Abstract
Larger serving sizes and more frequent eating episodes have been implicated in the rising prevalence of obesity at a population level. This study examines the relative contributions of meal size and frequency to weight gain in a large sample of British children. Using 3-day diet diaries from 1939 children aged 21 months from the Gemini twin cohort, we assessed prospective associations between meal size, meal frequency and weight gain from two to five years. Separate longitudinal analyses demonstrated that every 10 kcal increase in meal size was associated with 1.5 g/wk or 4% (p = 0.005) faster growth rate, while meal frequency was not independently associated with growth (β = 0.3 g/wk p = 0.20). Including both meal parameters in the model strengthened associations (meal size: β = 2.6 g/wk, p < 0.001; meal frequency: β = 1.0 g/wk, p = 0.001). Taken together, the implication is that meal size promotes faster growth regardless of frequency, but meal frequency has a significant effect only if meal size is assumed to be held constant. Clearer advice on meal size and frequency, especially advice on appropriate meal size, may help prevent excess weight gain.
Similar content being viewed by others
Introduction
Obesity rates have risen dramatically over the past 30 years, with increases in childhood obesity provoking particular concern1. The causes of this secular trend are likely to be multiple and complex; evidence indicates that, children are now consuming food more often, and in larger amounts at each occasion2. However, even in the pervasively ‘obesogenic’ environment, individuals vary considerably in weight, making it important to understand the individual behaviours associated with obesity risk. The behaviours that underlie population trends in weight cannot be assumed to explain individual differences.
Overconsumption might occur through eating too often and/or eating too much each time. There is some evidence for cross-sectional associations between weight and the amount of food consumed per eating occasion. Several studies have shown that adults who are obese tend to consume larger meals3,4,5. In children, one analysis of data from the Continuing Surveys of Food Intakes by Individuals (1994–1998) found that meal size (energy consumed per meal) was associated with weight centile in six to 19 year-olds, but not three to five year-olds6; another analysis of the same dataset found a linear association between consumed serving sizes (grams consumed per meal) and weight z-scores in one to two year-olds7. There are no longitudinal studies exploring the role of meal size in pediatric weight gain.
There is inconsistent evidence of the relationship between meal frequency and weight. A systematic review found no evidence of an association between eating frequency and weight in adults or children8, while a meta-analysis of 11 studies in children and adolescents found an inverse association between meal frequency and weight9. The only longitudinal analysis in children found that higher eating frequency at nine years was associated with lower weight gain over a ten year follow-up10. There are no longitudinal studies of meal frequency and weight gain in young children.
No study has examined meal size (energy consumed) and meal frequency in the same sample over the same recording period, making it difficult to determine their relative contribution to excess weight gain or obesity risk. There are no prospective studies in young children. We therefore examined associations between the size and frequency of eating occasions and weight gain, using a longitudinal design, in a large cohort of preschool children. We also examined differences in meal parameters by weight status at baseline to provide insights into differences in eating patterns between overweight and healthy weight children.
Methods
Study population
We used data from Gemini; a prospective birth cohort of twins set up to examine early growth. The UK Office for National Statistics asked all families with live twin births in England and Wales between March and December 2007 (N = 6754) if their contact details could be passed to the Gemini research team. 3435 (39%) agreed, and 2402 (70% of those contacted; 36% of all births) consented and completed baseline questionnaires. Gemini is comparable to national twin statistics on sex, gestational age, and birth weight11,12; but the twins were born earlier and had a lower weight than singletons12. Parents provided written informed consent, and the study was approved by the University College London Committee for the Ethics of Non-National Health Service Human Research. The methods were carried out in accordance with the approved guidelines.
Dietary data collection
At 21 months of age, diet diaries were mailed to families, inviting them to record all foods and drinks consumed by both children over three days (two weekdays and 1 weekend day). Diaries were returned for 2714 children (56.5%). We provided detailed instructions, and portion guides adapted from the British Preschool Food Atlas13, to illustrate how to accurately record consumption. Diaries were checked, coded, and linked with British food composition tables14 to estimate energy and nutrient intake using Diet In Nutrients Out15.
‘Meals’ were defined as eating occasions in which food was consumed at a single clock time (and drinks, if consumed at the same time). ‘Meal frequency’ was the number of meals per day, and ‘meal size’ the average energy consumed per meal (total energy consumed in eating occasions/eating frequency), averaged over three days. To estimate whether meal composition differed by weight status at baseline (two years of age), we calculated and compared meal weight (g) and composition (percentage of energy (%E) from protein, carbohydrate and fat), and energy density (kcal/g, with and without drinks included), for normal weight and overweight children.
Anthropometric measures
We used health visitor records (kept routinely up to two years of age) where possible. From two years families were sent electronic weighing scales (Tanita UK Ltd, Yewsley, UK) and a height chart, and were asked to weigh and measure their children every three months.
The longitudinal analysis used all available weight measurements between two to five years, with weight gain (kg/week) as the primary outcome measure. The cross-sectional analysis used weight at two years as the baseline measure. All children in the UK have a two year health assessment by a health visitor so considerably more weight data were available at this age (n = 1711) compared with 21 months (n = 960). If two year weight was missing it was replaced with the next available weight up to 27 months or the previously available weight after 21 months. Children were classified as overweight or normal weight at baseline using weight Standard Deviations Scores (SDS), calculated using LMS Growth macro for Excel16. For the reference population, mean SDS is 0 and the standard deviation 1; SDS > 0 indicates higher weight, and SDS < 0 indicates lower weight compared to reference children of the same age, sex and gestational age. Overweight was classified as a weight SDS > 1.04; above the 85th percentile.
Demographic and background information
Parents reported child sex, date of birth, birth weight, ethnicity (dichotomised into white and non-white). Parent-held health professional records provided maternal education (dichotomised into lower; no university education, and higher; university education) and gestational age.
Statistical analyses
We excluded children without three days of diary entries (n = 378), and those missing weight data at baseline and at least two additional measurements between two to five years (n = 356), gestational age (n = 4), and birth weight (n = 41); leaving 1939 children for analyses; 40% of the baseline sample. Figure 1 shows the flow of included in the analyses. The analysis sample included more mothers of white ethnicity, and were educated to a higher level than non-responders (n = 2865).
Multilevel mixed-effects linear regression explored longitudinal relationships between meal parameters (meal size and frequency) and growth up to five years. All weight measurements of the 1939 children are taken account of. Three-level hierarchical models, accounting for clustering of weight measurements within the child and family, regressed weight on age, sex and relevant dietary measures and their interactions with age, using Stata version 1317. The contribution of meal size (per 10 kcals) and meal frequency (per meal) to weekly weight gain (kg and %), in addition to the mean base growth rate of 0.036 kg/wk (coefficient of age in the multi-level model; the growth rate observed in the sample assuming no contribution from dietary intake) was assessed. Two models were run with each meal parameter separately, and a third model was run with both meal parameters included to account of the negative correlation between meal size and frequency (r = −0.55, p < 0.001). An interaction between meal size and frequency was tested by including a product term in the model. Complex Samples General Linear Models (CSGLMs), accounting for clustering of twins within families, examined associations between meal parameters and weight (kg) at baseline (age two years). Two CSGLMs were run with each meal parameter separately; a third model included both meal parameters. CSGLMS also explored mean differences in meal parameters (meal size, frequency and composition) and daily energy intake, by baseline weight status (overweight vs normal weight). Pearson’s correlation established the relationship between meal size (kcals) and meal weight (g) to explore the relationship between meal weight and energy intake.
Birth weight, sex, gestational age, and difference in age between diet diary completion and weight measurement were included as potential confounders. Longitudinal models were additionally adjusted for baseline weight to control for differences in subsequent growth rate driven by earlier weight.
Results
Demographics
Sample characteristics are shown in Table 1. There were an equal number of girls (51.2%) and boys and most children were of white ethnic background (95.8%). Children were on average 20.6 months (SD = 1.09) at diary completion, and 24.3 months at baseline weight (two years) measurement. At baseline, the prevalence of overweight/obesity (weight SDS > 1.04) was 17.2%.
Meal size, meal frequency and weight gain
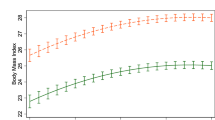
Table 2 shows that when each meal parameter was assessed separately, variation between children in weight gain from two to five years was partly explained by meal size. For a 10 kcal increase in meal size at 21 months, a child’s growth rate increased by an additional 1.5 g/week, or 4%, above the average growth rate. Meal frequency was not associated with weight gain (ß = 0.3, p = 0.20). However, in the model that included both meal parameters, higher meal frequency was associated with greater weight gain (ß = 1.0; p = 0.001); such that supposing meal sizes were held fixed, each extra meal increased a child’s growth rate by 1 g/week or 2.9%. Furthermore, the association between meal size and weight gain almost doubled (ß = 2.6; p < 0.001) from a 4% increase in weight gain for every 10 kcal increase in meal size, to 7.3%. There was no evidence of interaction between meal size and meal frequency (p = 0.06).
Meal size, meal frequency and baseline weight and weight status
Table 2 demonstrates that in separate cross-sectional models, meal size was positively associated with weight at baseline (ß = 21; p = 0.002). For every additional 10 kcals consumed per meal, a child weighed 21 g more. Adjusting for meal frequency increased the association between meal size and weight (ß = 33; p < 0.001). Meal frequency was not associated with weight at baseline (ß = 3; p = 0.93); although weak evidence of association emerged when meal size was added to the model (ß = 95; p = 0.02). Results were unchanged using weight SDS as the outcome variable.
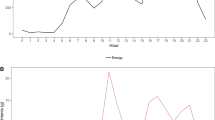
Associations between meal parameters and weight status at baseline are shown in Table 3. Overweight children consumed significantly larger meals (190 vs 178 kcals; p = 0.006) and had a greater energy intake (1092 vs 1026 kcals; p < 0.001) than normal weight children, but there was no difference in meal frequency (p = 0.72). The weight of meals (g) was higher in the overweight group (p = 0.002), and there was a significant correlation between meal size (kcals) and meal weight (g) (r = 0.73; p < 0.001). No other meal composition variables (protein, fat, carbohydrate or energy density) were associated with weight status (p-values all > 0.05). Larger meals predicted risk of overweight (OR 1.04; CI 1.01–1.07; p = 0.006); and results were largely unchanged when adjusting for meal frequency. Meal frequency was not associated with risk of overweight (p = 0.72), even when adjusting for meal size (p = 0.18), although the direction of the effect became positive, in line with the continuous associations (Table 4).
Discussion
This is the first study to explore the relative contributions of meal size and meal frequency on weight gain in young children. In a large sample of twins, larger meal size at 21 months was associated with greater weight gain from two to five years. Meal frequency was not associated with weight gain, except after adjustment for meal size.
Results suggest that young children gain more weight by eating larger amounts at each meal than eating more frequently. For every additional 10 kcals consumed per meal, a child’s growth rate was 4% above the average and the odds of being overweight at baseline was 6% greater.
Although our primary focus was the relationship between meal parameters and weight gain, we also explored associations at baseline; these supported the longitudinal findings. At baseline, meal size, but not meal frequency, was significantly associated with weight (kg). Meal frequency was weakly associated with weight when meal size was included in the model; but it was not associated with risk of overweight, with or without adjustment for meal size. Meal composition (proportions of protein, fat or carbohydrate, or energy density did not differ with weight status (p-values all > 0.05). Overweight children consumed more energy mostly by eating larger quantities of the same composition of food, suggesting a dominant role for meal size, rather than the type of food. The high Pearson’s correlation between meal size (kcals) and meal weight (g) supports this. This is an important issue in an environment where feeding advice often assumes that as long as children are given ‘healthy’ food, they can be left to choose how much to eat. It is sometimes even suggested that parental intrusion into the child’s food quantity decisions could be harmful. Overweight parents for example have been shown to engage in more restrictive feeding behaviours in young children which may result in poorer energy self-regulation and subsequent weight gain18. The moderating effect of factors such as parental weight status on children’s eating behaviours and subsequent weight gain is worth further exploration.
Experimental studies show that children consume more when served larger portions19,20, but there are few recent studies of consumed meal sizes in everyday life. Waxman & Stunkard (1980) observed food intake over four months in a small sample of families (n = 4), and found that obese boys ate substantially larger meals than their normal-weight sibling. Diet composition and meal frequency were not reported21. We and others have shown that heavier children exhibit poorer satiety responsiveness than their leaner counterparts22,23,24,25,26, We have demonstrated that children with poorer satiety responsiveness consume larger meals27, placing them at greater risk of excess weight gain. Numerous studies have also shown young children consume more when served larger portions19,28,29,30,31. Taken together, this might suggest that carers need to guard against ‘over-serving’.
One previous study found no association between weight and eating frequency in one to two year-olds7 and a recent meta-analysis found a negative association9. In the current study, meal frequency was not associated with weight gain, unless adjusted for meal size. No previous study has included both parameters concurrently, perhaps because information on meal size is typically lacking from questionnaire-based measures of meal frequency9. Here we show that meal size was associated with faster growth regardless of meal frequency, suggesting this is a key target for future studies to test public health guidance. Meal frequency only promotes faster growth if meal size remains constant. However, children eating more frequently typically ate smaller meals; thus increased eating frequency per se may not be a problem if meal size is reduced accordingly. The inter-play between guidance on meal size and frequency for weight requires further research.
Strengths of this study include detailed diary data, large sample, health professional measured weights for the first two years, and prospective weight data up to five years. Parents weighed and measured their children after two years, which could introduce error, although we previously showed high correlations between researcher- and parent-measured weights (0.83)32. Parental compliance with returning weight records reduced over time, but there was an average of six weight measurements per child after two years; with those with less than two measurements excluded from analyses. Our mixed-models analyses took advantage of all available data, and focused on growth rather than point estimates of overweight; however, the fitted model was likely to be biased towards earlier weights. Nevertheless, associations were essentially unchanged after adjusting for weight at baseline.
We did not have information on energy expenditure and were therefore unable to determine the independent contribution of energy intake on growth or explore the impact of under-reporting on meal parameters. Previous research suggests that adjustment for under-reporting could alter associations between meal frequency and weight, although over-reporting has been shown to be more prevalent at younger ages6.
Diet diaries were conducted at one time point so there is a lack of data on changes in diet over time. There is currently no consistent method of defining the parameters of eating occasions33,34,35,36 and we chose to denote a meal as any ‘eating occasion’ to avoid subjective judgements based on timing or content which could be unreliable for children of this age. An eating occasion included drinks consumed at the same time as food, which might have affected the energy density of the meal. However, meal energy density was not associated with weight or weight status, either with or without drinks included suggesting our definition of a meal was unaffected by the inclusion of drinks.
As with other cohort studies selection bias may have been introduced as the analysis sample consisted of 40% of the initial baseline Gemini sample, and the twin nature of the sample poses questions about generalizability to singletons. However the diets of children in Gemini are comparable to those recorded in a nationally representative sample37.
In conclusion, regardless of meal frequency, larger meal sizes contribute to excess weight in early childhood, and higher weight gain over the preschool years. There is a need for further research into how parental feeding practices and infant feeding behaviour may influence one another. Currently there is little guidance to parents on appropriate serving sizes for young children and an analysis of policies to promote healthy portion sizes in the US found this to be a neglected area38. More advice on feeding practices, including meal frequency and especially on meal size, may help prevent excess weight gain.
Additional Information
How to cite this article: Syrad, H. et al. Meal size is a critical driver of weight gain in early childhood. Sci. Rep. 6, 28368; doi: 10.1038/srep28368 (2016).
References
Onis, M. De, Blo, M. & Borghi, E. Global prevalence and trends of overweight and obesity among preschool children. Am. J. Clin. Nutr. 92, 1257–1264 (2010).
Duffey, K. J. & Popkin, B. M. Energy density, portion size, and eating occasions: contributions to increased energy intake in the United States, 1977–2006. PLoS Med. 8, e1001050 (2011).
Mills, J. P., Perry, C. D. & Reicks, M. Eating frequency is associated with energy intake but not obesity in midlife women. Obesity (Silver Spring) . 19, 552–9 (2011).
Pearcey, S. M. & de Castro, J. M. Food intake and meal patterns of weight-stable and weight-gaining persons. Am. J. Clin. Nutr. 76, 107–12 (2002).
Kant, A. K. & Graubard, B. I. Secular trends in patterns of self-reported food consumption of adult Americans: NHANES 1971–1975 to NHANES 1999–2002. Am. J. Clin. Nutr. 84, 1215–23 (2006).
Huang, T. T.-K., Howarth, N. C., Lin, B.-H., Roberts, S. B. & McCrory, M. a. Energy Intake and Meal Portions: Associations with BMI Percentile in U.S. Children. Obes. Res. 12, 1875–85 (2004).
McConahy, K. L., Smiciklas-Wright, H., Birch, L. L., Mitchell, D. C. & Picciano, M. F. Food portions are positively related to energy intake and body weight in early childhood. J. Pediatr. 140, 340–7 (2002).
Mesas, a. E., Muñoz-Pareja, M., López-García, E. & Rodríguez-Artalejo, F. Selected eating behaviours and excess body weight: a systematic review. Obes. Rev. 13, 106–35 (2012).
Kaisari, P., Yannakoulia, M. & Panagiotakos, D. B. Eating frequency and overweight and obesity in children and adolescents: a meta-analysis. Pediatrics 131, 958–67 (2013).
Ritchie, L. D. Less frequent eating predicts greater BMI and waist circumference. Am. J. Clin. Nutr. 95, 290–296 (2012).
Statistics, N., Buildings, G., Road, C., Office, M. & Centre, C. Office for National Statistics. Birth statistics series FM1 no. 35. Review of the Registrar General on births and patterns of family building in England andWales . Newport, United Kingdom: National Statistics, 2006 (2007).
Van Jaarsveld, C. H., Johnson, L., Llewellyn, C. & Wardle, J. Gemini: a UK twin birth cohort with a focus on early childhood weight trajectories, appetite and the family environment. Twin Res. Hum. Genet. 13, 72–8 (2010).
Foster, E., Hawkins, A. & Adamson, A. Young person’s food atlas—pre-school . London, UK: Food Standards Agency, 2010 (2010).
Food Standards Agency. McCance and Widdowson’s The Composition of Foods, Sixth Summary Edition . Royal Society of Chemistry, Cambridge (2002).
Fitt, E. et al. Disaggregating composite food codes in the UK National Diet and Nutrition Survey food composition databank. Eur. J. Clin. Nutr. 64 Suppl 3, S32–6 (2010).
Cole, T. J. et al. Software for LMS method: LMSGrowth program version 2.64. London, England: Child Growth Foundation . URL http://homepage.mac.com/tjcole/FileSharing1.html (2008).
StataCorp Stata Statistical Software: Release 13 . College Station, TX: StataCorp LP (2013).
Francis, L. a. & Birch, L. L. Maternal weight status modulates the effects of restriction on daughters’ eating and weight. Int. J. Obes. (Lond) . 29, 942–9 (2005).
Fisher, J. O., Arreola, A., Birch, L. L. & Rolls, B. J. Portion size effects on daily energy intake in low-income Hispanic and African American children and their mothers. Am. J. Clin. Nutr. 86, 1709–16 (2007).
Fisher, J. O. Effects of Age on Children’s Intake of Large and Self-selected Food Portions. Obesity 15, 403–412 (2007).
Waxman, M. & Stunkard, A. J. Caloric intake and expenditure of obese boys. J. Pediatr. 96, 187–193 (1980).
Webber, L., Hill, C., Saxton, J., Van Jaarsveld, C. H. M. & Wardle, J. Eating behaviour and weight in children. Int. J. Obes. (Lond) . 33, 21–8 (2009).
Jansen, A. et al. Overweight children overeat after exposure to food cues. Eat. Behav . 4, 197–209 (2003).
Carnell, S. & Wardle, J. Appetite and adiposity in children: evidence for a behavioral susceptibility theory of obesity. Am. J. Clin. Nutr. 88, 22–9 (2008).
Carnell, S. & Wardle, J. Appetitive traits in children. New evidence for associations with weight and a common, obesity-associated genetic variant. Appetite 53, 260–3 (2009).
van Jaarsveld, C. H., Llewellyn, C. H., Johnson, L. & Wardle, J. Prospective associations between appetitive traits and weight gain in infancy. Am. J. Clin. Nutr. 94, 1562–1567 (2011).
Syrad, H., Johnson, L., Wardle, J. & Llewellyn, C. H. Appetitive traits and food intake patterns in early life. Am. J. Clin. Nutr. 103, 231–235 (2015).
Fisher, J. O., Liu, Y., Birch, L. L. & Rolls, B. J. Effects of portion size and energy density on young children’s intake at a meal. Am. J. Clin. Nutr. 86, 174–179 (2007).
Mrdjenovic, G. & Levitsky, D. a. Children eat what they are served: the imprecise regulation of energy intake. Appetite 44, 273–82 (2005).
Fisher, J. O., Rolls, B. J. & Birch, L. L. Children’s bite size and intake of an entrée are greater with large portions than with age-appropriate or self-selected portions. Am J Clin Nutr 77, 1164–1170 (2003).
Looney, S. M. & Raynor, H. a. Impact of portion size and energy density on snack intake in preschool-aged children. J. Am. Diet. Assoc. 111, 414–8 (2011).
Wardle, J., Carnell, S., Haworth, C. M. & Plomin, R. Evidence for a strong genetic influence on childhood adiposity despite the force of the obesogenic environment. Am. J. Clin. Nutr. 87, 398–404 (2008).
Gatenby, S. J. Eating frequency: methodological and dietary aspects. Br. J. Nutr. 77 Suppl 1, S7–20 (1997).
Duval, K. & Doucet, É. Eating Frequency and Anthropometry. In Handbook of Anthropometry .Springer: New York (2012).
Oltersdorf, U., Schlettwein-gsell, D. & Winkler, G. Assessing eating patterns-an emerging research topic in nutritional sciences: introduction to the symposium. Appetite 32, 1–7 (1999).
Kerver, J. M., Yang, E. J., Obayashi, S., Bianchi, L. & Song, W. O. Meal and snack patterns are associated with dietary intake of energy and nutrients in US adults. J. Am. Diet. Assoc. 106, 46–53 (2006).
Syrad, H. et al. Energy and nutrient intakes of young children in the UK: findings from the Gemini twin cohort. Br. J. Nutr. 115, 1843–1850 (2016).
Pomeranz, J. L. & Miller, D. P. Policies to promote healthy portion sizes for children. Appetite 88, 50–8 (2015).
Cole, T. J., Freeman, J. V. & Preece, M. A. Body mass index reference curves for the UK, 1990. Arch. Dis. Child. 73, 25–9 (1995).
Acknowledgements
We would like to thank all the Gemini families that completed the diet diaries, and the Human Nutrition Research Unit, Cambridge, UK for coding the diaries.
Author information
Authors and Affiliations
Contributions
H.S., C.H.L., L.J., S.A.J., C.H.M.v.J. and J.W. contributed to the conception and design of the study. L.J. designed the diet diaries and coordinated the collection of dietary data. H.S. conducted the cross-sectional analyses and wrote the first draft of the manuscript. D.B. conducted the longitudinal analyses. All authors interpreted the findings and reviewed and revised the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing financial interests.
Rights and permissions
This work is licensed under a Creative Commons Attribution 4.0 International License. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in the credit line; if the material is not included under the Creative Commons license, users will need to obtain permission from the license holder to reproduce the material. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/
About this article
Cite this article
Syrad, H., Llewellyn, C., Johnson, L. et al. Meal size is a critical driver of weight gain in early childhood. Sci Rep 6, 28368 (2016). https://doi.org/10.1038/srep28368
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/srep28368
This article is cited by
-
The big squeeze: a product content and labelling analysis of ready-to-use complementary infant food pouches in Australia
BMC Public Health (2023)
-
A qualitative exploration of food portion size practices and awareness of food portion size guidance in first-time parents of one- to two-year-olds living in the UK
BMC Public Health (2023)
-
Protocol to evaluate the effectiveness and cost-effectiveness of an environmental nutrition and physical activity intervention in nurseries (Nutrition and Physical Activity Self Assessment for Child Care - NAP SACC UK): a multicentre cluster randomised controlled trial
BMC Public Health (2023)
-
Integration of Time-Based Recommendations with Current Pediatric Health Behavior Guidelines: Implications for Obesity Prevention and Treatment in Youth
Current Obesity Reports (2022)
-
The genomics of childhood eating behaviours
Nature Human Behaviour (2021)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.