Abstract
Systemic lupus erythematosus (SLE) is a systemic autoimmune disease characterized by the development of autoantibodies to nuclear antigens and inflammatory responses mediated by multiple cytokines. Although previous studies have determined clinical associations between SLE and the anti-inflammatory cytokines IL-10 and IL-37, their role in the disease, or their potential as biomarkers, remains unclear. We examined serum levels of IL-10 and IL-37 in a large cohort of SLE patients, with detailed longitudinal clinical data. We demonstrate a statistically significant association of serum IL-10 with disease activity, with higher levels in active compared to inactive disease. High first visit IL-10 was predictive of high subsequent disease activity; patients with IL-10 in highest quartile at first visit were 3.6 times more likely to have active disease in subsequent visits. Serum IL-37 was also higher in SLE patients compared to control, and was strongly associated with Asian ethnicity. However, IL-37 was not statistically significantly associated with disease activity. IL-37 was significantly reduced in patients with organ damage but this association was attenuated in multivariable analysis. The data suggest that IL-10, but not IL-37, may have potential as a biomarker predictive for disease activity in SLE.
Similar content being viewed by others
Introduction
Interleukin-10 (IL-10) is a homodimeric protein that is produced by macrophages, dendritic cells and helper T cells in response to multiple stimuli1,2,3. Actions of IL-10 on immune cells in vitro include the inhibition of both macrophage and T cell activation and of pro-inflammatory cytokine production4,5,6,7,8,9. In contrast, IL-10 increases B cell survival, proliferation, differentiation and antibody production10, and decreases auto-reactive B-cell apoptosis by increasing Bcl-2 expression, resulting in increased autoantibody production in systemic lupus erythematosus (SLE)11,12. Enhanced production of IL-10 has been reported in SLE and systemic sclerosis, while deficiency of IL-10 is reported in inflammatory bowel disease, psoriasis and rheumatoid arthritis1.
Previous studies evaluating clinical associations of IL-10 in SLE have mostly been small, retrospective, or have had other methodological limitations. In these smaller studies, serum concentrations of IL-10 have consistently been shown to be higher in SLE patients compared with healthy controls, and to positively correlate with measures of disease activity13,14,15, but the predictive value of IL-10 as a biomarker has not been examined in longitudinal studies. One study of administration of an anti-IL-10 monoclonal antibody in patients with SLE demonstrated a reduction in disease activity, consistent with a pathogenic role for IL-10 in SLE, but this finding is limited by the small sample size and lack of a control group16. In mouse models of SLE, IL-10 neutralization effectively delayed disease onset, but IL-10 deficiency resulted in more severe disease earlier in the disease course17. In contrast, IL-10 overexpression delayed the onset of autoantibody production and decreased nephritis in murine lupus19, suggesting that IL-10 can be either protective or pathologic at different stages of the disease20. Indeed, as the pathogenic drive in SLE shifts from innate immunity to a predominantly B-cell centric model, so too might the role of IL-1021.
Like IL-10, IL-37 is a cytokine known to have anti-inflammatory effects, but whose range of actions relevant to SLE are poorly understood. A member of the IL-1 family, IL-37 was first identified in 2000 by three independent groups22,23,24 as a new molecule within the IL-1 family locus on chromosome 2q13. Initially referred to as IL-1 family member 7 (IL-1F7), it was renamed IL-37 in 2010, as its unique physiological functions came to light25,26.
Constitutive levels of IL1F7 (the gene encoding IL-37) mRNA are low in human monocytes in the absence of inflammatory stimulation27, while TLR ligands such as LPS up-regulate IL1F7 transcription and increase IL1F7 mRNA stability28. Like IL-1β and IL-18, IL-37 is produced as a pro-form, which can undergo processing by caspase-1. IL-37 is expressed as multiple splice variants, with the longest and likely the biologically most relevant isoform, IL-37b, being expressed in monocytes and lymph nodes28,29. IL-37 uses a heterodimeric receptor complex comprising IL-1 receptor 8 (IL-1R8) and the alpha chain of the IL-18 receptor (IL-18Rα) to activate an intracellular anti-inflammatory program, inhibiting the kinases Fyn and TAK1, as well as mitogen-activated protein kinases (MAPK) and the transcription factor NF-κB30.
Only one previous study has examined the expression of IL-37 in SLE. Song et al. measured IL-37 levels in the sera of 30 patients with SLE and demonstrated a strong positive correlation between IL-37 levels and disease activity, as measured using the SLE disease activity index 2000 (SLEDAI-2k)31. Correlation between IL1F7 mRNA expression and mRNA of other inflammatory cytokines, including IL18, IL6 and IFNG, in SLE peripheral blood mononuclear cells (PBMCs) was also shown.
As limited studies have informed the value of serum IL-10 and IL-37 as biomarkers of SLE disease state, their potential as therapeutic targets remains poorly understood. Therefore, we undertook a study of clinical associations of these two anti-inflammatory cytokines in a large cohort of patients with SLE with detailed longitudinal clinical information.
Results
Patient Characteristics
Cytokines were quantified in a total of 141 serum samples obtained at a first study visit, and in 251 additional samples obtained from a subset of 129 patients at consecutive subsequent clinic visits within an approximately 24-month period. Patients’ characterisitcs are presented in Table 1. In brief, 84% of the patients were females, with a median age of 42 years and 41% (n = 58) were of Asian ethnicity (Table 1). The median age at first visit was 42 (IQR 32, 52) years and median disease duration was 103 (18–439) months. At first visit, 55 patients (39%) were found to have active disease (SLEDAI-2k > 4); of these, 17 patients had highly active disease (SLEDAI-2k ≥ 10). Medications used by the patients during study period are shown in Table 1; approximately 66% (n = 93) of patients were taking prednisolone (PNL) at the first visit of this study.
IL-10 and IL-37 concentration in SLE vs. Controls
IL-10 was detectable in 128 SLE patient samples (90.1%) at first visit and 91.8% of all samples. IL-10 measured at first visit was found to be significantly higher in the serum of SLE patients compared to controls (p < 0.01, Fig. 1A). This significant difference was reproduced at each individual time point, and when all results were pooled (data not shown).
Serum IL-10 is increased in SLE and active disease.
Serum levels of (A) IL-10 and (B) IL-37, measured by ELISA, in patients with SLE, compared with healthy controls. Correlations graphs of (C) First visit IL-10 and (D) IL-10 from all visits with SLEDAI-2k. (E) Comparison of Serum IL-10 in patients with inactive (SLEDAI-2k < 4) or active disease (SLEDAI-2k > 4) (F) Comparison of serum IL-37 levels in patients with inactive or active disease. The horizontal line in each dot plot depicts the median.
IL-37 was detectable in 77 SLE samples (54.2%) at first visit and 64.3% of all samples. At first visit, IL-37 was statistically significantly higher in SLE patients compared with controls (p < 0.01) (Fig. 1B). The finding of significantly higher serum IL-37 in SLE patients compared to controls was reproduced at each individual time point, and when all results were pooled (data not shown).
IL-10, IL-37 and SLE disease activity
We examined correlations between IL-10 and IL-37 and disease activity. A modest but statistically significant positive correlation was observed between first visit IL-10 and SLEDAI-2k (r = 0.3121, p < 0.01) (Fig. 1C). This correlation was reproduced when data from all visits was examined (r = 0.2176, p < 0.01) (Fig. 1D). When patients were categorized as having inactive (SLEDAI-2k ≤ 4) or active (SLEDAI-2k > 4) disease, a statistically significantly higher median IL-10 concentration was observed in those with active disease (p < 0.01) (Fig. 1E).
In contrast, in the same samples, no significant correlations were found between IL-37 and disease activity (r = −0.2910, p = 0.7) (not shown). No significant difference in median IL-37 was detected between patients categorized as inactive (SLEDAI-2k ≤4) or active (SLEDAI-2k > 4) (p = 0.6) (Fig. 1F).
Factors associated with serum IL-10
We next examined several factors associated with IL-10 levels measured at first visit, including demographics, disease activity, organ damage and PNL use, using linear regression analysis. Univariable analysis revealed Asian ethnicity, PNL use and disease activity (SLEDAI-2k > 4) were associated with elevated IL-10 expression with statistical significance (Table 2). Patients with Asian ethnicity had more than twice the amount of serum IL-10 when compared to non-Asians (ratio of the GM = 2.2 [95% CI 1.09, 4.42]; p = 0.03). Similarly, patients on PNL at first visit also had significantly higher IL-10 (ratio of the GM = 2.6 (95% CI 1.25, 5.31; p = 0.03). Patients with active disease had serum IL-10 concentrations nearly three times higher than those with inactive disease. There were no associations between the use of other immunomodulatory medications, including hydroxychloroquine, methotrexate, azathioprine and mycophenolate mofetil, with IL-10 expression.
In the multivariable linear regression analysis, only disease activity remained statistically significantly associated with serum IL-10 (Table 2). Interestingly, the association between PNL use and IL-10 disappeared when adjusted for disease activity; meaning disease activity confounded the association between PNL and IL-10. The association between Asian ethnicity and increased IL-10 was also attenuated (Table 2). Use of other drugs (Table 1) was too variable among patients to be the subject of analysis for associations with serum IL-10.
Factors associated with serum IL-37
Similarly, factors associated with serum IL-37 measured at first visit were examined and the results are presented in Table 3. Again, Asian ethnicity was statistically significantly associated with increased serum IL-37 levels when compared to non-Asians, and this association remained statistically significant in multivariable linear regression analysis (adjusted ratio of the GM = 3.58 [95% CI 1.34, 9.58]; p = 0.01). In contrast, disease activity was not found to be associated with IL-37 expression. In addition, we observed significantly reduced levels of IL-37 in patients who had organ damage at first visit during univariable analysis but the statistical significance was attenuated when adjusted for ethnicity (adjusted ratio of the GM = 0.42 [95% CI 0.17, 1.07]; p = 0.07).
First visit IL-10 levels and subsequent disease activity
We further examined whether levels of IL-10 measured at the first visit could predict subsequent disease activity. This analysis was restricted to patients with two or more visits; multivariable logistic regression analysis was carried out and the results are summarised in Table 4. Patients whose IL-10 levels were in the highest quartile were 3.6 times more likely to experience active disease (SLEDAI-2K > 4) even after adjusting for prednisolone use and ethnicity (adjusted odds ratio = 3.63 [95% CI; 1.31, 10.1], p = 0.01). PNL use at the first visit was also a predictor of subsequent active disease (Table 4).
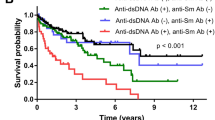
In addition to the association with overall disease activity, a significant positive correlation was seen between IL-10 measured at the first visit and commonly used markers of inflammation in SLE, including erythrocyte sedimentation rate (ESR) (r = 0.2189, p < 0.01) and anti-dsDNA antibodies (r = 0.2175, p < 0.01), and corresponding significant negative correlations with C3 (r = −0.2360, p < 0.01) and C4 (r = −0.2023, p = 0.02) (not shown). Similar statistically significant correlations between serum IL-10 and ESR, dsDNA, C3 and C4 were observed in the samples taken at each of the subsequent study timepoints (data not shown). No significant correlations were found between IL-37 and ESR, anti-dsDNA antibody, C3 and C4.
We also assessed the relationship between IL-10 and disease activity when both were measured over time, using the time-adjusted mean SLEDAI-2k (AMS) and time-adjusted mean (TAM) IL-10. TAM IL-10 was statistically significantly correlated with AMS (r = 0.2518, p = 0.02) (Fig. 2A). TAM IL-10 was also found to be higher in patients who suffered an episode of persistently active disease (PAD) during their disease course, compared to those who did not (p < 0.01) (Fig. 2B). IL-10 measured at the first visit was also significantly correlated with AMS (r = 0.2588, p < 0.01) (Fig. 2C) and was significantly higher in patients with subsequent PAD (p = 0.01) (Fig. 2D). In contrast, no statistically significant correlation was demonstrated between first visit IL-37 and subsequent disease activity (Supplementary Figure S1).
Serum IL-10 is correlated with longitudinal assessments of disease activity in SLE.
(A) Correlation between time-adjusted mean (TAM) serum IL-10 and time adjusted mean SLEDAI-2k (AMS). (B) comparison of TAM IL-10 in serum from patients with or without persistently active disease (PAD), measured by ELISA. (C) Correlation between first visit serum IL-10 with AMS. (D) Comparison of first visit IL-10 in serum from patients with or without persistently active disease (PAD), measured by ELISA. The horizontal line in each dot plot depicts the median.
IL-10, IL-37 and organ involvement
We next examined the association between IL-10 and IL-37 and specific organ involvement using the organ-domain SLEDAI-2k scores. Musculoskeletal activity (p = 0.05), renal activity (p = 0.03), serositis (p = 0.05) and serological activity (p < 0.01) were each found to be associated with increased IL-10 expression (Fig. 3). No significant difference in serum IL-10 was seen between SLE patients with and without CNS, vasculitis or cutaneous disease or in patients with or without fever or heamatoligical activity (Fig. 3).
Associations of serum IL-10 with organ-specific disease activity in SLE.
Geometric mean concentrations of IL-10 (with corresponding 95% confidnece interval in pg/mL), derived from univariable linear regression analyses by organ-specific disease; (A) Central nervous system (CNS) activity, (B) vasculitis (VAS), (C) musculoskeletal (MSK) activity, (D) renal activity, (E) Cutaneous (CUT) disease, (F) Serositis (SER), (G) Serological (Serol.) activity, (H) Fever, (I) Heamatological (Heam.) activity. Values are geometric means.
Discussion
Many cytokines are raised in the serum of SLE patients, reflective of the systemic inflammation inherent in the disease32. Previous studies have demonstrated that IL-10 is increased in the serum of SLE patients compared to controls13,14,15,33,34,35,36,37,38,39. Despite the uncertainty regarding its function, the consistency with which higher IL-10 levels are seen is informative about the altered cytokine milieu in SLE, particularly as studies, including this one, have shown a positive association between IL-10 and disease activity. In the current study we show that at an individual time point, and also when integrated over time, elevated serum IL-10 is associated with overall disease activity as measured by SLEDAI-2k.
The association observed between IL-10 and disease activity is supported by the correlations seen between IL-10 and other markers of disease severity, such as active renal disease and patients’ ESR, C3 and C4. As these laboratory markers are commonly used in addition to clinical features as indicators of disease activity, their correlation with IL-10 supports its potential as a marker of disease activity. Serum IL-10 has previously been found to be higher in patients with active nephritis compared to patients with inactive disease or controls, although interpretation of that study was limited by a sample size of 1240. In addition, levels of serum IL-10 correlated with anti-dsDNA antibody titers, as has been previously reported13,14,15. This correlation highlights a potential mechanism by which IL-10 might contribute to pathology in established SLE. The ability of IL-10 to enhance B-cell survival, proliferation, differentiation and antibody production, as well inhibiting auto-reactive B-cell apoptosis, may contribute to elevated anti-dsDNA titers in SLE patients10,11,12. Given that circulating immune complexes have been shown to increase IL-10 synthesis and that IL-10 can, in turn, facilitate the production of autoantibodies, it could be suggested that IL-10 acts pathogenically in SLE by amplifying and perpetuating an inflammatory cycle1,2,41. This hypothesis requires further in vitro and in vivo exploration.
IL-10 has only been measured in a longitudinal context in SLE in one previous study, performed by Park et al.37. However, this study contained only 40 participants followed up over 4 weeks. Here, we show that elevated IL-10 levels are associated with subsequent disease activity. The ability for a clinician to anticipate which patients may require more aggressive management or more frequent monitoring would represent a significant breakthrough in the management of SLE. In light of this, the predictive capacity of IL-10 should be investigated further, and evaluated in combination with other predictive biomarkers to generate a potentially more powerful composite measure42.
We found serum IL-10 to be higher in the samples of patients taking glucocorticoids. Glucocorticoids have been shown to up-regulate the production of IL-10 in vitro43, but importantly we found that the associations of serum IL-10 with glucocorticoids was attenuated after adjustment for disease activity. Higher IL-10 concentrations were also seen in SLE patients of Asian ethnicity. While studies of IL-10 in SLE have been performed in cohorts with a range of ethnic predominance, the small sample sizes of these studies made it difficult to develop a clear pattern of IL-10 in different ethnic groups. It is not clear to what extent specific cytokines are involved in the causation of the more severe pattern of disease seen in Asian SLE patients44. The role that IL-10 might play in this phenotype, however, presents an interesting area for future research. Of note, ethnicity was not recorded for healthy controls used in this study, but the low rates of detection of IL-10 and IL-37 in controls suggest this was not a confounder of the difference between controls and SLE patients.
Our data also demonstrates significantly higher levels of serum IL-10 in patients with specific organ disease in SLE, including musculoskeletal activity, renal disease, serositis and serological activity. Similar differences were not seen between patients with and without CNS, vasculitis or cutaneous disease or in patients with or without fever or heamatoligical activity. However, with the exception of cutaneous and heamatological activities, numbers of patients in the affected groups were very low (1 or 3), so greater numbers are needed to fully assess these comparisons.
IL-37 is an anti-inflammatory cytokine expressed by a range of immune and non-immune cells26,30, but its function and role in disease is not well understood. IL-37 has, however, been suggested to be a cytokine biomarker in SLE, as it was previously found to be significantly higher in SLE patients compared to controls31. Here, we also found serum IL-37 to be higher in SLE patients, but in contrast to the previous study31, we saw no associations between serum IL-37 and disease activity. One possible reason for this discrepancy may be the differences in cohorts between these two studies. Song et al. studied only treatment-naïve Asian patients with highly active disease (SLEDAI-2k ≥10)31, whereas our cohort included patients from different ethnic backgrounds with a range of disease activity and treatments. Nonetheless, subgroup analysis, examining only Asian patients with highly active disease, failed to replicate the results of Song et al. (data not shown). It should be noted, however, that IL-37 was detected in fewer patients than IL-10, so a larger cohort might reveal more positive associations. It is not clear whether this is due to technical issues (i.e. sensitivity of the ELISA), or other reasons. Indeed, in many cases, associations with IL-37 show similar trends to IL-10, but would require more samples to achieve significance.
In conclusion, in the largest study to date supported by longitudinal data, we show a strong association of serum IL-10 with disease activity in SLE, wherein levels are higher in active compared to inactive disease, are higher in Asian patients and in association with renal disease, and are predictive of subsequent disease activity. Our data do not indicate a strong association of serum IL-37 with disease activity, although we suggest an even larger cohort is required to validate this.
Methods
Patients and clinical assessments
Between May 2007 and January 2012, all patients aged over 18 fulfilling the 1982 American College of Rheumatology (ACR) criteria45 who received care at the Monash Lupus Clinic, Melbourne Australia, were invited to participate in a longitudinal study of disease activity and biomarkers, as previously described46,47. Patients received standard-of-care therapy and were assessed at clinic visits as scheduled by the treating physician. Patients were included in the current study if complete clinical data and matching serum samples were available on up to three consecutive visits. Birth date, gender, ethnicity and year of disease onset were recorded at the first visit. Documentation of disease activity was performed using SLEDAI-2k48 at each clinic visit. Active disease was defined as a SLEDAI-2k score > 4 and highly active disease was defined as a score ≥ 10. Persistently active disease (PAD) was classified according to Nikpour et al., as ≥2 consecutive visits with a SLEDAI-2k 4, excluding SLEDAI-2k scores comprising exclusively serological parameters49. To account for disease activity over time, the time-adjusted mean SLEDAI (AMS) was derived50. In this cohort, disease-related organ damage is recorded annually using the Systemic Lupus International Collaborating Clinics (SLICC) SLE Damage Index (SDI)51. The presence of active SLE in specific organs was determined as described46,47, on the basis of a positive score in the relevant categories of the SLEDAI-2k. For example, active renal disease was defined as a non-zero score in any of the renal components of the SLEDAI-2k. Anti-dsDNA antibodies were measured using a Farr assay (Anti-dsDNA kit, Trinity Biotech, Wicklow, Ireland) with a normal value of <7 or ELISA with a normal value of <29 and are expressed as a ratio to the upper limit of normal in the assay used. Data are represented as fold increase over the normal value. Written informed consent was obtained from all subjects. All experimental protocols were approved by the Human Research Ethics Committee, Monash Health. All methods were carried out in accordance with the relevant guidelines.
Serum cytokine quantification
Venous blood was collected in conjunction with routine laboratory testing for each visit, and serum obtained and stored at − 80 °C until analysis, as described46,47. Control serum was obtained from 28 healthy individuals whose age and gender was not significantly different to the patients. All controls had normal ESR, indicating that they represent a ‘non-inflamed’ population.
Specific enzyme-linked immunosorbent assay (ELISA) kits were used to measure serum IL-10 (Biolegend, San Diego, CA, USA) and IL-37 (Adipogen, Liestal, Switzerland) according the manufacturer’s protocols. Each sample was tested in duplicate. Where multiple samples over time were available, a TAM IL-10 or IL-37 concentration was calculated46. Any samples that exceeded the upper limit of the standard curve was subsequently diluted in PBS with 1% BSA and re-tested.
Statistical analysis
All statistical analyses were performed using Stata version 13.1 (StataCorp, College Station, Texas, USA). For the samples which had readings below the detection limit of the ELISA (3.9 pg/mL for IL-10 and 16 pg/mL for IL-37), a value of 1 was assigned. Sensitivity analyses were performed by including and excluding the readings below the limit of detection, and the results were unchanged; therefore, the data including all samples are presented.
Continuous variables were described as median (interquartile range [IQR], range) and categorical variables were described as frequency (%). Comparison of quantitative values was performed using the Mann-Whitney U test for unpaired data. Spearman’s rank correlation was used to examine correlations between two variables.
Both IL-10 and IL-37 values were positively skewed, therefore, they were log10 transformed in order to carry out linear regression analyses to examine their associations with demographics and clinical phenotypes. The serum IL-10 and IL-37 levels have been reported as the geometric means in pg/mL with corresponding 95% confidence intervals. In addition, logistic regression analysis was performed to examine whether IL-10 measured at first visit was associated with subsequent disease activity. Variables with p-value < 0.1 in the univariable regression models were included in multivariable regression models. A p value < 0.05 was considered statistically significant.
Additional Information
How to cite this article: Godsell, J. et al. Clinical associations of IL-10 and IL-37 in systemic lupus erythematosus. Sci. Rep. 6, 34604; doi: 10.1038/srep34604 (2016).
References
Boonstra, A. et al. Macrophages and myeloid dendritic cells, but not plasmacytoid dendritic cells, produce IL-10 in response to MyD88- and TRIF-dependent TLR signals, and TLR-independent signals. J Immunol 177, 7551–7558 (2006).
McGeachy, M. J. et al. TGF-beta and IL-6 drive the production of IL-17 and IL-10 by T cells and restrain T(H)-17 cell-mediated pathology. Nat Immunol 8, 1390–1397, 10.1038/ni1539 (2007).
Peng, H. et al. Role of interleukin-10 and interleukin-10 receptor in systemic lupus erythematosus. Clin Rheumatol 32, 1255–1266, 10.1007/s10067-013-2294-3 (2013).
Ding, L., Linsley, P. S., Huang, L. Y., Germain, R. N. & Shevach, E. M. IL-10 inhibits macrophage costimulatory activity by selectively inhibiting the up-regulation of B7 expression. J Immunol 151, 1224–1234 (1993).
Joss, A., Akdis, M., Faith, A., Blaser, K. & Akdis, C. A. IL-10 directly acts on T cells by specifically altering the CD28 co-stimulation pathway. Eur J Immunol 30, 1683–1690, 10.1002/1521-4141(200006)30:6<1683::AID-IMMU1683>3.0.CO;2-A (2000).
McBride, J. M., Jung, T., de Vries, J. E. & Aversa, G. IL-10 alters DC function via modulation of cell surface molecules resulting in impaired T-cell responses. Cell Immunol 215, 162–172 (2002).
Moore, K. W., de Waal Malefyt, R., Coffman, R. L. & O’Garra, A. Interleukin-10 and the interleukin-10 receptor. Annu Rev Immunol 19, 683–765, 10.1146/annurev.immunol.19.1.683 (2001).
Schuetze, N. et al. IL-12 family members: differential kinetics of their TLR4-mediated induction by Salmonella enteritidis and the impact of IL-10 in bone marrow-derived macrophages. Int Immunol 17, 649–659, 10.1093/intimm/dxh247 (2005).
Wang, H. et al. The abnormal apoptosis of T cell subsets and possible involvement of IL-10 in systemic lupus erythematosus. Cell Immunol 235, 117–121, 10.1016/j.cellimm.2005.08.031 (2005).
Ouyang, W., Rutz, S., Crellin, N. K., Valdez, P. A. & Hymowitz, S. G. Regulation and functions of the IL-10 family of cytokines in inflammation and disease. Annu Rev Immunol 29, 71–109, 10.1146/annurev-immunol-031210-101312 (2011).
Levy, Y. & Brouet, J. C. Interleukin-10 prevents spontaneous death of germinal center B cells by induction of the bcl-2 protein. J Clin Invest 93, 424–428, 10.1172/JCI116977 (1994).
Llorente, L. et al. Role of interleukin 10 in the B lymphocyte hyperactivity and autoantibody production of human systemic lupus erythematosus. J Exp Med 181, 839–844 (1995).
Chun, H. Y. et al. Cytokine IL-6 and IL-10 as biomarkers in systemic lupus erythematosus. J Clin Immunol 27, 461–466, 10.1007/s10875-007-9104-0 (2007).
Houssiau, F. A. et al. Serum interleukin 10 titers in systemic lupus erythematosus reflect disease activity. Lupus 4, 393–395 (1995).
Liu, T. F. & Jones, B. M. Impaired production of IL-12 in system lupus erythematosus. II: IL-12 production in vitro is correlated negatively with serum IL-10, positively with serum IFN-gamma and negatively with disease activity in SLE. Cytokine 10, 148–153, 10.1006/cyto.1997.0269 (1998).
Llorente, L. et al. Clinical and biologic effects of anti-interleukin-10 monoclonal antibody administration in systemic lupus erythematosus. Arthritis Rheum 43, 1790–1800, 10.1002/1529-0131(200008)43:8<1790::AID-ANR15>3.0.CO;2-2 (2000).
Ishida, H. et al. Continuous administration of anti-interleukin 10 antibodies delays onset of autoimmunity in NZB/W F1 mice. J Exp Med 179, 305–310 (1994).
Yin, Z. et al. IL-10 regulates murine lupus. J Immunol 169, 2148–2155 (2002).
Blenman, K. R. et al. IL-10 regulation of lupus in the NZM2410 murine model. Lab Invest 86, 1136–1148, 10.1038/labinvest.3700468 (2006).
Zulu, I. et al. Cytokine activation is predictive of mortality in Zambian patients with AIDS-related diarrhoea. BMC Infect Dis 8, 156, 10.1186/1471-2334-8-156 (2008).
Su, D. L., Lu, Z. M., Shen, M. N., Li, X. & Sun, L. Y. Roles of pro- and anti-inflammatory cytokines in the pathogenesis of SLE. J Biomed Biotechnol 2012, 347141, 10.1155/2012/347141 (2012).
Busfield, S. J. et al. Identification and gene organization of three novel members of the IL-1 family on human chromosome 2. Genomics 66, 213–216, 10.1006/geno.2000.6184 (2000).
Kumar, S. et al. Identification and initial characterization of four novel members of the interleukin-1 family. J Biol Chem 275, 10308–10314 (2000).
Smith, D. E. et al. Four new members expand the interleukin-1 superfamily. J Biol Chem 275, 1169–1175 (2000).
Dinarello, C. et al. IL-1 family nomenclature. Nat Immunol 11, 973, 10.1038/ni1110-973 (2010).
Nold, M. F. et al. IL-37 is a fundamental inhibitor of innate immunity. Nat Immunol 11, 1014–1022, 10.1038/ni.1944 (2010).
Boraschi, D. et al. IL-37: a new anti-inflammatory cytokine of the IL-1 family. Eur Cytokine Netw 22, 127–147, 10.1684/ecn.2011.0288 (2011).
Bufler, P., Gamboni-Robertson, F., Azam, T., Kim, S. H. & Dinarello, C. A. Interleukin-1 homologues IL-1F7b and IL-18 contain functional mRNA instability elements within the coding region responsive to lipopolysaccharide. Biochem J 381, 503–510, 10.1042/BJ20040217 (2004).
Sims, J. E. & Smith, D. E. The IL-1 family: regulators of immunity. Nat Rev Immunol 10, 89–102, 10.1038/nri2691 (2010).
Nold-Petry, C. A. et al. IL-37 requires the receptors IL-18Ralpha and IL-1R8 (SIGIRR) to carry out its multifaceted anti-inflammatory program upon innate signal transduction. Nat Immunol 16, 354–365, 10.1038/ni.3103 (2015).
Song, L. et al. Glucocorticoid regulates interleukin-37 in systemic lupus erythematosus. J Clin Immunol 33, 111–117, 10.1007/s10875-012-9791-z (2013).
Liu, Z. & Davidson, A. Taming lupus-a new understanding of pathogenesis is leading to clinical advances. Nat Med 18, 871–882, 10.1038/nm.2752 (2012).
Gelati, M. et al. IL-10 production in multiple sclerosis patients, SLE patients and healthy controls: preliminary findings. Ital J Neurol Sci 18, 191–194 (1997).
Hase, K. et al. Increased CCR4 expression in active systemic lupus erythematosus. J Leukoc Biol 70, 749–755 (2001).
Lacki, J. K., Samborski, W. & Mackiewicz, S. H. Interleukin-10 and interleukin-6 in lupus erythematosus and rheumatoid arthritis, correlations with acute phase proteins. Clin Rheumatol 16, 275–278 (1997).
Mellor-Pita, S. et al. Monocytes and T lymphocytes contribute to a predominance of interleukin 6 and interleukin 10 in systemic lupus erythematosus. Cytometry B Clin Cytom 76, 261–270, 10.1002/cyto.b.20468 (2009).
Park, Y. B. et al. Elevated interleukin-10 levels correlated with disease activity in systemic lupus erythematosus. Clin Exp Rheumatol 16, 283–288 (1998).
Waszczykowska, E. et al. Estimation of SLE activity based on the serum level of chosen cytokines and superoxide radical generation. Mediators Inflamm 8, 93–100, 10.1080/09629359990586 (1999).
Yang, P. T. et al. Increased CCR4 expression on circulating CD4(+) T cells in ankylosing spondylitis, rheumatoid arthritis and systemic lupus erythematosus. Clin Exp Immunol 138, 342–347, 10.1111/j.1365-2249.2004.02617.x (2004).
Koenig, K. F. et al. Serum cytokine profile in patients with active lupus nephritis. Cytokine 60, 410–416, 10.1016/j.cyto.2012.07.004 (2012).
Xu, Q. et al. IL-10 augments antibody production in in vitro immunized lymphocytes by inducing a Th2-type response and B cell maturation. Biosci Biotechnol Biochem 68, 2279–2284, 10.1271/bbb.68.2279 (2004).
Herbst, R., Liu, Z., Jallal, B. & Yao, Y. Biomarkers for systemic lupus erythematosus. Int J Rheum Dis 15, 433–444, 10.1111/j.1756-185X.2012.01764.x (2012).
Visser, J. et al. Differential regulation of interleukin-10 (IL-10) and IL-12 by glucocorticoids in vitro. Blood 91, 4255–4264 (1998).
Mok, M. Y. & Li, W. L. Do Asian patients have worse lupus? Lupus 19, 1384–1390, 10.1177/0961203310375832 (2010).
Hochberg, M. C. Updating the American College of Rheumatology revised criteria for the classification of systemic lupus erythematosus. Arthritis Rheum 40, 1725, 10.1002/1529-0131(199709)40:9<1725::AID-ART29>3.0.CO;2-Y (1997).
Vincent, F. B., Northcott, M., Hoi, A., Mackay, F. & Morand, E. F. Association of serum B cell activating factor from the tumour necrosis factor family (BAFF) and a proliferation-inducing ligand (APRIL) with central nervous system and renal disease in systemic lupus erythematosus. Lupus 22, 873–884, 10.1177/0961203313496302 (2013).
Vincent, F. B., Northcott, M., Hoi, A., Mackay, F. & Morand, E. F. Clinical associations of serum interleukin-17 in systemic lupus erythematosus. Arthritis Res Ther 15, R97, 10.1186/ar4277 (2013).
Gladman, D. D. et al. The Systemic Lupus International Collaborating Clinics/American College of Rheumatology (SLICC/ACR) Damage Index for Systemic Lupus Erythematosus International Comparison. J Rheumatol 27, 373–376 (2000).
Nikpour, M., Urowitz, M. B., Ibanez, D. & Gladman, D. D. Frequency and determinants of flare and persistently active disease in systemic lupus erythematosus. Arthritis Rheum 61, 1152–1158, 10.1002/art.24741 (2009).
Ibanez, D., Gladman, D. D. & Urowitz, M. B. Adjusted mean Systemic Lupus Erythematosus Disease Activity Index-2K is a predictor of outcome in SLE. J Rheumatol 32, 824–827 (2005).
Gladman, D. D., Ibanez, D. & Urowitz, M. B. Systemic lupus erythematosus disease activity index 2000. J Rheumatol 29, 288–291 (2002).
Acknowledgements
This work was supported in part by grants from the National Health and Medical Research Council (NHMRC) of Australia (1068040) and the Rebecca L. Cooper Medical Research Foundation.
Author information
Authors and Affiliations
Contributions
J.G., E.F.M., R.K.-R. and J.H. wrote the main manuscript text. J.G. and I.R. conducted experiments and J.G. and R.K.-R. analyzed data and prepared all figures. A.H. coordinated patient sample and longitudinal data collection. M.F.N., E.F.M. and J.H. supervised the project. All authors reviewed the manuscript.
Ethics declarations
Competing interests
The authors declare no competing financial interests.
Electronic supplementary material
Rights and permissions
This work is licensed under a Creative Commons Attribution 4.0 International License. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in the credit line; if the material is not included under the Creative Commons license, users will need to obtain permission from the license holder to reproduce the material. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/
About this article
Cite this article
Godsell, J., Rudloff, I., Kandane-Rathnayake, R. et al. Clinical associations of IL-10 and IL-37 in systemic lupus erythematosus. Sci Rep 6, 34604 (2016). https://doi.org/10.1038/srep34604
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/srep34604
This article is cited by
-
Utility of peripheral blood monocyte subsets, circulating immune complexes and serum cytokines in assessment of SLE activity: an observational, cross-sectional study
Clinical Rheumatology (2024)
-
CD19+CD24highCD27+ B cell and interleukin 35 as potential biomarkers of disease activity in systemic lupus erythematosus patients
Advances in Rheumatology (2022)
-
Assessing the expression of immunosuppressive cytokines in the newly diagnosed systemic lupus Erythematosus patients: a focus on B cells
BMC Immunology (2020)
-
High interleukin-18 and low FOXP3 mRNAs in peripheral blood of women with severe systemic lupus erythematosus: a cross-sectional study
Rheumatology International (2020)
-
Rare variants in non-coding regulatory regions of the genome that affect gene expression in systemic lupus erythematosus
Scientific Reports (2019)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.