Abstract
Most of the existing data on real-life management of bipolar disorder are from studies conducted in western countries (mostly United States and Europe). This multinational, observational cohort study aimed to describe the management and clinical outcomes of bipolar patients in real-life conditions across various intercontinental countries (Bangladesh, Egypt, Iran, Israel, Tunisia, and Ukraine). Data on socio-demographic and disease characteristics, current symptomatology, and pharmacological treatment were collected. Comparisons between groups were performed using standard statistical tests. Overall, 1180 patients were included. The median time from initial diagnosis was 80 months. Major depressive disorder was the most common initial diagnosis. Mood stabilizers and antipsychotics were the most common drugs being prescribed at the time of the study. Antidepressants (mainly selective serotonin uptake inhibitors [SSRIs]) were administered to 36.1% of patients. Patients with bipolar I disorder received higher number of antipsychotics and anxiolytics than those with bipolar II disorder (p < 0.001). Presence of depressive symptoms was associated with an increase in antidepressant use (p < 0.001). Bipolar disorder real-life management practice, irrespective of region, shows a delay in diagnosis and an overuse of antidepressants. Clinical decision-making appears to be based on a multidimensional approach related to current symptomatology and type of bipolar disorder.
Similar content being viewed by others
Introduction
Bipolar disorder (BD) is a recurrent and chronic disease characterized by the occurrence of manic (or hypomanic), depressive, or mixed episodes. According to the World Health Organization, BD is one of the world’s ten most disabling conditions1. Several studies have shown that a considerable proportion of BD patients (30–60%) in clinical remission live with significant functional impairment2,3,4,5,6. In the general population, the estimated lifetime prevalence of BD is approximately 0.2–5% and increases to 6% for a broad range of bipolar spectrum disorders7,8,9,10. A first depressive episode, the presence of psychotic symptoms, and/or various comorbidities can dissimulate bipolar symptoms and may result in a delay in the diagnosis of BD. An estimated 35–45% of BD patients are misdiagnosed with unipolar depression11,12,13,14, and delays of up to 20 years from the onset of symptoms to the first mood stabiliser treatment have been reported11. Although the disease burden appears equivalent in both BD types12, the longitudinal course of patients with bipolar II disorder (age of onset, clinical course, predominant polarity, duration of episodes, and suicidality) differs from patients with bipolar I disorder13. Consequently, the risks of delayed diagnosis and misdiagnosis (as unipolar depressive disorder, personality disorders, or mild bipolar I disorder) are likely to be higher in bipolar II patients than in bipolar I patients.
Management of BD (type I or II) comprises complex treatment regimens to achieve the stabilisation of a mood episode and then the prevention of relapses or recurrences to allow for functional recovery. In recent decades, an increasing number of drugs, including lithium, anticonvulsants, and more recently second-generation antipsychotics, have been approved for the treatment of BD, presenting a new challenge for clinicians in choosing the most appropriate medication. Numerous guidelines have been developed by national agencies and professional organisations to guide clinicians to make their choice in the practice of appropriate evidence-based care14,15,16,17,18. However, many clinicians do not adhere to guidelines in routine practice, potentially due to negative attitudes toward guidelines (guidelines “are published by experts and not clinicians,” “are biased,” and “do not correspond to my patients” were some of the more telling responses from clinicians recently surveyed about their perceptions of the methods used in the evidence based-guidelines)19,20. Indeed, guidelines are often limited by the fact that they are typically based on the positive results of randomised controlled double-blind trials, which include BD patients only under restrictive criteria (e.g., monotherapy, exclusion of patients with medical or psychiatric comorbidities) and for a limited duration of assessment. Considering the gap between the highly selected, controlled evidence from research studies and the management of BD patients in real-life conditions, the applicability of guidelines in routine practice can be difficult to ascertain. Furthermore, the clinical management of BD patients can be affected by local customs, expert opinions, relationships with pharmaceutical industry, or politico-economic environments.
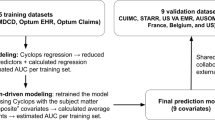
Most of the existing data on management of BD in real-life conditions are from studies conducted in western countries (particularly the United States and Europe)21,22,23,24,25,26,27,28,29,30,31,32,33. Few published trials have evaluated patients from other countries, and the data from these trials are very limited34. Therefore, the primary aim of the MAnagement of biPolar disorder in INtercontinental reGion (MAPING) study was to provide information on the management of BD patients in conditions representative of routine clinical practice across different countries (Bangladesh, Egypt, Iran, Israel, Tunisia, and Ukraine) from the intercontinental region. Secondary objectives were to compare clinical outcomes and management of patients according to BD type and current bipolar symptoms.
Methods
MAPING was an international, multicentre, non-interventional, cross-sectional study in adult BD patients conducted between September 2013 and May 2014. The study was performed in accordance with the Declaration of Helsinki and was carried out with the approved guidelines. All experiments were approved by Institutional Review Board or Institutional Ethics Committee from each participating country (Tehran university of medical science, Tehran, Iran; Razi hospital, La Manouba, Tunisia; Hadassah Hospital, Jerusalem, Israel; Kyiv City Clinical Psycho-neurological Hospital, Kiev, Ukraine; Sher-e-Bangla Hospital, Dhaka, Bangladesh; Ain Shams Hospital, Cairo, Egypt). All patients provided written informed consent to participate in the study.
Selection of physicians
A feasibility study was conducted in potential study centres to confirm the capacity of potential sites to recruit the targeted study population. In order to ensure representativeness of the sample, 90 investigational sites (including psychiatric hospitals, general hospitals, and community office-based practices) were randomly selected from the pre-established list of study sites in Bangladesh, Egypt, Iran, Israel, Tunisia, and Ukraine. In the event that a physician declined to participate, s/he was replaced by the next physician on the randomised list.
Patient selection
The study included patients aged ≥18 years fulfilling Diagnostic and Statistical Manual of Mental Disorders-Fourth Edition-Text Revision (DSM-IV-TR) diagnostic criteria for BD type I, type II, or not otherwise specified, and gave the informed consent. Exclusion criteria were concurrent enrolment in another study and presence of any acute physical condition. All consecutive eligible patients, at each site, were included in the study for a period of 8 months.
Data collection
A site questionnaire collected the following information on the physicians: age, gender, specialty, years of practicing, main workplace (hospital, community, others), location, number of BD patients seen per month, knowledge and use of international and/or national guidelines (very frequently, from time to time, never).
Patients’ data were collected in a single visit by physician, who completed a case report form for each patient. Information collected included:
-
Eligibility, date of visit and informed consent
-
Patient characteristics: socio-demographic data (age, sex, area of residence, marital status, educational level, and medication health coverage), employment status, work disability, and physical comorbidities;
-
Disease characteristics: type of BD, number of episodes and psychiatric hospitalizations during the last 12 months, predominant polarity of episodes (manic or depressive predominant polarity), family history of psychiatric history, age at initial diagnosis, initial diagnosis type, age at BD diagnosis, socio-familial and occupational functioning during the last 2 months (assessed by the Global Assessment of Functioning [GAF] scale35);
-
Current bipolar symptoms listed in the DSM-IV-TR diagnostic criteria for BD: manic symptoms (feeling unusually “high” and optimistic or extremely irritable, grandiose beliefs about one’s abilities or powers, sleeping very little but feeling extremely energetic, talking so rapidly that others can’t keep up, racing thoughts, highly distractible or unable to concentrate, impaired judgment and impulsiveness, acting recklessly without thinking about the consequences, delusions, and hallucinations) and depressive symptoms (feeling hopeless or sad or empty, changes in appetite or weight, sleep disturbances, concentration and memory problems, feeling of worthlessness or guilt, thoughts of death or suicide, irritability, inability to experience pleasure, fatigue or loss of energy, and physical and mental sluggishness);
-
Pharmacological treatment: treatment received at the time of initial diagnosis, antidepressant therapy at least once in life and if yes, the response to antidepressant (manic/hypomanic switches, resistance to treatment, mood lability, irritability, and unknown) and ongoing pharmacological treatment (mood stabilisers including lithium and anticonvulsants, first or second-generation antipsychotics, antidepressants, and electroconvulsive therapy).
Statistical methods
The primary endpoint was the description of BD management across various countries, which included pharmacological treatment received or ongoing, psychiatric hospitalizations during the last 12 months and other healthcare resources use.
Secondary endpoints included the description of patients’ and diseases’ characteristics.
Comparisons were performed among:
-
BD type I versus type II for the duration between initial identification of a pathological state and BD diagnosis (months), employment status, work disability, GAF score during the last 2 months, and ongoing pharmacological treatment (defined by class).
-
Current bipolar symptoms and previous use of antidepressant (lifetime).
All analyses were conducted on the analysis population, by country and overall. The analysis population consisted of all patients enrolled in the study who met all inclusion/exclusion criteria.
Descriptive statistics of continuous variables were presented as the number of data analyzed, mean, standard deviation, median, quartiles and extreme values. Descriptive statistics of categorical variables were presented as the number and proportion of patients in each category. Missing data were not counted in the percentage.
Statistical comparisons between groups were performed using Chi-square test or Fisher’s exact test for categorical variables. Quantitative variables were compared using the Student’s t-test when normality is verified or the Wilcoxon Mann-Whitney test otherwise. All analyses were two-tailed, and significance was set at p < 0.05.
All comparisons performed and all p-value calculated were provided only for descriptive purpose.
Bonferroni correction was applied for multiple testing (adjusted p = 0.0025).
Statistical analysis was performed using SAS version 9.2 (SAS Institute, Cary, NC).
Results
Overall, 89 participating physicians in hospital- and office-based settings screened 1447 patients diagnosed with BD. Of these patients, 1180 (81.5%) were included in the trial as the eligible population for the statistical analysis. The main reason for non-inclusion was patient refusal. Table 1 summarizes the number of sites and participating physicians and the number of screened, included, and eligible patients.
Study sample characteristics
Physician characteristics
The mean age of participating physicians (77.5% men) was 50.6 ± 8.2 years with an average of 21.4 ± 8.3 years of practice. The median number of BD patients seen per month was 40. Most physicians (82.2%) used international guidelines very frequently (49.4%) or from time to time (48.3%).
Patient characteristics
Mean age was 37.9 ± 13.2 years, and 52.8% of patients were men (Table 2). Most patients were married and living in urban area. Overall, 79.8% of patients had a secondary or higher level of education, ranging from 61.3% in Bangladesh to 98.6% in Ukraine. For 52, 9% of patients, the medication health coverage was as out of pocket. Over half of the patients were unemployed, of whom, 47.0% of patients were unemployed because of a work disability.
Few patients (<17%) had past or existing physical comorbidities: the most frequent comorbidities were obesity, cardiovascular disease, diabetes, and thyroid disorder. Moreover, less than 6% of patients had a medical or surgical history of respiratory diseases, migraine, infectious diseases, or renal insufficiency.
Disease characteristics
Overall, 72.2% and 25.7% of patients were diagnosed with BD type I and type II, respectively, (Table 2). The median time from initial diagnosis was 80 months (range: 0–608). Most patients (64.4%) were diagnosed before the age of 30. Major depressive disorder and BD were the predominant initial diagnoses (36.4% and 20.2%, respectively).
Most patients (80.8%) had experienced between one and three episodes in the last 12 months. The predominant polarity of episodes was manic (65.9%).
One third of patients had a first-degree relative suffering from BD.
Global assessment of functioning during the last two months revealed moderate social, familial, and occupational dysfunction with a mean GAF score of 54.7 ± 19.7.
Therapeutic management of BD
Therapies received at time of initial diagnosis
Overall, 67.2% of patients had received antipsychotic drugs at initial diagnosis, among them 51.1% received first-generation and 51.6% second-generation (Table 3). Moreover, 44.4% of patients had received antidepressants at initial diagnosis, mainly selective serotonin reuptake inhibitors (SSRIs; 67.2%). Mood stabilizers and anxiolytics were prescribed at initial diagnosis to an equivalent number of patients (29.7% and 30.0%, respectively).
Among the 63.8% patients who had received antidepressant at least once in lifetime, 46.1% experienced manic or hypomanic switches, 30.3% experienced irritability, and 29.6% experienced mood lability.
Ongoing pharmacological treatment
At the time of the study 85.7% of patients were being treated with mood stabilizers, mostly anticonvulsants (84.3%), and 83.4% of patients were receiving antipsychotics with a predominance of second-generation antipsychotics (79.6%), (Table 3). Anxiolytics were the third most frequently received therapy in 51.4% of patients. Antidepressants were being administered to 36.1% of patients (mainly SSRIs).
Psychiatric hospitalizations
46.0% of patients had at least one psychiatric hospitalization in the last 12 months, (Table 3).
BD management according to type of BD and current symptomatology
BD type I versus BD type II
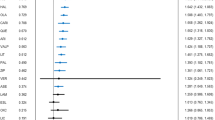
The average time from initial diagnosis to BD diagnosis was shorter for BD I patients (median, 0.8 years) than for BD II patients (median, 2.2 years), (Table 4). There was no observed difference in employment status and work disability based on the type of BD. However, BD I patients had a lower GAF score than BD II patients (53.8 ± 20.0 versus 56.9 ± 18.5, p = 0.017). BD I patients received more first-generation antipsychotics and anxiolytics than BD II patients (p < 0.001). Second-generation antipsychotics were used by more patients suffering from BD II than BD I (91.8% versus 75.9%). BD II patients received more antidepressants than BD I patients (p < 0.001). SSRIs remained the most common antidepressant for BD I (76.4%) and BD II (80.1%).
Current bipolar symptoms and treatment
Current symptoms of mania were associated with an increase in antipsychotic drug prescription (e.g., from 78.7% to 91.2% for “unrealistic or grandiose beliefs about one’s abilities or powers” (p < 0.001)). Patients who reported “racing thoughts: jumping quickly from one idea to the next” or “sleeping very little, but feeling extremely energetic,” used more mood stabilizers than others (90.0% versus 83.2%, p = 0.001 and 88.6% versus 82.6%, p = 0.003, respectively). Mania was also associated with decrease in antidepressant drug prescription.
Existing symptoms of bipolar depression were associated with a decrease in antipsychotic drug prescription (except for “feelings of worthlessness or guilt”, “thoughts of death or suicide”, and “irritability” (p < 0.01)) and an increase in antidepressant drug prescription (e.g., from 21.5% to 73.3% for “hopelessness, sadness or emptiness feelings” (p < 0.001)).
Most of these results (except decrease of antipsychotic prescription according to the presence of depressive symptoms) remained significant after Bonferroni correction (p < 0.0025).
Discussion
This is the primary report from the MAPING study, which was designed to describe the clinical management of BD under real-life conditions across 6 countries (Bangladesh, Egypt, Iran, Israel, Tunisia, and Ukraine) from the intercontinental region.
Our findings show that, in the countries included:
-
There is frequent initial misdiagnosis as major depressive disorder with resultant delay in the diagnosis of BD;
-
Preferential use of anticonvulsants and second-generation antipsychotics in the treatment of BD with an overuse of antidepressants;
-
Decision-making about treatment is based on BD type and existing symptoms.
In spite of some cultural aspects such as difference in medication health coverage, this is greatly similar to the clinical management of patients with BD in western countries24,25,26,27,28,29,30,31,32,33.
The challenges in diagnosing BD at the onset of disease arise from its complex and heterogeneous clinical presentation. As the first mood episode is frequently a depressive phase for BD patients, major depressive disorder was the predominant initial diagnosis in our study. The lifetime prevalence of major depressive disorder is approximately 4 times that of BD spectrum disorders, and the clinical presentation of a bipolar depression episode does not differ significantly from unipolar depression36. Consequently, there is often a delay of several years between initial diagnosis and BD diagnosis, associated with an initial over-prescription of antidepressants in 44.4% of patients. This issue is even more problematic in BD II patients, who are less quickly identified and consequently receive more antidepressants than BD I patients. The challenges of accurately identifying BD patients in clinical practice are similarly reported in western countries36,37,38. Therefore, the systematic screening of depressive patients with accurate assessment scales to identify hypomanic episodes, and the consideration of clinical characteristics associated with bipolar depression (family history of BD, earlier onset of illness, seasonality, mood reactivity, switching on antidepressants, history of suicide attempt) needed to be implemented in routine practice in all countries over the world13,36,39,40. In the future, an integrative approach with combinations of objective biomarkers could help in the differentiation between BD and unipolar depression41.
Overall, the most commonly prescribed medications were anticonvulsants, second-generation antipsychotics, and anxiolytics (almost always benzodiazepines). Over one third of patients were treated with antidepressants in spite of the increased risks of manic switches, irritability, mood lability, or inadequate response to treatment. Previous studies in western countries found the same trends of prescription in the treatment of BD. Psychotropic medications mainly involved antidepressants, anticonvulsants and second-generation antipsychotics in the United States28,30 and the European countries25.
Although most participating psychiatrists regularly used international guidelines to facilitate decision-making about treatment for BD management, they reported a preference for certain drugs depending on the type of BD or current bipolar symptoms. The presence of manic symptoms was associated with an increased use of antipsychotics and a decreased use of antidepressants. Conversely, depressive symptoms were associated with an increased use of antidepressants and a decreased use of antipsychotics. BD I patients received more first-generation antipsychotics and anxiolytics and BD II patients received more SSRIs, antidepressants, and second-generation antipsychotics. These findings are again in accordance with western studies. Several observational studies found highest antidepressant use in depression and higher second-generation antipsychotic prescription in mania25,30,32. In European countries, the BD II patients received more antidepressants33 and the BD I patients were treated with more antipsychotics in monotherapy or combination29.
Although most guidelines have focused on the use of mood stabilizers and not antidepressants, which are never recommended as monotherapy for acute or maintenance BD therapy, the use of antidepressants for the treatment of BD patients is still controversial42. As per certain international guidelines, insufficient levels of evidence justify that SSRIs in combination with mood stabilizers should not be recommended in bipolar depression, whereas other guidelines are more flexible regarding the use of antidepressants, particularly for BD II patients43. Inconclusive evidence is also available to consider antidepressant in combination with a prophylactic agent in the prevention of depressive episode42. All guidelines recommend avoiding antidepressant in patients with rapid cycling or history of mood switch during their use. If recent studies showed the possible interest of modern antidepressants in BD type II patients with lower risk of switching than BD type I, larger prospective trials are needed to confirm these findings44,45. The lack of expert consensus, paucity of evidence, and variability in guideline quality46 may explain the frequent use of antidepressants in our study but also in western countries.
Another relevant finding is the low rate of lithium use in comparison with anticonvulsants and second-generation antipsychotics, despite the fact that all international guidelines consider lithium as a first-line treatment in the acute manic phase and for prophylaxis47. As described in previous western studies19,25,26,27,30, the use of lithium seems to be declining due to clinicians’ apprehensions regarding the risk of side effects or intoxication, the long onset of action, or the practicability. The decline may also be the result of the recent development of second-generation antipsychotics for treatment of BD, and the lack of promotion of lithium, which is a generic and old medication.
Despite the large sample size, this study has several limitations. The cross-sectional design does not allow analysis of the causal relationship between the outcomes associated with management of bipolar patients and the different variables tested. The study did not involve all countries from the Middle East, Africa, South Asia, or Eurasia but selected some countries from these regions. The results cannot be considered as representative of routine clinical practice of regions that were not included in this study. Therefore, the analyses performed did not directly compare these intercontinental regions to each other. The high rates of type I BD and manic predominant polarity in this study, even if their prevalence varied broadly across studies, represent another limitation, which may be related to a selection bias.
Finally, the assessment of BD management was limited to patients who had access to the mental health care system, and BD patients without access to such care were not assessed.
In conclusion, the MAPING study provides relevant information on the management of BD patients in conditions representative of everyday clinical practice across 6 countries from the intercontinental region. An analysis of the findings indicates broad similarities in clinical management of BD patients included and those more widely studied in western countries. The real-life management of BD, irrespective of the country or region, shows a delay in diagnosis and is associated with a substantial use of antipsychotics, anticonvulsants, and SSRIs. Moreover, clinicians appear to base their decision making on a multidimensional approach related to the presence of manic or depressive symptoms. Taken together, management of patients with BD II presented some specific differences compared to management of those with BD I.
Additional Information
How to cite this article: Samalin, L. et al. Management of bipolar disorder in the intercontinental region: an international, multicenter, non-interventional, cross-sectional study in real-life conditions. Sci. Rep. 6, 25920; doi: 10.1038/srep25920 (2016).
References
World Health Organization. The Global Burden of Disease: 2004 Update. (2008) Available at:http://www.who.int/healthinfo/global_burden_disease/2004_report_update/en/ (Accessed: 28th September 2015).
Samalin, L. et al. Residual symptoms and functional performance in a large sample of euthymic bipolar patients in France (the OPTHYMUM study). J. Affect. Disord. 159, 94–102 (2014).
Sanchez-Moreno, J. et al. Functioning and disability in bipolar disorder: an extensive review. Psychother. Psychosom. 78, 285–297 (2009).
Bauer, M. S., Kirk, G., Gavin, C. & Williford, W. O. Determinants of functional outcome and healthcare costs in bipolar disorder: a high-intensity follow-up study. J. Affect. Disord. 65, 231–241 (2001).
Kleinman, L. et al. Costs of bipolar disorder. Pharmaco-economics 21, 601–622 (2001).
Bryant-Comstock, L., Stender, M. & Devercelli, G. Health care utilization and costs among privately insured patients with bipolar I disorder. Bipolar Disord. 4, 398–405 (2002).
Kessler, R. C. et al. Lifetime and 12-month prevalence of DSM-III-R psychiatric disorders in the United States. Results from the National Comorbidity Survey. Arch. Gen. Psychiatry 51, 8–19 (1994).
Weissman, M. et al. Cross-national epidemiology of major depression and bipolar disorder. JAMA 276, 293–299 (1996).
Waraich, P., Goldner, E. M., Somers, J. M. & Hsu, L. Prevalence and incidence studies of mood disorders: a systematic review of the literature. Can J Psychiatry 49, 124–138 (2004).
Angst, J. The emerging epidemiology of hypomania and bipolar II disorder. J. Affect. Disord. 50, 143–151 (1998).
Hirschfeld, R. M. Bipolar spectrum disorder: improving its recognition and diagnosis. J. Clin. Psychiatry 62, 5–9 (2001).
Merikangas, K. R. & Lamers, F. The ‘true’ prevalence of bipolar II disorder. Curr. Opin. Psychiatry 25, 19–23 (2012).
Vieta, E. & Suppes, T. Bipolar II disorder: arguments for and against a distinct diagnostic entity. Bipolar Disord. 10, 163–178 (2008).
Goodwin, G. M. et al. Evidence-based guidelines for treating bipolar bipolar disorder: revised third edition recommendations from the British Association for Psychopharmacology. J. Psycho-pharmacol. [cited 2016 Mar 15] doi:10.1177/0269881116636545. (2016).
Grunze, H. et al. The World Federation of Societies of Biological Psychiatry (WFSBP) guidelines for the biological treatment of bipolar disorders: update 2012 on the long-term treatment of bipolar disorder. World J. Biol. Psychiatry 14, 154–219 (2013).
National Institute for Health and Clinical Excellence. Bipolar disorder: the assessment and management of bipolar disorder in adults, children and young people in primary and secondary care (2015) Available at: http://www.nice.org.uk/guidance/cg185/resources/guidance-bipolar-disorder-the-assessment-and-management-of-bipolar-disorder-in-adults-children-and-young-people-in-primary-and-secondary-care-pdf. (Accessed: 28th September 2015).
Yatham, L. N. et al. Canadian Network for Mood and Anxiety Treatments (CANMAT) and International Society for Bipolar Disorders (ISBD) collaborative update of CANMAT guidelines for the management of patients with bipolar disorder: update 2013. Bipolar Disord. 15, 1–44 (2013).
Malhi, G. S. et al. Clinical practice recommendations for bipolar disorder. Acta Psychiatr. Scand. Suppl. 439, 27–46 (2009).
Samalin, L., Guillaume, S., Auclair, C. & Llorca, P. M. Adherence to guidelines by French psychiatrists in their real world of clinical practice. J. Nerv. Ment. Dis. 199, 239–243 (2011).
Perlis, R. H. Use of treatment guidelines in clinical decision making in bipolar disorder: a pilot survey of clinicians. Curr. Med. Res. Opin. 23, 467–475 (2007).
Haro, J. M. et al. Evidence for three distinct classes of ‘typical’, ‘psychotic’ and ‘dual’ mania: results from the EMBLEM study. Acta Psychiatr. Scand. 113, 112–120 (2006).
Henry, C. et al. A French network of bipolar expert centres: a model to close the gap between evidence-based medicine and routine practice. J. Affect. Disord. 131, 358–363 (2011).
Sachs, G. S. et al. Rationale, design and methods of the systematic treatment enhancement program for bipolar disorder (STEP-BD). Biol. Psychiatry 53, 1028–1042 (2003).
Ghaemi, S. N. et al. Pharmacological Treatment Patterns at Study Entry for the First 500 STEP-BD Participants. Psychiatr. Serv. 57, 660–665 (2006).
Vieta, E. et al. Clinical management and burden of bipolar disorder: results from a multinational longitudinal study (WAVE-bd). Int. J. Neuropsychopharmacol. 16, 1719–1732 (2013).
Carlborg, A., Ferntoft, L., Thuresson, M. & Bodegard, J. Population study of disease burden, management, and treatment of bipolar disorder in Sweden: a retrospective observational registry study. Bipolar Disord. 17, 76–85 (2015).
Hayes, J. et al. Prescribing trends in bipolar disorder: cohort study in the United Kingdom THIN primary care database 1995–2009. PLos One 6, e28725 (2011).
Baldessarini, R., Henk, H., Sklar, A., Chang, J. & Leahy, L. Psychotropic medications for patients with bipolar disorder in the United States: polytherapy and adherence. Psychiatr. Serv. 59, 1175–1183 (2008).
Grande, I. et al. Patterns of pharmacological maintenance treatment in a community mental health services bipolar disorder cohort study (SIN-DEPRES). Int. J. Neuro-psychopharmacol. 16, 513–523 (2013).
Blanco, C., Laje, G., Olfson, M., Marcus, S. C. & Pincus, H. A. Trends in the treatment of bipolar disorder by outpatient psychiatrists. Am. J. Psychiatry 159, 1005–1010 (2002).
Walpoth-Niederwanger, M. et al. Treatment patterns in inpatients with bipolar disorder at a psychiatric university hospital over a 9-year period: focus on mood stabilizers. Int. Clin. Psychopharmacol. 27, 256–266 (2012).
Kessing, L. V., Vradi, E. & Andersen, P. K. Nationwide and population-based prescription patterns in bipolar disorder. Bipolar Disord. 18, 174–182 (2016).
Karanti, A., Kardell, M., Lundberg, U. & Landén, M. Changes in mood stabilizer prescription patterns in bipolar disorder. J. Affect. Disord. 195, 50–56 (2016).
Okasha, T. A. et al. Longer-term treatment of patients with bipolar disorder: a 9-month observational study in Central and Eastern Europe, the Middle East and Africa. Curr. Med. Res. Opin. 25, 1889–1900 (2009).
Hall, R. C. W. Global Assessment of Functioning: A Modified Scale. Psychosomatics 36, 267–275 (1995).
Hirschfeld, R. M. Differential diagnosis of bipolar disorder and major depressive disorder. J. Affect. Disord. 169, 12–16 (2014).
Ghouse, A. A., Sanches, M., Zunta-Soares, G., Swann, A. C. & Soares, J. C. Over diagnosis of bipolar disorder: a critical analysis of the literature. Scientific World Journal 2013, 297087 (2013).
Keck, P. E., Kessler, R. C. & Ross, R. Clinical and economic effects of unrecognized or inadequately treated bipolar disorder. J. Psychiatr. Pract. 14, 31–38 (2008).
Carvalho, A. F. et al. Screening for bipolar spectrum disorders: A comprehensive meta-analysis of accuracy studies. J. Affect. Disord. 172C, 337–346 (2014).
Mitchell, A. J. Clinical utility of screening for clinical depression and bipolar disorder. Curr. Opin. Psychiatry 25, 24–31 (2012).
Phillips, M. L. & Kupfer, D. J. Bipolar disorder diagnosis: challenges and future directions. The Lancet 381, 1663–1671 (2013).
Pacchiarotti, I. et al. The International Society for Bipolar Disorders (ISBD) task force report on antidepressant use in bipolar disorders. Am. J. Psychiatry 170, 1249–1262 (2013).
Samalin, L. et al. Methodological differences between pharmacological treatment guidelines for bipolar disorder: what to do for the clinicians? Compr. Psychiatry 54, 309–320 (2013).
Amsterdam, J. D. et al. Safety and effectiveness of continuation antidepressant versus mood stabilizer monotherapy for relapse-prevention of bipolar II depression: A randomized, double-blind, parallel-group, prospective study. J Affect. Disord. 185, 31–37 (2015).
Amsterdam, J. D. & Shults, J. Efficacy and safety of long-term fluoxetine versus lithium monotherapy of bipolar II disorder: a randomized, double-blind, placebo-substitution study. Am. J. Psychiatry 167, 792–800 (2010).
Castellani, A., Girlanda, F. & Barbui, C. Rigor of development of clinical practice guidelines for the pharmacological treatment of bipolar disorder: systematic review. J. Affect. Disord. 174, 45–50 (2015).
Nivoli, A. M., Murru, A. & Vieta, E. Lithium: still a cornerstone in the long-term treatment in bipolar disorder? Neuro-psychobiology 62, 27–35 (2010).
Acknowledgements
This study was funded by Sanofi. The Sponsor had no involvement in the study design, data analysis and collection, or publication of the report. The authors are grateful to the investigators involved in the study.
Author information
Authors and Affiliations
Contributions
P.M.L. was responsible for the concept and design of the study. L.M. extracted and performed the statistical analysis. L.S., E.V. and P.M.L. wrote the manuscript. L.S., E.V., T.A.O., J.U., S.A.A.A., F.N., V.M., D.A., Y.R., L.M.M., I.S. and P.M.L. were involved in revision of the manuscript and approved the final version of the manuscript.
Corresponding author
Ethics declarations
Competing interests
Dr Samalin received grants, honoraria, or consulting fees from AstraZeneca, Bristol-Myers Squibb, Janssen-Cilag, Lundbeck, Otsuka, Sanofi, and Takeda. Pr Vieta received grants, CMErelated honoraria, or consulting fees from Alexza, Almirall, AstraZeneca, Bristol-Myers Squibb, Cephalon, Eli Lilly, Ferrer, Forest Research Institute, Gedeon Richter, GlaxoSmithKline, Janssen, Janssen-Cilag, Jazz, Johnson & Johnson, Lundbeck, Merck, Novartis, Organon, Otsuka, Pfizer, Pierre-Fabre, Qualigen, Roche, Sanofi, Schering-Plough, Servier, Shire, Solvay, Takeda, Teva, CIBERSAM, the Seventh European FrameWork Programme (ENBREC), the Stanley Medical Research Institute, United Bio-source Corporation, and Wyeth. Pr Okasha received honoraria from Sanofi. Dr Jalal Uddin received honoraria from Sanofi. Dr Ahmadi Abhari received grants, honoraria, or consulting fees from Pfizer, Actover, Bayer, Sanofi and Shafayab Pr Nacef received honoraria for consulting and lecturers from Sanofi Pr Mishyiev received honoraria for consulting and lecturers from Sanofi, Lundbeck and Janssen. Pr Aizenberg received honoraria from Sanofi. Dr Ratner received honoraria from Sanofi. Pr Llorca received grants, honoraria, or consulting fees from AstraZeneca, Bristol-Myers Squibb, Eli Lilly, Ferrer, Janssen-Cilag, Lundbeck, Otsuka, Sanofi, Servier, and Takeda.
Rights and permissions
This work is licensed under a Creative Commons Attribution 4.0 International License. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in the credit line; if the material is not included under the Creative Commons license, users will need to obtain permission from the license holder to reproduce the material. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/
About this article
Cite this article
Samalin, L., Vieta, E., Okasha, T. et al. Management of bipolar disorder in the intercontinental region: an international, multicenter, non-interventional, cross-sectional study in real-life conditions. Sci Rep 6, 25920 (2016). https://doi.org/10.1038/srep25920
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/srep25920
This article is cited by
-
Prevalence, Predictors, and Diagnostic Dilemmas: State of Bipolar Disorder in Post-Secondary Students in WHO EMRO
International Journal of Mental Health and Addiction (2019)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.