Abstract
The objective was to develop and characterise in vitro Bartonella bacilliformis antibiotic resistant mutants. Three B. bacilliformis strains were plated 35 or 40 times with azithromycin, chloramphenicol, ciprofloxacin or rifampicin discs. Resistance-stability was assessed performing 5 serial passages without antibiotic pressure. MICs were determined with/without Phe-Arg-β-Napthylamide and artesunate. Target alterations were screened in the 23S rRNA, rplD, rplV, gyrA, gyrB, parC, parE and rpoB genes. Chloramphenicol and ciprofloxacin resistance were the most difficult and easiest (>37.3 and 10.6 passages) to be selected, respectively. All mutants but one selected with chloramphenicol achieved high resistance levels. All rifampicin, one azithromycin and one ciprofloxacin mutants did not totally revert when cultured without antibiotic pressure. Azithromycin resistance was related to L4 substitutions Gln-66 → Lys or Gly-70 → Arg; L4 deletion Δ62–65 (Lys-Met-Tyr-Lys) or L22 insertion 83::Val-Ser-Glu-Ala-His-Val-Gly-Lys-Ser; in two chloramphenicol-resistant mutants the 23S rRNA mutation G2372A was detected. GyrA Ala-91 → Val and Asp-95 → Gly and GyrB Glu474 → Lys were detected in ciprofloxacin-resistant mutants. RpoB substitutions Gln-527 → Arg, His-540 → Tyr and Ser-545 → Phe plus Ser-588 → Tyr were detected in rifampicin-resistant mutants. In 5 mutants the effect of efflux pumps on resistance was observed. Antibiotic resistance was mainly related to target mutations and overexpression of efflux pumps, which might underlie microbiological failures during treatments.
Similar content being viewed by others
Introduction
Bartonella bacilliformis is the causative agent of Carrion’s disease, a biphasic endemic illness of the Andean valleys. In the acute stage (the so-called Oroya fever) severe haemolytic anaemia is present, resulting in 40–85% of deaths in untreated people and decreases to around 10% if correctly treated1,2,3. In this stage the presence of concomitant infections such as bloodstream Salmonella infections, among others1,4,5,6, are frequent due to the temporal immunosuppression induced by B. bacilliformis7.
Peruvian wart is the chronic non life-threatening phase, characterised by cutaneous proliferative vascular lesions, occurring some weeks or months after the acute infection3.
Additionally, the number of asymptomatic carriers is uncertain, although some studies have shown that 45% of the inhabitants of endemic areas present evidence of previous contact with the pathogen8.
The usual treatments are chloramphenicol (CHL) or ciprofloxacin (CIP), alone or combined with cephalosporins or aminoglycosides in for the acute stage. Rifampicin (RIF) or azithromycin (AZM) are used in the chronic stage6,9. Despite the reported ~10% of deaths among patients receiving adequate treatment3, it is widely considered that this microorganism has good clinical response to the above mentioned treatments.
The use of antibacterial agents in the treatment of Carrion’s disease has been profuse in recent decades10. Moreover, in asymptomatic carriers the microorganisms are also under antibiotic pressure related to the treatment of other infections. However, descriptions of antibiotic-resistant B. bacilliformis clinical isolates are scarce11,12. To date, only constitutive nalidixic acid resistance and related diminished fluoroquinolone susceptibility have been reported in association with the presence of an Ala as WT amino acids at positions 91 and 85 of GyrA and ParC, respectively13,14. These characteristics are extended to other members of the Bartonella genus13. Additionally, relatively high Minimal Inhibitory Concentration (MIC) levels of clindamycin and colistin12, have been observed as well as sporadic isolates presenting resistance to CHL or CIP and a trend towards diminished susceptibility to aminoglycosides11,16. Moreover, in vitro resistance to different antimicrobial agents, including coumermycin, CIP, RIF and erythromycin, has been described17,18,19. However, these studies were developed using either the KC583 or KC584 strain alone, being limited to the analysis of point mutations, and to date, no study has determined the role of efflux pump overexpression or the stability of the antibiotic resistance selected.
Analysis of in vitro obtained mutants may provide information in order to better understand antibiotic-resistance acquisition and evolution. The aim of this study was to develop and characterise a series of in vitro B. bacilliformis antibiotic resistant mutants and determine the presence of target mutations, the role of efflux pumps as well as the stability of selected resistance.
Results
Development of antibiotic-resistant mutants
The time required for bacterial lyophilised reactivation varied from 5 weeks (strains 57.19 and 57.20) to 9 weeks (strain 57.18). Interestingly, strain 57.18 showed an initially different morphology, coinciding with the previously described T1 morphology20, although this reverted in the next passage (Fig. 1).
The photograph shows B. bacilliformis presenting T1 colony morphology20. The colony is characterised by a small, translucent round morphology, with a regular edge and a small halo. The colonies present a “bubble” in the center of the colony. The morphology was unstable and disappeared after reculture.
The development of the antibiotic-resistant mutants required approximately 18 months, therefore, 4 antibiotic-resistant mutants were obtained from each parental strain, one for each antibiotic included in the study.
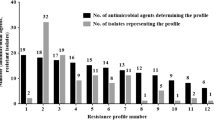
The first antibiotic to generate inhibitory halo 0 mm was RIF, with only 4 passages to obtain confluent growth (strain 57.19). However, overall, the antibiotic requiring the least number of passages to generate confluent growth was CIP with a mean of 10.6 passages. On the other hand, CHL required >37.3 passages (Table 1). Thin growth was observed inside the halo recorded during the process of mutant selection of 57.20Azm. Thus, after the initial 35 passages, most antibiotic-resistant mutants showed confluent growth in the presence of the antibiotic disc (inhibitory halo 0 mm) except for two out of three mutants selected with CHL, which presented inhibitory halos of 18 mm (57.18Chl-35) and 32 mm (57.20Chl-35). After 5 additional serial passages (total: 40 passages), 57.20Chl-40 achieved a halo of 0 mm, while 57.18Chl-40 remained with an inhibitory halo of 18 mm (Fig. 2).
(A) Azithromycin, (B) Chloramphenicol, (C) Ciprofloxacin, (D) Rifampicin. This figure demonstrates the ease with each mutant are selected for each antibiotic. The halo diameters (measured in mm) are reported every 5 passages or at the passage in which halo zero was obtained. In (B) is clearly visualised the difficulty with which resistance to chloramphenicol (CHL) is developed.
Analysis of MIC levels and stability of resistance
A maximum of 1 dilution difference between the MICs at 7 and 14 days was observed. Thus, those obtained at 7 days were used throughout the manuscript.
Analysis of the MIC levels showed that all but 1 mutant achieved MICs up to the E-test detection limit >256 mg/L (AZM, RIF and CHL) and >32 mg/L (CIP). The exception was the above mentioned 57.18Chl-40 mutant that reached a CHL MIC level of 4 mg/L (Table 2).
Interestingly, analysis of the stability of the resistance obtained showed that all RIF selected mutants were stable, as were 57.18Azm-5St and 57.18Cip-5St. Two strains (57.18Chl-5St and 57.19Chl-5St) returned to the parental MIC levels, while the remaining isolates showed intermediate MICs between parental and final mutant values. In the case of mutants 57.19Azm-5St and 57.20Cip-5St at 14 days the presence of colonies within the inhibitory halo were observed. Thus, 57.19Azm-5St-WH showed a MIC of AZM of 32 mg/L while 57.20Cip-5St-WH showed a MIC > 32 mg/L for CIP (Table 2).
Antibiotic cross resistance
When the mutants were selected with AZM the MICs to other antibiotics generally increased, while the selection with CHL usually resulted in decreases in other MICs, and in those selected with CIP and RIF the results were more variable (Tables 2 and 3).
Target mutations
None of the genes of the parental strains analysed presented differences with respect those of the KC583 strain except the amino acid codon change Thr-13 → Ala at L4 protein and Arg-9 → Cys at L22 protein.
AZM resistance was related to the presence of alterations in the rplD and rplV genes, encoding the L4 and L22 proteins, respectively. No mutation was observed in the 23S rRNA gene. Thus 57.18Azm and 57.18Azm-5st showed a predicted 4 amino acid deletion (Lys-Met-Tyr-Lys) at L4 protein from codons 62 to 65 (Δ62–65). Nonetheless, close analysis of the spherogram showed the presence of a double sequence from the deletion onwards under the majority peaks with in the reading-frame together with a non-deleting rplD (Supplementary Figure 1). Meanwhile, in mutants 57.19Azm-35 and 57.19Azm-5st we observed the presence of the L4 amino acid codon change Gly-70 → Arg, with a change His-74 → Tyr also being observed in 57.19Azm-5st-WH. The mutant 57.20Azm showed the presence of alterations at both the rplD and rplV genes. Thus, the presence of an amino acid codon change Gln-66 → Lys was observed in the rplD gene, while a 27 base-pair insertion (leading to the 9 amino acid Val-Ser-Glu-Ala-His-Val-Gly-Lys-Ser) was observed at one of the two rplD B. bacilliformis genes after position 83 (Supplementary Figure 1). Interestingly the 57.20Azm-5St rplD gene showed a double peak which presented a mixed population with a partial reversion of the change Gln-66 → Lys.
Regarding quinolone resistance, no mutation was observed in the Topoisomerase IV encoding genes (parC and parE). A GyrA amino acid substitution was observed in 2 out of 3 selected mutants, 57.18Cip-35 and 57.20Cip-35 (Ala-91 → Val and Asp-95 → Gly, respectively), and a GyrB amino acid substitution (Glu-475 → Lys) was observed in 57.19Cip-35. The mutations present in 57.18Cip-35 and 57.19Cip-35 were stable and were also observed in the mutants 57.18Cip-5St, and 57.19Cip-5St. In the case of 57.20Cip-35 the analysis of the sequence spherogram showed the presence of a double peak with two bacterial populations, one with the WT gyrA gene sequence and other possessing the aforementioned amino acid codon substitution. This was confirmed by analysing 57.20Cip-5St (possessing a WT gyrA gene sequence) and 57.20Cip-5St-WH (which maintained the amino acid change Asp-95 → Gly). The in silico determination of the hydrophobicity pattern showed an alteration in the presence of GyrA Val-91, while the presence of GyrA Asn-95 altered both the charge and slightly affected the hydrophobicity pattern (Fig. 3).
(A) Alterations in the hydrophobic pattern. Additionally to the amino acid substitutions detected (Ala-91 → Val and Asp-95 → Gly) the theoretical effect of the presence of Ser-91 also shows the gradual effect on the hydrophobic pattern related to the presence of Ser, Ala or Val at position 91. (B) Effect on the charge pattern. This graph only shows the effect of Asp-95 and Gly-95 since the presence of Val-91 does not result in charge pattern alterations. The (A) comprises the amino acid sequence from amino acids 84 to 99, while in (B) the amino acid sequences analysed are from amino acids 70 to 107.
In the 57.19Chl-35 mutant an alteration in the 23S rRNA gene (G2372A) was detected, which reverted after 5 passages without antibiotic pressure. The same mutation was also observed in the 57.20Chl-40 mutant, but a double peak was observed showing the presence of a double bacterial population, or, more probably, that the mutation was only present in one of the two 23S rRNA genes of the B. bacilliformis genome (Supplementary Figure 1).
Finally, the presence of mutations in the rpoB gene was observed in all RIF-selected mutants which were also present after the 5 passages without antibiotic pressure, leading to the amino acid changes Gln-527 → Arg (57.18Rif-35, 57.18Rif-5St), His-540 → Tyr (57.19Rif-35, 57.19Rif-5St) and Ser-545 → Phe plus Ser-588 → Tyr (57.20Rif-35 and 57.20Rif-5St). Interestingly, when the rpoB gene in the 57.20 RIF-derived mutant at passage 13 (57.20Rif-13), was sequenced, only the presence of the amino acid codon change Ser-588 → Tyr was observed.
Effect of Efflux Pumps Inhibitors (EPIs)
The study of the effect of Phe-Arg-β-Napthylamide (PAβN) and artesunate (ART) on normal bacterial growth showed that high PAβN concentrations (7.5, 10, 20 mg/L) allowed bacterial, albeit non normal, growth. Thus, a concentration of 5 mg/L was used in the assays. No effect of ART was observed on bacterial growth with 20 mg/L. Additionally, we confirmed the lack of effect on bacterial growth with ethanol at the concentration and required volume used.
Both PAβN and ART had a visible effect on the CHL MIC of 57.18Chl-40, and this effect was also confirmed by the increased disc inhibitory halo in the presence of both EPIs. Both EPIs also affected the AZM susceptibility levels of the 57.18Azm-35 mutant. Additionally, ART was found to affect the RIF MIC of 57.19Rif-35, and also enhanced the activity of RIF and CIP in 57.20Cip-35 and 57.20Rif-35 mutants respectively (Tables 2 and 4).
Discussion
Currently antimicrobial resistance levels have only been established in a few B. bacilliformis clinical or collection isolates11,12,14,15,16. Information about the mechanisms of antibiotic resistance exhibited by these isolates is very scarce and strictly focused on constitutive quinolone resistance13,14,15. This lack of data, together with the high percentage of clinical cure without microbiological elimination described in more than 22% of CIP and up to 50% of CHL treatments as well as the high-lethality related to the acute illness phase in the absence or delay of treatment2,3,21, highlight the need for in vitro information about the ease with which this microorganism develops resistance and which antibiotic resistance mechanisms are selected. To the best of our knowledge only three in vitro studies has been developed to date17,18,19, and none has determined the stability of the antibiotic resistance selected or the role of efflux pump overexpression.
Although the 57.19 strain only needed 4 consecutive passages to develop full resistance to RIF, overall, the antibiotic which most easily selected resistant mutants was CIP. This is in accordance with the possession of Ala-91 and Ala-85 of GyrA and ParC respectively which affect the hydrophobicity pattern of these proteins, impairing the interaction of quinolones and acting as a factor favouring the selection of resistance to fluoroquinolones14,22. In fact, it has been shown that the frequency of mutation of B. bacilliformis KC583 was 10-fold higher than that of Escherichia coli, while only 5 passages were needed to select high CIP-resistant mutants from strain KC58418,19. Regarding RIF and AZM, full resistance was obtained after 3 and 4 passages respectively18. There are no previous reports on the selection of Bartonella spp. CHL-resistant mutants. In our study, resistance to CHL was consistently the most difficult to obtain. Although this finding is in apparent disagreement with the observed 50% of persistent bacteraemia after CHL treatments21, it might be related to changes at the fitness level as has been observed in the presence of specific 23S rRNA gene point mutations in other microorganisms23,24,25.
The MIC of the mutants selected was higher than that of the parental isolates, achieving high MICs levels with all the antibacterial agents tested. This finding shows a worrisome scenario: the feasibility of selecting high antibiotic resistant mutants with the 4 main antibiotic families used in the treatment of Carrion’s disease. However, only those mutants selected with RIF showed consistent resistance stability, while only 1 out of 3 of CIP or AZM-resistant mutants did not revert either totally or partially. Regarding CHL, all the resistant mutants selected reverted, supporting the idea of a high biological cost of the development of CHL resistance. In the same line, the presence of double sequences when analysing some of antibiotic target gene sequences may be interpreted in three different ways: The survival of original susceptible parental strains, the partial reversion of the mutants obtained when antibiotic pressure disappears or the presence of mutations in only one of the gene copies when there is more than one. The first possibility is unlikely because of the high susceptibility levels of the parental strains to all the antibacterial agents tested (halo diameter >100 mm) which prevent the survival of the microorganisms when the disc was placed on the center of the plate (the maximum possible halo diameter is 50 mm). Meanwhile the other two possibilities may be considered, and, moreover, are not mutually exclusive. They might underlie the high number of microbiological failures, isolation of viable microorganisms from blood, after successful clinical treatments21. Moreover, the reversion observed in the 57.20Azm-35 mutant may be related to the slower growth described in association with L4 and L22 alterations26. Along this line, the reversion of resistance, the presence of double bacteria populations in at least two mutants (one selected with CIP and other with AZM) as well as the additional time needed by some of the resistant strains (57.19Azm-5St-WH, 57.20Cip-5st-WH) to grow, support the idea that the development of antibiotic resistance has a high biological cost in B. bacilliformis, resulting in the dilution of strains carrying specific antibiotic-related mutations within a general antibiotic susceptible bacterial population. Similarly, both the loss of biological efficiency and the decrement of virulence after the development of antimicrobial resistance have been observed in other microorganisms27,28. However, compensatory mutations might result in the development and spread of resistant isolates27,29.
Although non-uniform, cross effects, either increases or decreases, in the MIC levels were observed. These alterations might be explained by collateral antibiotic resistance effects that could interfere with normal bacteria biochemical processes. Three of antibacterial agents tested act at a ribosome level, while the remaining agent acts at the proteins involved in DNA decatenation and duplication. Ribosomal level alterations may differentially affect the expression of genes or may have a direct effect on the activity of other agents. In other microorganisms, specific points placed in 23S rRNA and in the ribosomal proteins may result in concomitant resistance between CHL and macrolides30,31. Among these, it has been suggested that L4 deletions Δ65–66 (Trp-Arg) and Δ68–69 (Lys-Gly) leading to macrolide-resistance in Streptococcus pneumoniae also confres low levels of CHL resistance. Thus, S. pneumoniae L4 Δ65–66 has been associated with an increase of the CHL MIC of up to 4-fold when cloned in a pan-susceptible S. pneumoniae strain31. Amino acid codons 65 and 66 of S. pneumoniae are equivalent to positions 64 and 65 of B. bacilliformis, both included within the Δ62–65 of 57.18Azm-35 mutant. Thus, the role of L4 deletions in the acquisition of the low levels of CHL resistance observed in this mutant (MIC 2 mg/L, 5.26-fold increases) is plausible, either directly due to alterations in the ribosome conformation affecting CHL binding or indirectly due to the possible induction of efflux pump overexpression as discussed below. This fact highlights the risk of co-selection of antibiotic resistance during B. bacilliformis treatment.
On the other hand, selection of CHL seems to negatively affect the ability of bacteria to survive in the presence of other antibiotic agents. This fact may also be related to the above mentioned possible effect on fitness, being probably underlain by alterations in the expression or regulation of different bacterial genetic factors. Additionally, selection of hypersusceptibility to unrelated antibiotics, such as macrolides, has also been observed in relation to specific 23S rRNA mutations32.
Two differences leading to the substitutions Thr-13 → Ala at L4 and Arg-9 → Cys at L22, were observed between the parental and KC583 strains. Nonetheless, both substitutions were present in other B. bacilliformis genomes. This finding, together with the high antibiotic susceptibility of the parental isolates, suggests the presence of DNA polymorphisms.
Regarding AZM resistance, in all the cases the presence of alterations at L4 and L22 was found, while no mutation at 23S rRNA was observed. This latter finding differs from that described in microorganisms with a low number of 23S rRNA gene copies33 and observed in previous studies developed in B. bacilliformis and Bartonella henselae18,34,35.
Amino acid changes at L4 and L22, including insertions and deletions, have been described in a series of unrelated microorganisms, such as E. coli26,36,37. Regarding Bartonellaceae, the mutations at L4 (Gly-70 → Arg and Gly-70 → Arg + His-74 → Tyr) have been previously described in in vitro obtained macrolide-resistant mutants of B. henselae35. In E. coli, a series of amino acid changes involving the L4 residues Gln-62 and Gly-66 equivalent to B. bacilliformis Gln-66 and Gly-70 have been reported as being involved in the development of AZM resistance26,36. Interestingly, in E. coli substitutions at position Ser-70 (equivalent to B. bacilliformis His-74) have been described36, but never alone, as reported by Biswas et al.34, suggesting a minor role of this substitution in the development of macrolide resistance.
This is the first report describing insertions and deletions in the L4 and L22 proteins of B. bacilliformis. The predicted L4 deletion is located close to the L4 “hot spot” region involved in macrolide resistance in which a deletion of the 2 equivalent later amino acids in macrolide-resistant S. pneumoniae has been reported31, while to the best of our knowledge no insertion has been described in equivalent positions in other microorganisms.
Two out of three CHL-resistant mutants (57.19Chl-35 and 57.20Chl-40) presented a G2372A mutation in the 23S rRNA gene. The equivalent mutation has previously been involved in CHL resistance in yeasts and E. coli25,38. Although in the case of the 57.20Chl-40 mutant double peaks were obtained suggesting either the presence of a double bacterial population, or, more probably, the presence of a mutation affecting only one of the two 23S rRNA genes. This fact, together with the rapid reversion of this mutation and the slow bacterial growth, which might be longer than 2 months in clinical samples cultures10,39, might explain the presence of microbiological failures after CHL treatments, contributing to the lack of reports of CHL resistance in clinical isolates. Supporting the biological cost of the development of CHL resistance, the equivalent G2447A mutation in E. coli results in both resistance to CHL and in retarded growth rates25.
The amino acid alterations observed in two out of three GyrA were located in the classical quinolone-DNA Gyrase interaction points, while resistance in the third isolate was related to the presence of mutations in the gyrB gene. Up to now, no amino acid change at GyrA position 91 has been described in B. bacilliformis. However, alterations at equivalent GyrA position have been extensively described in other quinolone-resistant microorganisms22, including the presence of Val-91, detected both in B. henselae and unrelated microorganisms22,34,40. The presence of an Ala in position 83 of the GyrA of E. coli (equivalent to 91 of B. bacilliformis) results in a decreased CIP MIC, and intermediate or low-level of nalidixic resistance40,41,42, while the presence of Val results in full fluoroquinolone-resistance as well as in high levels of resistance of nalidixic acid40. These findings may be directly related to the different effect on the GyrA hydrophobicity pattern and the subsequent involvement of the ability of quinolones to bind with their targets in relation to the presence of Ser (WT amino acid in E. coli and most other microorganisms) Ala or Val residues, as shown in Fig. 3.
Changes at position Asp-95, including Asp-95 → Gly, have been previously described in studies analysing quinolone-resistant mutants of B. bacilliformis, B. henselae and Bartonella quintana18,19,43. Changes at equivalent position have frequently been reported in other microorganisms22,40. The effect of different mutations is additive22, thus, in the absence of the effect on bacterial fitness, it would be more successful to add a change in a new position than to vary the amino acid at position 91. The presence of Gly at position 95 slightly affects the hydrophobicity pattern, but mainly affects the pattern of charges at this area, avoiding the interaction with radical 7 of the quinolones44.
This is the first description of a GyrB amino acid substitution Glu-475 → Lys in B. bacilliformis. The same amino acid change at the equivalent position of S. pneumoniae (Glu-474) has been associated with quinolone resistance45. Moreover, in S. pneumoniae a series of amino acid changes including Glu-476 → Ala and Arg-477 → His has also been described in the same region, showing the relevance of the GyrB region in the development of quinolone-resistance46,47. The 57.19Cip-5St mutant showed a MIC of 1.5 mg/L (3.95-fold higher than its parental isolate). Thus, by itself the Glu-475 → Lys alteration results in a slight increase in the CIP MIC. Moreover, this finding, together with the lack of PAβN and ART effect on the CIP MIC, highlight the presence of unstable mechanism/s of resistance in the 57.19Cip-35 mutant.
Rifamycin-resistant rpoB gene mutations are usually located within 3 highly conserved regions in the mid portion of the gene. In E. coli these regions include codons 505–537 (cluster I), 563–575 (cluster II) and 684–690 (cluster III)48,49. In the present study, the amino acid codon changes Gln-527 → Arg; His-540 → Tyr; Ser-545 → Phe are located within the B. bacilliformis equivalent cluster I, while Ser-588 → Tyr is located within the equivalent cluster II. Of these, the amino acid change Ser-545-Phe has been previously observed in B. bacilliformis and B. quintana in vitro RIF-resistant mutants18. However, substitutions at equivalent amino acid positions have been observed as being involved in the development of rifamycin resistance in other microorganisms including Mycobacterium tuberculosis50. Thus, in E. coli RpoB substitutions of Gln-513, His-526, Ser-531 or Ser-574 (equivalents to Gln-527, His-540, Ser-545 and Ser-588 of B. bacilliformis respectively) have been described; moreover, in some cases the same amino acid change (e.g. Ser-531 → Phe or His-526 → Tyr) has also been reported43,51,52. In one case (57.20Rif-35) a double mutation (Ser-545 → Phe plus Ser-588 → Tyr) was observed. However, when the presence of an RpoB alteration was sought in 57.20Rif at passage 13, only the presence of the amino acid change Ser-588 → Tyr was observed. This fact shows the sequential selection of RIF resistance related to continuous antibiotic pressure. In E. coli the substitution at Ser-574 (equivalent to Ser-588) results in low-levels of RIF resistance, being its effect strongly diminished in the presence of PAβN51. Thus, the selection of a mutation conferring low RIF resistance levels is followed by that of another additive mechanism of resistance, leading to an increase in the RIF resistance levels. Similarly, although substitutions at the equivalent Ser-545 position seem to result in high RIF MIC levels in E. coli49, in other microorganisms such as Rhodococcus equi only low levels of RIF resistance are conferred53.
This is the first determination of the role of efflux pumps in the development of antibiotic resistance in B. bacilliformis. The two EPI tested act differently, while PAβN competes with other efflux pump substrates to be extruded from bacteria, ART diminishes the expression levels of some efflux pump encoding genes54,55. These differences may underlie the disparity of results obtained in the present study with these inhibitors.
Both PAβN and ART affected the susceptibility levels of 57.18Azm-35 and 57.18Chl-40 mutants. In the first case the mutant presented L4 Δ62–65. Although related to deletions in L22, a similar scenario has been observed in E. coli strains carrying 3 amino acid deletions in L22 in which the inactivation of different efflux pump components results in a strong decrease in the erythromycin MIC levels56. Thus, it has been proposed that deletions at L22 alter the translation of specific proteins, possibly via changes in programmed stalling, modifying the cell envelope and resulting in efflux pump overexpression and lowering steady-state macrolide levels56. It is of interest to note that in 57.18Azm-35, the use of PAβN was only visible in the disc diffusion analysis. The most probable scenario for this is that the MIC of this strain is much higher than 256 mg/L and thus, the effect on the MIC levels, albeit present, was not observed. Regarding the 57.18Chl-40 mutant both the effect of PAβN and ART decreased the CHL MIC levels to only slightly higher than the parental isolate, showing that efflux pumps may play a role in the development of low levels of CHL resistance in B. bacilliformis. No effect was observed with any inhibitor tested in either 57.19Chl-35 or 57.20Chl-40. This finding, together with the effect of ART on the antimicrobial susceptibility levels of all remaining 57.20 derivative mutants, highlight two facts: (a) the high levels of resistance to CHL derived from the presence of 23S rRNA mutations which when present mask the effect of efflux pumps, and (b) the presence of efflux pumps able to extrude the 4 antimicrobial families tested in B. bacilliformis. Thus, the different level of antimicrobial resistance of each selected mechanism may allow or not visualization of the overexpression of efflux pumps and might underlie the differences in the effect of ART on the RIF-selected mutants. ART also affects the susceptibility to RIF in 57.19Rif-35 and 57.20Rif-35 mutants, showing that efflux pumps may also affect this antibiotic in B. bacilliformis and reinforcing the possibility that the selection of a double RpoB substitution in the 57.20Rif-35 mutant was due to the low level of RIF resistance conferred. In the case of the 57.19Rif-35 mutant the effect was only observed on the MIC levels, while in the case of 57.20Rif-35 the effect was observed in the disc diameter halo. Further studies are needed to determine the mechanisms of efflux pump overexpression (alterations in signal patterns, punctual mutations in promoter regions, among others).
In summary, the present data highlight the ability of B. bacilliformis to become antibiotic resistant both by the development of antibiotic-target alterations, but also mediated by efflux pump overexpression. However, regarding AZM, CHL and CIP, the instability of resistance detected in different mutants, either related to reversions and/or to dilution within a higher fitness susceptible population, suggests a high biological cost, which may underlie the rarity of antibiotic-resistant B. bacilliformis clinical isolates. Further studies analysing antibiotic target sequences from a relevant number of B. bacilliformis clinical isolates prior, during and after antibiotic treatment are necessary to better understand the natural history of antibiotic resistance in this microorganism.
Methods
Microorganisms
Three B. bacilliformis strains from the Institute Pasteur (Paris, France) collection were used (Table 5). The strains were reactivated following the instructions of the Institute Pasteur. Briefly, after opening, 0.2 ml of LB was added to the vial to resuspend the bacteria. Thereafter, the suspension was spread onto Columbia blood agar (Ref: 254005, BD, Heidelberg, Germany) and incubated at 28 °C. The plates were inspected weekly until bacterial growth was observed. Prior to the development of the antibiotic resistant mutants, the bacterial identity of all three isolates was confirmed by amplification and sequencing of the 16S rRNA gene (Table 6)59.
In vitro development of resistant mutants
The antibiotic resistant mutants were selected by plating the B. bacilliformis on blood agar with a disc of AZM (15 μg), CIP (5 μg), CHL (30 μg) or RIF (30 μg) (BD, Franklin Lakes, USA) which was initially put in the corner of each plate, and subsequently in the center of the plate according to halo diameter18. The confluent growth outside the zone of inhibition was recovered with a pre-sterilized plastic inoculation loop and subcultured 35 consecutive times. In those cases in which no halo zero was obtained, the isolates were grown in the presence of antibiotic for 5 additional passages.
At the beginning of the study, the passages with the selected antibiotic discs were performed every other week because of the difficulty to visualise the bacterial growth in the first weeks due the large halo sizes. Then, we changed to a weekly basis, according to the evolution of each strain.
Throughout the text, the mutants obtained are referred to by indicating the name of the parental isolate, the antibiotic used in its selection and the passage number (e.g.: 57.18Azm-35 is the AZM resistant mutant derived from strain 57.18 at passage 35).
Stability of resistance
Resistance stability was assessed by doing 5 final additional passages on Columbia blood agar, on a weekly basis, in the absence of antibiotic pressure. These are referred to in the text following the above mentioned nomenclature but including “5st” (5 serial passages to determine stability instead of passage number). When a mixed bacterial population was obtained (e.g.: growth of isolated colonies inside the inhibitory halo), isolates from inside of halo were additionally marked as “WH” (within halo).
Antibiotic susceptibility levels
The MICs of AZM, CIP, CHL and RIF of the parental isolates, the mutants at the final passage and after the 5 additional passages without antibiotic were determined by E-test (Liofilchem, IZASA, Barcelona, Spain). The MICs were read at 7 and 14 days. To determine the effect on the MIC levels the quotient MICF (final MIC)/MICI (initial MIC) was used. In all cases MIC differences >2-fold were considered as significant.
Antibiotic cross resistance
In the final passage in the presence of antibiotic discs, antibiotic cross resistance was determined by testing the MIC of each mutant with all the other antibiotics under study.
DNA extraction
B. bacilliformis were collected by adding sterile PBS into the plates and suspending the colonies with a one-use loop. This bacterial suspension was transferred to a sterile vial and the DNA was extruded by boiling at 100 °C for 10 minutes and stored at −20 °C until use.
Target mutation detection
The presence of mutations in the rplV and rplD genes (AZM) as well as in the 23S rRNA (AZM and CHL), quinolone resistance-determining regions (QRDR) of the gyrA, gyrB, parC and parE genes (CIP) and the rpoB gene (RIF) were determined by PCR using the primers and conditions listed in Table 6. The PCR products were purified using a commercial kit according to the manufacturer’s instructions (Gel Extraction Kit from Omega Bio-tek, Georgia, USA) and thereafter sequenced (Beckman Coulter, Takeley, United Kingdom). The sequences obtained were compared with those of their respective parental strains and with that of the type strain KC583 (http://www.bacterio.net/bartonella.html). In cases in which the presence of non-silent mutations was observed, the deduced amino acid sequence was compared against B. bacilliformis amino acid sequences present in GenBank. Regarding GyrA, hydrophobicity was determined using the method of Kyte and Doolittle as defined in the ProtScale software60,61, while the polarity pattern was determined using the charge software (http://www.bioinformatics.nl/cgi-bin/emboss/charge).
Throughout the text, both the DNA and amino acid numeration is referred to as that of B. bacilliformis KC583. When DNA or amino acid positions of other microorganisms are used for comparison purposes this is explicitly indicated.
Role of Efflux Pumps
The role of efflux pumps in the development of antibiotic resistance was established by determining the antibiotic susceptibility levels by disc diffusion and E-test in commercial blood agar media supplemented in house with PAβN, or ART. In order to determine the EPI concentrations to be used, the effect of different concentrations of these products (from 2.5 mg/L to 20 mg/L) on normal bacterial growth was tested. Additionally, the effect of 100% ethanol (ART solvent) was also independently assessed.
Additional Information
How to cite this article: Gomes, C. et al. Development and characterisation of highly antibiotic resistant Bartonella bacilliformis mutants. Sci. Rep. 6, 33584; doi: 10.1038/srep33584 (2016).
References
Angelakis, E. & Raoult, D. Pathogenicity and treatment of Bartonella infections. Int. J. Antimicrob. Agents 44, 16–25 (2014).
Ilher, G. M. Bartonella bacilliformis: dangerous pathogen slowly emerging from deep background. FEMS Microbiol. Lett. 144, 1–11 (1996).
Minnick, M. F. et al. Oroya fever and verruga peruana: bartonelloses unique to South America. PLoS Negl Trop Dis 8, e2919 (2014).
Huerta, A., Salas, M., Yarinsueca, J. & Maguiña, C. Enfermedad de Carrión grave complicada con leptospirosis aguda: reporte de un caso. Rev. Peru. Med. Exp. Salud Publ. 31, 380–384 (2014).
Maguiña, C., García, P. J., Gotuzzo, E., Cordero, L. & Spach, D. H. Bartonellosis (Carrión’s Disease) in the modern era. Clin. Infect. Dis. 33, 772–779 (2001).
Tarazona, A., Maguiña, C., Lopez de Guimaraes, D., Montoya, M. & Pachas, P. Terapia antibiótica para el manejo de la Bartonelosis o Enfermedad de Carrión en el Perú. Rev. Peru. Med. Exp. Salud Publ. 23, 188–200 (2006).
Ticona, E., Huaroto, L., Garcia, Y., Vargas, L. & Madariaga, M. G. The pathophysiology of the acute phase of human bartonellosis resembles AIDS. Med. Hypotheses 74, 45–49 (2010).
Chamberlin, J. et al. Epidemiology of endemic Bartonella bacilliformis: a prospective cohort study in a Peruvian mountain valley community. J. Infect. Dis. 186, 983–990 (2002).
Sanchez Clemente, N. et al. Bartonella bacilliformis: a systematic review of the literature to guide the research agenda for elimination PLoS Negl. Trop. Dis. 6, e1819 (2012).
Pachas, P. E. Enfermedad de Carrión (Bartonelosis) en el Perú. Lima (Peru). Ministerio de Salud, (2001). Available at: http://bvs.minsa.gob.pe/local/ogei/790_ms-oge110.pdf (accessed: 19 April, 2016).
Silva-Caso, W., Pons, M. J., Ruiz, J. & del Valle Mendoza, J. Antibiotic resistance in Bartonella bacilliformis clinical isolates from endemic area of Peru. J. Global Antimicrob. Resist. 3, 222–223 (2015).
Sobraques, M., Maurin, M., Birtles, R. J. & Raoult, D. In vitro susceptibilities of four Bartonella bacilliformis strains to 30 antibiotic compounds. Antimicrob. Agents Chemother. 43, 2090–2092 (1999).
Angelakis, E., Biswas, S., Taylor, C., Raoult, D. & Rolain, J. M. Heterogeneity of susceptibility to fluoroquinolones in Bartonella isolates from Australia reveals a natural mutation in gyrA . J. Antimicrob. Chemother. 61, 1252–1255 (2008).
del Valle, L. J. et al. Bartonella bacilliformis, endemic pathogen of the Andean region, is intrinsically resistant to quinolones. Int. J. Infect. Dis. 14, e506–510 (2010).
Espinoza-Culupú, A. et al. Caracterización molecular de la región determinante de resistencia a quinolonas (QRDR) de la topoisomerasa IV de Bartonella bacilliformis en aislados clínicos. Rev. Peru. Biol. 21, 89–98 (2014).
Mendoza-Mujica, G. & Flores-León, D. Resistencia antimicrobiana de cepas de Bartonella bacilliformis procedentes de regiones endémicas de la Enfermedad de Carrión en el Perú. Rev. Peru. Med. Exp. Salud Publ. 32, 659–666 (2015).
Battisti, J. M., Smitherman, L. S., Samuels, D. S. & Minnick, M. F. Mutations in Bartonella bacilliformis gyrB confer resistance to coumermycin A1. Antimicrob. Agents Chemother. 42, 2906–2913 (1998).
Biswas, S., Raoult, D. & Rolain, J. M. Molecular mechanisms of resistance to antibiotics in Bartonella bacilliformis . J. Antimicrob. Chemother. 59, 1065–1070 (2007).
Minnick, M. F., Wilson, Z. R., Smitherman, L. S. & Samuels, D. S. gyrA mutations in ciprofloxacin-resistant Bartonella bacilliformis strains obtained in vitro . Antimicrob Agents Chemother 47, 383–386 (2003).
Walker, T. S. & Winkler, H. H. Bartonella bacilliformis: colonial types and erythrocyte adherence. Infect. Immun. 31, 480–486 (1981).
Pachas, P. Generando evidencias para las políticas públicas de prevención y control: experiencia en la enfermedad de Carrión en el Perú. VII Congreso del INS. 2013. Lima (Perú). http://www.bvs.ins.gob.pe/congresos/images/ponencias/dia_7/1ra_sesion/evidencias_para_el_control_de_la_EC.pdf. (accessed: 19th April, 2016).
Ruiz, J. Mechanisms of resistance to quinolones: target alterations, decreased accumulation and DNA gyrase protection. J. Antimicrob. Chemother. 51, 1109–1117 (2003).
Besier, S., Ludwig, A., Zander, J., Brade, V. & Wichelhaus, T. A. Linezolid resistance in Staphylococcus aureus: gene dosage effect, stability, fitness costs, and cross-resistances. Antimicrob. Agents Chemother. 52, 1570–1572 (2008).
Ma, L. et al. Identification of a novel G2073A mutation in 23S rRNA in amphenicol-selected mutants of Campylobacter jejuni . PLoS One. 9, e94503 (2014).
Thompson, J. et al. Analysis of mutations at residues A2451 and G2447 of 23S rRNA in the peptidyltransferase active site of the 50S ribosomal subunit. Proc. Natl. Acad. Sci. USA 98, 9002–9007 (2001).
Zaman, S., Fitzpatrick, M., Lindahl, L. & Zengel, J. Novel mutations in ribosomal proteins L4 and L22 that confer erythromycin resistance in Escherichia coli . Mol. Microbiol. 66, 1039–1050 (2007).
Rieux, V., Carbon, C. & Azoulay-Dupuis, E. Complex relationship between acquisition of β-lactam resistance and loss of virulence in Streptococcus pneumoniae . J. Infect. Dis. 184, 66–72 (2001).
Velasco, M. et al. Decreased invasive capacity of quinolone-resistant Escherichia coli in patients with urinary tract infections. Clin. Infect. Dis. 33, 1682–1686 (2001).
Le Hello, S. et al. Highly drug-resistant Salmonella enterica serotype Kentucky ST198-X1: a microbiological study. Lancet Infect. Dis. 13, 672–679 (2013).
Ettayebi, M., Prasad, S. M. & Morgan, E. A. Chloramphenicol-erythromycin resistance mutations in a 23S rRNA gene of Escherichia coli . J. Bacteriol. 162, 551–557 (1985).
Wolter, N. et al. Novel mechanism of resistance to oxazolidinones, macrolides, and chloramphenicol in ribosomal protein L4 of the pneumococcus. Antimicrob. Agents Chemother. 49, 3554–3557 (2005).
Douthwaite, S. Functional interactions within 23S rRNA involving the peptidyltransferase center. J. Bacteriol. 174, 1333–1338 (1992).
Vester, B. & Douthwaite, S. Macrolide resistance conferred by base substitutions in 23S rRNA . Antimicrob. Agents Chemother. 45: 1–12 (2001).
Biswas, S., Maggi, R. G., Papich, M. G. & Breitschwerdt, E. B. Molecular mechanisms of Bartonella henselae resistance to azithromycin, pradofloxacin and enrofloxacin. J. Antimicrob. Chemother. 65, 581–582 (2010).
Biswas, S., Raoult, D. & Rolain, J. M. Molecular characterization of resistance to macrolides in Bartonella henselae . Antimicrob. Agents Chemother. 50, 3192–3193 (2006).
Diner, E. J. & Hayes, C. S. Recombineering reveals a diverse collection of ribosomal proteins L4 and L22 that confer resistance to macrolide antibiotics. J. Mol. Biol. 386, 300–315 (2009).
Gomes, C. et al. Which mechanisms of azithromycin resistance are selected when efflux pumps are inhibited? Int. J. Antimicrob. Agents 4, 307–311 (2013).
Dujon, B. Sequence of the intron and flanking exons of the mitochondrial 21S rRNA gene of yeast strains having different alleles at the omega and rib-1 loci. Cell 20, 185–197 (1980).
Ruiz, J. et al. Long time survival of Bartonella bacilliformis in blood stored at 4 °C. A risk for blood transfusions. Blood Transfus. 10, 563–564 (2012).
Pons, M. J. et al. Analysis of quinolone-resistance in commensal and diarrheagenic Escherichia coli isolates from infants in Lima, Peru. Trans. R. Soc. Trop. Med. Hyg. 108, 22–28 (2014).
Vila, J. et al. Quinolone resistance in enterotoxigenic Escherichia coli causing diarrhea in travelers to India in comparison with other geographical areas. Antimicrob. Agents Chemother. 44, 1731–1733 (2000).
Vila, J. et al. Susceptibility patterns of enteroaggregative Escherichia coli associated with traveller’s diarrhoea: emergence of quinolone resistance. J. Med. Microbiol. 50, 996–1000 (2001).
Angelakis, E., Raoult, D. & Rolain, J. M. Molecular characterization of resistance to fluoroquinolones in Bartonella henselae and Bartonella quintana . J. Antimicrob. Chemother. 63, 1288–1289 (2009).
Madurga, S., Sánchez-Céspedes, J., Belda, I., Vila, J. & Giralt, E. Mechanism of binding of fluoroquinolones to the quinolone resistance-determining region of DNA gyrase: towards an understanding of the molecular basis of quinolone resistance. Chembiochem 9, 2081–2086 (2008).
Pan, X. S. & Fisher, L. M. DNA gyrase and topoisomerase IV are dual targets of clinafloxacin action in Streptococcus pneumoniae . Antimicrob. Agents Chemother. 42, 2810–2816 (1998).
Huband, M. D. et al. In vitro and in vivo activities of PD 0305970 and PD 0326448, new bacterial gyrase/topoisomerase inhibitors with potent antibacterial activities versus multidrug-resistant gram-positive and fastidious organism groups. Antimicrob. Agents Chemother. 51, 1191–1201 (2007).
Sunagawa, S. et al. Comparison of drug sensitivity and genotypes of clinically isolated strains of levofloxacin-resistant Streptococcus pneumoniae obtained from Okinawa Island, the Japanese main island and Hong Kong. J. Antibiot. 64, 539–545 (2011).
Severinov, K., Soushko, M., Goldfarbs, A. & Nikiforov, V. New rifampicin-resistant and streptolydigin–resistant mutants in the β subunit of Escherichia coli RNA polymerase. J. Biol. Chem. 268, 14820–14825 (1993).
Xu, M., Ning, Y., Goldstein, B. P. & Jin, D. J. Cross-resistance of Escherichia coli RNA polymerases conferring rifampin resistance to different antibiotics. J. Bacteriol. 187, 2783–2792 (2005).
Heep, M. et al. Frequency of rpoB mutations inside and outside the cluster I region in rifampin-resistant clinical Mycobacterium tuberculosis isolates. J. Clin. Microbiol. 39, 107–110 (2001).
Kothary, V. et al. Rifaximin resistance in Escherichia coli associated with inflammatory bowel disease correlates with prior rifaximin use, mutations in rpoB, and activity of Phe-Arg-β-naphthylamide-inhibitable efflux pumps. Antimicrob. Agents Chemother. 57, 811–817 (2013).
Pons, M. J., Mensa, L., Gascón, J. & Ruiz, J. Fitness and molecular mechanisms of resistance to rifaximin in in vitro selected Escherichia coli mutants. Microb. Drug Resist. 18, 376–379 (2012).
Fines, M., Pronost, S., Maillard, K., Taouji, S. & Leclercq, R. Characterization of mutations in the rpoB gene associated with rifampin resistance in Rhodococcus equi isolated from foals. J. Clin. Microbiol. 39, 2784–2787 (2001).
Li, B. et al. Artesunate enhances the antibacterial effect of β-lactam antibiotics against Escherichia coli by increasing antibiotic accumulation via inhibition of the multidrug efflux pump system AcrAB-TolC. J. Antimicrob. Chemother. 66, 769–777 (2011).
Takatsuka, Y., Chen, C. & Nikaido, H. Mechanism of recognition of compounds of diverse structures by the multidrug efflux pump AcrB of Escherichia coli . Proc. Natl. Acad. Sci. USA 107, 6559–6565 (2010).
Moore, S. D. & Sauer, R. T. Revisiting the mechanism of macrolide-antibiotic resistance mediated by ribosomal protein L22. Proc. Natl. Acad. Sci. USA 105, 18261–18266 (2008).
Perez-Alva, S. La maladie de Carrion. Essai d’infection experimentale de la souris blanche par voie intranasale par Bartonella bacilliformis . Bull. Soc. Pathol. Exot. Filiales. 50, 184–188 (1957).
Birtles, R. J. et al. Identification of Bartonella bacilliformis genotypes and their relevance to epidemiological investigations of human bartonellosis. J. Clin. Microbiol. 40, 3606–3612 (2002).
García-Esteban, C. et al. Molecular method for Bartonella species identification in clinical and environmental samples. J. Clin. Microbiol. 46, 776–779 (2008).
Gasteiger, E. et al. Protein identification and analysis tools on the ExPASy server In The proteomics protocols handbook (ed. Walker, J. M. ) 571–607 (Humana Press, 2005).
Kyte, J. & Doolittle, R. F. A simple method for displaying the hydropathic character of a protein. J. Mol. Biol. 157, 105–132 (1982).
Acknowledgements
This study has been funded by the ISCIII [grant number: PI11/00983 which include FEDER funds], by the Programa Nacional de Innovación para la Competitividad y Productividad (Innóvate Perú), under the contract 117-PNICP-PIAP-2015 and by Generalitat de Catalunya, Departament d’Universitats, Recerca i Societat de la Informació (2014 SGR 26). JR has a fellowship from the program I3, of the ISCIII [grant number: CES11/012]. CG has a PhD fellowship of the ISCIII (FI12/00561). MJP has a postdoctoral fellowship from CONCYTEC/FONDECYT (grant number: CG05-2013-FONDECYT). We thank Donna Pringle for idiomatic corrections.
Author information
Authors and Affiliations
Contributions
J.R., C.G. and J.d.V.M. design the experiment; C.G., S.M.-P., L.R.-R. and J.R. developed the mutant strains, and perform the antibiotic susceptibility studies; C.G. and M.J.P. perform the molecular studies. C.G. and J.R. analyzed the data; J.R. and C.G. wrote the manuscript draft. All authors read the manuscript critically, provide suggestions and approved the final version.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing financial interests.
Supplementary information
Rights and permissions
This work is licensed under a Creative Commons Attribution 4.0 International License. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in the credit line; if the material is not included under the Creative Commons license, users will need to obtain permission from the license holder to reproduce the material. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/
About this article
Cite this article
Gomes, C., Martínez-Puchol, S., Ruiz-Roldán, L. et al. Development and characterisation of highly antibiotic resistant Bartonella bacilliformis mutants. Sci Rep 6, 33584 (2016). https://doi.org/10.1038/srep33584
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/srep33584
This article is cited by
-
Carrion’s disease: an eradicable illness?
Infectious Diseases of Poverty (2016)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.