Abstract
The Gram-positive bacterium Streptococcus suis serotype 2 (S. suis 2), an important zoonotic pathogen, induces strong systemic infections in humans; sepsis and meningitis are the most common clinical manifestations and are often accompanied by bacteremia. However, the mechanisms of S. suis 2 survival in human blood are not well understood. In our previous study, we identified muramidase-released protein (MRP), a novel human fibrinogen (hFg)-binding protein (FBP) in S. suis 2 that is an important epidemic infection marker with an unknown mechanism in pathogenesis. The present study demonstrates that the N-terminus of MRP (a.a. 283–721) binds to both the Aα and Bβ chains of the D fragment of hFg. Strikingly, the hFg-MRP interaction improved the survival of S. suis 2 in human blood and led to the aggregation and exhaustion of polymorphonuclear neutrophils (PMNs) via an αXβ2 integrin-dependent mechanism. Other Fg-binding proteins, such as M1 (GAS) and FOG (GGS), also induced PMNs aggregation; however, the mechanisms of these FBP-hFg complexes in the evasion of PMN-mediated innate immunity remain unclear. MRP is conserved across highly virulent strains in Europe and Asia and these data shed new light on the function of MRP in S. suis pathogenesis.
Similar content being viewed by others

Introduction
The Gram-positive bacterium Streptococcus suis serotype 2 (S. suis 2) is an emerging human pathogen that induces systemic infections in humans; sepsis and meningitis are the most common clinical manifestations and are often accompanied by bacteremia1,2,3. Severe sepsis from S. suis 2 leads to streptococcal toxic shock syndrome (STSS), which has a high incidence of morbidity and mortality despite antibiotic therapy4. To induce bacteremia, bacterial pathogens must survive in the blood and disseminate while evading polymorphonuclear leukocyte (PMN)-mediated phagocytosis. However, little is known about how this evasion is achieved by S. suis 2.
Fibrinogen (Fg) is a heterogeneous dimetric plasma glycoprotein consisting of three pairs of non-identical Aα, Bβ and γ peptide chains. Fg is the fundamental building block of insoluble fibrin clots and is well known for playing important roles in hemostatic processes5 and the innate immune system6. Numerous bacterial proteins that interact with Fg have been identified in Gram-positive species. Although many of these proteins employ distinct Fg-binding mechanisms7, they all manipulate the biology of Fg to enhance microbial survival in the host. Group A streptococci (GAS) avoid phagocytosis by M protein to inhibit complement activation8,9. FOG, a M1-like protein from group G streptococci, induce bacteria and PMN aggregation10. Staphylococcus aureus interfere with the recognition signal of phagocytes by Efb11. Streptococcus agalactiae form a semi-flexible polymer-like network by FbsA-Fg interaction, which becomes an efficient mask against phagocytic clearance12.
In silico analysis of the Chinese S. suis 2 reference strain 05ZYH33 genome revealed 33 putative cell wall-anchored proteins containing LPxTG or a related motif13; however, it remains to be determined whether these surface proteins play roles in S. suis pathogenesis; thus far, only an adhesin, FBP, was reported to bind to Fg14. In our recent study, a proteomics-based far-western blotting technique (PBFWB) was developed to identify the fibrinogen-binding surface proteins of S. suis (SsFBPs) on a large scale15. Muramidase-released protein (MRP) and Enolase are the major Fg-binding proteins of S. suis 05ZYH33, a Chinese pathogenic strain (NC_009442.1) isolated from a deceased STSS patient. S. suis Enolase functions as a protective antigen displayed on the bacterial cell surface16. However, Enolase is a functional important enzyme in both prokaryotic and eukaryotic organisms17 and its gene couldn’t be knocked out in our previous study15. The mechanism of Enolase in immune evasion remained unclear until now. MRP is a 136-kDa protein that associates with the cell wall of S. suis via an LPxTG motif but is also released into culture supernatants18; it is often reported as an epidemic infection marker for highly virulent strains in Europe and Asia and has low amino acid sequence similarity to other proteins with known functions19,20,21. In our previous study, rat antiserum to MRP had highly bactericidal activity against S. suis 05ZYH33 in human blood22 and the MRP-hFg interaction improved the antiphagocytic capacity of S. suis 2 against PMNs15, suggesting that MRP might be involved in the survival of the bacteria in the host blood. Therefore, the specific mechanism of MRP involvement in the evasion of innate immunity by S. suis in host blood needs to be clarified.
The results of this study indicate that MRP directly binds to the Aα and Bβ chains of the D fragment in hFg. Furthermore, the interaction of soluble (released) MRP with hFg enhanced the survival of S. suis 2 in human blood by disrupting the phagocytic activity of PMNs by inducing their aggregation in an αXβ2 integrin-dependent manner. These results provide useful insight into the molecular mechanism of S. suis pathogenesis and the biological basis of MRP as an important infection marker.
Results
Localization of the hFg-binding region in MRP
PMNs are the first line of defense against bacterial infections in the human blood. In our recent study, hFg enhanced the survival of S. suis 2 in a PMN killing assay. MRP was one of two major SsFBPs among the putative SsFBPs identified in that assay15. However, the specific binding mechanism remained unclear. The putative functional domain of MRP was not predicted in an analysis of the protein sequence with Interproscan (http://www.ebi.ac.uk/Tools), except for a cell wall attachment consensus motif, LPxTG (Supplementary Fig. 1A). Like most surface proteins of Gram-positive bacteria23,24, MRP contains a proline-rich repeat sequence (Fig. 1A). To determine the Fg-binding region of MRP, four recombinant fragments of MRP (Fig. 1A) were engineered mainly according to its predicted secondary structure (Supplementary Fig. 1B) by Psipred analysis (http://bioinf.cs.ucl.ac.uk/psipred) as follows: MRP-N (a.a. 48-721, the N-terminus of MRP), MRP-N1 (a.a. 48–282, the α-coil-rich region), MRP-N2 (a.a. 283–721, mainly consisting of β-sheets) and MRP-C (722–1257, a proline-rich region mainly formed by β-sheets). An interaction between recombinant MRP and immobilized hFg was identified for hisMRP-N (a.a. 48–721) and hisMRP-N2 (a.a. 283–721) (Fig. 1B), which increased as a function of the protein concentration. We detected no Fg-binding activity for hisMRP-N1 (a.a. 48–282) or the C-terminal hisMRP-C (a.a. 722–1257) (Fig. 1B). Similarly, when the system was reversed, immobilized hisMRP-N and hisMRP-N2, but not hisMRP-N1 and hisMRP-C, showed binding to Fg (Fig. 1C), indicating that a.a. 283–721 encompass the Fg-binding domain of MRP. The binding constants of hisMRP-N were further evaluated using bio-layer interferometry (BLI). The KD value for the binding of hisMRP-N to hFg was 340 nM (Fig. 1D), which was close to the value for the M1 protein in GAS25. Additionally, wild-type S. suis 05ZYH33 adhered to immobilized hFg were significantly higher than those observed with ∆MRP bacteria or C∆MRP-N (which express only the soluble binding region, MRP-N) (Fig. 1E), indicating that MRP is an important FBP of S. suis. These results provide important clues about the function of MRP in S. suis 2-induced pathogenesis.
Localization of the hFg-binding region in MRP.
(A) Schematic of MRP. Arrows indicate the truncated forms of MRP that were tested. *S: signal sequence; LPxTG: cell wall anchoring motif. (B) Immobilized Fg (0.25 μg/well) was incubated with the indicated concentrations of truncated hisMRP proteins (hisMRP-N48–721, hisMRP-N1100–282, hisMRP-N2283–721 and hisMRP-C722–1257). Bound proteins were detected with a monoclonal anti-his antibody (1:5000) and an HRP-conjugated anti-mouse antibody (1:10,000). The background values obtained for the control (incubated with PBST containing 1% BSA, but without truncated MRP) were subtracted. (C) Immobilized hisMRP-N48–721, hisMRP-N1100–282, hisMRP-N2283–721 and hisMRP-C722–1257 (100 nM) were incubated with the indicated concentrations of biotinylated hFg and bound proteins were detected with HRP-conjugated streptavidin (1:8000). The background values obtained for the control (incubated with PBST containing 1% BSA, but without biotinylated hFg) were subtracted. The assays were performed in triplicate and the mean ± SD is shown. (D) The binding constants of hisMRP-N were evaluated by BLI. Label-free binding of hFg to immobilized hisMRP-N was conducted in the Octet, which uses streptavidin-coated biosensors to detect protein:protein interactions via BLI. Baseline-corrected BLI response curves (shown in black, with the lower curve corresponding to a lower concentration of injected analyte) were globally fitted to the 1:1 binding model. Kinetic parameters obtained from the fitting are shown. (E) Binding of S. suis to immobilized hFg. The S. suis strains WT, ∆MRP and C∆MRP-N (~1 × 104 CFU per well) were incubated with wells pretreated with hFg or BSA (1, 5, 10 μg/ml per well). The values represent triplicate wells and the mean ± SD of the CFU of binding bacteria per well.
Identification of the hFg-binding site of MRP
Most FBPs of pathogens have specific Fg-binding mechanisms7; thus, the region within fibrinogen that is responsible for MRP binding was investigated. Fg consists of subunits D and E, each containing three polypeptide chains (Aα, Bβ and γ). When separated by SDS-PAGE under reducing conditions, fibrinogen appeared as three bands corresponding to the Aα (63.5 kDa), Bβ (56 kDa) and γ (47 kDa) chains (Fig. 2A). Both the Aα and Bβ chains were readily detected when transferred to a polyvinylidene difluoride (PVDF) membrane and were probed with purified biotinylated hisMRP-N and hisMRP-N2, but not hisMRP-N1 (Fig. 2A). To identify the MRP-binding site(s) in Fg, isolated D and E fragments of Fg (Fg-D and Fg-E, respectively) were tested in an ELISA-type binding assay. The data indicate that hisMRP-N2 (Fig. 2Bi) and hisMRP-N (Fig. 2Bii) bound well to Fg-D and intact Fg, but did not bind to Fg-E. An analysis of the MRP–Fg-D interaction by BLI further confirmed that Fg-D, but not Fg-E, bound to hisMRP-N2 (Fig. 2Ci) and hisMRP-N (Fig. 2Cii), providing insight into a possible mechanism by which MRP alters Fg to allow S. suis 2 to evade innate immunity.
MRP binding to the D fragment of the Fg Aα and Bβ chains.
(A) Binding of hisMRP to the hFg Aα and Bβ chains. Purified hFg was separated by SDS-PAGE and stained with Coomassie blue (lane 1) or transferred to PVDF and probed with biotinylated hisMRP-N (lane 2), hisMRP-N2 (lane 3), hisMRP-N1 (lane 4) (20 μg/ml) or PBST (lane 5). The bound proteins were detected with HRP-conjugated streptavidin (1:8000). (B) MRP binds to Fg-D, but not Fg-E, as determined by an ELISA-type binding assay. Immobilized Fg/Fg-D /Fg-E (0.25 μg/well) was incubated with the indicated concentrations of hisMRP-N2 and hisMRP-N and bound proteins were detected with anti-his antibody (1:5000) and HRP-conjugated anti-mouse antibody (1:10,000). The background values obtained for the control (incubated with PBST containing 1% BSA, but without truncated MRP) were subtracted. The data show that MRP-N2 (i) and MRP-N (ii) bound to the immobilized Fg (triangles) and Fg-D (circles), but not Fg-E (squares). The assays were performed in triplicate and the mean ± SD is shown. (C) BLI analysis of the binding response curves, which were generated by incubating Fg/Fg-D/Fg-E with immobilized hisMRP-N2 or hisMRP-N. Fg-D, but not Fg-E, binds to both hisMRP-N2 (i) and hisMRP-N (ii).
The presence of MRP in culture supernatants and the bacterial cell surface
MRP is a substrate of sortase A in a National Collection of Type Cultures (NCTC) European strain26. However, the protein is also detectable in the culture supernatants from serotype 2 strains isolated from European diseased pigs16. To further explore the function of MRP in 05ZYH33, the location of MRP was detected in 05ZYH33 cells. Western blotting indicated that MRP was detected in the culture supernatant in the 05ZYH33 strain (Fig. 3A) but was not detected in the mutant strain (Fig. 3A). To elucidate the function of soluble (released) MRP, a complementary strain (C∆MRP-N) was constructed for the soluble expression of MRP-N (which is identified as the hFg-binding region in Fig. 1). Western blotting analysis indicated that MRP-N was present in the supernatant from the C∆MRP-N strain (Fig. 3A). Additionally, the surface location of MRP was visualized using confocal laser scanning microscopy in the WT strain 05ZYH33 (Fig. 3Baiii), but not in the mutant (Fig. 3Bbiii) and complementary strains (Fig. 3Bciii). These data indicated that MRP was released into culture supernatant and that the complementary strain (C∆MRP-N) expressing the secreted MRP-N was successfully constructed.
The presence of MRP in the culture supernatant and on the bacterial cell surface.
(A) The released MRP in the supernatant was detected by western blotting. Samples of the concentrated culture supernatant (25:1, OD600 = 0.4) and truncated hisMRP proteins were separated by SDS-PAGE (Ai) and transferred to a PVDF membrane that was probed with rabbit anti-MRP-N serum (1:400) followed by HRP-conjugated goat anti-rabbit IgG (1:8000). MRP and MRP-N could be specifically detected in the supernatants from WT and C∆MRP-N bacteria, respectively (Aii). The specificity of the anti-MRP-N antibody was evaluated using hisMRP-N and hisMRP-C (Aii). (B) Visualizing MRP protein on the bacterial surface. The samples of the S. suis WT strain 05ZYH33 (ai)-(aiii), the mutant ∆MRP strain (bi)-(biii) and the complementary strain C∆MRP-N that expresses only soluble MRP-N (ci)-(ciii) were washed and stained for MRP-N using rabbit anti-MRP-N IgG and rhodamine (TRITC)-conjugated goat anti-rabbit IgG. For each sample, the merges of the two images are shown in panels (aiii), (biii) and (ciii), respectively.
MRP facilitates the survival of S. suis 2 in human blood in an αXβ2 integrin-dependent manner
To investigate the role of MRP in immune evasion in human blood, the survival of mrp-deficient mutants (∆MRP) was evaluated after the addition of hisMRP truncations. Interestingly, the viability of strain ∆MRP in human blood was increased by the exogenous addition of hisMRP-N or hisMRP-N2, but not hisMRP-N1 or hisMRP-C (Fig. 4A). Therefore, it is possible that the biological effects of MRP are exerted upon its release into the extracellular milieu. As expected, C∆MRP-N rescued the survival defect of the mutant ∆MRP bacteria in the blood, bringing the survival to levels similar to WT (Fig. 4B). Additionally, in a specific antibody-blocking assay, antiserum against MRP-N decreased the WT and C∆MRP-N bacterial survival, but not to ∆MRP in human blood (Fig. 4C), suggesting that MRP could be a promising candidate for antibody-based therapies for S. suis induced-sepsis. These results indicate that soluble (released) MRP is responsible for immune evasion by S. suis in human blood.
MRP facilitates S. suis 2 survival in human blood in an αXβ2 integrin-dependent manner.
(A) Incubation of ∆MRP bacteria with the MRP-binding domain (1.0 mM) increased bacterial survival in human blood after 60 min. *P < 0.05, ***P < 0.001; n.s., no significance. (B) MRP contributes to the survival of S. suis 2 in human blood at the measured time points (60, 120 and 180 min). Significant differences were detected between the WT and ∆MRP groups (P < 0.001 at 60 min; P < 0.05 at 120 min and 180 min) and between the C∆MRP-N and ∆MRP groups (P < 0.001 at 60 min; P < 0.05 at 120 min and 180 min). (C) Antibodies against the MRP-N-binding region decrease S. suis viability in human blood. Bacteria were pretreated with preimmune (control) or anti-MRP-N serum from rabbits immunized with MRP-N (1:5 dilution). Significant differences were found between preimmune and anti-MRP-N sera in the WT (P < 0.001) and C∆MRP-N (P < 0.001) groups, but not in the ∆MRP group (P > 0.05). (D) Viability of S. suis 2 in human blood in the presence or absence of GPRP (50 μg/ml) and GHRP (50 μg/ml). Significant differences were found between GPRP treatment and other treatments in the WT (P < 0.05) or C∆MRP-N (P < 0.001) groups but not in the ∆MRP group (P > 0.05). (E) Viability of S. suis 2 in human blood as determined by a bactericidal assay after treatment with the specific anti-αMβ2 antibody (10 μg/ml), the specific anti-αxβ2 antibody (10 μg/ml) or their isotype control mouse IgG1 (10 μg/ml). Significant differences were found between anti-αxβ2 treatment and other treatments in the WT (P < 0.001) and C∆MRP-N (P < 0.001) groups but not in the ∆MRP group (P > 0.05). In Figs. A–E, each symbol represents an individual human blood sample. In Figs. A, C, D and E, the horizontal lines indicate the mean for each group. In Figs. A, D and E, post hoc tests were used for statistical analysis. In Fig. C, an unpaired Student’s t test was used. In Fig. B, the horizontal lines indicate the median for each group and a Mann-Whitney test was used.
The mechanistic basis of MRP in immune evasion by S. suis 2 was further investigated in a bactericidal assay using a peptide derived from the Aα chain of Fg (Gly-Pro-Arg-Pro, GPRP), which acts as a β2 integrin antagonist and has been shown to impair the M1-Fg complex-induced aggregation of PMNs27. A second peptide, Gly-His-Arg-Pro (GHRP), which does not have this effect27, was also tested as a control. GPRP decreased the growth of WT and C∆MRP-N bacteria in human blood (Fig. 4D), while no effects were observed for the ∆MRP bacteria. The control peptide GHRP or H2O had no effect on the survival of WT, ∆MRP and C∆MRP-N in human blood, suggesting that the β2 integrins on PMNs were involved in this process. αXβ2 and αMβ2 are general integrins expressed by phagocytes; neutrophils interact with hFg through the β2 family of integrins, with the N-terminal portion of the Aα chain of Fg binding to αXβ228 while the C-terminal portion of the γ chain binds to αMβ2 integrins29. To determine which type of β2 integrin mediates the formation of MRP-hFg complexes for immune evasion by S. suis 2, monoclonal antibodies against the αM (clone CBRM1/5) and αx (clone BU15) integrin subunits and an isotype control mouse IgG1 were used in blocking assays. Like GPRP, the antibody against the αx integrin subunit decreased the survival of WT and C∆MRP-N, but not ∆MRP bacteria in human blood, while there was no interference detected using the antibody against αM or the control IgG1 (Fig. 4E).
These results suggest that the N-terminus of MRP (MRP-N) might interact with hFg and exert some effects on PMNs via αXβ2 integrin crosslinking to improve the survival of S. suis 2 in human blood.
The soluble (released) MRP was involved in the immune evasion of S. suis 2 by interacting with hFg
PMN-mediated innate immunity is the first line of defense against bacterial pathogens in human blood. To verify the hypothesis that MRP improves the immune evasion of S. suis 2 by interacting with hFg, a simplified model of whole blood, a PMN killing assay, was performed in the presence of fresh serum, fresh plasma or fresh serum supplemented with hFg (the serum and plasma were isolated from the same donor). Interestingly, as in the whole blood, the mutant ∆MRP bacteria had reduced viability compared to the WT bacteria in serum containing hFg at physiological concentrations (2–4 mg/ml) (Fig. 5A) and C∆MRP-N rescued the viability of ∆MRP to the level of WT in serum with hFg, but not in serum alone (Fig. 5A). Similarly, ∆MRP bacteria had reduced viability compared to WT and C∆MRP-N bacteria in plasma (Fig. 5B), but not in serum alone; additionally, supplementation of ∆MRP bacteria with MRP-N, but not MRP-C, rescued their viability in plasma but had no effect in serum alone (Fig. 5B). These results indicate that the N-terminus of MRP (MRP-N) is responsible for the immune evasion of S. suis by interacting with hFg.
The MRP–hFg interaction was involved in the immune evasion of S. suis 2.
(A) The MRP-hFg interaction enhanced the survival of S. suis 2 in serum supplemented with hFg in PMN killing assays. The WT, C∆MRP-N and ∆MRP strains were co-incubated with PMNs at an MOI of 1:15 (PMN:bacterium) in 50% serum without or with hFg (1–4 mg/ml) for 60 min. The mutant ∆MRP bacteria had reduced viability compared to the WT (P < 0.01 at 2 mg; P < 0.001 at 4 mg) and C∆MRP-N strains (P < 0.01 at 2 mg; P < 0.001 at 4 mg) in serum containing hFg at physiological concentrations (2–4 mg/ml), but not in serum alone (P > 0.05) or in 1 mg/ml hFg (P > 0.05). (B) The MRP-hFg interaction increased the survival of S. suis 2 in plasma in PMN killing assays. The WT, C∆MRP-N and ∆MRP strains and the ∆MRP strain with added truncated MRP were incubated with PMNs at an MOI of 1:15 (PMN:bacterium) in 50% serum or plasma isolated from the same healthy donors for 60 min. In Figs. A and B, the percentage of surviving S. suis 2 indicated was calculated as follows: (CFUPMN+/CFUPMN−) × 100%. The data are expressed as the means ± SD of three independent experiments and unpaired Student’s t tests were used for statistical analysis. *P < 0.05; **P < 0.01; n.s. (no significance).
The MRP-hFg interaction results in the integrin-triggered aggregation of PMNs and PMN exhaustion
The effects of the MRP–hFg interaction on PMNs in the PMN killing assay were further investigated by confocal laser scanning microscopy. The WT (Fig. 6A) and C∆MRP-N (Fig. 6C) strains induced PMN aggregation in serum supplemented with hFg; however, infection by either the ∆MRP strain (Fig. 6B) or the WT strain in serum alone had no effect (data not shown), suggesting that the aggregation was caused by the MRP–hFg interaction. Moreover, dead bacteria and PMNs (red staining by propidium iodide [PI]) were the principal constituents of these aggregates induced by the WT or C∆MRP-N strains (Fig. 6A,C and their magnified images in Supplementary Fig. 2) and greater numbers of green extracellular viable bacteria (green staining by SYTO9) were observed in these groups (white arrows in Fig. 6A,C and in Supplementary Fig. 2) than with the ∆MRP strain (Fig. 6B). Because soluble MRP enhanced the survival of S. suis 2 in PMN killing assays by interacting with hFg, the supernatants were assessed to determine whether they could induce PMN aggregation. As expected, the WT and C∆MRP-N-supernatants had a similar effect on PMNs in the presence of serum supplemented with hFg (Fig. 6J,L), but the ∆MRP supernatant did not (Fig. 6K). These results suggest that soluble (released) MRP induces PMNs aggregation and death by interacting with hFg.
PMN aggregation via an MRP-hFg interaction through αxβ2 integrin crosslinking.
PMNs incubated with S. suis at an MOI (PMN:bacterium) of 1:15 in 50% serum supplemented with hFg or serum alone for 60 min were analyzed by confocal laser scanning microscopy. Dead and viable PMNs/bacteria were stained with PI (red staining) and SYTO 9 (green staining), respectively. The extracellular viable bacteria are indicated by a white arrow. The regions enclosed by white boxes are shown enlarged in Fig. S1. PMNs were incubated with WT (A), ∆MRP (B) or C∆MRP-N (C) bacteria; PMNs pretreated with GPRP (D), GHRP (E) or anti-αxβ2 antibody (F) were incubated with WT bacteria; PMNs pretreated with GPRP (G), GHRP (H) or anti-αxβ2 antibody (I) were incubated with C∆MRP-N bacteria; PMNs were incubated with the supernatants from WT (J), ∆MRP (K) and C∆MRP-N (L) bacteria. The bars are as indicated in Fig. 6. GPRP, Gly-Pro-Arg-Pro; GHRP, Gly-His-Arg-Pro; anti-αxβ2, monoclonal antibody against αx integrin subunits; Sup, supernatant.
Furthermore, GPRP, but not GHRP, inhibited the aggregation induced by the WT (Fig. 6D,E) and C∆MRP-N (Fig. 6G,H) strains, as did a monoclonal antibody against αX integrin subunits (Fig. 6F,I). These results were consistent with the bactericidal assay in Fig. 5A,B, suggesting that the MRP-hFg interaction results in the αXβ2 integrin-triggered aggregate formation of PMNs and reduces the capacity of PMNs to clear S. suis in the blood by phagocytosis.
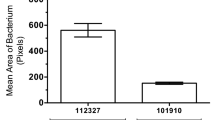
To further analyze PMN activation by S. suis, dihydrorhodamine (DHR)123, a fluorogenic substrate of active oxygen, was used to detect oxidative activity. The mean fluorescence intensity (MFI) as determined by flow cytometry in PMNs treated with the WT strain was twice that of PMNs treated with ∆MRP. The MFI of PMNs was 2-fold lower in the presence of GPRP relative to GHRP upon treatment with the WT strain opsonized in hFg-supplemented serum (Fig. 7), but not in serum alone (data not shown). These results suggest that the MRP–hFg interaction results in the excessive activation and exhaustion of PMNs via a β2 integrin-dependent mechanism.
Flow cytometric analysis of oxidative activity in the PMN killing assay.
(A) Representative histograms for fluorescence-activated cell sorting (FACS) analysis. (B) The MFI of DHR123 was measured. In the PMN killing assay, the PMNs were stimulated with the WT or ΔMRP strains in the absence or presence of GPRP or GHRP. PMNs without S. suis stimulation served as the control. DHR123 (1 μM) was used to detect oxidative activity. The data are expressed as the means ± SD of three replicates. *P < 0.05; n.s., no significance.
Discussion
S. suis is an emerging pathogen and a leading cause of skin wounds and bloodstream, brain and soft tissue infections30,31. The most common clinical manifestations of infection are sepsis and meningitis30, which are often accompanied by bacteremia, as is the case for Streptococcus pneumoniae- and Neisseria meningitidis-associated meningitis32. Outbreaks of S. suis 2 infection in China have highlighted the importance and relatively high frequency of a severe sepsis syndrome that shares features with toxic shock syndrome and is associated with high mortality1,3. However, little is known of the mechanism of S. suis survival in human blood and only a few virulence factors, such as Fhb24 and SLY33, are known to enable pathogens to evade the host immune response by inhibiting complement activation.
MRP is often reported as an epidemic infection marker in Europe and Asia19,20,21. Although this protein was reported not to be a critical virulence factor in an intranasal infection model in Anthony piglets34, the real contribution of MRP to bacterial virulence needs to be identified in a rational infection model because different infection models might lead to different conclusions35. For example, the Canadian virulent strain 89-1591 (MRP-) was reported as avirulent by Rasmussen et al.36 but was shown to be virulent in experimental models applied by other researchers37. Several North American virulent strains were reported to be MRP− genotype strains38. However, most North America virulent strains (MRP-) belong to ST25 strains, which were different from ST7 strains based on multilocus sequence typing39. The highly virulent Chinese strain 05ZYH33 used in this study belongs to ST7 strains which exhibit strong invasiveness and high pathogenicity, has resulted in the description of a new disease form of streptococcal toxic shock syndrome (STSS) and a putative pathogenicity island (termed 89 K)31. We believe that the real contribution of MRP to different strains need to consider the background of strains.
PMNs are the first line of defense against bacterial infections in human blood; in our recent study, MRP enhanced the survival of S. suis 2 in PMN killing assays by interacting with hFg15. However, the specific mechanism of this enhancement needed to be clarified. In this study, MRP was identified as a novel FBP of S. suis 2 that showed high binding affinity to hFg, suggesting that the MRP–hFg interaction may be critical for MRP function. The present study revealed that binding occurs via the interaction of the N-terminus of MRP (a.a. 283–721) and the D fragment of Fg, similar to that observed in the adhesins of other gram-positive bacteria7,11. Nonetheless, there are some notable differences from other FBPs: first, the binding region of MRP has no sequence homology to other known FBPs, which share a common domain architecture that enables fibrinogen binding through a “dock, lock and latch” (DLL) mechanism40,41,42,43. Second, in contrast to other FBPs that bind the Aα, Bβ or γ chain singly, MRP displayed specific binding to both the Aα and Bβ chains in a manner similar to Lysin, an FBP of Streptococcus mitis44, but different from that of the M1 protein, which binds to coiled coils in the β and γ chains of hFg45. Studies have been initiated to determine the crystal structure of the MRP–hFg complex, which can reveal the details of this interaction.
An intriguing observation was that the soluble MRP-hFg interaction enhanced the survival of S. suis 2 in human blood and induced the aggregation and hyperactivation of PMNs via the αXβ2 integrin receptor, which was independent of complement inhibition (data not shown). However, M proteins are important virulence factors for GAS that inhibit complement deposition on the bacterial surface via the binding of hFg to the surface M proteins8,46. Although the soluble (released) M1 induced PMN aggregation and HBP release and was blocked by the β2 integrin antagonist GPRP25, it was not determined which member of the β2 integrin subfamily was involved in the crosslinking of the M1–hFg complex and the immune evasion of GAS. Despite hFg being a physiologically relevant ligand for αMβ2, the integrin engagement of hFg is critical for leukocyte function and innate immunity in vivo47. αXβ2, but not αMβ2, was involved in the excessive activation of PMNs induced by the MRP–hFg complex in the present study. Although other FBPs, including M125 and FOG10, induce PMN aggregation, the specific receptor on PMNs that mediates crosslinking to the FBP/hFg complexes and the relationship of this process to immune evasion by pathogens remained unclear.
In summary, MRP is a known infection marker of S. suis 2 in most Chinese and European clinical isolates, but the role of MRP in the evasion of PMN-mediated innate immunity by S. suis remained unclear and controversial. Here, we showed that the N-terminus of MRP (a.a. 283–721) binds to both the Aα and Bβ chains of the D fragment in hFg. Moreover, the MRP-hFg interaction aggregates PMNs via the αXβ2 integrin receptor and promotes pathogen survival in host blood. These data shed new light on the function of MRP in the S. suis-host interaction. More objective consideration of strains and infection models is needed to reevaluate the contribution of MRP to the virulence of ST-7 strains in China and ST-1 strains in Europe.
Methods
Human blood, serum and plasma
The healthy donors who provided the serum and plasma in this study provided written informed consent in accordance with the Declaration of Helsinki. Approval was obtained from the Institutional Medical Ethics Committee of the Academy of Military Medical Sciences. The human blood, serum and plasma used in this study were obtained in accordance with the approved guidelines.
Bacterial strains and growth conditions
The highly virulent S. suis 2 strain 05ZYH33, originally isolated from a deceased STSS patient following an outbreak in Sichuan, China in 2005, was used in this study. S. suis 2 strains were cultured as previously described24. The bacterial strains and plasmids used in this study are listed in Supplementary Table 1.
Recombinant expression and purification of MRP
To determine the binding region of MRP, four recombinant fragments of MRP (Fig. 1A) were engineered mainly according to its predicted secondary structure (Supplementary Fig. 1B) as follows: MRP-N (a.a. 48–721, the N-terminus of MRP), including MRP-N1 (a.a. 48–282, the α-coil-rich region), MRP-N2 (a.a. 283–721, mainly consisting of β-sheets) and MRP-C (722–1257, a proline-rich region mainly consisting of β-sheets). The oligonucleotide primers and expression vector used for MRP-N, MRP-N1, MRP-N2 and MRP-C in this study are listed in Supplementary Table 1. All of the above ORFs were cloned into the pET-28a vector and the proteins were expressed and purified by Ni-chelating chromatography (GE Healthcare) according to the manufacturer’s recommendations.
Preparation of anti-MRP-N sera and IgG
To generate polyclonal anti-MRP-N antibodies, the recombinant MRP-N proteins were injected subcutaneously into two female rabbits as previously described20. All experiments on live vertebrates in this study were approved by the Institutional Medical Ethics Committee of the Academy of Military Medical Sciences; the permit number of all animal work was SCXK-(JUN) 2013–018. All experiments on live vertebrates were performed in accordance with the relevant guidelines and regulations20. The anti-MRP-N IgG in the antiserum was purified using a HiTrap Protein G HP column (GE Healthcare).
ELISA-type binding assay
To detect the binding of MRP to immobilized hFg, 96-well plates were coated overnight at 4 °C with 100 μl of 2.5 μg/ml Fg/Fg-D/Fg-E (Merck). After blocking with 3% BSA (bovine serum albumin) in PBST (phosphate-buffered saline with 0.05% Tween-20), recombinant MRP proteins were added and incubated for 1 h at room temperature. Bound MRP was detected by incubation with an anti-his monoclonal antibody (1:5000, Sigma) and HRP (horseradish peroxidase)-conjugated anti-mouse antibodies (1:10,000; Santa Cruz). The binding was quantified by measuring the absorbance at 450 nm. Background values obtained for the control (incubated with PBST containing 1% BSA, without truncated MRP) were subtracted. To detect the binding of hFg to immobilized MRP, 96-well plates were coated overnight at 4 °C with 100 μl of 100 nM truncated MRP. After blocking with 3% BSA in PBST, biotinylated hFg was added and the plates were incubated for 1 h at room temperature. Bound hFg was detected by incubation with HRP-conjugated streptavidin (1:8000; GE Health). Background values obtained for the control (incubated with PBST containing 1% BSA, without biotinylated hFg) were subtracted. The assays were performed in triplicate and the mean ± SD is shown.
BLI analysis of the MRP-hFg interactions
All BLI experiments were performed in PBST on a BLItz system (ForteBio, Inc.) as previously described48. Streptavidin-coated biosensors with immobilized biotinylated MRP-N proteins were exposed to different concentrations of hFg, Fg-D, or Fg-E. The association and dissociation rate constants (ka and kd, respectively) for the interactions were derived from curve fitting and were used to calculate the dissociation constant, KD (KD = kd/ka).
Binding of S. suis to immobilized fibrinogen
The binding of S. suis to immobilized fibrinogen was detected as previously described43. The 96-well plates were coated overnight at 4 °C with 100 μl of purified fibrinogen (1, 5, 10 μg/ml) or BSA (1, 5, 10 μg/ml) and were then washed four times with PBS. Overnight cultures of the WT, CΔMRP-N and ΔMRP strains were harvested by centrifugation and then adjusted to almost equal the original inocula (~105 CFU [colony-forming units]/ml) in PBS. The wells, which were pretreated with hFg/BSA, were then incubated with 100 μl of S. suis suspension for 30 min at 37 °C. The wells were washed four times with PBS to remove unbound bacteria and were then treated with 100 μl of trypsin (2.5 mg/ml) for 10 min at 37 °C to release the attached bacteria. The number of bound bacteria was determined by plating serial dilutions of the recovered bacteria onto THB agar plates.
Generation of the ∆MRP mutant and the complementary CΔMRP-N strains
The mrp mutant was obtained from the 05ZYH33 WT strain (accession number YP_001198119) by in-frame deletion of the SSU05_0753 gene, as previously described15,49. In the present study, for complementation assays, we selected MRP-N, but not the entire MRP sequence for cloning because MRP exists as a soluble protein in the supernatant and MRP-N (a.a. 48–721) was the hFg-binding region. Furthermore, it was difficult to construct a complementary strain expressing the entire MRP protein. The upstream promoter and a DNA fragment encoding MRP-N without the LPxTG motif were amplified using the primers CΔMRP-N-F/CΔMRP-N-R (Supplementary Table 1). The amplicon was subsequently cloned into the E. coli-S. suis shuttle vector pAT18, the recombinant plasmid pAT18::mrp-N was transformed into the ΔMRP strain and the CΔMRP-N strain was screened on THB agar with selective pressure from Em. Western blotting and confocal laser scanning microscopy analysis were used to confirm the soluble expression of MRP-N in CΔMRP-N bacteria.
Bactericidal and PMN killing assays
The bactericidal assay was used to compare the growth of the WT, CΔMRP-N and ΔMRP strains in human blood as described previously24. Briefly, diluted strain cultures (50 μl at 2 × 104 CFU/ml) were combined with fresh human blood (450 μl) and the mixtures were rotated at 37 °C; the samples were treated with 1% saponin, diluted and plated onto blood agar. The percentage of live bacteria was subsequently calculated as (CFU on plate/CFU in original inoculum) × 100%. In the integrin-blocking assay, GPRP (50 μg/ml), GHRP (50 μg/ml), monoclonal antibodies against αM (clone CBRM1/5, eBioscience, 10 μg/ml), αx integrin subunits (clone BU15, Acris Antibodies, 10 μg/ml) and the isotype control mouse IgG1 antibody (eBioscience, 10 μg/ml) were preincubated with the blood for 15 min at room temperature. In the PMN killing assay, PMNs were infected with S. suis 2 at a multiplicity of infection (MOI) of 1:15 (PMN:bacterium) in 50% non-immune human serum and were centrifuged at 380 × g for 5 min at 4 °C. The plates were then incubated at 37 °C in 5% CO2. Samples were taken at 60 min and analyzed immediately as described for the human blood. The colonies were counted and the percentage of surviving S. suis 2 bacteria was calculated as follows: (CFUPMN+/CFUPMN−) × 100%. GPRP and GHRP were dissolved in H2O.
Confocal laser scanning microscopy analysis
The LIVE/DEAD viability kit (Invitrogen) was used to determine the viability of PMNs and S. suis. In the PMN killing assay, a mixture of PMNs and bacteria was stained with PI and SYTO 9 and then spotted onto Petri dishes (World Precision Instruments Inc.) using cover slips placed over the liquid to stabilize the cells. The dead (PI, red staining) and viable (SYTO 9, green staining) PMNs/bacteria were then visualized by XYZ scanning using an FV1000 confocal laser scanning microscope (Olympus).
Visualization of MRP proteins on the bacterial surface was performed as previously described50. Briefly, an aliquot of streptococci (6 × 106 CFU/mL) was added to rabbit anti-MRP-N IgG (10 μg/ml), incubated for 45 min on ice and washed. Three hundred microliters of the resuspension was then incubated with rhodamine (TRITC)-goat anti-rabbit IgG (Santa Cruz) (0.3 mg/ml) for 45 min on ice. The bacteria were then washed with PBS and spotted onto CITOGLAS slides (SHITAI). The slides were then analyzed with an OLYMPUS FV1000 confocal scanning microscope.
Additional Information
How to cite this article: Pian, Y. et al. Binding of Human Fibrinogen to MRP Enhances Streptococcus suis Survival in Host Blood in a αXβ2 Integrin-dependent Manner. Sci. Rep. 6, 26966; doi: 10.1038/srep26966 (2016).
References
Tang, J. et al. Streptococcal toxic shock syndrome caused by Streptococcus suis serotype 2. PLoS Med 3, 668–676, doi: 10.1371/journal.pmed.0030151 (2006).
Wangkaew, S., Chaiwarith, R., Tharavichitkul, P. & Supparatpinyo, K. Streptococcus suis infection: a series of 41 cases from Chiang Mai University Hospital. J Infect 52, 455–460, doi: 10.1016/j.jinf.2005.02.012 (2006).
Yu, H. J. et al. Human Streptococcus suis outbreak, Sichuan, China. Emerg Infect Dis 12, 914–920 (2006).
Sriskandan, S. & Slater, J. D. Invasive disease and toxic shock due to zoonotic Streptococcus suis: an emerging infection in the East? PLoS Med 3, e187 (2006).
Herrick, S., Blanc-Brude, O., Gray, A. & Laurent, G. Fibrinogen. Int J Biochem Cell Biol 31, 741–746 (1999).
Rubel, C. et al. Fibrinogen promotes neutrophil activation and delays apoptosis. J Immunol 166, 2002–2010 (2001).
Rivera, J., Vannakambadi, G., Hook, M. & Speziale, P. Fibrinogen-binding proteins of Gram-positive bacteria. Thromb Haemost 98, 503–511 (2007).
Courtney, H. S., Hasty, D. L. & Dale, J. B. Anti-phagocytic mechanisms of Streptococcus pyogenes: binding of fibrinogen to M-related protein. Mol Microbiol 59, 936–947 (2006).
Carlsson, F., Sandin, C. & Lindahl, G. Human fibrinogen bound to Streptococcus pyogenes M protein inhibits complement deposition via the classical pathway. Mol Microbiol 56, 28–39 (2005).
Johansson, H. M., Morgelin, M. & Frick, I. M. Protein FOG–a streptococcal inhibitor of neutrophil function. Microbiology 150, 4211–4221 (2004).
Ko, Y. P., Liang, X., Smith, C. W., Degen, J. L. & Hook, M. Binding of Efb from Staphylococcus aureus to fibrinogen blocks neutrophil adherence. J Biol Chem 286, 9865–9874 (2011).
Pierno, M., Maravigna, L., Piazza, R., Visai, L. & Speziale, P. FbsA-driven fibrinogen polymerization: a bacterial “deceiving strategy”. Phys Rev Lett 96, 028108 (2006).
Wang, C. et al. The involvement of sortase A in high virulence of STSS-causing Streptococcus suis serotype 2. Arch Microbiol 191, 23–33 (2009).
de Greeff, A. et al. Contribution of fibronectin-binding protein to pathogenesis of Streptococcus suis serotype 2. Infect Immun 70, 1319–1325 (2002).
Pian, Y. et al. Proteomics identification of novel fibrinogen-binding proteins of Streptococcus suis contributing to antiphagocytosis. Front Cell Infect Microbiol. 5, 19, doi: 10.3389/fcimb.2015.00019 (2015).
Feng, Y. et al. Streptococcus suis enolase functions as a protective antigen displayed on the bacterial cell surface. J Infect Dis 200, 1583–1592 (2009).
Gerlt, J. A., Babbitt, P. C., Jacobson, M. P. & Almo, S. C. Divergent evolution in enolase superfamily: strategies for assigning functions. J Biol Chem 287, 29–34, doi: doi: 10.1074/jbc.R111.240945 (2012).
Vecht, U., Wisselink, H. J., Jellema, M. L. & Smith, H. E. Identification of two proteins associated with virulence of Streptococcus suis type 2. Infect Immun 59, 3156–3162 (1991).
Vecht, U., Wisselink, H. J., Stockhofe-Zurwieden, N. & Smith, H. E. Characterization of virulence of the Streptococcus suis serotype 2 reference strain Henrichsen S 735 in newborn gnotobiotic pigs. Vet Microbiol 51, 125–136 (1996).
Yang, W. Z. et al. [An outbreak of human Streptococcus suis serotype 2 infections presenting with toxic shock syndrome in Sichuan, China]. Zhonghua Liu Xing Bing Xue Za Zhi 27, 185–191 (2006).
Rehm, T. et al. Amplified fragment length polymorphism of Streptococcus suis strains correlates with their profile of virulence-associated genes and clinical background. J Med Microbiol 56, 102–109 (2007).
Geng, H. et al. Identification and characterization of novel immunogenic proteins of Streptococcus suis serotype 2. J Proteome Res 7, 4132–4142 (2008).
Wastfelt, M., Stalhammar-Carlemalm, M., Delisse, A. M., Cabezon, T. & Lindahl, G. Identification of a family of streptococcal surface proteins with extremely repetitive structure. J Biol Chem 271, 18892–18897 (1996).
Pian, Y. et al. Fhb, a novel factor H-binding surface protein, contributes to the antiphagocytic ability and virulence of Streptococcus suis. Infect Immun 80, 2402–2413 (2012).
Ringdahl, U. et al. A role for the fibrinogen-binding regions of streptococcal M proteins in phagocytosis resistance. Mol Microbiol 37, 1318–1326 (2000).
Osaki, M., Takamatsu, D., Shimoji, Y. & Sekizaki, T. Characterization of Streptococcus suis genes encoding proteins homologous to sortase of gram-positive bacteria. J Bacteriol 184, 971–982 (2002).
Herwald, H. et al. M protein, a classical bacterial virulence determinant, forms complexes with fibrinogen that induce vascular leakage. Cell 116, 367–379 (2004).
Loike, J. D. et al. CD11c/CD18 on neutrophils recognizes a domain at the N terminus of the A alpha chain of fibrinogen. Proc Natl Acad Sci USA 88, 1044–1048 (1991).
Wright, S. D. et al. Complement receptor type three (CD11b/CD18) of human polymorphonuclear leukocytes recognizes fibrinogen. Proc Natl Acad Sci USA 85, 7734–7738 (1988).
Feng, Y. et al. Streptococcus suis infection: an emerging/reemerging challenge of bacterial infectious diseases? Virulence 5, 477–497, doi: 10.4161/viru.28595 (2014).
Feng, Y., Zhang, H., Ma, Y. & Gao, G. F. Uncovering newly emerging variants of Streptococcus suis, an important zoonotic agent. Trends Microbiol. 18, 124–131, doi: 10.1016/j.tim.2009.12.003 (2010).
Dupas, D., Vignon, M. & Geraut, C. Streptococcus suis meningitis. A severe noncompensated occupational disease. J Occup Med 34, 1102–1105 (1992).
Lecours, M.-P. et al. Critical Role for Streptococcus suis Cell Wall Modifications and Suilysin in Resistance to Complement-Dependent Killing by Dendritic Cells. J Infect Dis 204, 919–929, doi: 10.1093/infdis/jir415 (2011).
Smith, H. E. et al. Mutants of Streptococcus suis types 1 and 2 impaired in expression of muramidase-released protein and extracellular protein induce disease in newborn germfree pigs. Infect Immun 64, 4409–4412 (1996).
Berthelot-Herault, F., Gottschalk, M., Morvan, H. & Kobisch, M. Dilemma of virulence of Streptococcus suis: Canadian isolate 89–1591 characterized as a virulent strain using a standardized experimental model in pigs. Can J Vet Res 69, 236–240 (2005).
Rasmussen, S. R., Aarestrup, F. M., Jensen, N. E. & Jorsal, S. E. Associations of Streptococcus suis serotype 2 ribotype profiles with clinical disease and antimicrobial resistance. J Clin Microbiol 37, 404–408 (1999).
Charland, N., Kobisch, M., Martineau-Doize, B., Jacques, M. & Gottschalk, M. Role of capsular sialic acid in virulence and resistance to phagocytosis of Streptococcus suis capsular type 2. FEMS Immunol Med Microbiol 14, 195–203 (1996).
Quessy, S., Dubreuil, J. D., Caya, M. & Higgins, R. Discrimination of virulent and avirulent Streptococcus suis capsular type 2 isolates from different geographical origins. Infect Immun 63, 1975–1979 (1995).
Ye, C. et al. Clinical, experimental and genomic differences between intermediately pathogenic, highly pathogenic and epidemic Streptococcus suis. J Infect Dis 199, 97–107, doi: 10.1086/594370 (2009).
Ponnuraj, K. et al. A “dock, lock and latch” structural model for a staphylococcal adhesin binding to fibrinogen. Cell 115, 217–228 (2003).
Ganesh, V. K. et al. A structural model of the Staphylococcus aureus ClfA-fibrinogen interaction opens new avenues for the design of anti-staphylococcal therapeutics. PLoS Pathog 4, e1000226 (2008).
Xiang, H. et al. Crystal structures reveal the multi-ligand binding mechanism of Staphylococcus aureus ClfB. PLoS Pathog 8, e1002751 (2012).
Seo, H. S., Mu, R., Kim, B. J., Doran, K. S. & Sullam, P. M. Binding of glycoprotein Srr1 of Streptococcus agalactiae to fibrinogen promotes attachment to brain endothelium and the development of meningitis. PLoS Pathog 8, e1002947 (2012).
Seo, H. S. & Sullam, P. M. Characterization of the fibrinogen binding domain of bacteriophage lysin from Streptococcus mitis. Infect Immun 79, 3518–3526 (2011).
Macheboeuf, P. et al. Streptococcal M1 protein constructs a pathological host fibrinogen network. Nature 472, 64–68 (2011).
Whitnack, E. & Beachey, E. H. Biochemical and biological properties of the binding of human fibrinogen to M protein in group A streptococci. J Bacteriol 164, 350–358 (1985).
Flick, M. J. et al. Leukocyte engagement of fibrin(ogen) via the integrin receptor alphaMbeta2/Mac-1 is critical for host inflammatory response in vivo. J Clin Invest 113, 1596–1606 (2004).
Oh, M. H. et al. Autophosphorylation of Tyr-610 in the receptor kinase BAK1 plays a role in brassinosteroid signaling and basal defense gene expression. Proc Natl Acad Sci USA 107, 17827–17832 (2010).
Takamatsu, D., Osaki, M. & Sekizaki, T. Thermosensitive suicide vectors for gene replacement in Streptococcus suis. Plasmid 46, 140–148 (2001).
Liu, P. et al. Streptococcus suis adenosine synthase functions as an effector in evasion of PMN-mediated innate immunit. J Infect Dis 210, 35–45 (2014).
Acknowledgements
This work was supported by grants from the National Basic Research Program (973) of China (2012CB518804) and the National Natural Science Foundation of China (81171528 and 81371766).
Author information
Authors and Affiliations
Contributions
Y.Y. and Y.J. conceived and designed the experiments. Y.P., Y.Y., X.L. and X.W. performed the experiments. Y.P. and Y.Y. analyzed the data. Y.Z. and Y.Y. contributed reagents/materials/analysis tools. Y.Y. wrote the paper.
Ethics declarations
Competing interests
The authors declare no competing financial interests.
Electronic supplementary material
Rights and permissions
This work is licensed under a Creative Commons Attribution 4.0 International License. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in the credit line; if the material is not included under the Creative Commons license, users will need to obtain permission from the license holder to reproduce the material. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/
About this article
Cite this article
Pian, Y., Li, X., Zheng, Y. et al. Binding of Human Fibrinogen to MRP Enhances Streptococcus suis Survival in Host Blood in a αXβ2 Integrin-dependent Manner. Sci Rep 6, 26966 (2016). https://doi.org/10.1038/srep26966
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/srep26966
This article is cited by
-
Proposed virulence-associated genes of Streptococcus suis isolates from the United States serve as predictors of pathogenicity
Porcine Health Management (2021)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.