Abstract
Retinitis pigmentosa (RP), the most frequent form of inherited retinal dystrophy is characterized by progressive photoreceptor degeneration. Many genes have been implicated in RP development, but several others remain to be identified. Using a combination of homozygosity mapping, whole-exome and targeted next-generation sequencing, we found a novel homozygous nonsense mutation in SAMD11 in five individuals diagnosed with adult-onset RP from two unrelated consanguineous Spanish families. SAMD11 is ortholog to the mouse major retinal SAM domain (mr-s) protein that is implicated in CRX-mediated transcriptional regulation in the retina. Accordingly, protein-protein network analysis revealed a significant interaction of SAMD11 with CRX. Immunoblotting analysis confirmed strong expression of SAMD11 in human retina. Immunolocalization studies revealed SAMD11 was detected in the three nuclear layers of the human retina and interestingly differential expression between cone and rod photoreceptors was observed. Our study strongly implicates SAMD11 as novel cause of RP playing an important role in the pathogenesis of human degeneration of photoreceptors.
Similar content being viewed by others
Introduction
Retinitis Pigmentosa (RP, [MIM #268000]) is the most frequent cause of inherited retinal dystrophy (IRD), with an estimated global incidence of 1:4000 individuals1. This condition is characterized by progressive loss of photoreceptor function and viability, ultimately leading to blindness. Subjects diagnosed with RP initially complain of night blindness and progressive peripheral constriction of their visual field due to primary rod photoreceptor dysfunction. Central vision loss is also frequently presented as a secondary outcome in advanced disease course due to cone photoreceptor involvement. Large phenotypic variations have been reported between individuals, with a variable onset of the disease from childhood to adulthood2.
RP is inherited in most cases as a Mendelian trait: autosomal recessive in 30% of patients, autosomal dominant in 20% and X-linked in 10%. Approximately 40% of RP patients represent isolated cases3,4. A remarkable characteristic of RP is their enormous allelic and genetic heterogeneity. To date, more than 3,000 mutations in at least 60 genes have been reported to cause non-syndromic autosomal recessive RP (arRP)5, most of which are mutated only in a small fraction of patients. Combining Sanger sequencing and targeted-capture next-generation sequencing (NGS), it is possible to identify underlying causative mutations in 40–70% of arRP cases6,7,8 which implies that additional genes have yet to be identified. To shed light on novel autosomal recessive RP genes, we focused on whole-exome sequencing (WES) in Spanish families with evidence of parental inbreeding who did not carry any mutation in known IRD genes after whole genome homozygosity mapping. Using this strategy, we identified recently two novel genes, ABHD12 and ZNF408, associated with non-syndromic arRP in our cohort of patients9,10.
Herein, we reported a homozygous nonsense mutation in SAMD11 in five patients diagnosed with RP, providing first link between this gene and a retinal disorder. Human SAMD11 is the human ortholog of the mouse major-retinal SAM domain (mr-s) gene, which is predominantly expressed in developing retinal photoreceptors11. Here, we determined for the first time the neural localization pattern of SAMD11 in the adult human retina. Thus, we observed a strong expression of SAMD11 in photoreceptor cells. Our findings allowed the identification of a new candidate gene underlying RP and provide insight into the SAMD11 dysfunction in human retinal degeneration.
Results
Whole-genome homozygosity mapping
Three affected siblings (II:5, II:6 and II:7) of a consanguineous Spanish family (Family RP-1105, Fig. 1b) were diagnosed with autosomal recessive adult-onset RP. To identify the genetic cause underlying the arRP within the family, first we performed whole genome homozygosity mapping using high resolution SNP-array in each of the three affected siblings (II:5, II:6 and II:7) using Illumina HumanCytoSNP-12 SNP microarrays. Three regions of homozygosity >1 Mb were shared by all affected individuals, containing a total of 302 genes (Supplementary Table S1): a 20.4 Mb interval on chromosome 3 and two intervals of 11.8 and 1.3 Mb on chromosome 1. CLRN1 was the only IRD-associated gene12,13 to be present within the candidate identity-by-descent (IBD) regions; however causal mutations were discarded by Sanger sequencing.
Identification of the homozygous nonsense mutation p.Arg630* associated to autosomal recessive Retinitis Pigmentosa by combining homozygosity mapping and whole-exome sequencing.
(a) Mapped reads from the whole-exome sequencing (WES) analysis in patient II:7 from Family RP-1105 revealed a homozygous change C>T at position 879375 on chromosome 1, leading to a stop gain p.Arg630* in the SAMD11 gene. Wild-type sequence and coverage per base are shown. (b) Pedigree of the two families carrying the p.Arg630* mutation in SAMD11, along with the correctly segregation of the mutant allele with a recessive inheritance. Individuals surrounded by a circle were analysed by homozygosity mapping using genome-wide SNP arrays. The red circle indicates the individual in which WES has been performed. The SAMD11 genotype of each available family member is represented below the individual symbol being “+” normal allele and “M”, mutated alleles. Electropherograms of homozygous affected, heterozygous carrier and a healthy control subject for the c.1888C>T variant were also shown. (c) Intron-exon structure of SAMD11 and position of novel likely pathogenic variants identified in this study. Exons are indicated by coloured rectangles that are wider for the coding regions. Exons in red encode the evolutionary conserved SAM domain of the SAMD11 protein. Nucleotide numbering reflects cDNA in the reference sequence NM_152486.2. (d) Expression of SAMD11 by RT-PCR analysis in total RNA from 22 different human tissues. Amplification of GAPDH mRNA was used as positive control.
Exome-sequencing detects a novel homozygous nonsense mutation in SAMD11
To analyse the above IBD candidate regions in this family, we performed whole-exome sequencing in the index case. A total of 69,657,399 reads were uniquely mapped to the exonic regions with a median of coverage of 86.25X. A total of 7,240 single nucleotide variations (SNVs) and 285 small insertions and deletions (INDELs) were identified by GATK program (Supplementary Table S2). Among them, 296 novel or rare variants were selected by excluding referenced polymorphisms with a minor allele frequency (MAF) >0.5% at dbSNP, 1000 genomes14 and Exome Variant Server (EVS)15 databases. No pathogenic variants were found in the more than 200 genes previously implicated in IRD. Under the assumption of recessive inheritance and consanguineous ancestry, homozygous variants within the previously candidate IBD regions were prioritized, remaining only two novel variants, both located at the third shared region on the short arm of chromosome 1 (1p36.33): i) a nonsense variant (NM_152486.2:c.1888C>T;p.Arg630*) in SAMD11 (Sterile alpha motif domain-containing 11) and ii) a missense change (NM_032129.2: c.995G>A; p.Gly332Glu) in PLEKHN1 (Pleckstrin homology domain containing, family N member 1) (Supplementary Tables S2 and S3). Both variants were validated by Sanger sequencing, segregating homozygously with the disease in the family (Fig. 1b) and were excluded from 196 ethnically matched-control individuals. In addition, they have not been described either in the Exome Agregation Consortium (ExAC) database or in an in-house 400 Spanish exomes database (CIBERER Spanish Variant Server).
The nonsense variant p.Arg630* at SAMD11 appeared to be the top candidate based on potential deleterious effect predicted by several in silico prediction tools, and biological and clinical relevance according to gene function, expression and in silico protein interaction network analysis with other known IRD genes16,17 (Supplementary TableS3). This gene is predominantly expressed in photoreceptor cells11. This mutation introduces a premature termination codon (PTC) at the last exon of SAMD11, truncating the last C-terminal 50 residues. In silico protein-protein interaction analysis revealed a network with a clustering coefficient significantly higher than expected by chance (p-value = 0.0022) that interestingly depicts relationships of SAMD11 to several retinal dystrophy-associated genes such as the photoreceptor-specific transcription factor Cone-Rod homeobox (CRX) (Supplementary Figure S1). By contrast, the second novel variant found in this family was a novel missense p.Gly332Glu in PLEKHN1, a gene with unknown function. This variant was predicted to be likely deleterious by several in silico tools (Supplementary Table S3), however a clear correlation of this gene with IRD could not be inferred.
Mutational screening in additional IRD cohorts
To further evaluate if these variants might be also present in other RP patients, both variants were also screened in 380 unrelated Spanish index cases suffering from autosomal recessive or sporadic RP (SRP). Remarkably, the p.Arg630* variant was also found homozygously in a second consanguineous pedigree (RP-0476, Fig. 1B) with two siblings suffering with adult-onset RP, and correctly segregated according to a recessive inheritance pattern in the family. The p.Arg630* mutation in SAMD11 seems not to be ancestrally inherited in both unrelated families as demonstrated by haplotype analysis (Supplementary Figure S2). In view of these evidences, the identification of a nonsense mutation in 5 affected subjects from two unrelated families reinforces a very likely pathogenic role of SAMD11 in the RP development.
To determine whether mutations in SAMD11 could be a common cause of IRD, this gene was exhaustively screened in additional 400 Spanish IRD patients using Sanger sequencing or customized targeted NGS approach18,19. In addition, genome-wide homozygous regions from 300 unrelated individuals with several autosomal recessive IRDs were also assessed through the European Retinal Disease Consortium (ERDC)20. Two families presented large IBD regions encompassing the SAMD11 locus and were also screened for mutations by Sanger sequencing.
During those screenings, we have additionally identified three novel likely pathogenic variants in SAMD11 (Supplementary Table S4), all carried in heterozygosis (Fig. 1b), including one nonsense mutation (c.502C>T; p.Arg168*), one splice site variant at intron 13 (c.1801–2A>C) and one missense (c.133A>G; p.Lys45Glu) variant. These novel variants were not present in any SNV database neither in 196 Spanish control individuals nor in our 400 in-house whole-exome dataset. The variant p.Lys45Glu affected a highly evolutionary conserved amino-acid and was predicted as a very likely pathogenic variant by several in silico predictor tools (Supplementary Table S5). Large rearrangements, small exon deletions or large copy number variations (CNVs) affecting the SAMD11 gene, were discarded in patients carrying a heterozygous likely pathogenic variant using a custom-designed high-resolution comparative genomic hybridization (CGH) array (Supplementary Figure S3).
Ophthalmic examination
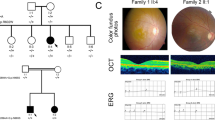
The clinical course and visual outcome of the 5 patients carrying the p.Arg630* mutation in SAMD11 were reviewed, as detailed in Table 1. Consistently, patients were diagnosed of RP between the third and fourth decade of life, presenting night blindness as first symptom and followed by progressive constriction of visual field. Overall, patients have a central visual field restricted between <10° and absolute scotoma. Loss of visual acuity was also observed in late stages of the disease, being the best-corrected visual acuity (BCVA) between 20/32 and hand movement, except for the youngest patient (II:8, Family RP-0476) who still maintained a well conserved BCVA at 55 years old (Table 1). When available, ERG registers were non-recordable in both scotopic and photophic conditions. Funduscopies showed typical RP changes as pale papilla, narrowed retinal vessels, abundant pigmentary changes in mid periphery and retinal pigment epithelium (RPE) atrophy in mid-periphery and in fovea (Fig. 2). Interestingly, similar findings on central retina were observed in two patients from different families, consisting in large plaques of atrophy, as revealed by optical coherence tomography (OCT) and fundus autofluorescence images (individual II:7, Family RP-1105: Fig. 2a,c and e; individual II:8, Family RP-0476: Fig. 2g–l). Macular OCTs also confirmed a generalized degeneration of rods, being compatible with diagnosis of RP, while cones were preserved only in fovea (Fig. 2). Bilateral posterior subcapsular cataracts were also present at both eyes in all patients.
Retinal imaging of patients carrying the p.Arg630* mutation in SAMD11.
Data from the index case (II:7) from family RP-1105 and the two affected siblings (II:4 and II:8) from family RP-0476 were included. (a–d) Fundus imaging of the right and left eye of individual II:7 at 66 years of age. (a,b) Fundus color photographs, showing pigmentary changes, retinal pigment epithelium (RPE) atrophy in the mid-periphery of both eyes and also atrophic changes in the macula (white arrowheads). (c,d) Fundus autofluorescence (FAF) showed a marked hypofluorescence area below the fovea manifesting the existence of a significant atrophic plaque in right eye (OD, black arrowhead), while it is not observed in the left eye (OS). (e,f) Macular optical coherence tomography (OCT), confirming the RPE loss in fovea and destructuring of outer layers in OD, and conservation of RPE and outer segment in fovea in OS. On the right image, black arrowheads indicate the localization of the atrophic plaques in parafoveal region. Red and yellow arrowheads indicate start and end position, respectively for atrophic RPE loss in OD. (g–j) Fundus imaging of the right and left eye of the index case II:4 from family RP-0476 at 74 years-old. (g-h) Fundus color photographs showing RPE alteration in paravascular areas and mid-periphery, round and bone-spicule pigmentation in mid-periphery, attenuated retinal vessels and central atrophic plaques (white arrowheads). (i,j) FAF, confirming also the presence of hypofluorescence regions at fovea in both eyes (black arrowheads). (k,l) OCT scan, showing loss of RPE in fovea and perifoveal region, epiretinal membrane and atrophic plaques in central macula. The right pictures of central macula evidence a large plaque of atrophy in OD fovea and four smaller parafoveal plaques in OS (black arrowheads). Red and yellow arrowheads indicate start and end position, respectively for atrophic RPE loss in fovea (OD). (m–p) Fundus imaging of the right and left eye of the individual II:8 from family RP-0476 at 55 years-old. (m,n) Fundus imaging, revealing macular RPE alteration, round and bone-spicule pigmentation in mid-periphery.(o-p) FAF, showing perifoveal hypoautofluorescence ring (q,r). OCT of both eyes, revealing conservation of inner and outer segments in fovea, epiretinal membrane and atrophy of external layers in parafoveal area. Blue arrowheads indicate the localization of preserved RPE in central fovea.
SAMD11 transcripts are widely expressed in human retina and extra-ocular tissues
The human SAMD11 reference transcript harbours 14 exons and encodes a 681 aa protein (Fig. 1c) that belongs to the SAM protein superfamily, characterized by the presence of the evolutionarily conserved sterile alpha motif (SAM) domain. A recent cloning of the human SAMD11 allowed the identification of up to 45 alternative splice variants21. Several alternative N-termini were described; however, all the isoforms that expect to be translated into proteins share the same C-terminal part. We investigated the expression profile in different human tissues by RT-PCR experiments using specific primers for the well-conserved 3′ region of SAMD11. We found expression of SAMD11 in all the 22 of the tissues tested except in whole blood (Fig. 1d). In concordance, SAMD11 could not be detected in lymphoblastoid cell lines derived from several control individuals and a homozygous carrier of the p.Arg630* mutation (Supplementary Figure S4). Thus, SAMD11 is widely expressed, showing the highest expression in kidney, prostate and human retina.
Immunolocalization of SAMD11 in human retina
To shed light on the implication of SAMD11 in retinal physiology, we investigated its expression and localization pattern in the distinct retinal cell types on adult healthy human retina by means of Western blotting and confocal immunofluorescence microscopy (Fig. 3). Immunoblotting analysis revealed the presence in the mentioned tissue of a prominent and specific immunoreactive band with apparent molecular weight of 68 kDa corresponding to the SAMD11 protein (Fig. 3n).
Immunolocalization of SAMD11 in vertical sections of human retina.
(a) SAMD11 is located in rod photoreceptor cell bodies in the ONL and in the inner and outer segments of cones and rods. A subset of amacrine cells (double arrowheads in a, c, d) also exhibits expression of SAMD11 protein. Besides, ganglion cells evidenced SAMD11 immunolabeling in their cell bodies and axons, which constitute the nerve fiber layer. (b) Pre-absorption control for SAMD11 antibodies specificity using the immunogenic peptide. (c,e,f) Double immunostaining with antibodies against SAMD11 and cone arrestin, a specific marker for cone photoreceptors, showed immunoreactivity of SAMD11 in the inner and outer segments of cones andextracellular matrix (arrows). (d,g,h) SAMD11 and rhodopsin, a specific marker that labels rod outer segments, double immunolabeling showed the localization of SAMD11 in rod inner and outer segments (arrowheads). (I,j) Long/medium wavelength opsin antibodies and peanut agglutinin lectin staining evidenced the presence of SAMD11 in outer and inner segments of cones, as well as in their extracellular matrix. (k–m) Detail of the immunolocalization of SAMD11 in cone outer segments and extracellular matrix. (n) Immunoblotting analysis of SAMD11 protein. Human retina samples expressed strongly immunoreactive bands detected with SAMD11 or GAPDH antibodies. The arrowheads point to the 68 and 36 kDa protein bands corresponding to SAMD11 and GAPDH, respectively. Protein molecular weight markers are given to the left. SAMD11 immunolabeling (peptide−) was specifically abolished when the SAMD11 antibody was preincubated with its immunogen peptide (peptide+). (a–h) represent a confocal stack projection of 5 pictures and (i–m) are single confocal images. Sky-blue color observed in (i,l) is the result of the co-localization in the outer segments of red/green cones of the immunoreactivity for long/medium wavelength opsins (dark-blue color) and SAMD11 (green color). OS, outer segments; IS, inner segments; ONL, outer nuclear layer; OPL, outer plexiform layer; INL, inner nuclear layer; IPL, inner plexiform layer; GCL, ganglion cell layer; NFL, nerve fiber layer. Scale bar a-i = 20 μm;k–m = 10 μm.
On the other hand, we characterized the SAMD11 distribution pattern in cryo-fixed vertical sections of human retina, which were immunolabeled with specific SAMD11 antibodies. As a result, SAMD11 protein was found in the three nuclear layers of the retina: outer and inner nuclear layers (ONL and INL, respectively), and ganglion cell layer (GCL) (Fig. 3a,c–d). Specifically, SAMD11 immunoreactivity was observed in a small population of amacrine cells located in the INL (Fig. 3a,c,d; double arrowheads), as well as in most of ganglion cells and their axons in the nerve fiber layer (NFL). SAMD11 was also detected in photoreceptors cells and interestingly we observed differential expression of this protein between cone and rods. In this regard, SAMD11 immunoreactivity was not detected in cone cell bodies (Fig. 3c,e,f; arrowheads) whereas rod cell bodies evidenced a prominent SAMD11 expression (Fig. 3a,c,d,f,h–j). Double immunolabelling of SAMD11 with cone arrestin, a specific marker for cone photoreceptors, revealed that SAMD11 protein was present in the inner and outer segments of cones (Fig. 3c,e,f), including the extracellular matrix (Fig. 3c,e,f; arrows). We double-checked the presence of SAMD11 in the outer segments of cones combining the SAMD11 antibody with long/medium wavelength opsin antibodies, which are specific markers for the outer segments of red/green cones (Fig. 3i–l). Double labelling with antibodies anti-SAMD11 and the peanut agglutinin lectin showed the localization of SAMD11 in the extracellular matrix of cones (Fig. 3i–m; arrowheads). Similarly to cones, SAMD11 immunoreactivity was observed in rod inner and outer segments (Fig. 3e,f), as verified the co-localization of this protein with rhodopsin, a specific marker that labels rod outer segments (Fig. 3d,g,h; arrowheads). Furthermore, Fig. 3i–k showed clearly the presence of SAMD11 in the outer (Fig. 3j,k; arrows) and inner segments (ellipsoid) of cones (double arrowheads), as well as in the extracellular matrix of cones (Fig. 3i–m; arrowheads). No immunoreactivity was found against SAMD11 in retina using the preabsortion of the antibody with their specific peptide (Fig. 3b).
Discussion
In the present study, we report a novel homozygous nonsense mutation in SAMD11, which was identified using homozygosity mapping followed by exome sequencing. Our findings provide evidence for the first association of this gene with an inherited retinal dystrophy. Five patients with late-onset Retinitis Pigmentosa from two unrelated families carried this mutation homozygously. In addition, after SAMD11 screening in our cohort, another three novel very likely pathogenic variants were also identified in heterozygous state. In these heterozygous patients, a second allele in coding region or large CNVs were discarded, however, we cannot exclude the presence of a second pathogenic variant in regulatory or deep intronic regions.
SAMD11 is a highly conserved protein from zebrafish to human, and has an isolated SAM domain in their C-terminus, without another known motif (Fig. 1c). SAMD11 was first described as a predominantly expressed protein in the terminal stage of photoreceptor differentiation11. In developing mouse retina, Samd11 expression begins at E18 with a peak level at P611, when rod outer segments formation occurs22. In adult humans, SAMD11 mRNA and protein expression have been determined in different ocular tissues, including the retina21,23. Consistent with these previous studies, our gene expression analysis showed that SAMD11 is a widely expressed gene, being present in both ocular and extra-ocular tissues. Additionally, among them, we detected higher values of SAMD11 expression in the retina. Moreover, in the present study, we identified for the first time the neural localization pattern of SAMD11 in the human retina by immunohistochemistry. As a consequence, SAMD11 was mainly localized in ONL, where the rod photoreceptor cell bodies are located, as well as in a small population of amacrine cells located in INL and in most of ganglion cells and their axons in NFL. The prominent SAMD11 immunoreactivity observed in rod cell bodies is indicative of a relevant SAMD11 role for the correct function of rod photoreceptors in the adult human retina. Hence, dysfunction of this protein could be critically involved in the primary rod loss underlying the RP pathogenesis.
The specific localization in human retina and its specific temporal prenatal and postnatal expression pattern in mouse correlating with developing and maturing of rod11,22 suggest a potential role of SAMD11 in photoreceptor differentiation and survival. Early fate and terminal differentiation of rods are mainly controlled by a hierarchical regulatory network including several transcription factors (TF), such CRX, the orthodenticle homeobox 2 (OTX2), neural retinal leucine (NRL) and the orphan nuclear receptor NR2E324,25,26,27,28. Interestingly, all of them have been involved in the rod dysfunction underlying retinal dystrophies29,30,31. As occurs in most of human genes associated with retinal dystrophies32, the retinal expression of SAMD11 seems to be directly regulated by CRX and OTX2 through several highly conserved binding sequences in the promoter region, as supported by different in vitro and in vivo studies11,21,33. Recently, several RP-associated genes, such as FAM161 and MAK, have been identified as candidate genes using the mouse retinal CRX targetome obtained by ChIP-seq34,35. Thus, prioritization of CRX target genes have revealed as a very effective strategy to pinpoint novel candidate retina-specific genes. Remarkably, in this experiment, the principal CRX-target is SAMD7, the closest phylogenetic relative of SAMD11 (Supplementary Figure S5) with a very similar expression profile in the human and mouse retina32,36. Although SAMD11 was apparently not included as a potential CRX-target in the above ChIP-seq dataset, we noticed that the mouse genome assembly (mm9) used at that time did not include yet the Samd11 gene. After converting genome coordinates to the most actualized assembly (mm10), we found that between the 100 most enriched CRX-bound regions (CBRs) identified by Corbo and collaborators, there was one CBR located to the promoter of mouse Samd11 (Supplementary Figure S6)32. This CRB seems to be actively transcribed by RNA Polymerase II complexes at mouse developing neural retina37, suggesting that these regulatory regions can act as initiation and elongation sites of SAMD11 transcription.
SAM domains are involved in protein-protein interactions during signal transduction and transcriptional regulation38,39. SAM domains, that are arranged in a small 4–5-helix bundle of two orthogonally packed α-hairpins40 (Supplementary Figure S5), can homo- and hetero-oligomerise, forming multiple self-association architectures41. In this sense, it was described the mouse Samd11 protein is able to self-associated mainly through the SAM domain11. SAM proteins have been implicated both in normal and pathological processes of eye development. In Drosophila eyes, Yan, Mae and Pointed-P2 are SAM domain-containing proteins acting as transcriptional factors of the Ras-MAPK pathway39,42,43. In these proteins, SAM domain plays an important role in the transcriptional activity via heterotypic interactions, as suggested by in vitro studies44,45. It is unknown whether comparable SAM-mediated interactions could influence photoreceptor development in Mammals. A SAM domain is also found in the SANS/USH1G protein, a scaffolding protein involved in the pathogenesis of the Usher syndrome type 146.
Experimental evidences suggested that SAMD11, similarly to SAMD7, is implicated into the CRX-mediated transcription acting as transcriptional repressor11,36. Its interaction with yet-unknown proteins could promote rod fate and/or maintenance. It is noteworthy that this transcriptional regulation seems to be exerted without the presence of an obvious DNA binding domain. In addition, repressor activity of SAMD11 is not due to SAM interactions but it resides at the conserved C-terminal region11. Remarkably, it is the C-terminus domain, but not the SAM domain, which is lost in the homozygous RP patients carrying the truncating mutation p.Arg630*, evidencing a likely important role of this domain. In an effort to provide more experimental evidence of the involvement of the mutation identified in this work, LCLs derived from a homozygous carrier were obtained and additional experiments of SAMD11 expression were performed, comparing with control individuals. Unfortunately, we could not detected neither RNA nor protein expression in LCLs (Supplementary Figure S4). Thus, the specific functional role of SAMD11 remains unclear and warrants further research.
Identification of SAMD11 as causative gene in two RP families highlights a putatively important role for other SAM-related proteins, such SAMD7, in the pathogenesis of the retinal dystrophies. SAMD11 and SAMD7 share common features including their site and timeline of expression in the mouse retina, their nuclear localization, the presence of a very similar C-terminal SAM motif, lack of additional functional domains, their regulation by CRX and a very likely function as transcriptional repressors. In view of their high expression levels in the retina, and the weak expression of other SAM family members with isolated SAM domain36, it has been suggested a likely interaction of both proteins in the retina. Therefore, it could be very interesting to determine if they can act synergistically or if they have overlapping functions in the retina. Supporting this last supposition, the patients carrying the deleterious nonsense mutation in SAMD11 developed a late rod affectation with first symptoms of night blindness and field constriction in the third to fourth decade of life. By contrast, mutations in CRX and other CRX-regulated genes, such RS1, FAM161 and MAK, are responsible of congenital and early-onset forms of retinal dystrophy29,34,35,47,48.
Recently, a very rare missense variant in SAMD11 has been putatively associated with autism spectrum disorders (ASDs)49, suggesting that SAMD11 could be a good candidate for autism. However, none of patients carrying the novel mutations and variants in SAMD11 here reported suffer from autistic behaviour, related-neurodevelopmental disorders or intellectual disability. By contrast, we report a very homogeneous phenotype in both families consisting in Retinitis Pigmentosa with atrophic macular RPE degeneration in late stages of the disease. Significant and distinctive plaques of atrophy were clearly observed in late stages of disease in FAF and OCT.
In brief, we have identified a nonsense mutation in a novel gene as cause of adult-onset RP in five patients. The identification of a SAMD11 truncating mutation affecting the C-terminus of the protein highlights the putative importance of this domain both in the repressive function of this gene and in RP pathogenesis. Our findings strongly suggest the involvement of this protein in the development of the rod degeneration in human and in photoreceptor maintenance. This work contributes to shed further light on the molecular mechanisms underlying the pathogenesis of the retinal dystrophies. Further research on SAMD11 is expected to provide insights into its specific role in the retina and its pathogenic mechanism responsible for Retinitis Pigmentosa.
Materials and Methods
Subject recruitment and clinical evaluation
A total of 560 unrelated Spanish families with different IRDs are included in this study: 486 families with arRP and 74 families with Leber congenital amaurosis (LCA). In addition, 196 Spanish healthy unrelated individuals were used as a control samples. They were randomly selected from blood donors who voluntarily participate in this study after filling out a questionnaire specifically designed to inquire about ophthalmic diseases. They did not report any personal or familial history of retinal dystrophy. All patients and control individuals were collected at Fundación Jiménez Díaz University Hospital (FJD, Madrid, Spain). Written informed consent was obtained from all subjects or their legal guardians prior to their participation in this study, also covering the publication of the clinical data. All procedures were approved by the FJD Ethics Committee and adhered to the tenets of the Declaration of Helsinki.
Diagnosis and follow-up of patients were based on ophthalmic evaluation including measurements of BCVA and visual field tests, fundus and OCT examination and ERG responses. Diagnostic criteria of LCA included severely impaired bilateral visual function at birth or before one year-old, congenital nystagmus, weak pupillary responses and non-detectable or severely reduced ERG. Diagnostic criteria of RP included poor night vision and/or peripheral visual, with poor visual acuity and visual field loss in advanced stages of the pathology.
Genomic DNA was obtained from peripheral blood samples using an automated DNA extractor (BioRobot EZ1 Qiagen, Hilden, Germany) following the manufacturer instructions. Known mutations in LCA or ARRP genes were previously excluded in index cases using a genotyping microarray based on Arrayed Primer Extension (APEX) technology (LCA or ARRP chip, AsperOphthalmics, Tartu, Estonia). In addition, for families RP-1105 and RP-0476, direct Sanger sequencing of the coding exons and flanking intronic sequences of the EYS gene50 and ABHD12 and ZNF408, two new genes recently associated to arRP by our group9,10, was performed and no pathogenic variants were found.
Lymphoblastoid cell lines (LCLs) were established by Epstein Barr virus (EBV)-transformation of peripheral blood lymphocytes from one patient (II:7, family RP-1105) and three control individuals. Generation of EBV-derived LCLs was performed by the CIBERER Biobank (Valencia, Spain). Cell lines were cultured in RPMI-1640 media (GIBCO/BRL, Grand Island, NY, USA) supplemented with 10% fetal bovine serum (Gibco), 1% (v/v) antibiotics/antimycotics that included penicillin-streptomycin (Gibco) and 2 μg/ml Fungizone (Gibco). The cultures were carried out in 25 cm2 flasks at 37 °C in 5% CO2 atmosphere.
Homozygosity mapping
Whole-genome homozygosity mapping was performed using high-resolution commercial SNP arrays from Illumina (HumanCytoSNP-12 SNP microarrays, Illumina, San Diego, CA, USA). Arrays were processed according to the manufacturer′s protocols. IBD regions were calculated as previously reported51,52. Regions of homozygosity were interrogated for the presence of retinal disease-associated and candidate genes were screened by Sanger sequencing.
Whole-exome sequencing
Whole-exome sequencing analysis was performed by the Spanish Centre for Genome Analysis (CNAG, Barcelona, Spain). Genomic DNA was enriched for exonic sequences of approximately 30,000 genes using the Agilent SureSelect Human All Exon version 4 kit (Agilent Technologies, Santa Clara, CA, USA), following manufacturer’s standard protocol. Captured DNA library was sequenced on a HiSeq 2000 sequencing platform (Illumina) to generate pair-end reads up to 100 cycles.
Base calling and quality control were performed using the Illumina RTA sequence analysis pipeline. Analysis of the primary data (FASTQ files) was done using the BIER´s platform pipeline (BiERapp: http://bierapp.babelomics.org/)10. Sequence reads were aligned to the human reference genome build GRCh37 (hg19) using the Burrows-Wheeler Aligner (BWA)53. Mapped reads were filtered (leaving only those mapping in unique genomic positions with enough quality), sorted and indexed with SAMtools. GATK was then used to realign the reads as well as for the base quality score recalibration54. Once a satisfactory alignment was achieved, identification of SNVs and INDELs was performed using GATK standard hard filtering parameters55. For the final exome sequencing analysis report we used the VARIANT annotation tool, which provide additional relevant variant information for the final process of candidate gene selection56. In particular, MAF, obtained from dbSNP database, 1000 Genomes14 and EVS15 projects, was provided to help on the selection of new variants not reported in healthy population to date14,57. SIFT and Polyphen damage scores were computed to predict the putative impact of the discovered variants over the protein structure and functionality58,59. This information was completed with the evolutionary conservation obtained from PhastCons60. Also disease related annotations were provided at both variant and gene levels if available. Finally, GO terms for the affected genes were also retrieved. The successive application of quality control filters and the prioritization by the parameters accounting for potential functional impact led us to build up a list of candidate genes (and variants) ranked by its segregation with the cases and the putative potential impact. Such prioritization list was further inspected to look for potential candidate genes and/or variants.
Targeted NGS
A customized panel including two candidate genes (SAMD11 and ZNF40818,19) and 73 previously known RD genes was developed using the Haloplex capture technology (Agilent Technologies Inc., Santa Clara, CA, USA), as previously described18,19. Amplicons for all coding and non-coding exons, including 20 bp of flanking 5′ and 3′ intronic sequence were designed using the SureDesign webtool (Agilent Technologies, https://earray.chem.agilent.com/suredesign/).
Using this approach, the 14 target regions of SAMD11 were completely covered with 123 amplicons. Target enrichment was performed according to HaloPlex Enrichment System (Agilent Technologies) for Illumina Sequencing protocol with some modifications previously described18,19. Captured target libraries from 180 probands were sequenced on an Illumina MiSeq system (11 samples per run) to obtain 150 bp paired-end reads. A specific custom pipeline for HaloPlex kits on Illumina implemented into the commercial DNAnexus platform (https://www.dnanexus.com/) was used for the bioinformatic analysis, as previously described18,19.
Mutational screening
Bidirectional automatic sequencing was performed in order to confirm and segregate the obtained results by NGS, to determine the frequency of novel variants in a cohort of 380 autosomal recessive or sporadic RP patients and a control cohort and, also to screen the SAMD11 gene in additional 220 patients diagnosed with adulthood - onset arRP. Primers for amplification of the coding exons and splice boundaries of SAMD11 were specifically designed using Primer3 software (Supplementary Table S6). PCR products were enzymatically purified with ExoSAP-it (USB, Affymetrix, Santa Clara, CA, USA) and sequenced on both strands using Big Dye Terminator Cycle Sequencing Kit v3.1 Kit (Applied Biosystems, Waltham, MA, USA). The PCR products were purified on a 96-well multiscreen filter plate (Montage SEQ96 Sequencing Reaction Cleanup Kit, Millipore, Bedford, MA) and resolved on an automated sequencer (ABI 3130xl Genetic Analyzer, Applied Biosystems).
Haplotype analysis
For the STRs genotyping, PCR products were electrophoresed using the automated ABI 3130xl Genetic Analyzer (Applied Biosystems) and analyzed with the GeneMapper v3.5 software (Applied Biosystems). Polymorphic microsatellites with high heterozygosity located at telomeric region of short arm of chromosome 1 were searched on public databases. Haplotype reconstruction was performed using the software Cyrillic ver. 2.1 (Cyrillic Software, Wallingford, UK).
Assessment of the pathogenicity of new variants
The pathogenicity of unreported variants was established by the following criteria: i) co-segregation in the family, ii) absence in 196 Spanish healthy control individuals after screening by Sanger sequencing and in variant databases, such as 1000 genomes14 and EVS15 (http://evs.gs.washington.edu/EVS/), and the CIBERER Spanish Variant Server (http://csvs.babelomics.org/), iii) amino acid conservation for missense mutations in orthologs of the SAMD11 belonging to different evolutionary branches, and iv) pathogenicity prediction with in silico tools, such as Align-GVGD (http://agvgd.iarc.fr/agvgd_input.php)61, SIFT (http://sift.jcvi.org/)58, PolyPhen-2 (http://genetics.bwh.harvard.edu/pph2/)59, Protein Variation Effect Analyzer (PROVEAN; http://provean.jcvi.org/index.php)62, and Human Splicing Finder (HSF; http://www.umd.be/HSF/)63. The BLINK tool and the Jalview Alignment Editor program were used to analyze the multiple sequence alignments.
Array-based comparative genomic hybridization (aCGH)
A custom aCGH 8×60k using the Agilent SurePrint G3 CGH technology was designed using the Agilent eArray website (https://earray.chem.agilent.com/earray/) with an average distribution of 1 probe per 150 bp in the SAMD11 gene with a total of 95 probes. Briefly, genomic DNA (200 ng) from the patient and from a sex-matched control were digested by AluI and RsaI restriction enzymes for 2 h at 37 °C and the digested products were labelled with Cy3-dUTP and Cy5-dUTP fluorochromes using the Sure Tag DNA Labeling Kit (Agilent Technologies). The labelled products were purified, hybridized and washed according to Agilent protocols. The slide was scanned on a SureScan G4900DA scanner (Agilent Technologies), and the resulting TIFF images were converted by the image conversion Feature Extraction software (Agilent Technologies). Results were analyzed by Agilent CytoGenomics software v.2.7 using default analysis method – CGH v2 with the ADM-2 aberration algorithm.
Reverse transcription PCR (RT-PCR)
Blood RNA was isolated from peripheral blood lymphocytes using PAXgene blood RNA kit (Qiagen), according to the protocol provided by the manufacturer. A commercial panel of human RNA from 22 different human tissues (Human Total RNA Master Panel II, Takara Bio Clontech, CA, USA) and human retina (Human Retina QUICK-Clone™ cDNA, Takara Bio Clontech) were analysed by RT-PCR. Total RNAs were reversely transcribed to cDNA with ImProm-II™ Reverse Transcription System (Promega, Madison, WI, USA) using random primers. RT-PCR experiments were performed using SAMD11 exonic primers pairs spanning exons 12, 13 and 14 (Supplementary Table S6). Primers for the housekeeping GAPDH gene were used as internal control. Subsequent Sanger sequencing of the RT-PCR products confirmed correct SAMD11 amplification.
Immunohistochemistry
Anonymized human retina samples were obtained from the eye donors that were collected and stored at the Eye BioBank from Hospital General Universitario de Alicante (Alicante, Spain). Written informed consents were obtained from relatives who donated voluntarily eyeballs for use in research procedures. All experiments were performed in accordance with relevant guidelines and regulations. All procedures were approved by the Ethics Committee from University of Alicante and adhered to the tenets of the Declaration of Helsinki.
Eyes were fixed in 4% paraformaldehyde for 2 hours at room temperature and after washing, cryoprotected using a sucrose gradient. Vertical sections of 16 μm thickness were cut on a cryostat and were immunostained at room temperature overnight with goat polyclonal antibodies to human SAMD11 from Santa Cruz Biotechnology (Santa Cruz, CA, USA; Catalog No. sc-248525) at a 1:50 dilution in 0.1 M sodium phosphate buffer (pH 7.4), 0.5% Triton X-100 in the presence or absence of blocking peptide (20:1 peptide:antibody ratio; Santa Cruz; Catalog No. sc-248525P). Double immunohistochemistry were performed using SAMD11 antibodies in combination with monoclonal mouse anti-rhodopsin at a 1:500 dilution (Millipore Temecula, CA, USA; Catalog No. MAB5356) or monoclonal mouse anti-cone arrestin at a 1:200 dilution (Dr. MacLeish, Morehouse School of Medicine; Atlanta, GA, USA)64, or polyclonal rabbit antibodies anti-red/green opsins at a 1:200 (Millipore; Catalog No.AB5405). Subsequently, the sections were incubated at room temperature for 1 h with Alexa Fluor 488 donkey anti-goat IgG or Alexa Fluor 546 donkey anti-goat IgG, Alexa Fluor 555 donkey anti-mouse IgG and/or Alexa Fluor 633 donkey anti-rabbit IgG secondary antibodies from Molecular Probes (Eugene, OR, USA) at a 1:100 dilution. FITC-labeled peanut agglutinin (PNA) (Vector laboratories, Peterborough, UK; Catalog No.FL-1071) at a 1:100 dilution was incubated together with secondary antibodies. Images were finally obtained under a Leica (Wetzlar, Germany) TCS SP2 confocal laser-scanning microscope.
Western blotting
SAMD11 protein expression was assessed using Western blotting on adult healthy human retina. Proteins (40 μg/lane) were resolved by SDS-PAGE on 4–20% polyacrylamide-gradient gels and electrotransferred to Hybond-P PVDF membranes (GE Healthcare, Buckinghamshire, UK). These were probed at 4 °C overnight with the same SAMD11 antibodies used in immunohistochemistry assays at a 1:500 dilution in 25 mM Tris (pH 8.0), 150 mM NaCl, 2.7 mM KCl (TBS) in the presence or absence of blocking peptide (10:1 peptide:antibody ratio), or with mouse monoclonal antibodies to rabbit muscle GAPDH at a 1:1,000 dilution (Millipore; Catalog No. MAB374). Thereafter, the membranes were incubated at room temperature for 1 h with horseradish peroxidase-conjugated donkey anti-goat (Abcam, Cambridge, UK) or goat anti-mouse (Pierce, Rockford, IL, USA) IgG at a 1:20,000 dilution. Detection was performed by enhanced chemiluminescence using the SuperSignal West Dura system (Pierce).
Network analysis
Network analysis of the candidate gene products was carried out with the SNOW tool, implemented in the Babelomics web package (http://www.babelomics.org/)16,65. SNOW identifies the proteins corresponding to the candidate genes within the human interactome, calculates the Minimal Connected Network (MCN) (the smallest network that connects all the genes in the list) allowing one intermediate interaction and, finally, evaluates its topology by comparing the average clustering coefficient of the MCN versus the resulting value of this parameter in empirical MCNs generated from 1000 random gene lists of same size. The clustering coefficient accounts for the propensity of proteins in the MCN to form a connected unit.
Additional Information
How to cite this article: Corton, M. et al. Identification of the Photoreceptor Transcriptional Co-Repressor SAMD11 as Novel Cause of Autosomal Recessive Retinitis Pigmentosa. Sci. Rep. 6, 35370; doi: 10.1038/srep35370 (2016).
References
Ayuso, C. & Millan, J. M. Retinitis pigmentosa and allied conditions today: a paradigm of translational research. Genome Med 2, 34 (2010).
Hartong, D. T., Berson, E. L. & Dryja, T. P. Retinitis pigmentosa. Lancet 368, 1795–1809 (2006).
Ayuso, C. et al. Retinitis pigmentosa in Spain. The Spanish Multicentric and Multidisciplinary Group for Research into Retinitis Pigmentosa. Clin Genet 48, 120–122 (1995).
den Hollander, A. I., Black, A., Bennett, J. & Cremers, F. P. Lighting a candle in the dark: advances in genetics and gene therapy of recessive retinal dystrophies. J Clin Invest 120, 3042–3053 (2010).
Ran, X. et al. ‘RetinoGenetics': a comprehensive mutation database for genes related to inherited retinal degeneration. Database (Oxford) 2014, (2014).
Daiger, S. P., Sullivan, L. S. & Bowne, S. J. Genes and mutations causing retinitis pigmentosa. Clin Genet 84, 132–141 (2013).
Eisenberger, T. et al. Increasing the yield in targeted next-generation sequencing by implicating CNV analysis, non-coding exons and the overall variant load: the example of retinal dystrophies. PLoS One 8, e78496 (2013).
Consugar, M. B. et al. Panel-based genetic diagnostic testing for inherited eye diseases is highly accurate and reproducible, and more sensitive for variant detection, than exome sequencing. Genet Med 17, 253–261 (2015).
Nishiguchi, K. M. et al. Exome sequencing extends the phenotypic spectrum for ABHD12 mutations: from syndromic to nonsyndromic retinal degeneration. Ophthalmology 121, 1620–1627 (2014).
Avila-Fernandez, A. et al. Whole-exome sequencing reveals ZNF408 as a new gene associated with autosomal recessive retinitis pigmentosa with vitreal alterations. Hum Mol Genet 24, 4037–4048 (2015).
Inoue, T. et al. Cloning and characterization of mr-s, a novel SAM domain protein, predominantly expressed in retinal photoreceptor cells. BMC Dev Biol 6, 15 (2006).
Khan, M. I. et al. CLRN1 mutations cause nonsyndromic retinitis pigmentosa. Ophthalmology 118, 1444–1448 (2011).
Joensuu, T. et al. Mutations in a novel gene with transmembrane domains underlie Usher syndrome type 3. Am J Hum Genet 69, 673–684 (2001).
Abecasis, G. R. et al. An integrated map of genetic variation from 1,092 human genomes. Nature 491, 56–65 (2012).
Tennessen, J. A. et al. Evolution and functional impact of rare coding variation from deep sequencing of human exomes. Science 337, 64–69 (2012).
Minguez, P., Gotz, S., Montaner, D., Al-Shahrour, F. & Dopazo, J. SNOW, a web-based tool for the statistical analysis of protein-protein interaction networks. Nucleic Acids Res 37, W109–W114 (2009).
Medina, I. et al. Babelomics: an integrative platform for the analysis of transcriptomics, proteomics and genomic data with advanced functional profiling. Nucleic Acids Res 38, W210–W213 (2010).
Fernandez-San Jose, P. et al. Targeted Next-Generation Sequencing Improves the Diagnosis of Autosomal Dominant Retinitis Pigmentosa in Spanish Patients. Invest Ophthalmol Vis Sci 56, 2173–2182 (2015).
Perez-Carro, R. et al. Panel-based NGS Reveals Novel Pathogenic Mutations in Autosomal Recessive Retinitis Pigmentosa. Sci Rep 6, 19531 (2016).
Roosing, S. et al. Mutations in RAB28, encoding a farnesylated small GTPase, are associated with autosomal-recessive cone-rod dystrophy. Am J Hum Genet 93, 110–117 (2013).
Jin, G. et al. Identification and characterization of novel alternative splice variants of human SAMD11. Gene 530, 215–221 (2013).
Marquardt, T. & Gruss, P. Generating neuronal diversity in the retina: one for nearly all. Trends Neurosci 25, 32–38 (2002).
Farkas, M. H. et al. Transcriptome analyses of the human retina identify unprecedented transcript diversity and 3.5 Mb of novel transcribed sequence via significant alternative splicing and novel genes. BMC Genomics 14, 486 (2013).
Furukawa, T., Morrow, E. M. & Cepko, C. L. Crx, a novel otx-like homeobox gene, shows photoreceptor-specific expression and regulates photoreceptor differentiation. Cell 91, 531–541 (1997).
Nishida, A. et al. Otx2 homeobox gene controls retinal photoreceptor cell fate and pineal gland development. Nat Neurosci 6, 1255–1263 (2003).
Peng, G. H., Ahmad, O., Ahmad, F., Liu, J. & Chen, S. The photoreceptor-specific nuclear receptor Nr2e3 interacts with Crx and exerts opposing effects on the transcription of rod versus cone genes. Hum Mol Genet 14, 747–764 (2005).
Mollema, N. J. et al. Nuclear receptor Rev-erb alpha (Nr1d1) functions in concert with Nr2e3 to regulate transcriptional networks in the retina. PLoS One 6, e17494 (2011).
Oh, E. C. et al. Rod differentiation factor NRL activates the expression of nuclear receptor NR2E3 to suppress the development of cone photoreceptors. Brain Res 1236, 16–29 (2008).
Freund, C. L. et al. De novo mutations in the CRX homeobox gene associated with Leber congenital amaurosis. Nat Genet 18, 311–312 (1998).
Schorderet, D. F. & Escher, P. NR2E3 mutations in enhanced S-cone sensitivity syndrome (ESCS), Goldmann-Favre syndrome (GFS), clumped pigmentary retinal degeneration (CPRD), and retinitis pigmentosa (RP). Hum Mutat 30, 1475–1485 (2009).
Bessant, D. A. et al. A mutation in NRL is associated with autosomal dominant retinitis pigmentosa. Nat Genet 21, 355–356 (1999).
Corbo, J. C. et al. CRX ChIP-seq reveals the cis-regulatory architecture of mouse photoreceptors. Genome Res 20, 1512–1525 (2010).
Omori, Y. et al. Analysis of transcriptional regulatory pathways of photoreceptor genes by expression profiling of the Otx2-deficient retina. PLoS One 6, e19685 (2011).
Langmann, T. et al. Nonsense mutations in FAM161A cause RP28-associated recessive retinitis pigmentosa. Am J Hum Genet 87, 376–81 (2010).
Ozgul, R. K. et al. Exome sequencing and cis-regulatory mapping identify mutations in MAK, a gene encoding a regulator of ciliary length, as a cause of retinitis pigmentosa. Am J Hum Genet 89, 253–264 (2011).
Hlawatsch, J. et al. Sterile alpha motif containing 7 (samd7) is a novel crx-regulated transcriptional repressor in the retina. PLoS One 8, e60633 (2013).
Tummala, P., Mali, R. S., Guzman, E., Zhang, X. & Mitton, K. P. Temporal ChIP-on-Chip of RNA-Polymerase-II to detect novel gene activation events during photoreceptor maturation. Mol Vis 16, 252–271 (2010).
Schultz, J., Ponting, C. P., Hofmann, K. & Bork, P. SAM as a protein interaction domain involved in developmental regulation. Protein Sci 6, 249–253 (1997).
Qiao, F. & Bowie, J. U. The many faces of SAM. Sci STKE 2005, re7 (2005).
Stapleton, D., Balan, I., Pawson, T. & Sicheri, F. The crystal structure of an Eph receptor SAM domain reveals a mechanism for modular dimerization. Nat Struct Biol 6, 44–49 (1999).
Peterson, A. J. et al. A domain shared by the Polycomb group proteins Scm and ph mediates heterotypic and homotypic interactions. Mol Cell Biol 17, 6683–6692 (1997).
Lai, Z. C. & Rubin, G. M. Negative control of photoreceptor development in Drosophila by the product of the yan gene, an ETS domain protein. Cell 70, 609–620 (1992).
Zhang, J. et al. Sterile alpha motif domain-mediated self-association plays an essential role in modulating the activity of the Drosophila ETS family transcriptional repressor Yan. Mol Cell Biol 30, 1158–1170 (2010).
Qiao, F. et al. Derepression by depolymerization; structural insights into the regulation of Yan by Mae. Cell 118, 163–173 (2004).
Qiao, F. et al. Mae inhibits Pointed-P2 transcriptional activity by blocking its MAPK docking site. EMBO J 25, 70–79 (2006).
Yan, J., Pan, L., Chen, X., Wu, L. & Zhang, M. The structure of the harmonin/sans complex reveals an unexpected interaction mode of the two Usher syndrome proteins. Proc Natl Acad Sci USA 107, 4040–4045 (2010).
Sohocki, M. M. et al. A range of clinical phenotypes associated with mutations in CRX, a photoreceptor transcription-factor gene. Am J Hum Genet 63, 1307–1315 (1998).
Langmann, T. et al. CRX controls retinal expression of the X-linked juvenile retinoschisis (RS1) gene. Nucleic Acids Res 36, 6523–6534 (2008).
Chapman, N. H. et al. Whole exome sequencing in extended families with autism spectrum disorder implicates four candidate genes. Hum Genet 134, 1055–1068 (2015).
Barragan, I. et al. Mutation spectrum of EYS in Spanish patients with autosomal recessive retinitis pigmentosa. Hum Mutat 31, E1772–E1800 (2010).
Avila-Fernandez, A. et al. Identification of an RP1 prevalent founder mutation and related phenotype in Spanish patients with early-onset autosomal recessive retinitis. Ophthalmology 119, 2616–2621 (2012).
Corton, M. et al. Involvement of LCA5 in Leber congenital amaurosis and retinitis pigmentosa in the Spanish population. Ophthalmology 121, 399–407 (2014).
Li, H. & Durbin, R. Fast and accurate short read alignment with Burrows-Wheeler transform. Bioinformatics 25, 1754–1760 (2009).
McKenna, A. et al. The Genome Analysis Toolkit: a MapReduce framework for analyzing next-generation DNA sequencing data. Genome Res 20, 1297–1303 (2010).
DePristo, M. A. et al. A framework for variation discovery and genotyping using next-generation DNA sequencing data. Nat Genet 43, 491–498 (2011).
Medina, I. et al. VARIANT: Command Line, Web service and Web interface for fast and accurate functional characterization of variants found by Next-Generation Sequencing. Nucleic Acids Res 40, W54–W58 (2012).
Sherry, S. T. et al. dbSNP: the NCBI database of genetic variation. Nucleic Acids Res 29, 308–311 (2001).
Kumar, P., Henikoff, S. & Ng, P. C. Predicting the effects of coding non-synonymous variants on protein function using the SIFT algorithm. Nat Protoc 4, 1073–1081 (2009).
Adzhubei, I. A. et al. A method and server for predicting damaging missense mutations. Nat Methods 7, 248–249 (2010).
Siepel, A. et al. Evolutionarily conserved elements in vertebrate, insect, worm, and yeast genomes. Genome Res 15, 1034–1050 (2005).
Mathe, E. et al. Computational approaches for predicting the biological effect of p53 missense mutations: a comparison of three sequence analysis based methods. Nucleic Acids Res 34, 1317–1325 (2006).
Choi, Y., Sims, G. E., Murphy, S., Miller, J. R. & Chan, A. P. Predicting the functional effect of amino acid substitutions and indels. PLoS One 7, e46688 (2012).
Desmet, F. O. et al. Human Splicing Finder: an online bioinformatics tool to predict splicing signals. Nucleic Acids Res 37, e67 (2009).
Zhang, H. et al. Identification and light-dependent translocation of a cone-specific antigen, cone arrestin, recognized by monoclonal antibody 7G6. Invest Ophthalmol Vis Sci 44, 2858–2867 (2003).
Alonso, R. et al. Babelomics 5.0: functional interpretation for new generations of genomic data. Nucleic Acids Res 43, W117–W121 (2015).
Acknowledgements
The authors would like to thank everyone at the Genetics and Ophthalmology Services of Fundación Jiménez Díaz University Hospital, especially all patients who participated in the study. We would also like to thank other members of the European Retinal Disease Consortium (ERDC, http://trish08.wix.com/erdc) for the accession to IBD data and especially Frans Cremers for providing samples. We thank Salvador Marti and Virginia Corrochano from CIBERER Biobank (Valencia, Spain) for their help in the generation of LCLs. This work was supported by several grants from the Spanish Centre for Biomedical Network Research on Rare Diseases (CIBERER)(06/07/0036), Instituto de Salud Carlos III (ISCIII, Spanish Ministry of Health)/FEDER, including FIS (PI013/00226) and RETICS (RD09/0076/00101 and RD12/0034/0010), Ministry of Economy and Competitiveness (MINECO), including FEDER (BFU2012-36845), and BIO2011-27069, Conselleria de Educació of the Valencia Community (PROMETEOII/2014/025), Spanish National Organization of the Blind (ONCE) and the Spanish Fighting Blindness Foundation (FUNDALUCE). M.C. was sponsored by the Miguel Servet Program for Researchers in the Spanish National Health Service (CP12/03256) and RSA by Sara Borrel Postdoctoral Program (CD12/00676), both from the ISCIII/FEDER. A.A-F. was sponsored by CIBERER, RPC is supported by Fundación Conchita Rábago (FCR), L.C is sponsored by RETICS (RD12/0034/0010) from ISCIII and L.d.S. was supported by CAPES Foundation, Ministry of Education of Brazil.
Author information
Authors and Affiliations
Contributions
M.C. participated in study design, participated in the homozigosity mapping, WES analysis, designed and checked the customized gene panel for R.D., participated in the targeted NGS, aCGH, mutation screening and RT-PCR experiments, performed the in silico analysis and drafted the manuscript. A.A.-F. carried out the previously studies of both families, participated in the homozigosity mapping, WES and targeted NGS analysis. L.C. carried out Western blotting and immunohistochemistry experiments. M.S. participated in the mutational screening by Sanger sequencing. B.B. participated in validation of WES data, mutational screening and segregation analysis. M.I.L.-M. carried out the ophthalmologic examinations and participated in the clinical classification of patients. LFS participated in Western blotting and immunohistochemistry experiments. R.S.-A. and da S.L.R.J. designed and performed aCGH experiments. N.R. participated in the mutational screening by Sanger sequencing and RT-PCR analysis. E.M.-G. participated in validation of WES data, RT-PCR analysis and segregation analysis. O.Z. participated in validation of variants from targeted NGS analysis. P.F.-S.J. and R.P.-C. participated in the targeted NGS analysis. F.G.-G. and J.D. performed bioinformatic analysis of WES and carried out in silico protein networks. B.G.-S. carried out the ophthalmologic examinations and participated in the clinical classification of patients. N.C. conceived in the design of Western blotting and immunohistochemistry experiments and obtained funding. C.A. obtained funding, participated in the study design, supervised the clinical classification of patients and reviewed the manuscript. All authors read and approved the final manuscript.
Ethics declarations
Competing interests
The authors declare no competing financial interests.
Electronic supplementary material
Rights and permissions
This work is licensed under a Creative Commons Attribution 4.0 International License. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in the credit line; if the material is not included under the Creative Commons license, users will need to obtain permission from the license holder to reproduce the material. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/
About this article
Cite this article
Corton, M., Avila-Fernández, A., Campello, L. et al. Identification of the Photoreceptor Transcriptional Co-Repressor SAMD11 as Novel Cause of Autosomal Recessive Retinitis Pigmentosa. Sci Rep 6, 35370 (2016). https://doi.org/10.1038/srep35370
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/srep35370
This article is cited by
-
Genetic characteristics and epidemiology of inherited retinal degeneration in Taiwan
npj Genomic Medicine (2021)
-
PRPF31 reduction causes mis-splicing of the phototransduction genes in human organotypic retinal culture
European Journal of Human Genetics (2020)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.