Abstract
Approximately 80% of new HIV infections in the United States occur in men. Four out of five men diagnosed with HIV infection are men who have sex with men (MSM), with an increasing proportion of young MSM (i.e. ≤24 years of age). We performed a retrospective analysis 11,873 cisgender men participating in a community based HIV screening program in San Diego between 2008 and 2014 to characterize the HIV prevalence and sexual risk behaviors among young men. In young heterosexual men HIV prevalence was lower compared to heterosexual men between 25 and 49 years of age (0.3% vs. 1.4%, p = 0.043). Among young MSM, HIV prevalence was 5.5%, per test positivity rate 3.6%, and HIV incidence 3.4 per 100 person years (95% CI 2.2–5.4). Per test positivity rate (p = 0.008) and incidence (p < 0.001) were significantly higher among young MSM than among MSM above 24-years of age. Young MSM diagnosed with HIV infection reported significantly more serodiscordant condomless anal intercourse, bacterial sexually transmitted infections, and higher rates of methamphetamine and gamma hydroxybutyrate use when compared to young MSM who tested negative. In conclusion, young MSM are particularly vulnerable to HIV infection and may represent ideal candidates for targeted prevention interventions that increase testing uptake and/or decrease the risk of acquiring HIV infection.
Similar content being viewed by others
Introduction
Men account for about 80% of new HIV infections in the United States1. Four out of five men diagnosed with HIV infection are men who have sex with men (MSM). While most HIV infections are still diagnosed in men above 25 years of age, HIV incidence and prevalence among young MSM (i.e. ≤24 years of age) is increasing1,2. In particular black young MSM are disproportionately affected by HIV, accounting for half of new HIV diagnoses among young MSM2,3,4. While a number of studies have evaluated prevalence and incidence of HIV infection among young MSM in settings where African Americans account for a significant proportion of the population3,4,5,6,7,8,9,10, fewer studies have characterized HIV risk among young MSM in other settings of the United States11. The objective of this study was to examine prevalence and incidence of HIV, as well as racial disparities and risk behavior, all stratified by age, among men undergoing community-based testing in San Diego, where African Americans represent less than 7% of the population.
Results
HIV prevalence and incidence, per test positivity rates and demographics in MSM and heterosexual men stratified by age are depicted in Table 1. Young MSM were more likely to report Hispanic ethnicity and less likely white race when compared to older MSM (p < 0.001). Among young MSM, HIV prevalence was 5.5% (95% CI 4.4–6.6%), and per test positivity rate was 3.6% (95% CI 2.9–4.3%). HIV prevalence did not differ between young MSM and MSM between 25 and 49 years of age (5.5% vs. 4.9%, n.s.), but was significantly higher among young MSM than among MSM 50 years or older (5.5% vs. 2.5%, p < 0.001). When compared to MSM above 24 years of age per test positivity rate was significantly higher among young MSM (3.6% vs. 2.2%, p < 0.001). HIV incidence was 3.4 per 100 person years (95% CI 2.2–5.4) among young MSM and therefore significantly higher than among MSM above 24 years of age (HIV incidence 1.6, 95% CI 1.3–2.0; p < 0.001). In contrast, HIV prevalence was lower among young heterosexual men when compared to heterosexual men between 25 and 49 years of age (0.3% vs.1.4%, p = 0.043), and incidence or per-test positivity did not differ by age.
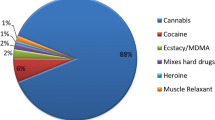
Risk Behaviour reported for the 12 months prior to diagnosis/last HIV test in MSM and heterosexual men ≤24 years and ≥50 years of age (i.e. two groups with significantly differing HIV prevalence among MSM) are depicted in Table 2. Compared to MSM ≥50 years of age, young MSM reported more condomless anal intercourse (p < 0.001), bacterial sexually transmitted infections (STI) (p < 0.001) and non-injection stimulant drug use (p < 0.001), but total number of partners did not differ. Young heterosexual males reported also more female partners and non-injection stimulant drug use when compared to heterosexual men ≥50 years of age. When compared to MSM between 25 and 49 years of age young MSM reported more condomless receptive anal intercourse (CRAI) (p < 0.001), while rates of condomless insertive anal intercourse, bacterial STI, non-injected stimulant drug use and also numbers of partners did not differ significantly (data not shown, risk behaviour for the overall MSM cohort – not stratified by age - published previously19). Markedly lower HIV prevalence and risk behavior was observed in young heterosexual men, resembling those in young cisgender women (HIV prevalence in women 0.4%, median 2 male partners, CRAI in 12.3%, condomless receptive vaginal intercourse in 83%, bacterial STI in 6.6%, non-injection stimulant drug use in 25.4% and IDU in 6%; detailed data not shown). Overall, in MSM and heterosexual men condom use did not differ significantly over the years of the study, and no increase in condomless sex was observed over the study period (detailed data not shown).
For young MSM risk behaviors in those newly diagnosed with HIV infection versus those with negative HIV test results are displayed in Table 3. Median age of those 90 young MSM newly diagnosed with HIV infection was 22 years (IQR 21–23 years). Overall, 40/90 (44%) reported Hispanic ethnicity, 54 (60%) white race, and 3 (3%) black race. Race and ethnicity distributions among young MSM diagnosed with HIV infection did not differ significantly from young MSM with negative HIV test results. Young MSM diagnosed with HIV infection had more condomless anal intercourse and in particular also more CRAI with HIV positive partners (p < 0.001) when compared to those who tested negative (Table 3). In addition bacterial STI (p = 0.002) as well as use of methamphetamine (p < 0.001) and gamma hydroxybutyrate (GHB) (p < 0.001) were significantly more frequent reported by young MSM diagnosed with HIV. San Diego Early test (SDET) risk behavior scores were significantly higher in young MSM diagnosed with HIV compared to those who tested negative (median 3, IQR 1–7 vs. median 2, IQR 0–5; p < 0.001).
Discussion
Our study found that young MSM had the highest incidence of HIV when compared to other MSM, and heterosexual men. While the finding that young MSM are at particular risk for HIV infection confirms results of previous studies3,4,5,7,8,10,12,13,14, it is important to highlight that our findings are not being driven by young African American men as in other parts of the country; only 3% of young MSM diagnosed with HIV reported black race in our cohort (in the most recent census in 2010, 5% of the population of San Diego county was Black or African American). In contrast, Hispanics accounted for 44% of HIV diagnoses among young MSM (Hispanics represented 31.6% of the population of San Diego county). While HIV prevalence rates were about the same in young MSM and those between 25 and 49 years of age (5.5% vs. 4.9%, n.s.), young MSM had significantly fewer testing encounters (25% vs. 35% were repeat testers with the Early Test, p < 0.001), which resulted in higher per-test positivity rates among young MSM (1 out of 28 tests positive) when compared MSM 25 years or older (1 out of 45 tests positive, p < 0.001). Interestingly, those young MSM who underwent voluntary repeat testing were at particular risk for acquiring HIV infection with an incidence rate of 3.4 per 100 person years which was twice as high as the one observed among MSM above 25 years.
When compared to MSM 50 years or older (HIV prevalence 2.5%), significantly higher rates of unprotected anal intercourse, bacterial STI and stimulant substance use were reported among young MSM, whereas total number of partners during the last 12 months did not differ. While higher rates of stimulant substance use may explain the higher rates of condomless anal sex among young MSM15, the observation of a recent study that condom use errors and problems, such as breakage and slippage were very common among young MSM16, may offer additional explanation. However, individual risk behaviors did not fully explain HIV incidence among young MSM which may make a cause for the need to address sociodemographic and structural-level factors in public health interventions targeted toward young MSM5.
In contrast to MSM, young heterosexual men had lower HIV prevalence compared to heterosexual men between 25 and 49 years, and similar prevalence compare to those 50 years or older. Interestingly, the main difference in risk behavior between young heterosexual men and those 50 years or older, besides higher stimulant substance use, was higher numbers of partners, while overall rates of unprotected sex did not differ.
Young MSM diagnosed with HIV infection had more condomless anal intercourse and in particular also more CRAI with serodiscordant partners when compared to young MSM with negative HIV test results. In addition self-reported bacterial STI as well as use of methamphetamine and GHB were significantly more frequent in young MSM diagnosed with HIV. Our findings indicate that at risk young MSM may be ideal candidates for targeted prevention interventions that increase condom use and/or preexposure prophylaxis (PrEP). PrEP with daily tenofovir and emtricitabine has been proven to reduce the acquisition of HIV among MSM by 68% in those who had 90% self-reported adherence17, and over 90% in those with high levels of adherence by TDF drug levels18. Whether high TDF adherence rates can be achieved among young MSM, in particular those with substance use, remains to be determined in future trials.
Our study has several limitations including its single-center and retrospective design. Additionally, incidence rates observed among young MSM in this study, although high, were still markedly lower than those observed previously among some cohorts of young black MSM4,8. Together with our previous finding that black MSM, when compared to white MSM, are more likely to be diagnosed at a late stage of HIV infection19, these findings may indicate that the low number of young black MSM diagnosed with HIV may be a result of infrequent testing.
In conclusion, our study indicates that young MSM across race are particularly vulnerable to HIV infection and may represent ideal candidates for targeted prevention interventions to encourage use of condoms or PrEP, increase HIV testing and/or decrease risk behaviors.
Material and Methods
In this cohort study we analyzed HIV prevalence and incidence, per test positivity rate, and race/ethnicity in 11,873 cisgender men who enrolled in the “Early Test”, a voluntary, community-based, confidential acute and early HIV-screening program in San Diego, California. The “Early Test” provides point-of-care (POC) rapid HIV serologic testing followed by reflex HIV nucleic acid amplification testing (NAT) in all antibody (Ab)-negative persons19,20,21,22,23. Between April 2008 and July 2014, the “Early Test” program provided no cost HIV screening to approximately 4,000 individuals per year at five testing sites in central San Diego plus additional mobile testing sites (including sites targeting MSM at the Lesbian, Gay, Bisexual, Transgender Center and the Gay Men’s Health Clinic; the AntiViral Research Center (AVRC); substance abuse treatment centers; and special community event venues) in San Diego21. Pre-test counseling was provided at each Early Test visit throughout the study period and utilized a client-centered harm reduction model offering personalized risk reduction options21. Demographics and behavioral risks for the previous 12 months were collected using a short 19-question survey [focusing primarily on sexual risk behavior, substance use, and sexually transmitted infection (STI) diagnoses]. In repeat testers, data reported at the most recent Early Test encounter were used. Survey questions were assessed and the form filled out by the testing staff before each HIV testing encounter, and data was later entered into the data system (always in duplicate to minimize data entry errors). After testing negative, MSM clients were recommended to come back 3 months later for the next testing encounter, while those who tested positive were referred to care21.
Study inclusion was limited to cisgender male adolescents and men ≥13 years of age. MSM were defined as men who reported sexual contact with one or more male partners during the previous 12 months and/or self-identified as MSM. Cisgender men not reporting sex with men who did not self-identify as MSM were defined as heterosexual men for study purposes.
Overall, the study included 11,873 men that were stratified by age group (≤24 years, 25 to 49 years, and ≥50 years of age) and sexual behavior (men who did or did not report sex with men). We calculated HIV prevalence and incidence, per test positivity rate as well as demographics for MSM and heterosexual men stratified by age group (≤24 years, 25 to 49 years, and ≥50 years of age). HIV Risk behavior for the overall MSM cohort (i.e. not stratified by age) has been published previously19. As a second step we compared risk behavior between young men (≤24 years) and older men (≥50 years), to evaluate whether risk behavior may offer explanation for differing prevalence and per test positivity rates. Finally we compared risk behavior among young MSM who tested positive for HIV with those young MSM who remained negative (factors associated with acute and early HIV infection and risk behaviors for the overall cohort of MSM and also transgender men and women– not stratified by age – have been published previously19,24).
San Diego Early Test (SDET) scores were calculated as a measure of HIV associated risk behavior25, and compared between young MSM newly diagnosed with HIV infection and those with negative test results. The SDET score was recently developed to better estimate incident HIV infection risk in MSM, as assessed by a score ranging from 0 to 10. The score is based on key risk variables that predict risk of HIV acquisition among MSM: condomless receptive anal intercourse (CRAI), number of male partners, and self-reported bacterial STI. While the SDET score captures changes in sexual risk behavior associated with substance use, the score remains independent of specific regional/individual drug use behavior (e.g. methamphetamine use) and thus may be broadly applicable to MSM populations15.
The UCSD Human Research Protections Program approved the study protocol, consent and all study related procedures. All study participants provided voluntary, written informed consent before any study procedures were undertaken. The methods were carried out in accordance with the approved guidelines. For statistical analysis SPSS 21 (SPSS Inc., Chicago, IL, USA) was used. Proportions were compared using Fishers exact test or Chi-squared test including Yates correction, as appropriate, and two sided p-values were displayed. Continuous variables were compared using Mann Whitney U test due to non-normality of distribution. 95% confidence intervals (CI) were calculated for all rates, using Poisson confidence intervals specifically for incidence rates.
Additional Information
How to cite this article: Hoenigl, M. et al. HIV Infection Rates and Risk Behavior among Young Men undergoing community-based Testing in San Diego. Sci. Rep. 6, 25927; doi: 10.1038/srep25927 (2016).
References
Center for Disease Control and Prevention (CDC). HIV Surveillance Report, 2013. (2015). Available at: http://www.cdc.gov/hiv/pdf/library/reports/surveillance/cdc-hiv-surveillance-report-vol-25.pdf. (Accessed: 4th April 2016).
Centers for Disease Control and Prevention (CDC). Estimated HIV incidence among adults and adolescents in the United States, 2007–2010. (2012). Available at: http://www.cdc.gov/hiv/pdf/statistics_hssr_vol_17_no_4.pdf. (Accessed: 4th April 2016).
Clerkin, E. M., Newcomb, M. E. & Mustanski, B. Unpacking the racial disparity in HIV rates: the effect of race on risky sexual behavior among Black young men who have sex with men (YMSM). J. Behav. Med. 34, 237–243 (2011).
Wejnert, C. et al. Age-Specific Race and Ethnicity Disparities in HIV Infection and Awareness Among Men Who Have Sex With Men-20 US Cities, 2008–2014. J. Infect. Dis. 213, 776–783 (2016).
Balaji, A. B. et al. High HIV incidence and prevalence and associated factors among young MSM, 2008. AIDS 27, 269–278 (2013).
Garofalo, R. et al. Racial/Ethnic Difference in HIV-related Knowledge among Young Men who have Sex with Men and their Association with Condom Errors. Health Educ. J. 74, 518–530 (2015).
Garofalo, R., Hotton, A. L., Kuhns, L. M., Gratzer, B. & Mustanski, B. Incidence of HIV infection and Sexually Transmitted Infections and Related Risk Factors among Very Young Men Who Have Sex with Men. J. Acquir. Immune Defic. Syndr. (2016), 10.1097/QAI.0000000000000933.
Halkitis, P., Kapadia, F. & Ompad, D. Incidence of HIV Infection in Young Gay, Bisexual, and Other YMSM: The P18 Cohort Study. J. Acquir. Immune Defic. Syndr. 69, 466–473 (2015).
Mustanski, B., Newcomb, M. E. & Clerkin, E. M. Relationship characteristics and sexual risk-taking in young men who have sex with men. Health Psychol. 30, 597–605 (2011).
Mustanski, B. S., Newcomb, M. E., Du Bois, S. N., Garcia, S. C. & Grov, C. HIV in young men who have sex with men: a review of epidemiology, risk and protective factors, and interventions. J. Sex Res. 48, 218–253 (2011).
Fernandez, M. I., Perrino, T., Bowen, G. S., Royal, S. & Varga, L. Repeat HIV testing among Hispanic men who have sex with men–a sign of risk, prevention, or reassurance? AIDS Educ. Prev. 15, 105–116 (2003).
Rangsin, R. et al. Risk Factors for HIV Infection among Young Thai Men during 2005-2009. Plos One 10, e0136555 (2015).
Li, Z. et al. Trends of HIV subtypes and phylogenetic dynamics among young men who have sex with men in China, 2009–2014. Sci. Rep. 5, 16708 (2015).
Ellen, J. M. et al. Cross-sectional survey comparing HIV risk behaviours of adolescent and young adult men who have sex with men only and men who have sex with men and women in the U.S. and Puerto Rico. Sex. Transm. Infect. 91, 458–461 (2015).
Hoenigl, M. et al. Clear Links between Starting Methamphetamine and Increasing Sexual Risk Behavior: a cohort study among Men who have Sex with Men. J. Acquir. Immune Defic. Syndr. 71, 551–557 (2016).
Crosby, R. et al. Condom Use Errors and Problems: A Comparative Study of HIV-Positive Versus HIV-Negative Young Black Men Who Have Sex With Men. Sex. Transm. Dis. 42, 634–636 (2015).
Grant, R. M. et al. Preexposure chemoprophylaxis for HIV prevention in men who have sex with men. N. Engl. J. Med. 363, 2587–2599 (2010).
Anderson, P. L. et al. Emtricitabine-tenofovir concentrations and pre-exposure prophylaxis efficacy in men who have sex with men. Sci. Transl. Med. 4, 151ra125 (2012).
Hoenigl, M., Green, N., Mehta, S. R. & Little, S. J. Risk Factors for Acute and Early HIV Infection Among Men Who Have Sex With Men (MSM) in San Diego, 2008 to 2014: A Cohort Study. Medicine (Baltimore) 94, e1242 (2015).
Hoenigl, M., Graff-Zivin, J. & Little, S. J. Costs per diagnosis of acute HIV infection in community-based screening strategies: a comparative analysis of four screening algorithms. Clin. Infect. Dis. 62, 501–511 (2016).
Hoenigl, M. et al. Repeat HIV-testing is associated with an increase in behavioral risk among men who have sex with men: a cohort study. BMC Med. 13, 218-015-0458-5 (2015).
Morris, S. R. et al. Evaluation of an HIV nucleic acid testing program with automated Internet and voicemail systems to deliver results. Ann. Intern. Med. 152, 778–785 (2010).
Hoenigl, M. et al. Signs or Symptoms of Acute HIV Infection in a Cohort Undergoing Community-Based Screening. Emerg Infect Dis 22, http://dx.doi.org/10.3201/eid2203.151607 (2016).
Green, N., Hoenigl, M., Morris, S. R. & Little, S. J. Risk Behavior and Sexually Transmitted Infections Among Transgender Women and Men Undergoing Community-Based Screening for Acute and Early HIV Infection in San Diego. Medicine (Baltimore) 94, e1830 (2015).
Hoenigl, M. et al. Development and Validation of the San Diego Early Test (SDET) Score to Predict Acute and Early HIV Infection Risk in Men who have Sex with Men. Clin. Infect. Dis. 61, 468–575 (2015).
Acknowledgements
This work was supported by funds from the following: Interdisciplicinary Research Fellowship in NeuroAIDS (R25-MH081482), TMARC pilot study (P50DA026306), the Max Kade Foundation, New York (Max Kade Postdoctoral Research grant), the California HIV/AIDS Research Program (CHRP) Grant F13SD321 and the Bettencourt-Schueller Foundation, and grants from the National Institutes of Health: AI106039, AI043638, AI074621, AI108351, and MH100974. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Author information
Authors and Affiliations
Contributions
M.H. was the principal investigator, and designed the study together with S.L., analyzed the data, and drafted the manuscript. A.C. and S.M. helped in analyzing the data and drafting the manuscript. S.J.L. contributed in designing the study, coordinated and supervised data analysis, and helped drafting of the manuscript. All authors revised the manuscript critically for important intellectual content and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
Dr. Hoenigl served on the speakers’ bureau of Merck. Dr. Little reported grant funding from Gilead Sciences, Inc. All other authors no conflicts.
Rights and permissions
This work is licensed under a Creative Commons Attribution 4.0 International License. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in the credit line; if the material is not included under the Creative Commons license, users will need to obtain permission from the license holder to reproduce the material. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/
About this article
Cite this article
Hoenigl, M., Chaillon, A., Morris, S. et al. HIV Infection Rates and Risk Behavior among Young Men undergoing community-based Testing in San Diego. Sci Rep 6, 25927 (2016). https://doi.org/10.1038/srep25927
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/srep25927
This article is cited by
-
Factors affecting optimal adherence to antiretroviral therapy and viral suppression amongst HIV-infected prisoners in South Ethiopia: a comparative cross-sectional study
AIDS Research and Therapy (2022)
-
Design and Delivery of Real-Time Adherence Data to Men Who Have Sex with Men Using Antiretroviral Pre-exposure Prophylaxis via an Ingestible Electronic Sensor
AIDS and Behavior (2021)
-
Universal HIV and Birth Cohort HCV Screening in San Diego Emergency Departments
Scientific Reports (2019)
-
Self-initiated continuation of and adherence to HIV pre-exposure prophylaxis (PrEP) after PrEP demonstration project roll-off in men who have sex with men: associations with risky decision making, impulsivity/disinhibition, and sensation seeking
Journal of NeuroVirology (2019)
-
Molecular Epidemiology of the HIV Epidemic in Three German Metropolitan Regions – Cologne/Bonn, Munich and Hannover, 1999–2016
Scientific Reports (2018)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.