Abstract
To revisit the autosomal dominant Sorsby fundus dystrophy (SFD) as a syndromic condition including late-onset pulmonary disease. We report clinical and imaging data of ten affected individuals from 2 unrelated families with SFD and carrying heterozygous TIMP3 mutations (c.572A > G, p.Y191C, exon 5, in family 1 and c.113C > G, p.S38C, exon 1, in family 2). In family 1, all SFD patients older than 50 (two generations) had also a severe emphysema, despite no history of smoking or asthma. In the preceding generation, the mother died of pulmonary emphysema and she was blind after the age of 50. Her two great-grandsons (<20 years), had abnormal Bruch Membrane thickness, a sign of eye disease. In family 2, eye and lung diseases were also associated in two generations, both occurred later and lung disease was moderate (bronchiectasis). This is the first report of a syndromic SFD in line with the mouse model uncovering the role of TIMP3 in human lung morphogenesis and functions. The TIMP3 gene should be screened in familial pulmonary diseases with bronchiectasis, associated with a medical history of visual loss. In addition, SFD patients should be advised to avoid tobacco consumption, to practice sports and to undergo regular pulmonary examinations.
Similar content being viewed by others
Introduction
Sorsby fundus dystrophy (SFD, MIM 136900) is a rare autosomal dominant retinal dystrophy described by Sorsby, Mason and Gardener in 19491. SFD is characterized by bilateral deposition of yellow drusen-like material and extensive choroidal neovascularization (CNV) occurring between the third to fifth decades of life. Despite variable and confounding phenotypes, this dystrophy should be considered in patients with early neovascularization in absence of predisposing factors such as high myopia, or with irregular thickening of the Bruch membrane as shown on SD-OCT.
Weber and al. published in 1994 the first causal heterozygous mutation in the tissue inhibitor of metalloproteinases -3 (TIMP3, 22q12.3, 5 exons) in a family with SFD2. The autosomal dominant inheritance was further confirmed in all families, including those with a presumed recessive trait. TIMP3 as well as TIMP1 and TIMP2 regulate extracellular matrix renewal by the inhibition of matrix metalloproteinases (MMP). TIMPs form complexes with MMP-1, MMP-2, MMP-3, MMP-7, MMP-9, MMP-13, MMP-14 and MMP-15 and irreversibly inactivate them by binding to their catalytic zinc cofactor. The NH2-terminal domain of TIMP1, TIMP2 and TIMP3 is responsible for MMP inhibition, whereas the COOH-terminal domain is involved in additional functions of the protein. In the retina, TIMP3 interacts with epithelial growth factor-containing fibulin-like extracellular matrix protein 1 (EFEMP1) and blocks the binding of VEGF to VEGFR2 resulting in inhibition of angiogenesis3,4,5,6,7,8,9,10,11,12,13. The majority of known mutations in TIMP3 underlying SFD are located in exon 5, with a substitution by a cysteine residue in most cases (for examples codons 174, 177 and 191). In the eye, Sorsby fundus retinal dystrophy is then characterized by a thickening of Bruch Membrane and subsequent risk of choroidal neovascularization after the age of 40. The thickening of Bruch Membrane in SFD is located between the basement membrane of the RPE and the inner collagenous zone as previously reported in electron microscopic studies14,15. The current pathological hypothesis is that TIMP3 mutants with unpaired cysteine residue lead to the formation and accumulation of dimers in the extracellular matrix (ECM, Bruch Membrane). Bruch Membrane thickening contributes to a relative hypoxia and a dysfunction of the RPE with occurrence of choroidal neovascularization and progressive RPE loss.
Chronic Obstructive Pulmonary Disease (COPD) is characterized by an irreversible airflow limitation, caused by an increase in the resistance of the small conducting airways and in lung compliance due to emphysema16,17,18,19,20. The main causes are tobacco smoking together with atmospheric and domestic pollution. As only 15 to 20% smokers develop the disease, genetic factors could be involved in the pathogenesis. To date, polymorphisms in metalloproteinases (MMP3, MMP9) and their inhibitors (TIMP2, TIMP3) have been shown to be implicated21,22.
So far, SFD was strictly considered as an ocular disease. We report herein for the first time two unrelated families carrying heterozygous mutations in TIMP3 with an autosomal dominant syndromic form of SFD associated with pulmonary disease.
Results
Clinical findings
All SFD patients older than 55 years had pulmonary involvement either moderate (asymptomatic air trapping) or severe (severe panlobular emphysema, very severe obstruction and chronic respiratory failure).
Family 1
Ocular involvement
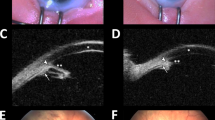
In this family (Figs 1 and 2), the 5 patients older than 30 had extensive bilateral CNV with diffuse drusen-like changes (Table 1). CNV occurred at a young age (23 to 40 years). The oldest patient complained of moderate night-blindness. All were legally blind except patient IV:1, who received intravitreal injections of anti-vascular endothelial growth factor (bevacizumab) and retained 20/20 best-corrected visual acuity in the right eye. The grand-mother (II:3) of patient IV:1 was legally blind after the age of 50. The two younger boys (V:1, V:2) were asymptomatic, but their Bruch Membrane was abnormally thickened on SD-OCT.
Family 1.
Color fundus photographs. (A,B) The youngest patient (V:2 ) had a normal fundus appearance. His father (C,D- IV:1) had a severe macular scarring in his left eye (D) and a preserved macula in his right eye by the use of anti-VEGF injections (C). Patients III:3 (E,F) and III:4 (G,H) had severe macular lesions.
Pulmonary involvement
Without smoking exposure or any other pulmonary disease, generation III (70, 67, 59 and 53 years) had airflow limitation with a reduction of (FEV1) between 28% and 73% (according to American and European Thoracic Society criteria). On CT scans, these patients showed air trapping and abnormal bronchial wall thickening with mild basal bronchiectasis (Fig. 3). Two of them (III:1 and III:2)had chronic respiratory failure with oxygen supplementation. Their mother (II:3) died from severe emphysema. Patients IV:1 (44 years) had air trapping on chest tomography with normal pulmonary function tests. Patient V:1 (16 years) had air trapping and hypoxemia (79 mmHg) at rest. This patient had also complex cardiac congenital malformation with ventricular septal defect, obstruction of the right ventricular outflow tract, mitral valve dysplasia and hypoplasia of the left ventricle. An emergency surgical procedure was performed at 15 days of life for cyanosis. His brother V:2 (14 years) had a normal thoracic tomography and normal pulmonary function tests at rest.
High resolution computed tomographic scans of patients III:3 (A) and III:2 (B). On CT scans, note bronchiectasis, diffuse bronchial wall thickening (large arrows), air trapping and emphysema bullae (thin arrows). These lesions are localized at the basal part of the lung and not at the apex as noted in smokers. Patient III:2 uses domiciliary oxygen.
Family 2
Ocular involvement
Night blindness, reported after the age of 45 was the first symptom in this family (Figs 4 and 5) (Table 1). At onset, multiple diffuse drusen-like accumulations or large yellow lesions were observed at the posterior pole and in the whole peripheral retina. In patients III:2- 3 and 6, after the age of 40 to 50 years, best-corrected visual acuity decreased rapidly in both eyes in less than 10 years due to recurrent and extensive choroidal neovascularization. At the final stage, extensive subretinal fibrosis and macular atrophy with pigmentary changes were observed in both eyes (Fig. 5). The mother (patient II:2) carried the presumed diagnosis of macular degeneration and was blind before 60 years.
Color fundus photographs.
(A) Patient III:2 at the age of 55, note the numerous drusen-like lesions and yellow large material all over the retina. (B) Same patient at the age of 81, macular atrophy occurred with subsequent ambulatory vision loss. (C) Patient III:6 at the age of 57, note the atrophic lesions at the posterior pole in the right eye. (D) Same patient at the age of 65.
Pulmonary involvement
In this family, the two living patients of generation III underwent chest CT and had mild to marked bronchial wall thickening with mild cylindrical bronchiectasis in a single case (Fig. 6). None had CT features of emphysema. The mother II:2 developed after the age of 70 years atypical asthma with no history of smoking.
Genetic findings
Family 1
We found the TIMP3 variation c.572A > G (p.Y191C) in exon 5, previously described in a family with isolated SFD (initially p.Y168C)2. This variation is considered to be probably damaging by PolyPhen 2 with a score = 1 (http://genetics.bwh.harvard.edu/pph2), damaging according to SIFT with a score = 0 (http://sift.jcvi.org) and to interfere most likely with the function of the protein by the align-GVDG program with a class C65 (http://agvgd.iarc.fr/agvgd_input.php), disease causing for mutation taster with a probability of 0.99 (www.mutationtaster.org) and neutral for Provean (provean.jcvi.org). The mutation co-segregated with the disease in the family and is not reported in the ExAc database (http://exac.broadinstitute.org).
Multiple amino-acid sequence alignment of TIMP3 orthologs showed the conservation of the leucine at position 191 in all eukaryotic sequences available. According to Nextprot database (www.nextprot.org), this mutation has been noted in several families since the initial identification of TIMP32,23.
Family 2
We found the TIMP3 variation c.113C > G (p.S38C) in exon 1 which has been previously described in SFD24. This variation is considered to be probably damaging by PolyPhen 2 with a score = 1 (http://genetics.bwh.harvard.edu/pph2), damaging according to SIFT with a score = 0 (http://sift.jcvi.org) and to interfere most likely with the function of the protein by the align-GVDG program with a class C65 (http://agvgd.iarc.fr/agvgd_input.php), disease causing for mutation taster with a probability of 0.99 (www.mutationtaster.org) and deleterious for Provean (provean.jcvi.org). This variation is not present in ExAC. In addition, the mutation co-segregated with the disease in the family. This mutation has been reported previously in 5 SFD unrelated patients24,25.
Discussion
This is the first report of a syndromic association of autosomal dominant SFD with an autosomal dominant pulmonary disease. This latter aspect is characterized by distal bronchiolar and alveolar dysfunctions leading to a chronic obstructive pulmonary disease in absence of asthma and tobacco consumption. In addition, the basal location of pulmonary lesions is not in keeping with COPD secondary to smoking. In these families, the two oldest generations developed pulmonary lesions in line with an autosomal dominant transmission and with an extracellular matrix remodeling disease (Bruch Membrane in the eye). Indeed, there are several experimental data that plead for the pathological role of TIMP3 mutations in the pulmonary disease.
First, TIMP3 is highly expressed in the lung. Its role in this organ was well established in developmental phases, in resolution of inflammation following lung injury and in idiopathic pulmonary fibrosis26,27,28. At the developmental stage, bronchiole branching morphogenesis depends on interactions between the bronchiole epithelium, the mesenchyme and the extracellular matrix or basement membrane which serves as an interface between the two compartments. Remarkably, it was shown that in Timp3-/- null mice, enhanced MMP activity interferes with extra cellular matrix proteolysis, perturbing the formation of the bronchiole tree during morphogenesis. These homozygous mice have abnormal bronchiolar morphology and respiratory dysfunction with reduction in carbon monoxide uptake and a progressive increased alveolar size proved by a decline in hydroxy-proline content (http://www.informatics.jax.org/allele/genoview/MGI:3056101).
Another aspect of the role of TIMP3 in the pulmonary disease is its involvement in the resolution of inflammation following lung injury, by regulating the neutrophil influx in the injury site. In Timp3-/- mice, the inflammation persisted up to 28 days with increased neutrophil chemotactic activity28. This prolonged abnormal response was reversed under synthetic inhibitor of MMP. In addition, in idiopathic pulmonary fibrosis characterized by fibroblast expansion and extracellular matrix accumulation, TIMP3 gene expression is increased and the protein is localized to fibroblastic foci and extracellular matrix. This dysregulation of ECM remodeling could involve in the lung the p38 kinase pathway and the TGF-beta1 which are important mediators in lung fibrosis.
The role of polymorphisms in metalloproteinases (MMP3-MMP9, ADAM33) and their inhibitors (TIMP2 and TIMP3) in the onset and severity of COPD in smokers has been reported21,22. In our families, a mutation in TIMP3 is also probably the cause of the autosomal dominant lung disease with lung extracellular matrix damaging.
This syndromic disease could be unsuspected because the pulmonary disease starts one to three decades after visual loss. For example, in our family 2, pulmonary involvement was only confirmed by CT imaging. This new syndrome has an autosomal dominant inheritance as it concerns three generations (6 patients) in family one and two generations (three patients) in family two.
To shed light on the potential impact of the two mutations and differences of disease onset or severity, a theoretical model of the full-length TIMP3 was based on the crystal structure of TIMP2 and TIMP3 as a combined template using the server @TOME-2 (Pons et Labesse 2009)29,30. The differences in lung severity involvement between families 1 and 2 could be linked with both the type of substitutions/mutations (non-conservative/conservative, respectively) and their locations in distinct domains (C-terminal and N-terminal respectively, Fig. 7). Indeed, in family 1, a large and hydrophobic residue is substituted by a small cysteine while in the family 2, a serine is substituted by an isosteric cysteine. Furthermore, in the first case, the additional cysteine lies spatially close to two disulphide bridges (C145–C192; C163, C184) and it may interfere with them especially during TIMP3 folding and maturation. In the second case, the substitution occurs further from any other cysteines (C36–C143). Finally, the two mutated sites correspond to two distinct protein-protein interaction sites. The mutation p.S38C is located at the interface with the MMPs and is not predicted to affect significantly the binding affinity. On the contrary, due to a more pronounced change in amino-acid size, the mutation p.Y191C could impact more dramatically on the interaction with EFEMP1 which has been mapped to the C-terminal part of TIMP313. Accordingly, the mutation in family 1 is predicted to be more detrimental to the protein function and/or stability than the second mutation. It should be noted that EFEMP1 is also expressed in the lung, but we cannot exclude that TIMP3 interacts with a distinct lung specific molecule. Regarding SFD, CNV occurred during the third and fourth decades in family 1 versus the fifth decade for family 2. The other reported cases with p.S38C and p.Y191C displayed similar differences in age of onset2,23,24,25.
Representation of a theoretical model of the TIMP3 mature protein.
The main-chain is shown as ribbon with the N-terminal domain (24–127) and C-terminal domain (128–209) colored in light blue and light green, respectively. The side-chain of the cysteines and the two mutated residues (S38 and Y191) are shown as stick in orange and red color, respectively. The figure was prepared using Pymol (http://www.pymol.org).
In conclusion, Sorsby fundus dystrophy should be reappraised as a syndromic condition with a risk of late onset bronchiolar and pulmonary disease. SFD patients should avoid tobacco smoking and practice sports. Furthermore, a pulmonary disease should be investigated after the age of 55. In this line, TIMP3 should be screened in patients with familial bronchiectasis or emphysema, particularly if a medical history of visual loss or choroidal neovascularization is reported.
Patients and Methods
Informed consent was obtained for clinical examination and genetic analysis from all patients. All methods were carried out in accordance with approved protocols of Montpellier and Lille University Hospitals and in agreement with the Declaration of Helsinki. The Ministry of Public Health accorded approval for biomedical research under the authorization number 11018S.
Clinical and functional retinal evaluation
For each patient, age at examination, refraction, initial and final best-corrected visual acuity were noted. The best-corrected visual acuity was obtained with Snellen charts. Near visual acuity was assessed with the current French near vision chart (Parinaud). Color fundus photographs were performed with Topcon Imagenet (Ophthalmic Imaging Systems, Japan) or Nidek non-mydriatic automated fundus camera AFC 330 (Nidek Inc, Japan). Autofluorescence imaging and spectral domain optical coherent tomography were performed with Combined Heidelberg Retina Angiograph + OCT Spectralis device (Heidelberg Engineering, Dossenheim, Germany).
Pulmonary evaluation
Chest computed tomography (CT)
We performed high-resolution chest CT scans in 8 patients (6 in family 1 and 2 in family 2). Chest CT was obtained on different multi-detector (MDCT) scanners, including a 64-slice MDCT equipment (SOMATON Definition AS+, SIEMENS, Healthcare, Forchheim, Germany) and a third-generation, dual source CT scanner (SOMATOM Force, SIEMENS Healthcare, Forchheim, Germany) detectors. The scanning protocol included end-inspiratory and -expiratory acquisitions over the entire thorax. The CT parameters analyzed on lung images included emphysema (i.e., centrilobular, panlobular, bullous), bronchial wall thickening, bronchiectasis and CT features of small airways disease (i.e., bronchiolectases, ill-defined micronodules, mosaic attenuation and air trapping) on lung images.
Pulmonary function test
Spirometry was performed in all affected patients of family 1, in accordance with American Thoracic Society standards19,31. Values of percent-predicted for spirometry were calculated using reference values based on age, height, sex and race19,31. The basic parameters used to properly interpret lung function were forced vital capacity (FVC), forced expiratory volume in 1 s (FEV1) and FEV1/FVC ratio. Airway obstruction was defined by reduction of the FEV1/FVC ratio (also known as Tiffeneau-index) below 70%.
Genetic analysis
Genomic DNA was extracted using a standard salting-out procedure. All exons of TIMP3 (refseq NG_009117.1) were screened in all patients. The screening was performed on genomic DNA using primers designed to flank the splice junctions of each exon (sequences available upon request). After standard polymerase chain reaction (PCR) amplification, products were purified with ExoSAP-IT (GE Healthcare Life Sciences, USB Corporation) and direct sequencing was performed on an Applied Biosystems (ABI) 3130 xL genetic analyzer (Applied BioSystems, Foster City, CA, USA) using the BigDye Terminator Cycle Sequencing Ready Reaction kit V3.1. Sample sequences were aligned to the wild-type sequence and analyzed with the Collection and Sequence Analysis software package (Applied Biosystems).
The pathogenicity of nucleotide changes was estimated by different predictive software including, Polyphen program - Harvard University, Boston, MA. http://genetics.bwh.harvard.edu/pph, SIFT (http://sift.jcvi.org), Align-GVDG program (http://agvgd.iarc.fr/agvgd_input.php), Mutation taster (www.mutationtaster.org) and Provean (provean.jcvi.org). The pathogenicity was also assessed considering multiple-amino-acid sequence alignment of TIMP3 orthologs and the protein structure identity according to Nextprot database (www.nextprot.org). Indeed, the variation had to segregate with the disease in the family. The identified variations were tracked in all genetic databases and in previous articles about Sorsby fundus dystophy.
Additional Information
How to cite this article: Meunier, I. et al. A new autosomal dominant eye and lung syndrome linked to mutations in TIMP3 gene. Sci. Rep. 6, 32544; doi: 10.1038/srep32544 (2016).
References
Sorsby, A., Mason, M. E. J. & Gardener, N. A Fundus dystrophy with unusual features (Late onset and dominant inheritance of a central retinal lesion showing oedema, haemorrhage and exudates developing into generalised choroidal atrophy with massive pigment proliferation). Br. J. Ophthalmol. 33, 67–97 (1949).
Weber, B. H., Vogt, G., Pruett, R. C., Stöhr, H. & Felbor, U. Mutations in the tissue inhibitor of metalloproteinases-3 (TIMP3) in patients with Sorsby’s fundus dystrophy. Nat. Genet. 8, 352–356 (1994).
Weber, B. H. F. et al. A mouse model for Sorsby fundus dystrophy. Invest. Ophthalmol. Vis. Sci. 43, 2732–2740 (2002).
Qi, J. H. et al. A novel function for tissue inhibitor of metalloproteinases-3 (TIMP3): inhibition of angiogenesis by blockage of VEGF binding to VEGF receptor-2. Nat. Med. 9, 407–415 (2003).
Pescosolido, N. et al. Role of Protease-Inhibitors in Ocular Diseases. Molecules 19, 20557–20569 (2014).
Sukhikh, G. T. & Soboleva, G. M. Sorsby fundus dystrophy-related mutation in tissue inhibitor of metalloproteinases-3 impairs regulation of its expression in mouse fibroblasts. Bull. Exp. Biol. Med. 143, 64–67 (2007).
Qi, J. H., Ebrahem, Q. & Anand-Apte, B. Tissue inhibitor of metalloproteinases-3 and Sorsby fundus dystrophy. Adv. Exp. Med. Biol. 533, 97–105 (2003).
Saihan, Z. et al. Clinical and biochemical effects of the E139K missense mutation in the TIMP3 gene, associated with Sorsby fundus dystrophy. Mol. Vis. 15, 1218–1230 (2009).
Smookler, D. S. et al. Cutting Edge: Tissue Inhibitor of Metalloproteinase 3 Regulates TNF-Dependent Systemic Inflammation. J. Immunol. 176, 721–725 (2006).
Anand-Apte, B. et al. Inhibition of angiogenesis by tissue inhibitor of metalloproteinase-3. Invest. Ophthalmol. Vis. Sci. 38, 817–823 (1997).
Qi, J. H. et al. S156C Mutation in Tissue Inhibitor of Metalloproteinases-3 Induces Increased Angiogenesis. J. Biol. Chem. 284, 19927–19936 (2009).
Soboleva, G., Geis, B., Schrewe, H. & Weber, B. H. F. Sorsby fundus dystrophy mutation Timp3 (S156C) affects the morphological and biochemical phenotype but not metalloproteinase homeostasis. J. Cell. Physiol. 197, 149–156 (2003).
Klenotic, P. A., Munier, F. L., Marmorstein, L. Y. & Anand-Apte, B. Tissue Inhibitor of Metalloproteinases-3 (TIMP-3) Is a Binding Partner of Epithelial Growth Factor-containing Fibulin-like Extracellular Matrix Protein 1 (EFEMP1) IMPLICATIONS FOR MACULAR DEGENERATIONS. J. Biol. Chem. 279, 30469–30473 (2004).
Ashton, N. & Sorsby, A. Fundus Dystrophy with Unusual Features. Br. J. Ophthalmol. 35, 751–764 (1951).
Capon, M. R. et al. Sorsby’s fundus dystrophy. A light and electron microscopic study. Ophthalmology 96, 1769–1777 (1989).
Cigarette smoking and health. American Thoracic Society. Am. J. Respir. Crit. Care Med. 153, 861–865 (1996).
Løkke, A., Lange, P., Scharling, H., Fabricius, P. & Vestbo, J. Developing COPD: a 25 year follow up study of the general population. Thorax 61, 935–939 (2006).
Pauwels, R. A. et al. Global strategy for the diagnosis, management and prevention of chronic obstructive pulmonary disease. NHLBI/WHO Global Initiative for Chronic Obstructive Lung Disease (GOLD) Workshop summary. Am. J. Respir. Crit. Care Med. 163, 1256–1276 (2001).
Lung function testing: selection of reference values and interpretative strategies. American Thoracic Society. Am. Rev. Respir. Dis. 144, 1202–1218 (1991).
Celli, B. R. et al. The body-mass index, airflow obstruction, dyspnea and exercise capacity index in chronic obstructive pulmonary disease. N. Engl. J. Med. 350, 1005–1012 (2004).
Korytina, G. F. et al. [Association of the MMP3, MMP9, ADAM33 and TIMP3 genes polymorphic markers with development and progression of chronic obstructive pulmonary disease]. Mol. Biol. (Mosk.) 46, 487–499 (2012).
Navratilova, Z., Kolek, V. & Petrek, M. Matrix Metalloproteinases and Their Inhibitors in Chronic Obstructive Pulmonary Disease. Arch. Immunol. Ther. Exp. (Warsz.) 64, 177–193 (2016).
Felbor, U. et al. A second independent Tyr168Cys mutation in the tissue inhibitor of metalloproteinases-3 (TIMP3) in Sorsby’s fundus dystrophy. J. Med. Genet. 33, 233–236 (1996).
Schoenberger, S. D. & Agarwal, A. A novel mutation at the N-terminal domain of the TIMP3 gene in Sorsby fundus dystrophy. Retina Phila. Pa 33, 429–435 (2013).
Warwick, A., Gibson, J., Sood, R. & Lotery, A. A rare penetrant TIMP3 mutation confers relatively late onset choroidal neovascularisation which can mimic age-related macular degeneration. Eye Lond. Engl. 30, 488–491 (2016).
García-Alvarez, J. et al. Tissue inhibitor of metalloproteinase-3 is up-regulated by transforming growth factor-beta1 in vitro and expressed in fibroblastic foci in vivo in idiopathic pulmonary fibrosis. Exp. Lung Res. 32, 201–214 (2006).
Gill, S. E., Pape, M. C. & Leco, K. J. Tissue inhibitor of metalloproteinases 3 regulates extracellular matrix–cell signaling during bronchiole branching morphogenesis. Dev. Biol. 298, 540–554 (2006).
Gill, S. E. et al. Tissue inhibitor of metalloproteinases 3 regulates resolution of inflammation following acute lung injury. Am. J. Pathol. 176, 64–73 (2010).
Fernandez-Catalan, C. et al. Crystal structure of the complex formed by the membrane type 1-matrix metalloproteinase with the tissue inhibitor of metalloproteinases-2, the soluble progelatinase A receptor. EMBO J. 17, 5238–5248 (1998).
Wisniewska, M. et al. Structural determinants of the ADAM inhibition by TIMP-3: crystal structure of the TACE-N-TIMP-3 complex. J. Mol. Biol. 381, 1307–1319 (2008).
Pellegrino, R. et al. Interpretative strategies for lung function tests. Eur. Respir. J. 26, 948–968 (2005).
Acknowledgements
We thank all the family members who participated in this study. We acknowledge the support from the INSERM, CNRS and ANR-10-BINF-03-03.
Author information
Authors and Affiliations
Contributions
Study concept and design: I.M., B.B., B.P. Data acquisition: I.M., B.B., G.L., C.Z., S.D.-D., A.L., M.M.-F., I.D., A.-S.G., C.M., V.M., L.S., C.-M.D., C.A., P.C., M.R.-J., S.Y.C., J.-A.S., B.P., I.A., S.M. and C.P.H. Data analysis and interpretations: I.M., B.B., G.L., C.Z., S.D.-D., A.L., M.M.-F., I.D., A.-S.G., C.M., V.M., L.S., C.-M.D., C.A., P.C., M.R.-J., S.Y.C., J.-A.S., B.P., I.A., S.M. and C.P.H. Manuscript preparation: I.M., B.B., G.L., A.-S.G, M.R.-J. and B.P.
Ethics declarations
Competing interests
The authors declare no competing financial interests.
Rights and permissions
This work is licensed under a Creative Commons Attribution 4.0 International License. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in the credit line; if the material is not included under the Creative Commons license, users will need to obtain permission from the license holder to reproduce the material. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/
About this article
Cite this article
Meunier, I., Bocquet, B., Labesse, G. et al. A new autosomal dominant eye and lung syndrome linked to mutations in TIMP3 gene. Sci Rep 6, 32544 (2016). https://doi.org/10.1038/srep32544
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/srep32544
This article is cited by
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.