Abstract
This study was carried out to explore associations between assisted reproductive technology (ART) and maternal and neonatal outcomes compared with similar outcomes following spontaneously conceived births. We conducted a retrospective cohort study of pregnancies conceived by ART (N = 2641) during 2006–2014 compared to naturally conceived pregnancies (N = 5282) after matching for maternal age and birth year. Pregnancy complications, perinatal complications and neonatal outcomes of enrolled subjects were investigated and analysed by multivariate logistic regression. We found that pregnancies conceived by in vitro fertilization (IVF) were associated with a significantly increased incidence of gestational diabetes mellitus, gestational hypertension, preeclampsia, intrahepatic cholestasis of pregnancy, placenta previa, placental abruption, preterm premature rupture of membranes, placental adherence, postpartum haemorrhage, polyhydramnios, preterm labour, low birth weight, and small-for-date infant compared with spontaneously conceived births. Pregnancies conceived by intracytoplasmic sperm injection (ICSI) showed similar elevated complications, except some of the difference narrowed or disappeared. Singleton pregnancies or nulliparous pregnancies following ART still exhibited increased maternal and neonatal complications. Therefore, we conclude that pregnancies conceived following ART are at increased risks of antenatal complications, perinatal complications and poor neonatal outcomes, which may result from not only a higher incidence of multiple pregnancy, but also the manipulation involved in ART processes.
Similar content being viewed by others
Introduction
As a result of advances in technology and provision of services, an increasing number of infants are born as a result of assisted reproductive technology (ART) therapy. In developed countries, ART pregnancies represent 1.7% to 4.0% of all births1, while 1.0% of all births in China are the result of ART2.
A “good perinatal outcome” among live births after ART is defined as the live birth of a singleton infant born at term (≥37 completed weeks of gestation) and at a normal birth weight (≥2,500 g)3. However, concern is mounting over the safety of ART and its effect on maternal and fetal well-being. It is well documented that ART pregnancies have a significantly higher risk of multiple pregnancy and adverse perinatal outcomes, including preterm delivery, low birth weight, and birth defects4,5,6. Some studies have suggested an increased risk of preeclampsia, gestational hypertension, placenta previa, and gestational diabetes in ART pregnancies2,7,8.
Nevertheless, there is scarce data examining the type of ART used in relation to the maternal and live-birth outcomes. Also, many prior studies failed to control for maternal age and other relevant variables, for example, gravidity and parity history. The present retrospective cohort study was undertaken to compare the risks of pregnancy complications, perinatal complications and neonatal outcomes in pregnancies following different types of ART with matched spontaneously conceived pregnancies, and in addition to explore the relationship between ART and adverse outcomes with discussion of the underlying mechanisms.
Results
Maternal Characteristics in Pregnancies Conceived after ART and Spontaneity
From 2006 to 2014, 2641 ART-derived pregnancies and 5282 matched spontaneous pregnancies were enrolled in our study. The ART group was divided into in vitro fertilization (IVF) subgroup (n = 2327) and intracytoplasmic sperm injection (ICSI) subgroup (n = 314). The ART group consisted of 1659 singleton gestations and 982 twin gestations, while the spontaneously conceived group consisted of 5193 singleton gestations and 89 twin gestations. Table 1 summarized the maternal and prenatal characteristics. The IVF/ICSI patients in this study tended to be nulliparous, and had higher body mass indices (BMI) and yet a lower rate of previous cesarean delivery. ART births were closer to 20 times more likely to be twins. 2117 women (91%) who conceived after IVF and 209 pregnant women (66.6%) by ICSI had their babies by cesarean section.
Pregnancy, Perinatal Complications and Neonatal Outcomes in ART and Spontaneously Pregnant Groups with Stratified Analysis by Birth Plurality
It was demonstrated that women undergoing ART were more likely to develop pregnancy complications during pregnancy (Table 2). Pregnancies after ART were 1.99 times more likely to develop gestational diabetes mellitus (GDM) (95% CI 1.69–2.36), 2.58 times more likely to have gestational hypertension (95% CI 2.11–3.15), 1.49 times more likely to develop preeclampsia (95% CI 1.12–1.98), and 2.86 times more likely to develop intrahepatic cholestasis of pregnancy (ICP) (95% CI 2.39–3.42) compared with controls. In singleton gestations, the incidence of GDM, gestational hypertension and ICP was still significantly higher than those of the controls. However, there was no statistically significant difference in the incidence of these obstetric complications in twins.
An association between ART and perinatal complications was also significant, which should not be neglected (Table 2). Nearly all the perinatal complications listed, including placenta previa (OR, 2.23, 95% CI 1.79–2.78), placental abruption (OR, 5.06, 95% CI 2.83–9.06), preterm premature rupture of membranes (pPROM) (OR, 3.05, 95% CI 2.48–3.74), placental adherence (OR, 2.37, 95% CI 1.90–2.95), postpartum haemorrhage (OR, 2.72, 95% CI 2.18–3.41), and polyhydramnios (OR, 1.79, 95% CI 1.26–2.53), were more likely to occur after ART in all birth, as well as in singletons with the exceptions of preeclampsia, abnormal placental cord insertion, and oligohydramnios. Nevertheless, no significantly increased incidence of perinatal complications, apart from postpartum haemorrhage, was observed in twins on comparison of the two groups.
The proportions of preterm labour, low birth weight, small for date infant, 1-minute Apgar ≤ 7 and 5-minute Apgar ≤ 7 were significantly higher for ART births than spontaneously conceived births in the total births (Table 3). The incidence rate of fetal macrosomia in the ART group was 3.3%, significantly lower than that in the control group. The differences in macrosomia, small for date infant, and 1-minute Apgar ≤ 7 were not statistically significant after restriction to singletons.
Pregnancy, Perinatal Complications and Neonatal Outcomes in IVF, ICSI and Spontaneously Pregnant Groups
We futher studied the incidences of pregnancy and perinatal complications related with different type of ART, including IVF and ICSI (Table 4). As expected, patients who underwent IVF were more likely to suffer from GDM (11.7%), gestational hypertension (9.3%), preeclampsia (4.0%), ICP (11.8%), placenta previa (7.1%), placental abruption (1.6%), pPROM (9.9%), placental adherence (7.7%), postpartum haemorrhage (7.3%), and polyhydramnios (2.2%), compared with spontaneously conceived pregnancies. We also observed a decrease in the incidence of oligohydramnios in pregnancies undergoing IVF. ICSI pregnancies exhibited higher rates of GDM, gestational hypertension, ICP, pPROM, and postpartum haemorrhage in comparison with spontaneous pregnancies. It seemed that ICSI did not bring more extra pregnancy complications than IVF.
The neonatal outcomes of the three groups were summarized in Table 5. Statistically significant increases were noted in preterm labour (39.9%), low birth weight (37%), and small for date infant (3.6%) among infants who were born after IVF treatment, as well as 1-minute Apgar ≤ 7(5.1%) and 5-minute Apgar ≤ 7 (0.9%). Also, the ICSI group had more negative neonatal outcomes (preterm labour, low birth weight, and small for date infant) than the control group. A decreased incidence of infants with macrosomia was found in the IVF and ICSI group. Differences became insignificant when comparing the incidence between IVF subgroup and ICSI subgroup, apart from preterm labour.
Pregnancy, Perinatal Complications and Neonatal Outcomes in Nulliparous and Multiparous Groups
The incidences of pregnancy and perinatal complications in nulliparous and multiparous women were exhibited in Table 6. There were 2392 ART nulliparous women and 4328 spontaneously pregnant nulliparous women in our study. In the ART nulliparous group, 260 women had a pregnancy complicated by GDM (10.9%), compared with 269 women in the spontaneously pregnant nulliparous group (6.2%, P < 0.001). Significant rises of incidence were also observed in gestational hypertension, preeclampsia, ICP, placenta previa, placental abruption, pPROM, abnormal placental cord insertion, placental adherence, postpartum haemorrhage and polyhydramnios in ART nulliparous women. Meanwhile, among the 249 ART multiparous women and 954 spontaneously pregnant multiparous women, the risk of GDM, gestational hypertension, ICP, placental adherence, and postpartum haemorrhage in ART multiparous women were also markedly increased.
The incidences of poor newborn outcomes in ART nulliparous and multiparous women were shown in Table 7. Statistically significant increases were noted in preterm labour (39.4%), low birth weight (36.8%), small for date infant (4.0%), 1-minute Apgar ≤ 7(4.9%) and 5-minute Apgar ≤ 7 (1.3%) in ART nulliparous women, compared to spontaneously pregnant nulliparous women. On the contrary, there was a decline in the incidence of macrosomia in ART nulliparous group. The occurring rates of preterm labour (42.2%) and low birth weight (33.4%) were significantly elevated in ART multiparous group, compared to spontaneously pregnant multiparous women, with no significant difference in small for date infant, 1 minute Apgar ≤ 7 and 5 minute Apgar ≤ 7.
We then compared the incidences of pregnancy, perinatal complications and infant outcomes in singletons of nulliparous group conceived with ART and conceived spontaneously (Table 8). Totally, there were 1493 ART nulliparous singletons and 4255 spontaneously pregnant nulliparous singletons. In the ART nulliparous singletons group, 177 women had a pregnancy complicated by GDM (11.9%), compared with 262 women in the spontaneously pregnant nulliparous singletons (6.2%), suggesting that ART nulliparous singletons had a greater risk of GDM (P < 0.001). Similarly, statistically significant elevated risks of pregnancy complications including gestational hypertension, preeclampsia, ICP, placenta previa, placental abruption, pPROM, Abnormal placental cord insertion, placental adherence, postpartum haemorrhage, and polyhydramnios were observed in ART nulliparous singletons. However, no statistically significant difference was shown in the incidence of oligohydramnios.
ART nulliparous singletons exhibited significantly increased rates of preterm labour (17.1%), low birth weight (10.3%), 1-minute Apgar ≤ 7 (3.8%) and 5-minute Apgar ≤ 7 (0.7%). compared with spontaneously pregnant nulliparous singletons. Nevertheless, the differences in small for date infant and macrosomia were not statistically significant between the two groups.
Discussion
Despite the wide spread application of ART, studies focused on the obstetric, perinatal, and neonatal outcomes following ART are limited, and the previous studies remain controversial, partly because of different study designs, populations and countries. The present retrospective, hospital-based cohort study containing 7923 subjects was carried out from 2006 to 2014, and corroborated the increased risks of pregnancy complications, perinatal complications and neonatal poor outcomes related to ART. A 20-fold increased incidence of twin gestations in ART pregnancies compared with spontaneous pregnancies was found, and the stratified analysis by birth plurality was then carried out. Furthermore, associations between different types of ART, gravidity and parity history and adverse maternal and live-birth outcomes were investigated.
After restriction to singletons, these rates were reduced, consistent with previous researches9,10, suggesting the necessity to limit the number of embryo transferred legally and to promote single embryo transfer (SET) by the national policy guide. In the ART singleton gestations, 124 women had a pregnancy complicated by gestational hypertension (7.5%), as compared with 125 women in the ART twin gestations (12.7%), suggesting that ART multiples were associated with an increased risk of gestational hypertension. However, singletons of ART pregnancy still exhibited increased maternal and neonatal complications as well. These findings highlight the importance of better IVF process management, and provide valuable information for estimating and improving the safety of ART.
In the present study, we found that an increased risk of hypertensive disorders in pregnancy was associated with pregnancies conceived by ART: gestational hypertension (2.58-fold), preeclampsia (1.49-fold). To date, a wealth of studies had reported that women conceived by ART were at an increased risk for preeclampsia7,11,12, which was consistent with our study. The associations were reduced when analyses were limited to singletons, while significant differences yet remained. Preeclampsia and eclampsia, the etiology of which remains unclear, are major causes of maternal and perinatal mortality and morbidity. Recent studies suggested an association between preeclampsia and defective placental vascular remodeling, abnormal genetic polymorphisms, immune intolerance, vascular endothelial cell activation, and exaggeration of a systemic inflammatory process13,14. The mechanisms by which ART might lead to the increased risk for preeclampsia were elusive. While Chen XK et al.12 reported that there was no increased incidence of preeclampsia among pregnancies conceived by controlled ovarian hyperstimulation (COH) and intrauterine insemination, ART procedure itself might contribute to the marked increased incidence of preeclampsia. Future researches to further delineate placental development in ART births are needed to reveal the underlying mechanism.
GDM results from abnormal glucose tolerance and insulin resistance during pregnancy. The incidence of GDM in our ART group was 11.7%, 1.99-fold increase compared with controls. After restricting to singletons, the incidence increased slightly to 12.9%. Reddy et al.15 and Allen et al.16 also reported that pregnancies after ART demonstrated increased rate of GDM. It is clear that ART is an independent risk factor for GDM. The etiology of GDM is not yet clear. It is suggested that insulin resistance and hyperinsulinemia might partly explain the etiology of GDM17. GDM could be related to the relatively high prevalence of polycystic ovary syndrome (PCOS) among patients undergoing ART18. Furthermore, insulin resistance, which is a known risk factor for the development of GDM, has been proven in a certain proportion of PCOS patients. Moreover, several human studies found that active demethylation might be induced by ART19,20 while epigenetic changes were likely to be involved in GDM. The development of GDM is proposed to be resulted from epigenetic modifications. Well-designed multiple-center longitudinal and intervention-based studies would be helpful and are need in the future.
Our study also found that pregnancies with ART had a higher rate of ICP (11.4% vs. 4.3%, for with ART and no ART, respectively). We compared the risk of ICP in singletons and twins between the ART and spontaneous groups, and the results showed increased risk only in singletons (OR, 1.59, 95% CI 1.25–2.02). Given the low incidence of ICP for most areas, there were few earlier researches on associations between ART and ICP21. The disease appears to be more prevalent among pregnant women in China and it has been associated with increased rates of fetal morbidity and mortality, and an increased risk of maternal coagulopathy. The national conditions underscore the need for study of the possible link between ART and ICP.
We had established that women who underwent ART were more likely to have placenta-mediated pregnancy complications, which comprised a group of diseases, including placenta previa, placenta abruption, abnormal insertion of umbilical cord, and placental adherence. Compared with spontaneous conceptions, ART singleton pregnancies were associated with significantly higher odds of placenta previa (OR, 2.25, 95% CI 1.75–2.89), placenta abruption (OR, 4.43, 95% CI 2.28–8.61), and placental adherence (OR, 2.21, 95% CI 1.71–2.84). This interesting finding raises the possibility that intrauterine operation and manipulation of embryonic cells in ART might be related to abnormalities of location, development and function of the placenta. Shevell et al.11 observed an increased incidence of abnormal placentation in IVF pregnancies, and supposed that initiating of pregnancy and chorion formation in vitro might be the reasons for these complications during gestation. Romundstad et al.22 compared the risk of placenta previa between consecutive pregnancies in the same mother, where one sibling was conceived spontaneously and the other by IVF, and found that placenta previa occurred six times more often in singleton pregnancies after assisted reproduction. Only a few studies have been conducted to evaluate the possible differences in abnormal placental cord insertion and placental adherence among women who delivered after ART with matched controls of spontaneous pregnancies. In the present study, we found that placental adherence and abnormal placental cord insertion occurred more frequently in the ART group. Placental adherence reflects abnormal development of the placenta, and it is an independent risk factor for postpartum haemorrhage, affecting maternal and fetal health. Abnormal placental cord insertion, classified as marginal, and velamentous, may induce intrauterine growth restriction in IVF twins23. Still, it is reasonable to assume that the abnormal placental cord insertion plays a role in adverse neonatal outcomes. Our group has been considering future study to further explore the underlying mechanism. Earlier studies implied that high incidence of placental features in the IVF group may be related to inadequate orientation and/or superficial implantation of the blastocyst due to intrauterine embryo transfer24, and trophectodermal cells might be more sensitive to preimplantation epigenetic upset than inner cell mass25. Taking those studies into consideration, it was suggested that abnormal material exchanges at maternal-fetal interface resulting from inadequate or abnormal placental development might be the reason for poor maternal and live-birth outcome events.
Additionally, it was clear from the study that ART carried an increased risk of polyhydramnios. Findings from our study also indicated a decreased risk of oligohydramnios, not meeting agreements with previous study26. The investigation of this is seldom and the underlying mechanisms were uncertain. One possible explanation was regulating disorder of amniotic fluid production, transportation and absorption, leading to the unbalance of the amniotic fluid volume. The mechanisms leading to these adverse outcomes require a multicenter study and fundamental research for elucidation.
Besides, there were significantly more ART pregnant women diagnosed with pPROM compared to the controls (9.8% vs. 3.3% in total births, 5.1% vs. 3.1% in singletons, respectively). Although its causes remained unknown, pPROM after ART, is the crucial factor for preterm labour and low birthweight. This finding should arouse more recognition of the link between ART and pPROM.
In accordance with other authors, higher rates of preterm birth, low birthweight, and small for dates infant were observed in the ART group. 38.8% gestations conceived following ART were born preterm, 36.5% infants were low birthweight, and 3.8% were small for dates. This phenomenon was thought to result from multiple births in the view of clinicians and researcher. It has previously been suggested that twin pregnancies represents the key factor in the adverse complication for both mother and newborns after IVF/ICSI treatment27. Our observations support these results. The prevalence of twin pregnancies was as high as 37.7% in IVF and 33.4% in ICSI. The risk of adverse outcomes was much higher for both pregnant women and children born from multiple pregnancies. Currently, many clinicians remain to be convinced that single embryo transfer is a better clinical option to lower multiple pregnancy rate, with its following adverse outcomes28,29. Interestingly, an analysis in Australian and New Zealand assisted reproduction programs showed that liveborn singletons conceived by double embryo transfer (DET) had significantly lower mean birthweight and a higher rate of preterm birth than singletons conceived by SET30, which supported the suggestion that increase in proportion of SET procedures would result in a lower rate of multiple births and better perinatal outcomes, even in singletons. Although the incidence of multiplets following ART in China is significantly higher than that of North America and European countries31,32, we surely believe that, with the advancement of ART technology and the strengthen of national guidance, SET will be the top choice in the days to come.
Romundstad et al.33 reported that in the sibling-relationship comparisons, birthweight did not differ substantially between women who conceived spontaneously or after ART, and might therefore be caused by the underlying infertility, rather than ART procedures. Nevertheless, some other researchers held the view that ART procedures might be a major cause of the increased adverse maternal and live-birth outcomes34. There are still a lot of unsolved problems with regard to ART, and we need to make its molecular and cellular mechanism clear. Our study showed an increased risk for preterm labour and low birthweight in both total ART group and singleton group compared with the corresponding controls, but unexpectedly, we did not observe an increase in the incidence of preterm labour in twin pregnancies. The reasons for that were probably: (1) lack of enough samples of twin pregnancies with spontaneously achieved pregnancies; (2) most of the twins conceived by DET are dizygotic, while most spontaneously conceived twins are monozygotic. Therefore, we speculated that it was the result of statistical deflection instead of the advantage of assisted fertilization.
In the IVF subgroup, rates of most pregnancy-induced diseases, perinatal complications and infant outcomes were increased. However, when it came to ICSI, in many instances, the difference narrowed or even disappeared. This finding might be explained by the lower rate of twin gestation in ICSI or limited sample size of women undergoing ICSI. Zollner et al.35 found an increased risk of high blood pressure, preeclampsia, growth retardations and bleeding after IVF pregnancies as well as premature births and intrauterine deaths, attributing more to multiples and to the risk factors of the women involved, rather than the technology itself.
Due to the previous one-child policy in China, only a small number of multipara cases were included in this study. Although complications of ART in multiparas had a similar increased trend in the comparison of nulliparous, the difference of many complications were not statistically significant. With the releasing and carrying out of two-child policy in 2016, the number of multiparas undergoing ART is expected to increase in the coming years. We will continue to follow up more multiparas to enlarge our sample size.
Since the above logistic regression revealed that parity might influence pregnancy outcome, and multiple gestations have negative effects on pregnancy outcomes, we eliminated the cases of twins and multiparas to compare ART nulliparous singletons and spontaneously pregnant nulliparous singletons. We found that ART nulliparous singletons still had higher risks of pregnancy and perinatal complications, compared with spontaneously pregnant nulliparous singletons, implying that some potential factors, such as in vitro ART process or maternal factors might impact the pregnant outcomes. A meta-analysis demonstrated that ART singleton pregnancies were associated with higher risks of adverse obstetric outcomes which need obstetricians spend more concerns on perinatal stage in ART singleton pregnancy26. Our results that ART nulliparous singletons had increased rates of preterm labour, low birth weight and 5-minute Apgar scoring confirmed the above-mentioned statements. Previous researches showed maternal characteristics of subfertile women were associated with a lower birthweight, rather than in vitro fertilization treatment itself additionally contributed to a lower birthweight in the offspring36. However, there was no difference in the incidence of macrosomia and small-for-date infant between the two groups in our study, which might be the result of good nutritional status.
Limitations in our study cannot be overlooked, since no data were collected on the particular cause of infertility, baseline endocrine level, ovarian stimulation protocol, serum hormone levels during ovarian stimulation, as well as number and quality of embryos transferred. Therefore we cannot comment on how these different factors may affect maternal and neonatal outcomes. Ovarian stimulation might be associated with a greater incidence of adverse outcomes than natural cycles, and ovarian stimulation protocol and the hormone levels during ovarian stimulation might be an important confounding variable. The intrauterine insemination (IUI) is a relatively less invasive form of ART. The analysis of the maternal and neonatal outcomes of IUI with ovarian simulation versus natural cycles should be helpful for testing the theoretical paradigm that the more intricate and invasive the form of ART used, the more likely is the pregnancy outcome to be adverse. However, the records of IUI outcomes are lacked in our database, and not included in the present study. It should be considered in future research plan.
In summary, ART births are strongly associated with poorer maternal and live-birth outcomes. Multiple pregnancies can partly explain this phenomenon. However, ART nulliparous singletons still exhibited higher risks of pregnancy and perinatal complications, compared with spontaneously pregnant nulliparous singletons. Elective single embryo transfer should be strongly advocated to reduce the obstetrical risks of ART pregnancy. Since singletons born after the use of ART do worse than those conceived spontaneously, it is suggested that ART process itself is also significantly related to pathologic pregnancy, especially abnormal placental development. Given our findings, we suggest the following: (1) strict control of indications for ART (2) promoting SET; (3) improve the safety of manipulation in the ART process; (4) strengthen antenatal care of ART pregnancies. Whether these adverse outcomes are attributed to couples’ subfertility or ART itself need to be investigated further.
Materials and Methods
Study Population
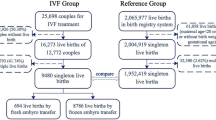
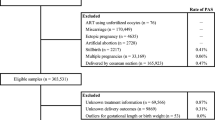
This study is a retrospective, hospital-based cohort study, carried out at Women’s Hospital, School of Medicine, Zhejiang University between January 2006 and December 2014. All 2641 ART-derived pregnancies were matched in a 1:2 fashion to a random sample of spontaneous pregnancies for maternal age and birth year. ART group consisted of 2327 cases of IVF and 314 cases of ICSI. The mean (±SD) maternal age was 31.87 ± 3.96 years in the IVF group, 31.62 ± 3.98 years in ICSI group and 31.72 ± 3.21 years in the control group (Table 1). The ART group and control group were compared for the rates of pregnancy, perinatal complications and neonatal outcomes. Then we further conducted the stratification analysis by types of ART, birth plurality and parity. Figure 1 presents the study flow chart.
Flow chart of context diagram in the study.
(a) IVF vs. ICSI vs. Control Group. (b) ART Total Group vs. Control Total Group; ART Singletons vs. Control Singletons; ART Multiples vs. Control Multiples. (c) ART Nulliparas vs. Control Nulliparas; ART Multiparas vs. Control Multiparas. (d) ART Nulliparous Singletons vs. Control Nulliparous Singletons.
Available information in this dataset included maternal and prenatal factors (maternal age, gravidity with a range of 1 to 11, parity with a range of 1 to 6, birth plurality, maternal education, health problems, previous cesarean delivery, caesarean section, pre-pregnant BMI), and birth outcome (gestational age, birth weight, Apgar score). Clinical definition of the related complications and outcomes were listed in Supplementary Table S1. All data were retrospectively collected on a computerized database or by telephone interview. This retrospectively was approved by the Institutional Review Board of Women’s Hospital, School of Medicine, Zhejiang University. Informed consent was obtained from all patients.
Only data from live newborns after the 28th week of gestation were included in the analysis. Donor oocytes/sperm or embryo recipients, ovulation induction or women applied preimplantation genetic diagnosis were excluded. All subjects with chronic hypertension (hypertension that predated or was diagnosed before the 20th week of gestation), diabetes (insulin dependent or noninsulin dependent diabetes occurred before gestation), or heart disease (any preexisting cardiac diseases including dysrythmias, congenital anomalies, etc.), or fetal anomalies were excluded from this study, because they might be important confounding variables in the observed associations. The methods were carried out in accordance with the approved guidelines.
Statistical analysis
Fisher’s exact probability test was used to compare categorical data. F test was used to evaluate statistical significances of continuous parametric data. Adjusted odds ratios (OR) with 95% confidence intervals (CI) were calculated to approximate relative risks of adverse outcomes. Odds ratios, adjusted for gravidity (1, ≥2), parity(1, ≥2), maternal education (<secondary school, secondary school, collage grade, post-graduate), previous caesarean section (yes, no) and BMI (<18.5, 18.5~23.9, 24.0~27.9, ≥28), were estimated using multivariate logistic regression. The method of backward LR was used for the selection of independent variables in logistic regressions with entry p-value = 0.05 and removal p-value = 0.1. The equations of logistic regression were described in Supplementary Table S2. P values of less than 0.05 were considered statistically significant. Bonferroni correction was employed in our data analyses in multiple comparisons. SPSS software (Version 16, Chicago, IL, USA) was used for data analyses.
Additional Information
How to cite this article: Zhu, L. et al. Maternal and Live-birth Outcomes of Pregnancies following Assisted Reproductive Technology: A Retrospective Cohort Study. Sci. Rep. 6, 35141; doi: 10.1038/srep35141 (2016).
References
Talaulikar, V. S. & Arulkumaran, S. Reproductive outcomes after assisted conception. Obstet Gynecol Surv 67, 566–583 (2012).
Yang, X., Li, Y., Li, C. & Zhang, W. Current overview of pregnancy complications and live-birth outcome of assisted reproductive technology in mainland China. Fertil Steril 101, 385–391 (2014).
Joshi, N. et al. Trends and correlates of good perinatal outcomes in assisted reproductive technology. Obstet Gynecol 120, 843–851 (2012).
Hansen, M., Bower, C., Milne, E., de Klerk, N. & Kurinczuk, J. J. Assisted reproductive technologies and the risk of birth defects–a systematic review. Hum Reprod 20, 328–338 (2005).
Rimm, A. A., Katayama, A. C., Diaz, M. & Katayama, K. P. A meta-analysis of controlled studies comparing major malformation rates in IVF and ICSI infants with naturally conceived children. J Assist Reprod Genet 21, 437–443 (2004).
Wen, J. et al. Birth defects in children conceived by in vitro fertilization and intracytoplasmic sperm injection: a meta-analysis. Fertil Steril 97, 1331-1337 e1331–e1334 (2012).
Jackson, R. A., Gibson, K. A., Wu, Y. W. & Croughan, M. S. Perinatal outcomes in singletons following in vitro fertilization: a meta-analysis. Obstet Gynecol 103, 551–563 (2004).
Sun, L. M. et al. Assisted reproductive technology and placenta-mediated adverse pregnancy outcomes. Obstet Gynecol 114, 818–824 (2009).
Bhattacharya, S. & Kamath, M. S. Reducing multiple births in assisted reproduction technology. Best Pract Res Clin Obstet Gynaecol 28, 191–199 (2014).
Sazonova, A., Kallen, K., Thurin-Kjellberg, A., Wennerholm, U. B. & Bergh, C. Neonatal and maternal outcomes comparing women undergoing two in vitro fertilization (IVF) singleton pregnancies and women undergoing one IVF twin pregnancy. Fertil Steril 99, 731–737 (2013).
Shevell, T. et al. Assisted reproductive technology and pregnancy outcome. Obstet Gynecol 106, 1039–1045 (2005).
Chen, X. K. et al. In vitro fertilization is associated with an increased risk for preeclampsia. Hypertens Pregnancy 28, 1–12 (2009).
Sibai, B. M. Preeclampsia: an inflammatory syndrome? Am J Obstet Gynecol 191, 1061–1062 (2004).
Eastabrook, G., Hu, Y. & von Dadelszen, P. The role of decidual natural killer cells in normal placentation and in the pathogenesis of preeclampsia. J Obstet Gynaecol Can 30, 467–476 (2008).
Reddy, U. M., Wapner, R. J., Rebar, R. W. & Tasca, R. J. Infertility, assisted reproductive technology, and adverse pregnancy outcomes: executive summary of a National Institute of Child Health and Human Development workshop. Obstet Gynecol 109, 967–977 (2007).
Allen, V. M., Wilson, R. D. & Cheung, A. Pregnancy outcomes after assisted reproductive technology. J Obstet Gynaecol Can 28, 220–250 (2006).
Kopp, W. Role of high-insulinogenic nutrition in the etiology of gestational diabetes mellitus. Med Hypotheses 64, 101–103 (2005).
Maman, E., Lunenfeld, E., Levy, A., Vardi, H. & Potashnik, G. Obstetric outcome of singleton pregnancies conceived by in vitro fertilization and ovulation induction compared with those conceived spontaneously. Fertil Steril 70, 240–245 (1998).
Li, T. et al. IVF results in de novo DNA methylation and histone methylation at an Igf2-H19 imprinting epigenetic switch. Mol Hum Reprod 11, 631–640 (2005).
Zhang, Y. L. et al. Active demethylation of individual genes in intracytoplasmic sperm injection rabbit embryos. Mol Reprod Dev 72, 530–533 (2005).
Davidson, K. M. Intrahepatic cholestasis of pregnancy. Semin Perinatol 22, 104–111 (1998).
Romundstad, L. B. et al. Increased risk of placenta previa in pregnancies following IVF/ICSI; a comparison of ART and non-ART pregnancies in the same mother. Hum Reprod 21, 2353–2358 (2006).
Cai, L. Y. et al. Abnormal placental cord insertion may induce intrauterine growth restriction in IVF-twin pregnancies. Hum Reprod 21, 1285–1290 (2006).
Daniel, Y. et al. Do placentae of term singleton pregnancies obtained by assisted reproductive technologies differ from those of spontaneously conceived pregnancies? Hum Reprod 14, 1107–1110 (1999).
Mann, M. R. et al. Selective loss of imprinting in the placenta following preimplantation development in culture. Development 131, 3727–3735 (2004).
Qin, J., Liu, X., Sheng, X., Wang, H. & Gao, S. Assisted reproductive technology and the risk of pregnancy-related complications and adverse pregnancy outcomes in singleton pregnancies: a meta-analysis of cohort studies. Fertil Steril 105, 73-85 e71–e76 (2016).
Prevention of twin pregnancies after IVF/ICSI by single embryo transfer. ESHRE Campus Course Report. Hum Reprod 16, 790–800 (2001).
Guidelines on number of embryos transferred. Fertil Steril 92, 1518–1519 (2009).
Wang, J., Lane, M. & Norman, R. J. Reducing multiple pregnancy from assisted reproduction treatment: educating patients and medical staff. Med J Aust 184, 180–181 (2006).
Wang, Y. A., Sullivan, E. A., Healy, D. L. & Black, D. A. Perinatal outcomes after assisted reproductive technology treatment in Australia and New Zealand: single versus double embryo transfer. Med J Aust 190, 234–237 (2009).
Andersen, A. N. et al. Assisted reproductive technology in Europe, 2004: results generated from European registers by ESHRE. Hum Reprod 23, 756–771 (2008).
Koivisto, M., Jouppila, P., Kauppila, A., Moilanen, I. & Ylikorkala, O. Twin pregnancy. Neonatal morbidity and mortality. Acta Obstet Gynecol Scand Suppl, 21–29 (1975).
Romundstad, L. B. et al. Effects of technology or maternal factors on perinatal outcome after assisted fertilisation: a population-based cohort study. Lancet 372, 737–743 (2008).
Terada, Y., Luetjens, C. M., Sutovsky, P. & Schatten, G. Atypical decondensation of the sperm nucleus, delayed replication of the male genome, and sex chromosome positioning following intracytoplasmic human sperm injection (ICSI) into golden hamster eggs: does ICSI itself introduce chromosomal anomalies? Fertil Steril 74, 454–460 (2000).
Zollner, U. & Dietl, J. Perinatal risks after IVF and ICSI. J Perinat Med 41, 17–22 (2013).
Seggers, J. et al. Effects of in vitro fertilization and maternal characteristics on perinatal outcomes: a population-based study using siblings. Fertil Steril 105, 590–598 e592 (2016).
Acknowledgements
The authors are grateful to Dr. Suresh John Duthie, the Consultant Obstetrician and Gynaecologist of Blackpool Victoria Hospital NHS Trust, UK, who aided in the revision of the manuscript. We would like to thank Professor Guangdi Chen, Jing Guo for their assistance in the statistical analysis, and all our colleagues providing help during the data collection. Grant support was provided by the National Basic Research Program of China (No. 2013CB967404), the National Natural Science Foundation of China (Nos 81270664 and 81471421), the Science Foundation for Distinguished Young Scholars of Zhejiang Province (No. LR14H040001), and the Program for Changjiang Scholars and Innovative Research Team in University (No. IRT1184).
Author information
Authors and Affiliations
Contributions
D.Z. and H.F.H. contributed to the conception and design of the study. L.L.Z., Y.Z., Y.H., Y.Q.W., L.B.Z., Y.Y.C. and L.X. contributed to the data collection. Y.F.L., R.J.Z., F.L., M.G.L., S.J.S., L.F.X. and Y.M.Z. contributed to the follow-up of enrolled subjects. L.L.Z., Y.Z., D.Z. and H.F.H. contributed to the analysis and interpretation of data. L.L.Z., Y.Z., D.Z. and R.J.Z. contributed to draft the article and revise it critically. All authors reviewed the manuscript and approved the version to be published.
Ethics declarations
Competing interests
The authors declare no competing financial interests.
Electronic supplementary material
Rights and permissions
This work is licensed under a Creative Commons Attribution 4.0 International License. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in the credit line; if the material is not included under the Creative Commons license, users will need to obtain permission from the license holder to reproduce the material. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/
About this article
Cite this article
Zhu, L., Zhang, Y., Liu, Y. et al. Maternal and Live-birth Outcomes of Pregnancies following Assisted Reproductive Technology: A Retrospective Cohort Study. Sci Rep 6, 35141 (2016). https://doi.org/10.1038/srep35141
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/srep35141
This article is cited by
-
Maternal and neonatal outcomes of intrahepatic cholestasis of pregnancy after in vitro fertilization
BMC Pregnancy and Childbirth (2024)
-
Atrial fibrillation considerations in the fourth trimester (postpartum period)
Journal of Interventional Cardiac Electrophysiology (2024)
-
Reproductive Outcomes of Conventional In Vitro Fertilization and Intracytoplasmic Sperm Injection in Patients with Non-Severe Male Infertility Across Poor and Different Sub-Optimal Ovarian Response Categories: A Cohort Study Based on 30,352 Fresh Cycles from 2009–2019
Reproductive Sciences (2024)
-
Gestational diabetes mellitus in patients undergoing assisted reproductive techniques or conceiving spontaneously: an analysis on maternal and foetal outcomes
Journal of Endocrinological Investigation (2024)
-
The risk of perinatal and cardiometabolic complications in pregnancies conceived by medically assisted reproduction
Journal of Assisted Reproduction and Genetics (2024)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.