Abstract
The clinical behavior of patients with advanced non-small cell lung cancer (NSCLC) differ between epidermal growth factor receptor (EGFR) exon 19 deletion (Ex19) and EGFR exon 21 L858R mutation (Ex21). This study aimed to evaluate whether these differences exist in surgically resected NSCLC. A total of 198 patients with surgically resected NSCLC harbouring Ex19 (n = 53), Ex21 (n = 51), and EGFR wild-type (Wt) (n = 94) were analyzed. The clinicopathological features, laboratory parameters, recurrent sites and disease-free survival (DFS) were compared according to mutational EGFR status. Ex21 occurred more frequently in female (p < 0.001), never-smokers (p < 0.001), adenocarcinoma (p < 0.001), low grade (p = 0.013) than Wt lesions. Ex19 occurred more frequently in female (p = 0.016), never-smokers (p = 0.008), adenocarcinoma (p < 0.001), low grade (p = 0.025) than Wt lesions. Ex 21 lesions (p = 0.026) had larger lepidic components than Wt lesions. Wt lesions had larger mucinous variant components than Ex21 lesions (p = 0.045) and Ex19 lesions (p = 0.015). Ex21 lesions were associated with lower pretreatment neutrophil: lymphocyte ratio (NLR) than Wt lesions (p = 0.017). The recurrent sites and DFS were similar among patients with Wt, Ex19 and Ex21.
Similar content being viewed by others
Introduction
In the last decades, with the progress of targeted therapies in non-small cell lung cancer (NSCLC), the treatment paradigm has been changed for patients with metastatic NSCLC. The epidermal growth factor receptor (EGFR) gene mutations status are with key determinant when using small molecule tyrosine kinase inhibitors (TKIs) for NSCLC patients. EGFR mutations are found in 30% to 50% of lung adenocarcinomas, with the most common mutations being deletion in exon 19 (Ex19 in 45% patients) and a mutation in exon 21 L858R point (Ex21 in 40% patients). Both mutations are referred to as sensitizing EGFR mutations1,2. Based on the results of eight classic phase 3 randomized trials (IPASS, FIRST-SIGNAL, OPTIMAL, EURTAC, WJTOG3405, NEJ002, LUX-Lung 3, LUX-Lung 6)3,4,5,6,7,8,9,10 in which both the first-generation (gifitinib, erlotinib) and second-generation (afatinib) of EGFR TKIs have demonstrated increased PFS and response rates than chemotherapy for patients harboring sensitive EGFR mutations, the role of EGFR TKIs have been established as first-line therapy for advanced NSCLC with sensitizing EGFR mutations.
Although the predictive effects of sensitive EGFR mutations-Ex19 and Ex21-are well defined, accumulating data have shown clinical differences between Ex19 and Ex21. Several studies have reported that patients with Ex19 had better survival outcomes than those with Ex21 in advanced NSCLC11,12. However, little reports has evaluated these differences in surgically resected NSCLC.
In 2011, the International Association for the Study of Lung Cancer (IASLC)/American Thoracic Society (ATS)/European Respiratory Society (ERS) proposed an international classification for lung adenocarcinoma (2011IASLC/ATS/ERS classification)13. The system divides adenocarcinoma into adenocarcinoma in situ (AIS), minimally invasive adenocarcinoma (MIA), invasive adenocarcinoma (InvAd)-lepidic predominant (LP), InvAd-acinar predominant (AP), InvAd -papillary predominant (PP), InvAd-micropapillary predominant (MP), InvAd-solid predominant (SP), and InvAd-mucinous variant (MV). Previous studies have reported differences features according to the 2011IASLC/ATS/ERS classification between EGFR mutant (Mt) and EGFR wild-type (Wt) resected lung adenocarcinoma. But the conclusions were inconsistent14,15,16.
In this study, we aimed to investigate the differences of clinicopathological features as well as survival outcomes among Ex19, Ex21, and Wt lesions in surgically resected NSCLC. In addition, we analyzed the association between the EGFR mutation status and histological subtypes in the subgroup of lung adenocarcinoma according to the 2011IASLC/ATS/ERS classification.
Results
Descriptive characteristics
A total of 198 patients were enrolled in this study: 53 patients (26.8%) with Ex19 lesions, 51 patients (25.8%) with Ex21 lesions, and 94 patients (47.4%) with Wt lesions. The median age at diagnosis was 61 years (range: 26–77). There were 97 (49%) male and 101 (51%) female. The number of patients in stages I–III was 100, 36, and 62 respectively. Thirty-two (16.2%) patients were diagnosed with squamous carcinoma, 161 (81.3%) with adenocarcinoma, and 5 (2.5%) with adenosquamous carcinoma. Thirty-seven (18.7%), 131 (66.2%), and 30 (15.2%) tumors were poorly, moderately, and well differentiated, respectively. One hundred and twelve (56.6%) patients received adjuvant chemotherapy (cisplatinum-based doublets) after operation, and among these patients, the mean cycle of chemotherapy is 3.91 (from 1 to 4). In patients with sensitive mutations, none of them received targeted therapy after operation since there was no indication of EGFR TKIs in the postoperative adjuvant therapy for NSCLC.
Correlation between EGFR mutation status and clinicopathological features
As shown in Table 1, clinicopathological features were compared among patients with the 3 EGFR statuses. Ex21 occurred more frequently in female (p < 0.001), never-smokers (p < 0.001), adenocarcinoma (p < 0.001), low grade (p = 0.013) than Wt lesions. Ex19 occurred more frequently in female (p = 0.016), never-smokers (p = 0.008), adenocarcinoma (p < 0.001), low grade (p = 0.025) than Wt lesions. Ex21 occurred more frequently in never-smokers (p = 0.041) than Ex19. There were no significant differences in age, T stage, N stage, or tumor size among the 3 groups.
Correlation between EGFR mutation status and laboratory parameters
As shown in Table 2, laboratory parameters were compared among patients with the 3 EGFR statuses. Ex21 lesions were associated with lower pretreatment NLR than Wt lesions (p = 0.017). While there were no significant differences in CEA, HGB, PLT, or white cell among the 3 groups.
Correlation between EGFR mutation status and survival outcome
Till December 31, 2015, 74 patients were diagnosed with recurrent or metastatic tumors after surgery. Of the 74 patients, 36 patients had local or lymphatic recurrence, 19 patients had bone metastasis, 14 patients had brain metastasis, 1 patients had adrenocortical metastasis, 2 patients had chest wall metastasis, and 2 patients had liver metastasis. There were no significant differences in recurrent or metastatic sites among the 3 groups (Table 3).
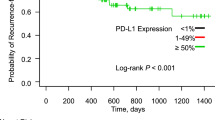
Till December 31, 2015, 191 patients’ DFS data were obtained and 7 patients’ data were censored. The median follow-up was 30.0 months (ranging from 1.7 to 43.9 months). The median DFS were 33.6, 29.4, and 25.7 months for patients with Wt, Ex19, and Ex21 lesions, respectively. There were no significant difference in DFS among the three groups (p = 0.941) (Fig. 1).
Correlation between EGFR mutation status and pathological subtypes in adenocarcinoma
In the subgroup of 161 patients with adenocarcinoma, we compared the pathological subtypes based on the 2011IASLC/ATS/ERS classification among the three EGFR mutation groups. The most common histological subtype was InvAd-AP (43.5%), followed by InvAd-PP (19.9%), InvAd-LP (13.0%), InvAd-SP (11.2%), and InvAd-MV (7.5%). Other subtypes included one MIA, one AIS and five InvAd-MP. There were 100% of AIS, 81.0% of InvAd-LP, 68.8% of InvAd-PP, 62.9% of InvAd-AP, 60% of InvAd-MP, 44.4% of InvAd-SP, and 23.1% of InvAd-MV subtype were Mt tumors. Ex21 mutations occurred at approximately twice the incidence rate of Ex19 mutations in InvAd-SP and InvAd-MV subtype tumors. Ex19 mutations occurred at approximately twice the incidence rate of Ex21 mutations in InvAd-PP subtype tumors (Figs 2 and 3).
As shown in Table 4, Ex21 lesions (p = 0.026) had larger lepidic components than Wt lesions. Wt lesions had larger mucinous variant components than Ex21 lesions (p = 0.045) and Ex19 lesions (p = 0.015). There were no significant difference in components of other subtypes among the three groups.
Discussion
At present, we are entering the age of precise medicine for cancer treatment. In recent years, NSCLC, especially lung adenocarcinoma has been found to harbor mutations or rearrangements of specific driver oncogenes, which are used to predict the therapeutic effect of relevant targeted inhibitors17,18. The most landmark example is that the EGFR mutation status can predict the efficacy of EGFR TKIs. EGFR is a transmembrane receptor tyrosine kinase with extracellular ligand-binding domain, a lipophilic transmembrane region and an intracellular regulatory domain with tyrosine kinase activity. It has been demonstrated that the signaling pathways of EGFR are essential for different cell functions. Mutations of the EGFR genes may result in persistent activation of the tyrosine kinase which could promote proliferation, angiogenesis, invasion, and metastasis of tumor cells in NSCLC19,20. The two most common sensitive mutations that account for more than 85% of all EGFR gene mutations are Ex19 and Ex21. Several researches have explored clinicopathological differences and prognostic value between Wt and Mt tumors21,22,23,24, till now, few studies have compared differences between Ex19 and Ex21. In this study, we for the first time investigate the differences of clinicopathological features as well as survival outcomes among Ex19, Ex21, and Wt lesions in surgically resected NSCLC.
Previous studies have demonstrated that EGFR mutations are commonly observed in a subset of NSCLC patients with the following features: nonsmoker, female, adenocarcinoma, and well- or moderately differentiated tumor cells25,26. In our study, Ex21 occurred more frequently in female, never-smokers, adenocarcinoma, and low grade tumors than Wt. While the frequencies of female, never-smokers, adenocarcinoma, and low grade tumors with Ex19 tumors were intermediate between the values for Ex21 and Wt tumors. In addition, Ex21 occurred more frequently in never-smokers than Ex19.
Neutrophils in tumor microenvironment have been shown to interact with tumor cells producing cytokines and chemokines, which influence tumor cell growth, angiogenesis and metastasis. In contrast to neutrophils, lymphocytes generally act as the host defense against tumor27,28. Elevated pretreatment NLR has been proved associated with the poor prognosis of patients with lung cancer29. For all we know, so far there has been none of study reported the correlation between NLR and EGFR mutation status. Our study for the first time demonstrated that Ex21 lesions were associated with lower pretreatment NLR than Wt lesions, while the proportion of lower NLR with Ex19 tumors were intermediate between the values for Ex21 and Wt tumors. It is currently believed that inflammatory cells in the tumor microenvironment play a significant role in tumor development. Further evaluation is necessary to examine the interaction and related mechanism between EGFR mutation status and host-derived stromal tissues as well as host immune cells.
The prognostic value of EGFR mutations in resected NSCLC remains controversial. Lee et al.21 analyzed 117 patients with surgically resected pulmonary adenocarcinoma and found that patients with EGFR mutations had longer DFS than those with Wt. Similarly, D’Angelo et al.30 analyzed 1118 patients with surgically resected NSCLC and found that patients with EGFR mutations had longer OS than those with Wt. Conversely, some studies revealed that EGFR mutation had no prognostic value for resected NSCLC. Liu et al.23 investigated 131 patients with resected pulmonary adenocarcinoma and the result showed that there was no significant correlation between EGFR mutation status and DFS, OS. Several article reported different predictive and prognostic value between Ex21 and Ex19 in advanced NSCLC. Liu et al.23 analyzed 131 patients with resected pulmonary adenocarcinoma and found that patients with Ex19 had longer DFS than those with Ex21. Conversely, Shigemastsu et al.26 analyzed 62 patients with early-stage NSCLC who underwent resections and found that patients with Ex21 had longer survival time than those with Ex19. In our study, there were no significant difference in DFS among patients with Ex21, Ex19 and Wt. In addition, there were no significant differences in recurrent or metastatic sites among the 3 groups.
Subclassification of lung adenocarcinoma based on the 2011IASLC/ATS/ERS classification had different prognosis. According to previous report, AIS and MIA are classified into low grade; InvAd-LP, InvAd-PP, and InvAd-AP are classified into intermediated grade; and InvAd-SP, InvAd-MP, InvAd-MV are classified into high grade31. Yanagawa et al.15 compared histological subtypes of adenocarcinoma between 131 Mt tumors and 110 Wt tumors. In their report, there were 62% of AIS, 60% of MIA, 77% of InvAd-LP, 49% of InvAd-AP, 50% of InvAd-PP, 28% of InvAd-SP, and 43% of InvAd-MP subtype were Wt tumors, which were incompletely similar to our results. In our study, there were 100% of AIS, 81.0% of InvAd-LP, 68.8% of InvAd-PP, 62.9% of InvAd-AP, 60% of InvAd-MP, 44.4% of InvAd-SP, and 23.1% of InvAd-MV subtype were Mt tumors.
Several studies reported that Mt tumors comprised more commonly the InvAd-LP subtype of lung adenocarcinoma14,16,32. In our study, Mt tumors also more commonly comprised the InvAd-LP subtype than Wt tumors. Several studies reported that Mt tumors comprised more commonly the InvAd-MP subtype of lung adenocarcinoma33,34. In our study, Wt tumors more commonly comprised the InvAd-MV subtype. Few studies have compared histologic subtypes based on 2011IASLC/ATS/ERS classification between Ex19 and Ex21. Yoshizawa et al.14 compared 48 Ex19 tumors and 36 Ex21 tumors and found that there were no significant differences in histologic subtypes of adenocarcinoma between Ex19 and Ex21. Villa et al.35 reported that Ex21 tumors was associated with InvAd-LP subtype when they compared 22 Ex19 tumors and 12 Ex21 tumors. In our study, Ex21 mutations occurred at approximately twice the incidence rate of Ex19 mutations in InvAd-SP and InvAd-MV subtype tumors. Ex19 mutations occurred at approximately twice the incidence rate of Ex21 mutations in InvAd-PP subtype tumors. Both Ex19 and Ex21 lesions had smaller mucinous variant components than Wt lesions. Ex21 lesions had larger lepidic growth components than Wt lesions.
While no significant difference in DFS was observed, the clinicopathological features were different among Wt, Ex19 and Ex21 in early-stage NSCLC who underwent resections. Both Ex19 and Ex21 occurred more frequently in female, never-smokers, adenocarcinoma, low-grade tumors than Wt lesions. Ex21 occurred more frequently in never-smokers than Ex19. Ex21 lesions were associated with lower pretreatment NLR than Wt lesions. Both Ex19 and Ex 21 lesions had smaller mucinous variant components than Wt lesions. Ex 21 lesions had larger lepidic growth components than Wt lesions.
Methods
Patients Enrollment
From January 1, 2011 to December 31, 2013, 1775 patients received lung tumors resection with curative intent in Zhejiang Cancer Hospital, Hangzhou, China. Study protocols were approved by the Ethical Review Community of Zhejiang Cancer Hospital. The requirement of informed consent was waived by the committee as it was a retrospective research. All experiments were performed in accordance with the approved guidelines. Subjects eligible for this study had to meet the following criteria: pathologically confirmed NSCLC; surgical specimens for EGFR mutational test were conducted. Patients who received neoadjuvant chemotherapy were excluded. Of the 1775 patients, the EGFR mutation status was analyzed in 209 patients (11.8%). Of the 209 patients, 198 patients were enrolled in this study: 53 patients (26.8%) with Ex19 lesions, 51 patients (25.8%) with Ex21 lesions, and 94 patients (47.4%) with Wt lesions. The 11 patients with other mutation statuses were excluded: 6 patients (2.9%) with G719X mutations in exon 18, 3 patients (1.4%) with L861Q mutations in exon 21, and 2 patients (1.0%) with exon 20 insertions.
EGFR Mutation Analysis
Genomic DNA was isolated and purified from formalin-fixed paraffin-embedded tissues using the GTpure FFPE Tissue DNA Extraction Kit (GeneTech, Shanghai, China) in accordance with the manufacturer’s instructions. A fragment method was used to detect Ex19/exon 20 insertion. Mt genes were amplified by polymerase chain reaction. To detect exon 18 mutations (G719X), and exon 21 mutations (L858R and L861Q), the Cycleave method was used based on the basic principle of realtime polymerase chain reaction. Each PCR assay contained forward and reverse primers (each 4 pmol), 2 μl template DNA solution, and 2 units of Hot-Start Taq DNA polymerase (Takara, Shiga Japan) in a 40 ml volume. The PCR conditions consisted of initial denaturation at 95 °C for 3 min; 50 cycles of 95 °C for 15 s, annealing at 56 °C for 30 s and 72 °C for 30 s; and final extension at 72 °C for 5 min. The PCR products were sequenced using the Pyrosequencing PyroMark ID system (Qiagen, Hilden, Germany) following the manufacturer’s instructions.
Clinicopathological Variables and Laboratory Parameters
Clinicopathological data collected for analysis included age at diagnosis, gender, smoking history, tumor size, pathological TNM stage (the seventh edition of the lung cancer staging classification system), pathological types, tumor differentiation, pleural invasion, vessel invasion and histological subtypes of adenocarcinoma according to the 2011IASLC/ATS/ERS multidisciplinary classification of lung adenocarcinoma.
Laboratory data collected for analysis included pretreatment peripheral carcinoembryonic antigen (CEA), haemoglobin (HGB), platlet (PLT), white cell, and neutrophil : lymphocyte ratio (NLR).
Statistical Analysis
Statistical analysis was performed using SPSS22.0 package. Continuous variables among the 3 EGFR mutation groups were compared using analysis of variance and post hoc comparisons test (Tukey test). We analyzed the association between categorical variables and EGFR mutation status using the Chi-Square test. Whenever it was possible and when the expected value in any of the tests was less than 5, the Fisher exact test was used. A 2-way analysis was performed in all comparisons. Survivals were analyzed using the Kaplan –Meier method and were compared using the log-rank test. Statistical significance was defined as when P < 0.05.
Additional Information
How to cite this article: Jin, Y. et al. Differences among lesions with exon 19, exon 21 EGFR mutations and wild types in surgically resected non-small cell lung cancer. Sci. Rep. 6, 31636; doi: 10.1038/srep31636 (2016).
References
Ge, L. & Shi, R. Progress of EGFR-TKI and ALK/ROS1 inhibitors in advanced non-small cell lung cancer. International journal of clinical and experimental medicine 8, 10330–10339 (2015).
Russo, A. et al. A decade of EGFR inhibition in EGFR-mutated non small cell lung cancer (NSCLC): Old successes and future perspectives. Oncotarget 6, 26814–26825, 10.18632/oncotarget.4254 (2015).
Fukuoka, M. et al. Biomarker analyses and final overall survival results from a phase III, randomized, open-label, first-line study of gefitinib versus carboplatin/paclitaxel in clinically selected patients with advanced non-small-cell lung cancer in Asia (IPASS). Journal of clinical oncology: official journal of the American Society of Clinical Oncology 29, 2866–2874, 10.1200/JCO.2010.33.4235 (2011).
Han, J. Y. et al. First-SIGNAL: first-line single-agent iressa versus gemcitabine and cisplatin trial in never-smokers with adenocarcinoma of the lung. Journal of clinical oncology: official journal of the American Society of Clinical Oncology 30, 1122–1128, 10.1200/JCO.2011.36.8456 (2012).
Zhou, C. et al. Erlotinib versus chemotherapy as first-line treatment for patients with advanced EGFR mutation-positive non-small-cell lung cancer (OPTIMAL, CTONG-0802): a multicentre, open-label, randomised, phase 3 study. The Lancet. Oncology 12, 735–742, 10.1016/S1470-2045(11)70184-X (2011).
Rosell, R. et al. Erlotinib versus standard chemotherapy as first-line treatment for European patients with advanced EGFR mutation-positive non-small-cell lung cancer (EURTAC): a multicentre, open-label, randomised phase 3 trial. The Lancet. Oncology 13, 239–246, 10.1016/S1470-2045(11)70393-X (2012).
Mitsudomi, T. et al. Gefitinib versus cisplatin plus docetaxel in patients with non-small-cell lung cancer harbouring mutations of the epidermal growth factor receptor (WJTOG3405): an open label, randomised phase 3 trial. The Lancet. Oncology 11, 121–128, 10.1016/S1470-2045(09)70364-X (2010).
Inoue, A. et al. Updated overall survival results from a randomized phase III trial comparing gefitinib with carboplatin-paclitaxel for chemo-naive non-small cell lung cancer with sensitive EGFR gene mutations (NEJ002). Annals of oncology: official journal of the European Society for Medical Oncology/ESMO 24, 54–59, 10.1093/annonc/mds214 (2013).
Sequist, L. V. et al. Phase III study of afatinib or cisplatin plus pemetrexed in patients with metastatic lung adenocarcinoma with EGFR mutations. Journal of clinical oncology: official journal of the American Society of Clinical Oncology 31, 3327–3334, 10.1200/JCO.2012.44.2806 (2013).
Wu, Y. L. et al. Afatinib versus cisplatin plus gemcitabine for first-line treatment of Asian patients with advanced non-small-cell lung cancer harbouring EGFR mutations (LUX-Lung 6): an open-label, randomised phase 3 trial. The Lancet. Oncology 15, 213–222, 10.1016/S1470-2045(13)70604-1 (2014).
Rosell, R. et al. Screening for epidermal growth factor receptor mutations in lung cancer. The New England journal of medicine 361, 958–967, 10.1056/NEJMoa0904554 (2009).
Yang, J. C. et al. Afatinib versus cisplatin-based chemotherapy for EGFR mutation-positive lung adenocarcinoma (LUX-Lung 3 and LUX-Lung 6): analysis of overall survival data from two randomised, phase 3 trials. The Lancet. Oncology 16, 141–151, 10.1016/S1470-2045(14)71173-8 (2015).
Travis, W. D. et al. International association for the study of lung cancer/american thoracic society/european respiratory society international multidisciplinary classification of lung adenocarcinoma. Journal of thoracic oncology: official publication of the International Association for the Study of Lung Cancer 6, 244–285, 10.1097/JTO.0b013e318206a221 (2011).
Yoshizawa, A. et al. Validation of the IASLC/ATS/ERS lung adenocarcinoma classification for prognosis and association with EGFR and KRAS gene mutations: analysis of 440 Japanese patients. Journal of thoracic oncology: official publication of the International Association for the Study of Lung Cancer 8, 52–61, 10.1097/JTO.0b013e3182769aa8 (2013).
Yanagawa, N. et al. The correlation of the International Association for the Study of Lung Cancer (IASLC)/American Thoracic Society (ATS)/European Respiratory Society (ERS) classification with prognosis and EGFR mutation in lung adenocarcinoma. The Annals of thoracic surgery 98, 453–458, 10.1016/j.athoracsur.2014.04.108 (2014).
Ninomiya, H. et al. Correlation between morphology and EGFR mutations in lung adenocarcinomas Significance of the micropapillary pattern and the hobnail cell type. Lung cancer 63, 235–240, 10.1016/j.lungcan.2008.04.017 (2009).
Boolell, V., Alamgeer, M., Watkins, D. N. & Ganju, V. The Evolution of Therapies in Non-Small Cell Lung Cancer. Cancers 7, 1815–1846, 10.3390/cancers7030864 (2015).
Ryska, A. et al. [Molecular diagnostics of lung cancer]. Magyar onkologia 59, 259–266 (2015).
Franklin, W. A., Veve, R., Hirsch, F. R., Helfrich, B. A. & Bunn, P. A. Jr. Epidermal growth factor receptor family in lung cancer and premalignancy. Seminars in oncology 29, 3–14 (2002).
Bunn, P. A. Jr. & Franklin, W. Epidermal growth factor receptor expression, signal pathway, and inhibitors in non-small cell lung cancer. Seminars in oncology 29, 38–44, 10.1053/sonc.2002.35646 (2002).
Lee, Y. J. et al. Activating mutations within the EGFR kinase domain: a molecular predictor of disease-free survival in resected pulmonary adenocarcinoma. Journal of cancer research and clinical oncology 135, 1647–1654, 10.1007/s00432-009-0611-7 (2009).
Jeon, J. H. et al. Prognostic and predictive role of epidermal growth factor receptor mutation in recurrent pulmonary adenocarcinoma after curative resection. European journal of cardio-thoracic surgery: official journal of the European Association for Cardio-thoracic Surgery 47, 556–562, 10.1093/ejcts/ezu177 (2015).
Liu, W. S. et al. Prognostic value of epidermal growth factor receptor mutations in resected lung adenocarcinomas. Medical oncology 31, 771, 10.1007/s12032-013-0771-9 (2014).
Kosaka, T. et al. Mutations of the epidermal growth factor receptor gene in lung cancer: biological and clinical implications. Cancer research 64, 8919–8923, 10.1158/0008-5472.CAN-04-2818 (2004).
Lynch, T. J. et al. Activating mutations in the epidermal growth factor receptor underlying responsiveness of non-small-cell lung cancer to gefitinib. The New England journal of medicine 350, 2129–2139, 10.1056/NEJMoa040938 (2004).
Shigematsu, H. et al. Clinical and biological features associated with epidermal growth factor receptor gene mutations in lung cancers. Journal of the National Cancer Institute 97, 339–346, 10.1093/jnci/dji055 (2005).
Kusumanto, Y. H., Dam, W. A., Hospers, G. A., Meijer, C. & Mulder, N. H. Platelets and granulocytes, in particular the neutrophils, form important compartments for circulating vascular endothelial growth factor. Angiogenesis 6, 283–287, 10.1023/B:AGEN.0000029415.62384.ba (2003).
Fridlender, Z. G. et al. Polarization of tumor-associated neutrophil phenotype by TGF-beta: “N1” versus “N2” TAN. Cancer cell 16, 183–194, 10.1016/j.ccr.2009.06.017 (2009).
Cedres, S. et al. Neutrophil to lymphocyte ratio (NLR) as an indicator of poor prognosis in stage IV non-small cell lung cancer. Clinical & translational oncology: official publication of the Federation of Spanish Oncology Societies and of the National Cancer Institute of Mexico 14, 864–869, 10.1007/s12094-012-0872-5 (2012).
D’Angelo, S. P. et al. Distinct clinical course of EGFR-mutant resected lung cancers: results of testing of 1118 surgical specimens and effects of adjuvant gefitinib and erlotinib. Journal of thoracic oncology: official publication of the International Association for the Study of Lung Cancer 7, 1815–1822, 10.1097/JTO.0b013e31826bb7b2 (2012).
Yoshizawa, A. et al. Impact of proposed IASLC/ATS/ERS classification of lung adenocarcinoma: prognostic subgroups and implications for further revision of staging based on analysis of 514 stage I cases. Modern pathology: an official journal of the United States and Canadian Academy of Pathology, Inc 24, 653–664, 10.1038/modpathol.2010.232 (2011).
Sonobe, M., Manabe, T., Wada, H. & Tanaka, F. Mutations in the epidermal growth factor receptor gene are linked to smoking-independent, lung adenocarcinoma. British journal of cancer 93, 355–363, 10.1038/sj.bjc.6602707 (2005).
Zhang, Y. et al. A comprehensive investigation of molecular features and prognosis of lung adenocarcinoma with micropapillary component. Journal of thoracic oncology: official publication of the International Association for the Study of Lung Cancer 9, 1772–1778, 10.1097/JTO.0000000000000341 (2014).
Shim, H. S., Lee da, H., Park, E. J. & Kim, S. H. Histopathologic characteristics of lung adenocarcinomas with epidermal growth factor receptor mutations in the International Association for the Study of Lung Cancer/American Thoracic Society/European Respiratory Society lung adenocarcinoma classification. Archives of pathology & laboratory medicine 135, 1329–1334, 10.5858/arpa.2010-0493-OA (2011).
Villa, C. et al. Correlation of EGFR mutation status with predominant histologic subtype of adenocarcinoma according to the new lung adenocarcinoma classification of the International Association for the Study of Lung Cancer/American Thoracic Society/European Respiratory Society. Archives of pathology & laboratory medicine 138, 1353–1357, 10.5858/arpa.2013-0376-OA (2014).
Acknowledgements
This work was supported by Wu Jie Ping medical foundation (Grant No. 320.6750.13393).
Author information
Authors and Affiliations
Contributions
Y.J. prepared the manuscript and took responsibility for the statistical analysis; M.C. edited and reviewed the manuscript; X.Y. designed the study and took responsibility for the integrity of the data.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing financial interests.
Rights and permissions
This work is licensed under a Creative Commons Attribution 4.0 International License. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in the credit line; if the material is not included under the Creative Commons license, users will need to obtain permission from the license holder to reproduce the material. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/
About this article
Cite this article
Jin, Y., Chen, M. & Yu, X. Differences among lesions with exon 19, exon 21 EGFR mutations and wild types in surgically resected non-small cell lung cancer. Sci Rep 6, 31636 (2016). https://doi.org/10.1038/srep31636
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/srep31636
This article is cited by
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.