment, and control of hypertension in the United States, 1988–2000. Jama 290, 199–206 (2003).
Guo, F., He, D., Zhang, W. & Walton, R. G. Trends in prevalence, awareness, management, and control of hypertension among United States adults, 1999 to 2010. J Am Coll Cardiol 60, 599–606 (2012).
Carroll, M. D. et al. Trends in serum lipids and lipoproteins of adults, 1960–2002. Jama 294, 1773–1781 (2005).
Toth, P. P., Potter, D. & Ming, E. E. Prevalence of lipid abnormalities in the United States: the National Health and Nutrition Examination Survey 2003–2006. J Clin Lipidol 6, 325–330 (2012).
Ford, E. S., Li, C., Pearson, W. S., Zhao, G. & Mokdad, A. H. Trends in hypercholesterolemia, treatment and control among United States adults. Int J Cardiol 140, 226–235 (2010).
Jamerson, K. et al. Benazepril plus amlodipine or hydrochlorothiazide for hypertension in high-risk patients. N Engl J Med 359, 2417–2428 (2008).
Brenner, B. M. et al. Effects of losartan on renal and cardiovascular outcomes in patients with type 2 diabetes and nephropathy. N Engl J Med 345, 861–869 (2001).
Ward, B. W. & Schiller, J. S. Prevalence of multiple chronic conditions among US adults: estimates from the National Health Interview Survey, 2010. Prev Chronic Dis 10, E65 (2013).
Kannel, W. B. Risk stratification in hypertension: new insights from the Framingham Study. Am J Hypertens 13, 3s–10s (2000).
Wilson, P. W., Kannel, W. B., Silbershatz, H. & D’Agostino, R. B. Clustering of metabolic factors and coronary heart disease. Arch Intern Med 159, 1104–1109 (1999).
Onat, A. et al. Dyslipidemic hypertension: distinctive features and cardiovascular risk in a prospective population-based study. Am J Hypertens 18, 409–416 (2005).
Grundy, S. M., Pasternak, R., Greenland, P., Smith S. Jr. & Fuster, V. Assessment of cardiovascular risk by use of multiple-risk-factor assessment equations: a statement for healthcare professionals from the American Heart Association and the American College of Cardiology. Circulation 100, 1481–1492 (1999).
Neaton, J. D. & Wentworth, D. Serum cholesterol, blood pressure, cigarette smoking, and death from coronary heart disease. Overall findings and differences by age for 316,099 white men. Multiple Risk Factor Intervention Trial Research Group. Arch Intern Med 152, 56–64 (1992).
Ji, L. et al. Primacy of the 3B approach to control risk factors for cardiovascular disease in type 2 diabetes patients. Am J Med 126, 925.e911–922 (2013).
Gaede, P., Lund-Andersen, H., Parving, H. H. & Pedersen, O. Effect of a multifactorial intervention on mortality in type 2 diabetes. N Engl J Med 358, 580–591 (2008).
Cost effectiveness analysis of improved blood pressure control in hypertensive patients with type 2 diabetes: UKPDS 40. UK Prospective Diabetes Study Group. Bmj 317, 720–726 (1998).
Grant, R. W. & Kirkman, M. S. Trends in the evidence level for the American Diabetes Association’s “Standards of Medical Care in Diabetes” from 2005 to 2014. Diabetes Care 38, 6–8 (2015).
Standards of medical care in diabetes–2015: summary of revisions. Diabetes Care 38 Suppl, S4 (2015).
Stone, N. J. et al. 2013 ACC/AHA guideline on the treatment of blood cholesterol to reduce atherosclerotic cardiovascular risk in adults: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol 63, 2889–2934 (2014).
Ganda, O. P. Deciphering cholesterol treatment guidelines: a clinician’s perspective. Jama 313, 1009–1010 (2015).
Estoppey, D., Paccaud, F., Vollenweider, P. & Marques-Vidal, P. Trends in self-reported prevalence and management of hypertension, hypercholesterolemia and diabetes in Swiss adults, 1997–2007. BMC Public Health 11, 114 (2011).
MacDonald, T. M. & Morant, S. V. Prevalence and treatment of isolated and concurrent hypertension and hypercholesterolaemia in the United Kingdom. Br J Clin Pharmacol 65, 775–786 (2008).
Wong, N. D., Lopez, V., Tang, S. & Williams, G. R. Prevalence, treatment, and control of combined hypertension and hypercholesterolemia in the United States. Am J Cardiol 98, 204–208 (2006).
Centers for Disease Control and Prevention. National Center for Health Statistics (NCHS). National Health and Nutrition Examination Survey Data. Hyattsville, MD: U.S. Department of Health and Human Services, Centers for Disease Control and Prevention, 1999–2010. Available at http://www.cdc.gov/nchs/nhanes/nhanesquestionnaires.htm (2012).
Survey Questionnaires, Examination Components and Laboratory Components 2009–2010. http://www.cdc.gov/nchs/nhanes/nhanes2009–2010/questexam09_10.htm.
Centers for Disease Control and Prevention. National Center for Health Statistics. National Health and Nutrition Examination Survey Response Rates and CPS Totals, 2009–2010. A available at http://www.cdc.gov/nchs/nhanes/response_rates_CPS.htm (2012).
Johnson, C. L. et al. National health and nutrition examination survey: analytic guidelines, 1999–2010. Vital Health Stat 2, 1–24 (2013).
National Center for Health Statistics. National Health and Nutrition Examination Survey: Analytic Guidelines, 1999–2010. Available at www.cdc.gov/nchs/data/series/sr_02/sr02_161.pdf (2013).
Analytic Note Regarding 2007–2010 Survey Design Changes and Combining Data Across Other Survey Cycles. Available at: http://www.cdc.gov/nchs/data/nhanes/analyticnote_2007–2010.pdf.
James, P. A. et al. 2014 evidence-based guideline for the management of high blood pressure in adults: report from the panel members appointed to the Eighth Joint National Committee (JNC 8). Jama 311, 507–520 (2014).
Acknowledgements
This study was sponsored by MSD China Holding Co., Ltd., China. We would like to thank Chen Yang, Gao Peng, Robert Lubwama, Ahmed Shirin, Karen Kurtyka and Huang Xingyue from Merck & Co., Inc., Whitehouse Station, NJ, USA, for scientific and editing support during the research project.
Author information
Authors and Affiliations
Contributions
Y.S., X.L., X.Z., B.Z., B.H. and J.Z. were responsible for the conception and design of the study. Y.S., X.L., X.Z., B.Z., B.H., X.S., L.C., M.Y., T.Y. and J.Z. were responsible for acquisition of data. Y.S., X.L., X.Z., B.Z., B.H., X.S., L.C., M.Y., T.Y. and J.Z. performed the data analysis. Y.S., X.L. and J.Z. drafted the manuscript. All authors participated in interpretation of the findings. J.Z. revised and commented on the draft, and all authors read and approved the final version of the manuscript.
Ethics declarations
Competing interests
The authors declare no competing financial interests.
Electronic supplementary material
Rights and permissions
This work is licensed under a Creative Commons Attribution 4.0 International License. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in the credit line; if the material is not included under the Creative Commons license, users will need to obtain permission from the license holder to reproduce the material. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/
About this article
Cite this article
Song, Y., Liu, X., Zhu, X. et al. Increasing trend of diabetes combined with hypertension or hypercholesterolemia: NHANES data analysis 1999–2012. Sci Rep 6, 36093 (2016). https://doi.org/10.1038/srep36093
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/srep36093
This article is cited by
-
The clinical impact of anti-hypertensive treatment drug-gene pairs in the asian population: a systematic review of publications in the past decade
Journal of Human Hypertension (2022)
-
High prevalence of cardiovascular risk factors in adults living in Greece: the EMENO National Health Examination Survey
BMC Public Health (2020)
-
Epidemiology of Diabetes Mellitus and Cardiovascular Disease
Current Cardiology Reports (2019)
-
Predictors of poor blood pressure control among Iranian hypertensive patients
BMC Research Notes (2017)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.